Examination of the Quality of Particulate and Filtered Mandibular Bone Chips for Oral Implants: An In Vitro Study
Abstract
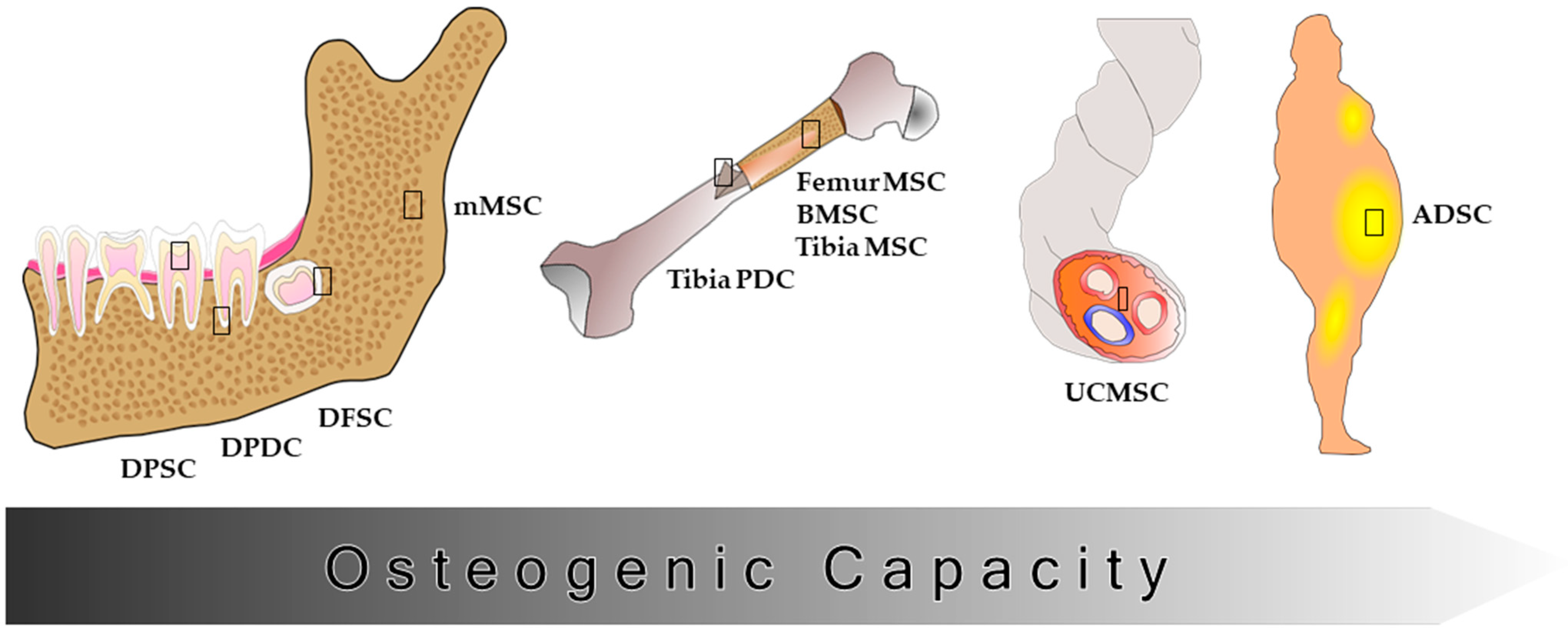
1. Introduction
2. Materials and Methods
2.1. Patient Groups
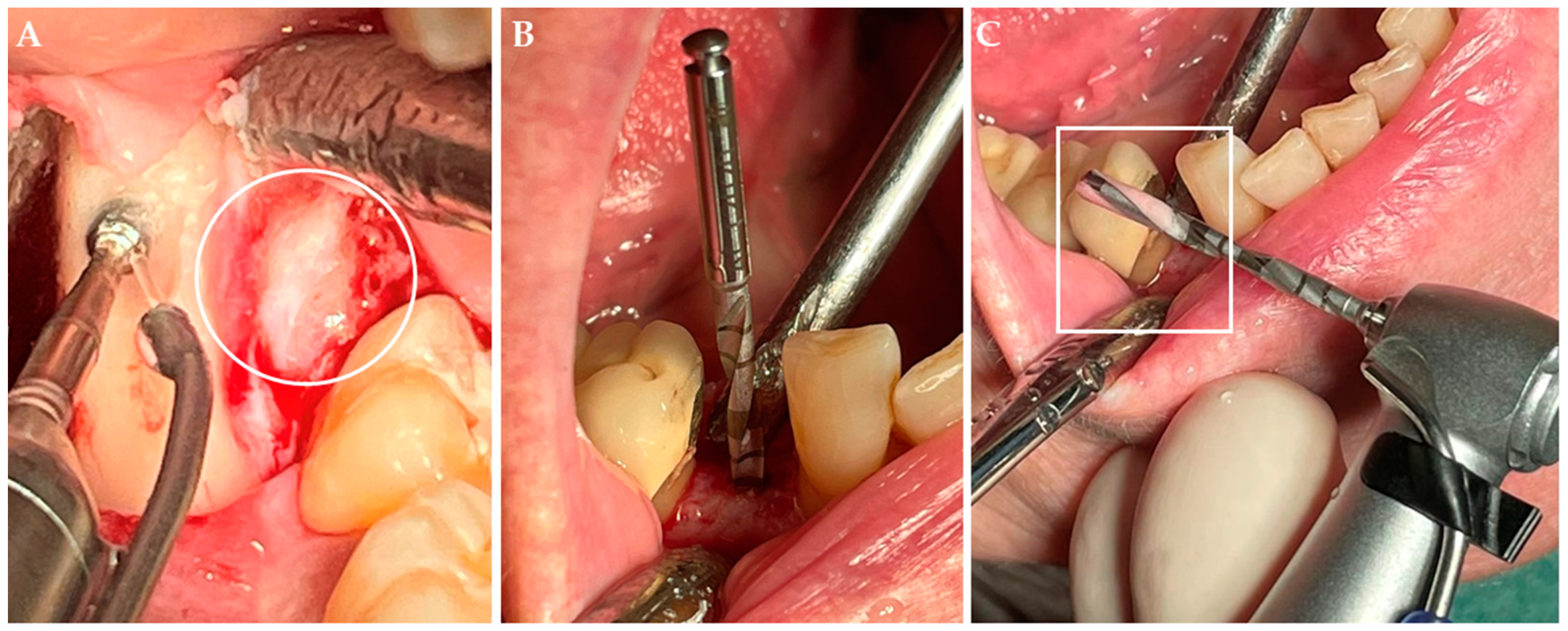
2.2. Surgical Procedure
2.3. Sample Size Measurement
2.4. Cell Culture
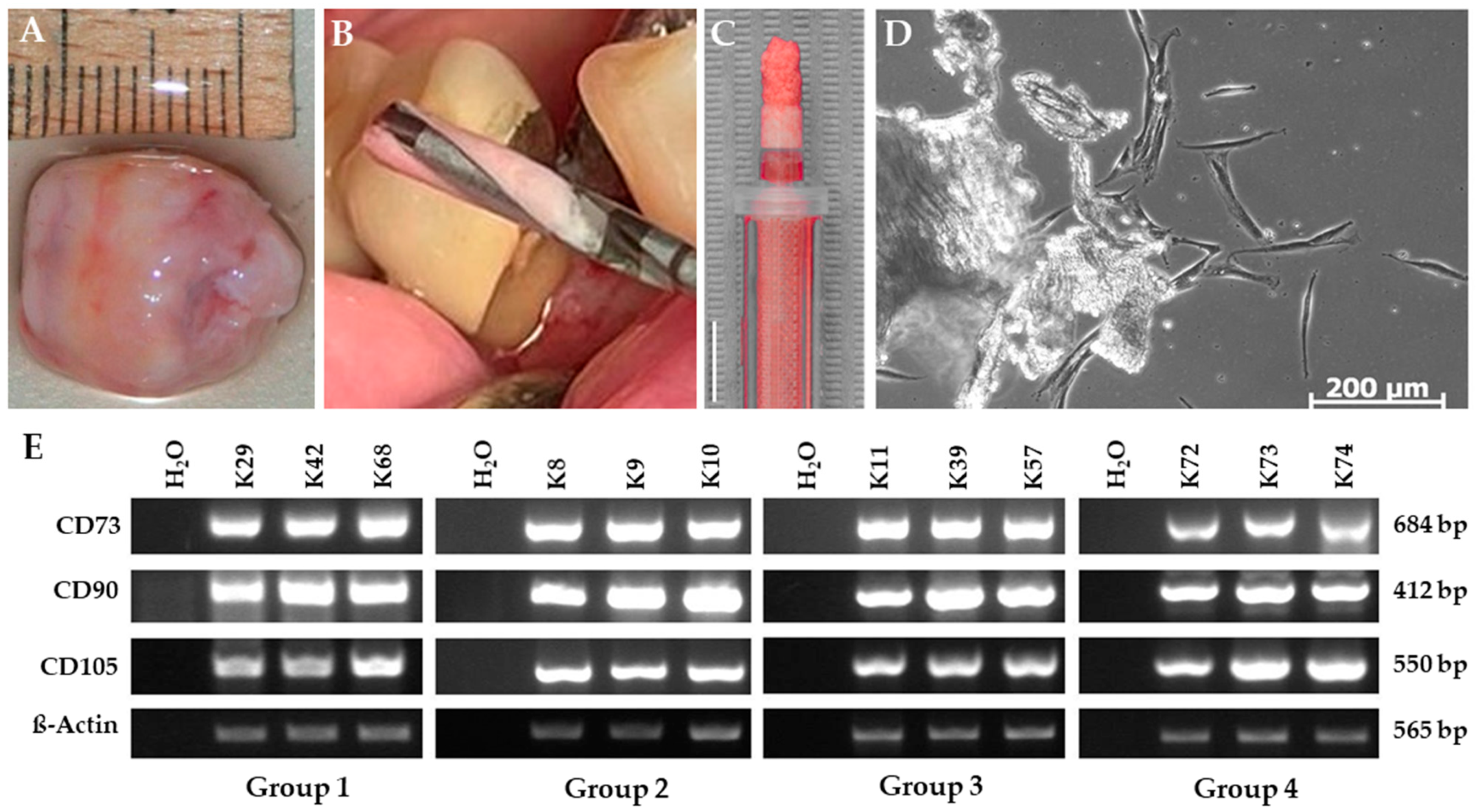
2.4.1. Isolation of Bone Chip-Derived Stem Cells (BDSCs)
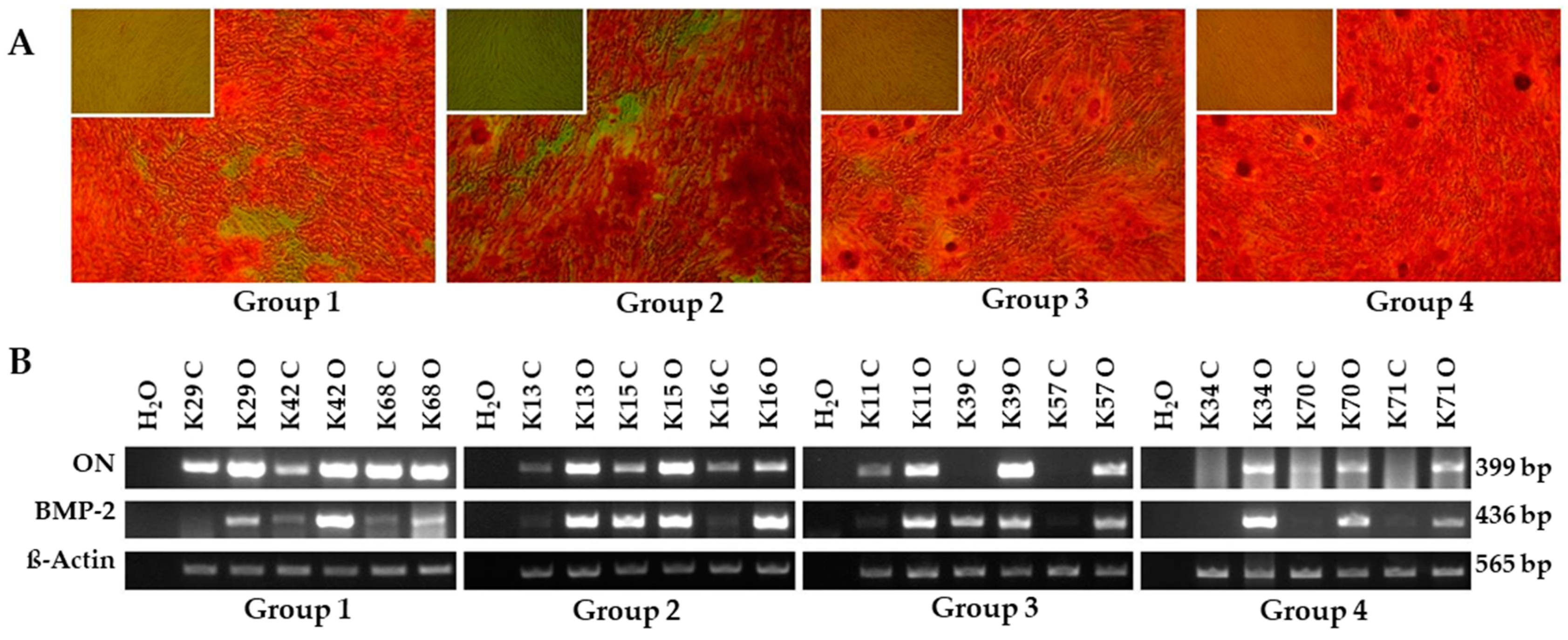
2.4.2. In Vitro Osteogenic Differentiation
2.4.3. Semiquantitative RT-PCR
2.5. Microbiological Analysis
2.6. Statistical Analysis
3. Results
3.1. Outgrowth Statistics
3.2. Characterization of Bone Chip-Derived Stem Cells (BDSCs)
3.2.1. Confirmation of the BDSC Stem Cell Character
3.2.2. In Vitro Osteogenic Differentiation
3.3. Microbiological Analysis
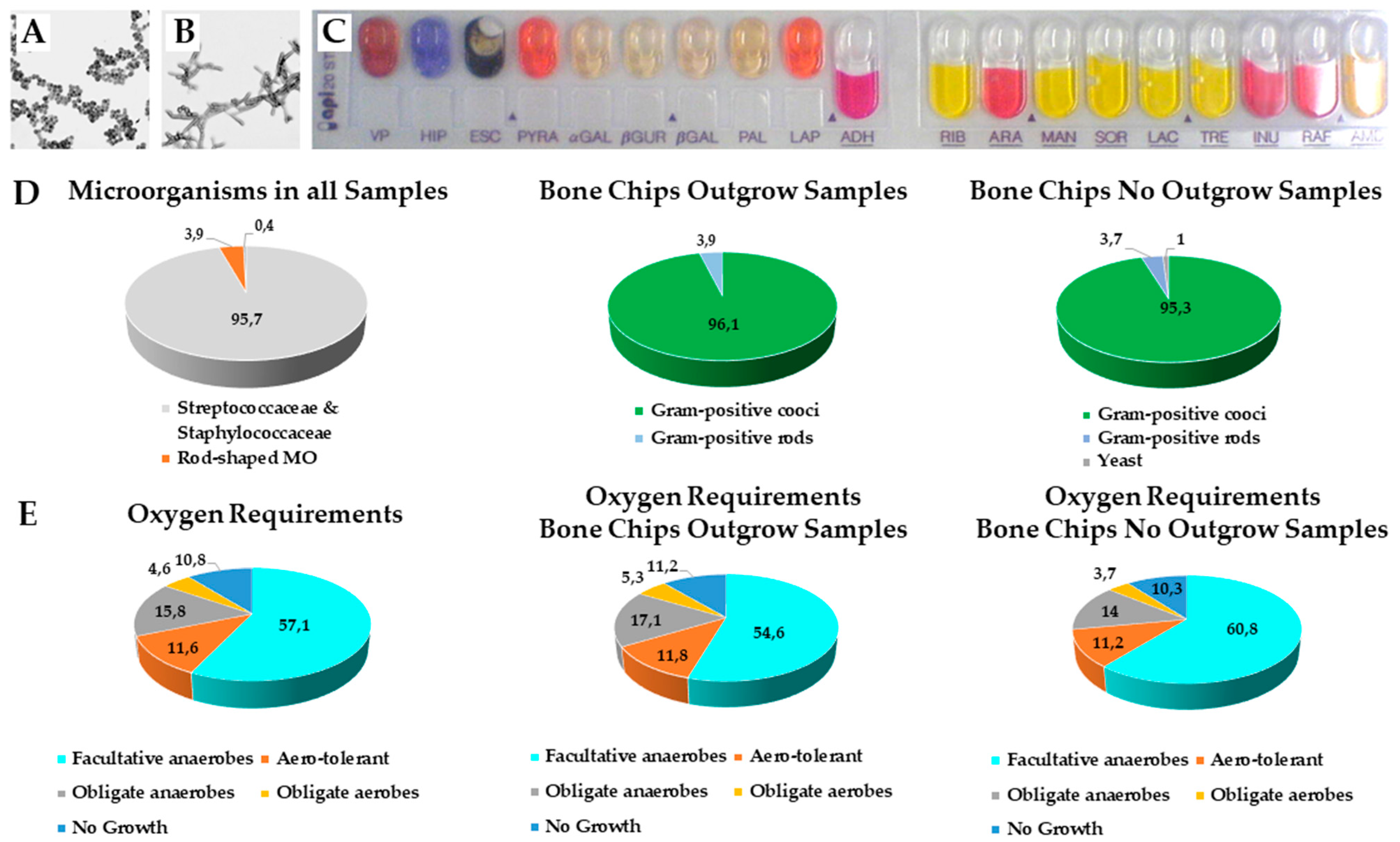
3.3.1. Distribution of Gram Staining Forms and Morphology
3.3.2. Oxygen Requirements of Microorganisms
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Nefussi, J.R. Biology and physiology of the implant bone site. In Bone Augmentation in Oral Implantology; Khoury, F., Antoun, H., Missika, P., Eds.; Quintessence Publishing Co., Ltd.: Hanover Park, IL, USA, 2007; pp. 1–27. [Google Scholar]
- Schlegel, K.A.; Fichtner, G.; Schultze-Mosgau, S.; Wiltfang, J. Histologic findings in sinus augmentation with autogenous bone chips versus a bovine bone substitute. Int. J. Oral Maxillofac. Implant. 2003, 18, 53–58. [Google Scholar]
- Miron, R.J.; Hedbom, E.; Saulacic, N.; Zhang, Y.; Sculean, A.; Bosshardt, D.D.; Buser, D. Osteogenic potential of autogenous bone grafts harvested with four different surgical techniques. J. Dent. Res. 2011, 90, 1428–1433. [Google Scholar] [CrossRef] [PubMed]
- Zippel, N.; Schulze, M.; Tobiasch, E. Biomaterials and mesenchymal stem cells for regenerative medicine. Recent Pat. Biotechnol. 2010, 4, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.; Tobiasch, E. Artificial scaffolds and mesenchymal stem cells for hard tissues. Adv. Biochem. Eng. Biotechnol. 2012, 126, 153–194. [Google Scholar]
- Koole, R.; Bosker, H.; van der Dussen, F.N. Late secondary autogenous bone grafting in cleft patients comparing mandibular (ectomesenchymal) and iliac crest (mesenchymal) grafts. J. Cranio-Maxillo-Facial Surg. 1989, 17, 28–30. [Google Scholar] [CrossRef]
