Toward a Symbolic AI Approach to the WHO/ACSM Physical Activity & Sedentary Behavior Guidelines
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Reference Use Cases and Motivating Application Scenarios
2.1.1. Lifestyle-Related Early Detection and Interventions
2.1.2. Health Reasoning and Explainable AI (XAI): Establishing a Shared and Validated Interpretation
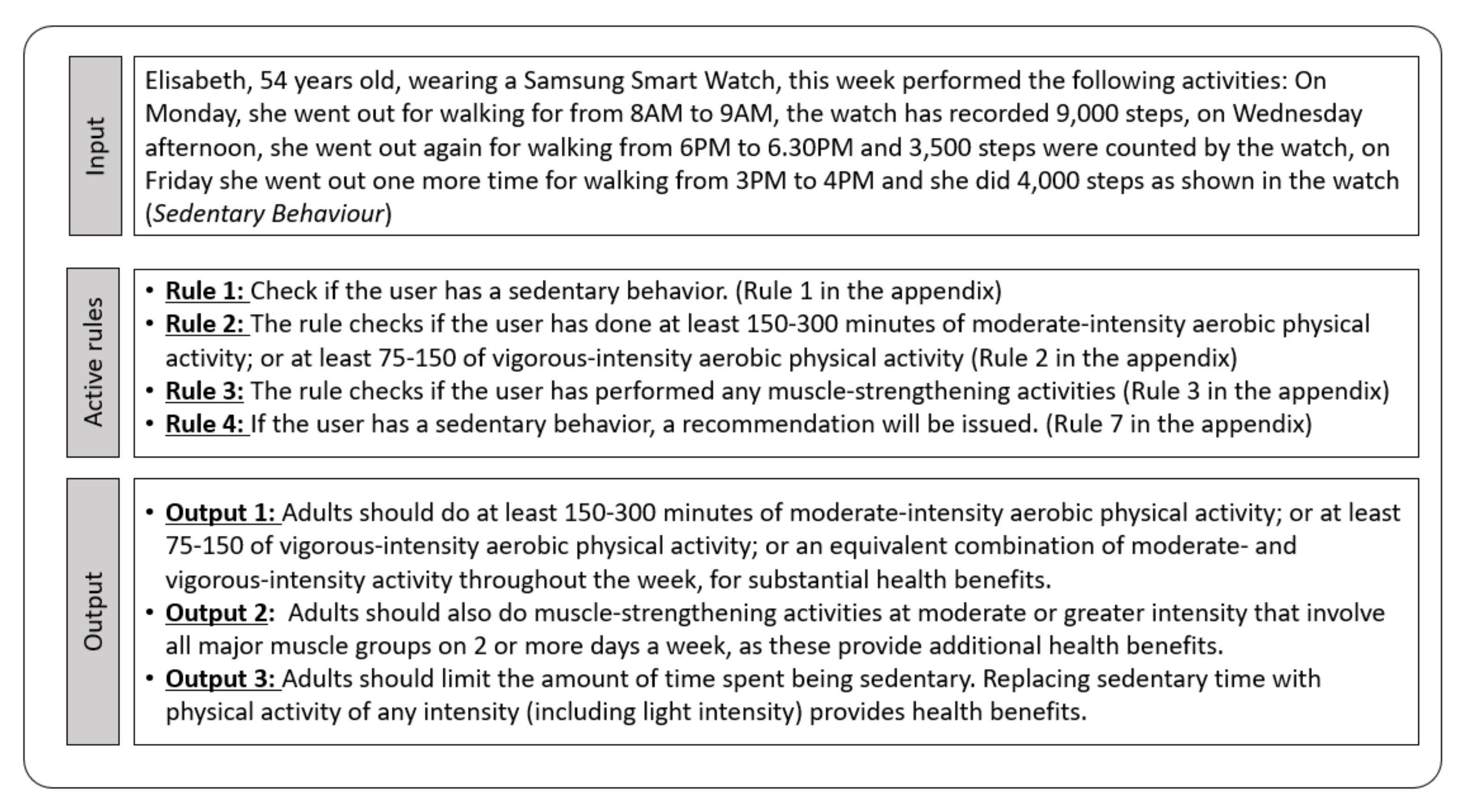
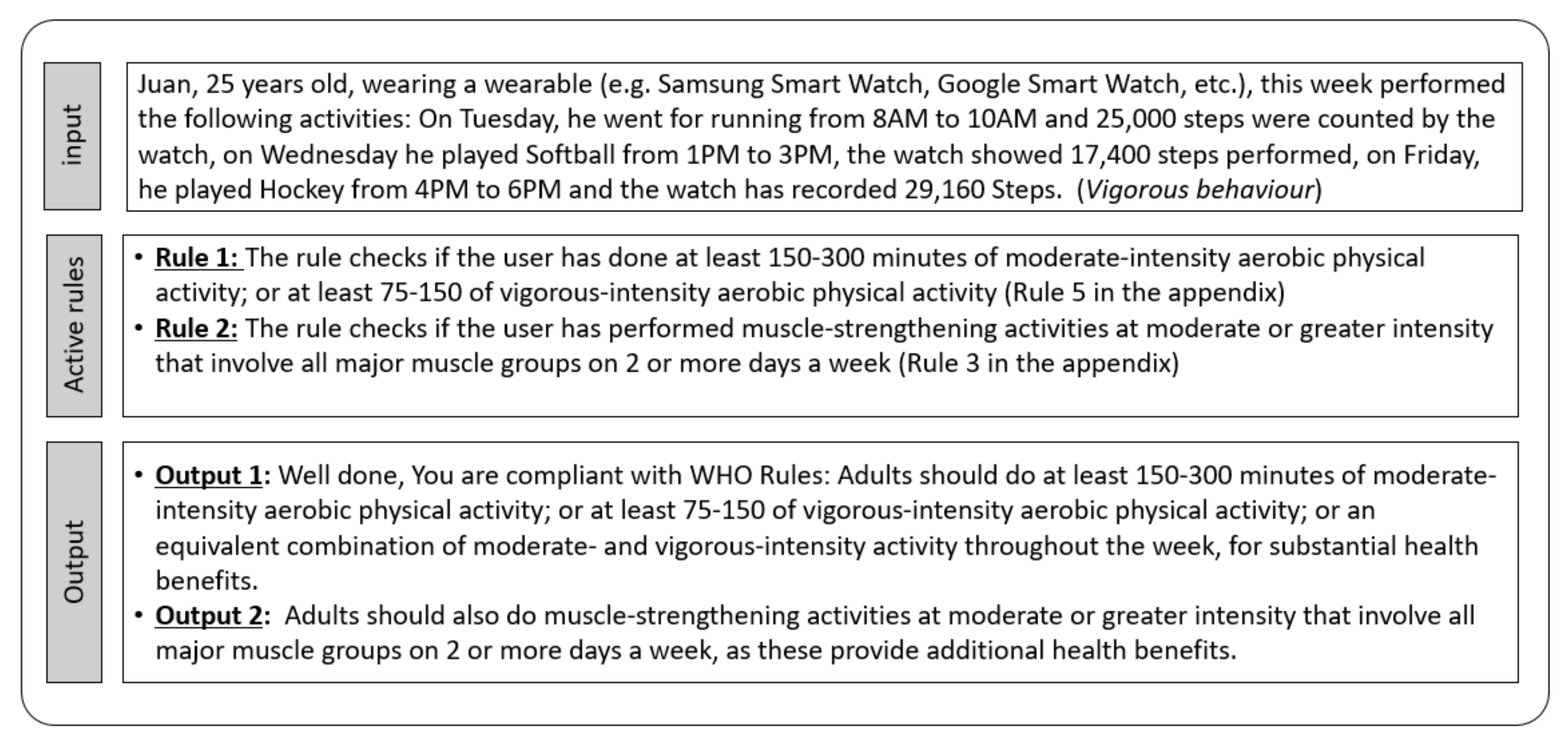
- [Not compliant:] Juan, 25 years old, wearing a smart watch, has performed this week the following activities: On Wednesday, he did yoga from 8 a.m. to 8:45 a.m., which is equivalent to 2025 steps and on Friday, he went for a run from 7 a.m. to 8 a.m., in total, 6000 steps were recorded by the watch.