- Sindet-Pedersen, S.; Enemark, H. Reconstruction of alveolar clefts with mandibular or iliac crest bone grafts: A comparative study. J. Oral Maxillofac. Surg. 1990, 48, 554–560. [Google Scholar] [CrossRef]
- Chen, N.T.; Glowacki, J.; Bucky, L.P.; Hong, H.Z.; Kim, W.K.; Yaremchuk, M.J. The roles of revascularization and resorption on endurance of craniofacial onlay bone grafts in the rabbit. Plast. Reconstr. Surg. 1994, 93, 714–722. [Google Scholar] [CrossRef]
- Girdler, N.M.; Hosseini, M. Orbital floor reconstruction with autogenous bone harvested from the mandibular lingual cortex. Br. J. Oral Maxillofac. Surg. 1992, 30, 36–38. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Meijndert, L.; Kalk, W.W.; Vissink, A. Morbidity of mandibular bone harvesting: A comparative study. Int. J. Oral Maxillofac. Implant. 2007, 22, 359–365. [Google Scholar]
- Kainulainen, V.T.; Kainulainen, T.J.; Oikarinen, K.S.; Carmichael, R.P.; Sàndor, G.K.B. Performance of six bone collectors designed for dental implant surgery. Clin. Oral Implant. Res. 2006, 17, 282–287. [Google Scholar] [CrossRef]
- Shoushrah, S.; Transfeld, J.; Tonk, C.; Büchner, D.; Witzleben, S.; Sieber, M.; Schulze, M.; Tobiasch, E. Sinking Our Teeth in Getting Dental Stem Cells to Clinics for Bone Regeneration. Int. J. Mol. Sci. 2021, 22, 6387. [Google Scholar] [CrossRef] [PubMed]
- Smukler, H.; Capri, D.; Landi, L. Harvesting bone in the recipient sites for ridge augmentation. Int. J. Periodont. Restor. Dent. 2008, 28, 411–419. [Google Scholar]
- Di Vito, A.; Giudice, A.; Chiarella, E.; Malara, N.; Bennardo, F.; Fortunato, L. In Vitro Long-Term Expansion and High Osteogenic Potential of Periodontal Ligament Stem Cells: More Than a Mirage. Cell Transpl. 2019, 1, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Yamada, Y.; Nakamura, S.; Ueda, M. Osteogenic potential of effective bone engineering using dental pulp stem cells, bone marrow stem cells, and periosteal cells for osseointegration of dental implants. Int. J. Oral Maxillofac. Implant. 2011, 26, 947–954. [Google Scholar]
- Rezai-Rad, M.; Bova, J.F.; Orooji, M.; Pepping, J.; Qureshi, A.; Del Piero, F.; Hayes, D.; Yao, S. Evaluation of bone regeneration potential of dental follicle stem cells for treatment of craniofacial defects. Cytotherapy 2015, 11, 1572–1581. [Google Scholar] [CrossRef]