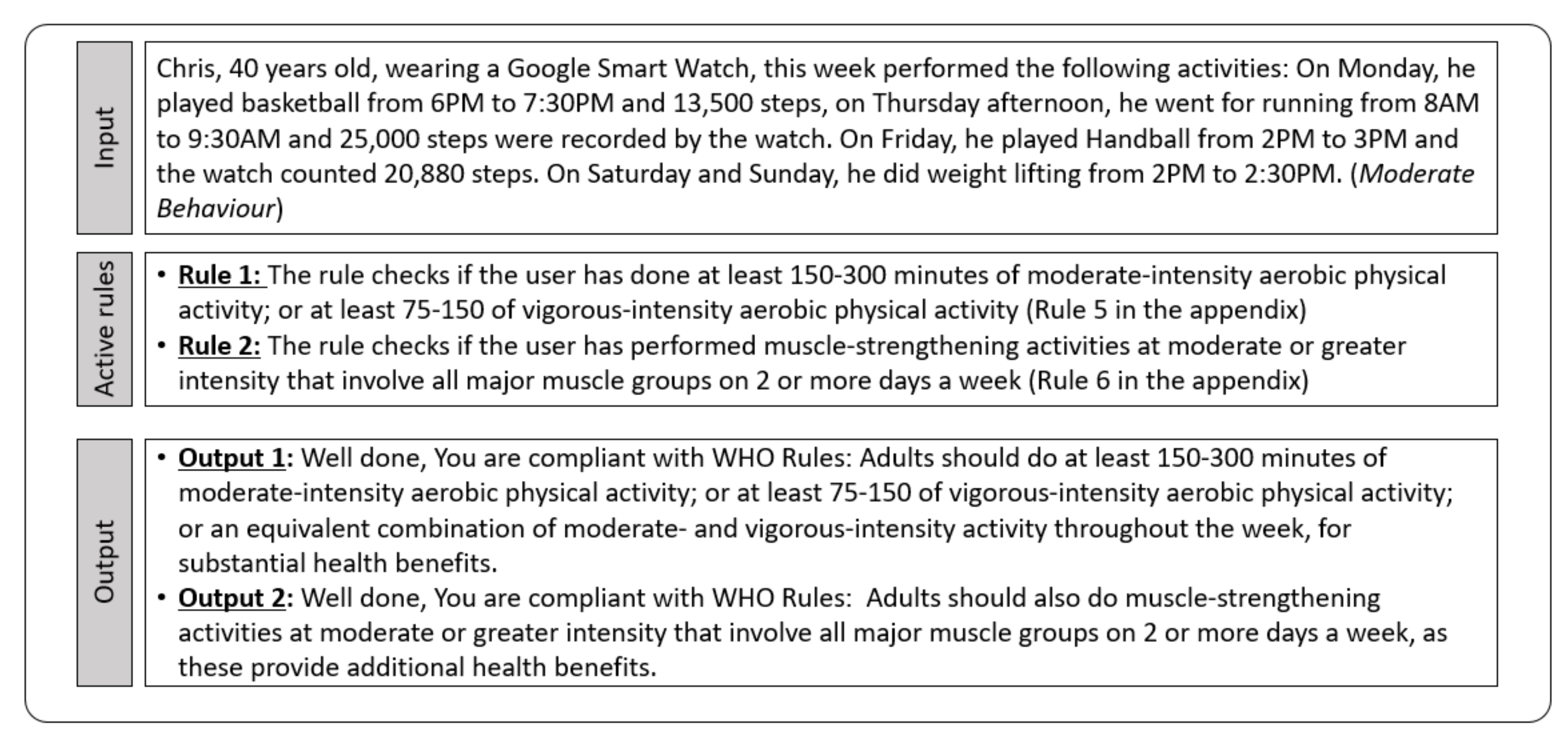
- [Compliant:] Sara, 35 years old, wearing a Google smart watch, this week performed the following activities: On Monday, she played basketball from 6 p.m. to 7:30 p.m. and 13,500 steps were recorded by the watch; on Thursday afternoon, she went running from 8 a.m. to 9:30 a.m. and she did 25,000 steps, as counted by the watch. On Friday, she played handball from 2 p.m. to 3 p.m., with the watch shoowing 20,880 steps recorded. On Saturday and Sunday, she did weight lifting from 2 p.m. to 2:30 p.m.