- Jin, Q.; Yuan, K.; Lin, W.; Niu, C.; Ma, R.; Huang, Z. Comparative characterization of mesenchymal stem cells from human dental pulp and adipose tissue for bone regeneration potential. Artif. Cells Nanomed. Biotechnol. 2019, 47, 1577–1584. [Google Scholar] [CrossRef]
- Lloyd, B.; Tee, B.C.; Headley, C.; Emam, H.; Mallery, S.; Sun, Z. Similarities and differences between porcine mandibular and limb bone marrow mesenchymal stem cells. Arch. Oral Biol. 2017, 77, 1–11. [Google Scholar] [CrossRef][Green Version]
- Lee, D.J.; Kwon, J.; Current, L.; Yoon, K.; Zalal, R.; Hu, X.; Xue, P.; Ko, C.C. Osteogenic potential of mesenchymal stem cells from rat mandible to regenerate critical sized calvarial defect. J. Tissue Eng. 2019, 10, 2041731419830427. [Google Scholar] [CrossRef]
- Li, C.; Wang, F.; Zhang, R.; Qiao, P.; Liu, H. Comparison of Proliferation and Osteogenic Differentiation Potential of Rat Mandibular and Femoral Bone Marrow Mesenchymal Stem Cells In Vitro. Stem Cells Dev. 2020, 29, 728–736. [Google Scholar] [CrossRef]
- Groeneveldt, L.C.; Herpelinck, T.; Maréchal, M.; Politis, C.; van IJcken, W.F.J.; Huylebroeck, D.; Geris, L.; Mulugeta, E.; Luyten, F.P. The Bone-Forming Properties of Periosteum-Derived Cells Differ Between Harvest Sites. Front. Cell Dev. Biol. 2020, 8, 1–17. [Google Scholar] [CrossRef]
- Hendrijantini, N.; Kusumaningsih, T.; Rostiny, R.; Mulawardhana, P.; Danudiningrat, C.P.; Rantam, F.A. A potential therapy of human umbilical cord mesenchymal stem cells for bone regeneration on osteoporotic mandibular bone. Eur. J. Dent. 2018, 12, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Young, M.P.J.; Korachi, M.; Carter, D.H.; Worthington, H.; Drucker, D.B. Microbial analysis of bone collected during implant surgery: A clinical and laboratory study. Clin. Oral Implant. Res. 2001, 12, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Young, M.P.J.; Korachi, M.; Carter, D.H.; Worthington, H.V.; McCord, J.F.; Drucker, D.B. The effects of an immediately pre-surgical chlorhexidine oral rinse on the bacterial contaminants of bone debris collected during dental implant surgery. Clin. Oral Implant. Res. 2002, 13, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Kuttenberger, J.J.; Hardt, N.; Rutz, T.; Pfyffer, G.E. Mit Knochenkollektor bei dentaler Implantation gewonnenes Knochenmaterial. Mikrobiologische Analyse. Mund-Kiefer-Und Gesichtschirurgie 2005, 9, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Kürkçü, M.; Öz, I.A.; Köksal, F.; Benlidayi, M.E.; Günesli, A. Microbial analysis of the autogenous bone collected by bone filter during oral surgery: A clinical study. J. Oral Maxillofac. Surg. 2005, 63, 1593–1598. [Google Scholar] [CrossRef]