2.1.3. Digital Coaching in the Health Care Domain
2.2. Computer-Interpretable Guidelines
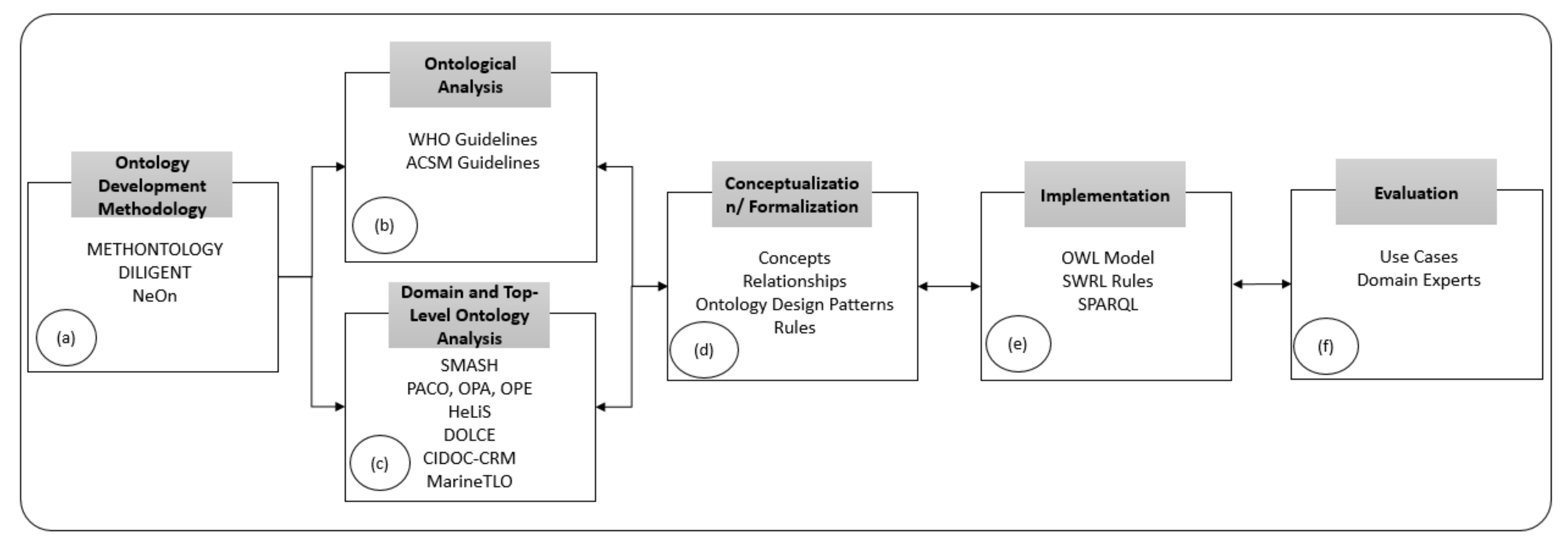
2.3. Symbolic AI Approach: From Analysis to Design
- (a)
- (b)
- An ontological analysis of the main concepts and relationships that are involved in the domain of Physical Activity & Sedentary Behavior Guidelines [3].
- (c)
- An analysis of existing domain ontologies, including PACO [24], HELIOS [25], and OPA [41], to reuse as much as possible existing concepts and relationships. At the same time, we also analyzed top-level ontologies, such as DOLCE [42], CIDOC-CRM [43], and SUMO [44], to maximize interoperability and facilitate a design approach based on ontology patterns.
- (d)
- The design of an appropriate domain ontology—concepts and properties—to model what WHO/ACSM requires in relation of physical activity and the formulation of the recommendations as IF-THEN rules.
- (e)
- The implementation of an ontology (HeLiFit) using OWL—Ontology Web Language—and of the set of rules (HeLiFit-Rule) using RDFox Rule Language.
- (f)
- A validation process centred on checking the logical consistency of the ontology and evaluating it in terms of appropriateness and usefulness, as determined by domain experts.