- Sivolella, S.; Berengo, M.; Scarin, M.; Mella, F.; Martinelli, F. Autogenous particulate bone collected with a piezo-electric surgical device and bone trap: A microbiological and histomorphometric study. Arch. Oral Biol. 2006, 51, 883–891. [Google Scholar] [CrossRef]
- Etcheson, A.W.; Miley, D.D.; Gillespie, M.J. Osseous coagulum collected in bone traps: Potential for bacterial contamination and methods for decontamination. J. Oral Implantol. 2007, 33, 109–115. [Google Scholar] [CrossRef]
- Dent, C.D.; Olson, J.W.; Farish, S.E.; Bellome, J.; Casino, A.J.; Morris, H.F.; Ochi, S. The influence of preoperative antibiotics on success of endosseous implants up to and including stage II surgery: A study of 2641 implants. J. Oral Maxillofac. Surg. 1997, 55, 19–24. [Google Scholar] [CrossRef]
- Abu-Ta’a, M.; Quirynen, M.; Teughels, W.; van Steenberghe, D. Asepsis during periodontal surgery involving oral implants and the usefulness of peri-operative antibiotics: A prospective, randomized, controlled clinical trial. J. Clin. Periodontol. 2008, 35, 58–63. [Google Scholar] [CrossRef]
- Al-Nawas, B.; Stein, K. Indication of a preoperative antibiotic prophylaxis for insertion of dental implants—A systematic review. J. Dent. Implantol. 2010, 26, 49–60. [Google Scholar]
- Esposito, M.; Grusovin, M.G.; Loli, V.; Coulthard, P.; Worthington, H.V. Does antibiotic prophylaxis at implant placement decrease early implant failures? A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 101–110. [Google Scholar] [PubMed]
- Eicker, L.A.; Tomakidi, P.; Haessler, D.; Neugebauer, J.; Zöller, J.E. Die Vitalität von gefilterten Knochenspänen zum präimplantologischen Knochenaufbau–Histochemische Untersuchungen und klinische Erfahrungen. Zeitschrift für Zahnärztliche Implantologie 2002, 18, 93–100. [Google Scholar]
- Blay, A.; Tunchel, S.; Sendyk, W.R. Viability of autogenous bone grafts obtained by using bone collectors: Histological and microbiological study. Pesquisa Odontológica Brasileira 2003, 17, 234–240. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gruber, R.; Baron, M.; Busenlechner, D.; Kandler, B.; Fuerst, G.; Watzek, G. Proliferation and osteogenic differentiation of cells from cortical bone cylinders, bone particles from mill, and drilling dust. J. Oral Maxillofac. Surg. 2005, 63, 238–243. [Google Scholar] [CrossRef]
- Chiriac, G.; Herten, M.; Schwarz, F.; Rothamel, D.; Becker, J. Autogenous bone chips: Influence of a new piezoelectric device (Piezosurgery®) on chip morphology, cell viability and differentiation. J. Clin. Periodontol. 2005, 32, 994–999. [Google Scholar] [CrossRef]
- Zhang, Y.; Khan, D.; Delling, J.; Tobiasch, E. Mechanisms underlying the osteo- and adipo-differentiation of human mesenchymal stem cells. Sci. World J. 2012, 2012, 793823. [Google Scholar] [CrossRef]
- Graziani, F.; Cei, S.; Ivanovski, S.; La Ferla, F.; Gabriele, M.A. systematic review of the effectiveness of bone collectors. Int. J. Oral Maxillofac. Implant. 2007, 22, 729–735. [Google Scholar]
- Haessler, D.; Zöller, J.; Vizethum, F. Autogene Knochentransplantation mit Hilfe eines Spankollektors–Eine Methodenbeschreibung. Implantologie 1995, 4, 315–322. [Google Scholar]
- Rasmusson, L. Knochenaufbau bei lokalen Alveolarkammdefekten. Dent. Implantol. Parodontol. 2002, 6, 24–26. [Google Scholar]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Haddouti, E.M.; Skroch, M.; Zippel, N.; Müller, C.; Birova, B.; Pansky, A.; Kleinfeld, C.; Winter, M.; Tobiasch, E. Human dental follicle precursor cells of wisdom teeth: Isolation and differentiation towards osteoblasts for implants with and without scaffolds. Mater. Sci. Eng. Technol. 2009, 40, 732–737. [Google Scholar] [CrossRef]
- Khan, D.; Kleinfeld, C.; Winter, M.; Tobiasch, E. Oral tissues as source for bone regeneration in dental implantology. In Tissue Regeneration-From Basic Biology to Clinical Application; Davies, J., Ed.; IntechOpen: London, UK, 2012; pp. 325–338. [Google Scholar]
- Zippel, N.; Limbach, C.A.; Ratajski, N.; Urban, C.; Luparello, C.; Pansky, A.; Kassack, M.U.; Tobiasch, E. Purinergic receptors influence the differentiation of human mesenchymal stem cells. Stem Cells Dev. 2012, 21, 884–900. [Google Scholar] [CrossRef] [PubMed]