2.3.1. Ontology Development Methodology
2.3.2. Ontological Analysis
- 1.
- Physical activity—a range of waking behaviors that share the common feature of increasing energy expenditure that is determined, for a given activity, by the intensity, duration, and frequency of muscular movement.
- 2.
- Physical inactivity—the failure to achieve the minimum activity recommendations for health.
- 3.
- Sedentary behavior—sedentary behavior refers to any waking behavior characterized by an energy expenditure less or equal to 1.5 METs while in a sitting, reclining, or lying posture.
- 4.
- Exercise—a form of physical activity that is planned, structured, and repetitive with the aim of improving or maintaining fitness.
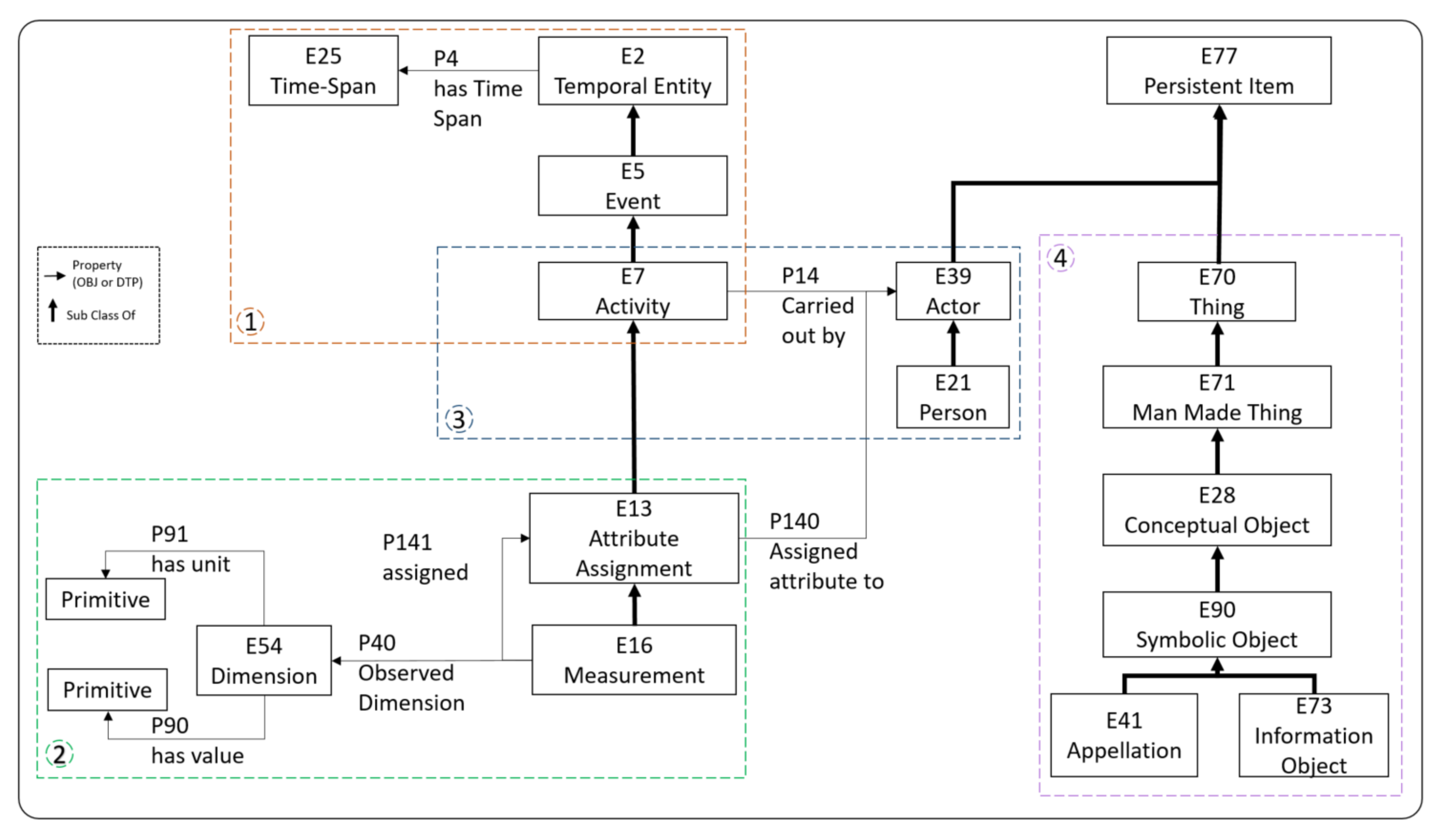
2.3.3. Domain and Top-Level Ontology Analysis
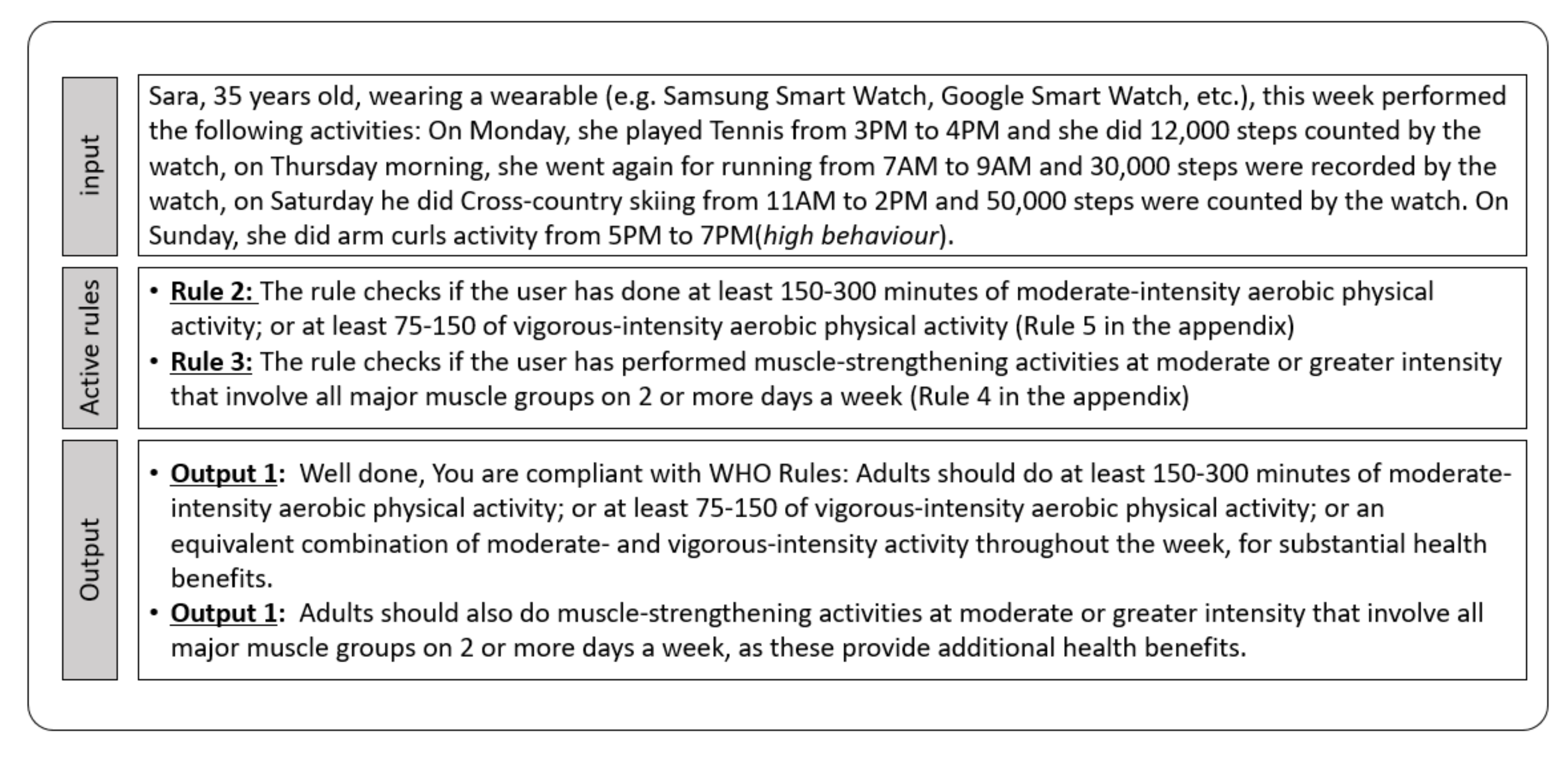
2.3.4. Conceptualization and Formalization
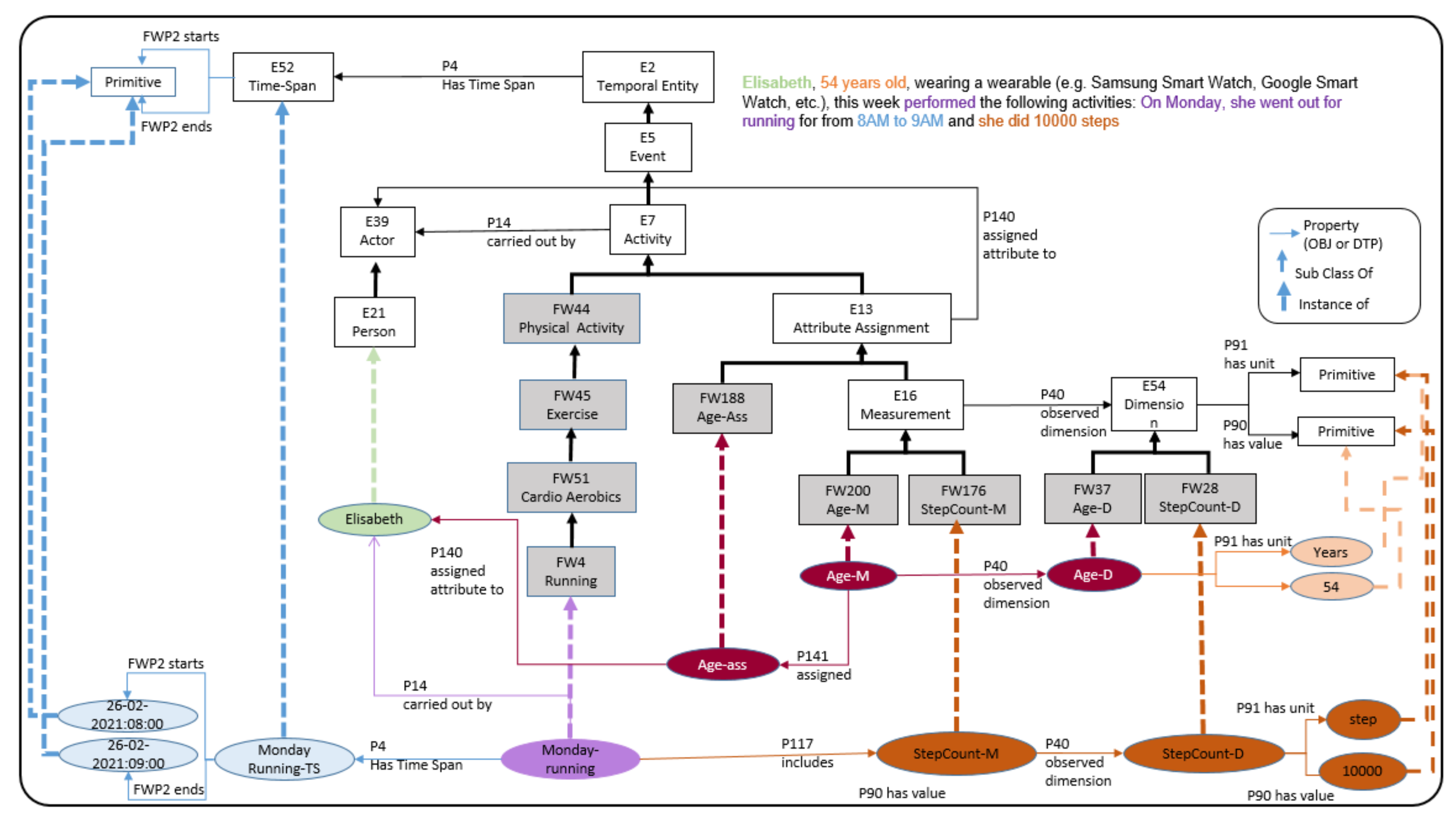
- Rule to convert a physical activity into steps: In order to make physical activities comparable, and hence apply aggregation operations when more that one physical activity is performed over a specific time window, we convert them into steps using the duration and an activity-specific conversion factor, as shown in Equation (1).D specifies the duration in minutes of the physical activity performed while is a coefficient that depends on the physical activity. For example, 30 min of baseball, which has a coefficient of 150, is equivalent to steps. This conversion is formulated in Figure 7.