- Tobiasch, E. Differentiation potential of adult human mesenchymal stem cells. In Stem Cell Engineering; Artmann, G.M., Hescheler, J., Minger, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Springer, I.N.G.; Terheyden, H.; Geiß, S.; Härle, F.; Hedderich, J.; Açil, Y. Particulated bone grafts-effectiveness of bone cell supply. Clin. Oral Implant. Res. 2004, 15, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Longo, A.; Librizzi, M.; Naselli, F.; Caradonna, F.; Tobiasch, E.; Luparello, C. PTHrP in differentiating human mesenchymal stem cells: Transcript isoform expression, promoter methylation, and protein accumulation. Biochimie 2013, 95, 1888–1896. [Google Scholar] [CrossRef]
- Chung, S.M.; Kim, E.-B.; Park, S.-Y.; Sung, M.C.; Youn, H.K.; Ahn, M.-W. Effect of bone marrow cell collection techniques and donor site locations on in-vitro growth of bone forming cells. Asian Spine J. 2008, 2, 59–63. [Google Scholar] [CrossRef]
- Kotte, B.M. Optimierung der Wachstumsbedingungen Humaner Osteoblasten In Vitro. Ph.D. Thesis, Medizinische Fakultät der Universität Leipzig, Leipzig, Germany, 2005. [Google Scholar]
- Evaldson, G.; Heimdahl, A.; Kager, L.; Nord, C.E. The normal human anaerobic microflora. Scand. J. Infect. Dis. Suppl. 1982, 35, 9–15. [Google Scholar]
- Duewelhenke, N.; Krut, O.; Eysel, P. Influence on mitochondria and cytotoxicity of different antibiotics administered in high concentrations on primary human osteoblasts and cell lines. Antimicrob. Agents Chemother. 2007, 51, 54–63. [Google Scholar] [CrossRef]
- Lambrecht, J.T.; Glaser, B.; Meyer, J. Bacterial contamination of filtered intraoral bone chips. Int. J. Oral Maxillofac. Surg. 2006, 35, 996–1000. [Google Scholar] [CrossRef]
- Tezulas, E.; Dilek, O.C. Decontamination of autogenous bone grafts collected from dental implant sites via osteotomy: A review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 679–684. [Google Scholar] [CrossRef]
- Takamoto, M.; Takechi, M.; Ohta, K.; Ninomiya, Y.; Ono, S.; Shigeishi, H.; Tada, M.; Kamata, N. Risk of bacterial contamination of bone harvesting devices used for autogenous bone graft in implant surgery. Head Face Med. 2013, 9, 3. [Google Scholar] [CrossRef]
- Petri, W.H., 3rd; Schaberg, S.J. The effects of antibiotic-supplemented bone allografts on contaminated, partially avulsive fractures of the canine ulna. J. Oral Maxillofac. Surg. 1984, 42, 699–704. [Google Scholar] [CrossRef]
- Petri, W.H., 3rd; Wilson, T.M. Clinical evaluation of antibiotic-supplemented bone allograft. J. Oral Maxillofac. Surg. 1993, 51, 982–985. [Google Scholar] [CrossRef]
- Isefuku, S.; Joyner, C.J.; Simpson, A.H. Toxic effect of rifampicin on human osteoblast-like cells. J. Orthop. Res. 2001, 19, 950–954. [Google Scholar] [CrossRef]
- Isefuku, S.; Joyner, C.J.; Simpson, A.H. Gentamycin may have an adverse effect on osteogenesis. J. Orthop. Trauma 2003, 17, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Lupșe, I.; Pall, E.; Tudoran, L.B.; Bulboacă, A.E.; Ciurea, A.; Micu, I.C.; Roman, A.; Delean, A.G.; Muntean, A.; Soancă, A. Cytotoxic Effects on Gingival Mesenchymal Stromal Cells and Root Surface Modifications Induced by Some Local Antimicrobial Products Used in Periodontitis Treatment. Materials 2021, 14, 5049. [Google Scholar] [CrossRef] [PubMed]
- Riecke, B.; Heiland, M.; Hothan, A.; Morlock, M.; Amling, M.; Blake, F.A. Primary implant stability after maxillary sinus augmentation with autogenous mesenchymal stem cells: A biomechanical evaluation in rabbits. Clin. Oral Implant. Res. 2011, 11, 1242–1246. [Google Scholar] [CrossRef]
- Lima, R.G.; Lima, T.G.; Francischone, C.E.; Turssi, C.; Souza Picorelli Assis, N.M.; Sotto-Maior, B.S. Bone Volume Dynamics and Implant Placement Torque in Horizontal Bone Defects Reconstructed with Autologous or Xenogeneic Block Bone: A Randomized, Controlled, Split-Mouth, Prospective Clinical Trial. Int. J. Oral Maxillofac. Implant. 2018, 33, 888–894. [Google Scholar] [CrossRef]
- Giudice, A.; Bennardo, F.; Antonelli, A.; Barone, S.; Wagner, F.; Fortunato, L.; Traxler, H. Influence of clinician’s skill on primary implant stability with conventional and piezoelectric preparation techniques: An ex-vivo study. J. Biol. Regul. Homeost. Agents 2020, 2, 739–745. [Google Scholar]
- Ding, S.J.; Chu, Y.H.; Chen, P.T. Mechanical Biocompatibility, Osteogenic Activity, and Antibacterial Efficacy of Calcium Silicate-Zirconia Biocomposites. ACS Omega 2021, 10, 7106–7118. [Google Scholar] [CrossRef]
- Lu, X.; Chen, Y.; Mao, P.; Chen, L.; Han, X.; Sun, F. Nanoparticle Shaped Titanium Promotes Osteogenic Differentiation of Bone Mesenchymal Stem Cells Through Integrin/Integrin Linked Kinase/Glycogen Synthase Kinase-3β Axis. J. Biomed. Nanotechnol. 2020, 8, 1267–1275. [Google Scholar] [CrossRef]
| Patient Group | Number of Samples | Mean Age | Female | Male |
|---|---|---|---|---|
| Cortical w/antibiotic pretreatment | 15 | 22.2 ± 13.3 | 7 | 8 |
| Cortical w/o antibiotic pretreatment | 30 | 19.4 ± 5.5 | 20 | 10 |
| Cortical-cancellous w/antibiotic pretreatment | 20 | 61.7 ± 11.8 | 12 | 8 |
| Cortical-cancellous w/o antibiotic pretreatment | 19 | 60.3 ± 15.1 | 10 | 9 |
| Total | 84 | 39.2 ± 23.2 | 49 | 35 |
| Patient Group | Number of Samples | Outgrown Samples | Outgrowth Time [days] | SEM | Outgrowth Probability [%] |
|---|---|---|---|---|---|
| Cortical w/antibiotic pretreatment | 15 | 13 | 12.85 ± 3.24 | 0.90 | 86.67 |
| Cortical w/o antibiotic pre-treatment | 30 | 21 | 15.81 ± 5.32 | 1.16 | 70.00 |
| Cortical-cancellous w/antibiotic pretreatment | 20 | 17 | 13.47 ± 5.25 | 1.27 | 85.00 |
| Cortical-cancellous w/o antibiotic pretreatment | 19 | 14 | 7.00 ± 2.18 * | 0.58 | 73.68 |
| Patient Group | Number of Samples | Outgrown Samples | Outgrowth Probability [%] |
|---|---|---|---|
| Cortical w/& w/o antibiotic pretreatment | 45 | 34 | 75.56 |
| Cortical-cancellous w/& w/o antibiotic pretreatment | 39 | 31 | 79.49 |
| Cortical and cortical-cancellous w/antibiotic pretreatment | 35 | 30 | 85.71 * |
| Cortical and cortical-cancellous w/o antibiotic pretreatment | 49 | 35 | 71.43 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babczyk, P.; Winter, M.; Kleinfeld, C.; Pansky, A.; Oligschleger, C.; Tobiasch, E. Examination of the Quality of Particulate and Filtered Mandibular Bone Chips for Oral Implants: An In Vitro Study. Appl. Sci. 2022, 12, 2031. https://doi.org/10.3390/app12042031
Babczyk P, Winter M, Kleinfeld C, Pansky A, Oligschleger C, Tobiasch E. Examination of the Quality of Particulate and Filtered Mandibular Bone Chips for Oral Implants: An In Vitro Study. Applied Sciences. 2022; 12(4):2031. https://doi.org/10.3390/app12042031
Chicago/Turabian StyleBabczyk, Patrick, Martin Winter, Claudia Kleinfeld, Andreas Pansky, Christina Oligschleger, and Edda Tobiasch. 2022. "Examination of the Quality of Particulate and Filtered Mandibular Bone Chips for Oral Implants: An In Vitro Study" Applied Sciences 12, no. 4: 2031. https://doi.org/10.3390/app12042031
APA StyleBabczyk, P., Winter, M., Kleinfeld, C., Pansky, A., Oligschleger, C., & Tobiasch, E. (2022). Examination of the Quality of Particulate and Filtered Mandibular Bone Chips for Oral Implants: An In Vitro Study. Applied Sciences, 12(4), 2031. https://doi.org/10.3390/app12042031