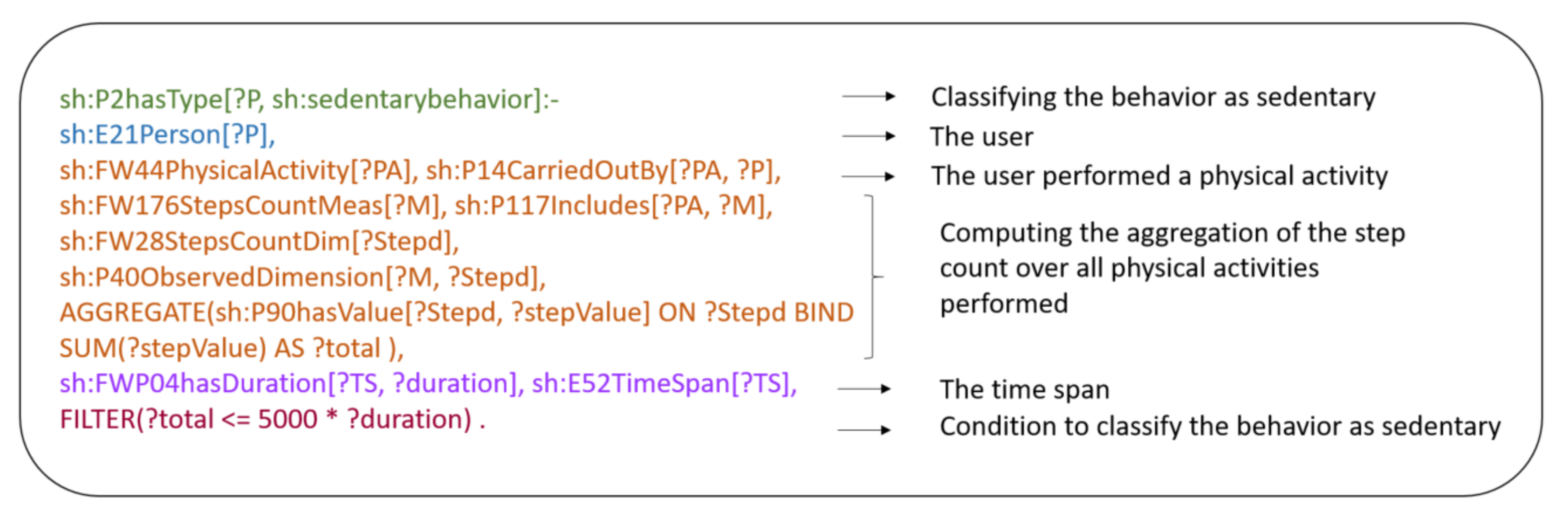
- Rule to compute the intensity of a physical activity: The intensity of a physical activity is related to how hard our body works while doing a specific physical activity [51]. There are four levels of the physical activity intensity: High, Vigorous, Moderate, and Sedentary and they are measured and estimated by one of the variables: Heart rate reserve (), rate reserve max (), metabolic equivalents (), maximal oxygen consumption (), and steps count. In Table 3, we present the different rules to estimate the physical activity intensity.The WHO and ACSM guidelines are structured for four main categories of users: (i) children and adolescents (aged 5–17 yeas old); (ii) adults (aged 18–64); (iii) older adults (aged 64 years and older), and (iv) pregnant women. HeLiFit-Rule implements 137 rules to cover all the above users. In the paper, we describe a few of them and leave the rest in the Appendix A. Figure 8 below models the case of a physical activity with low intensity that is classified as Sedentary.
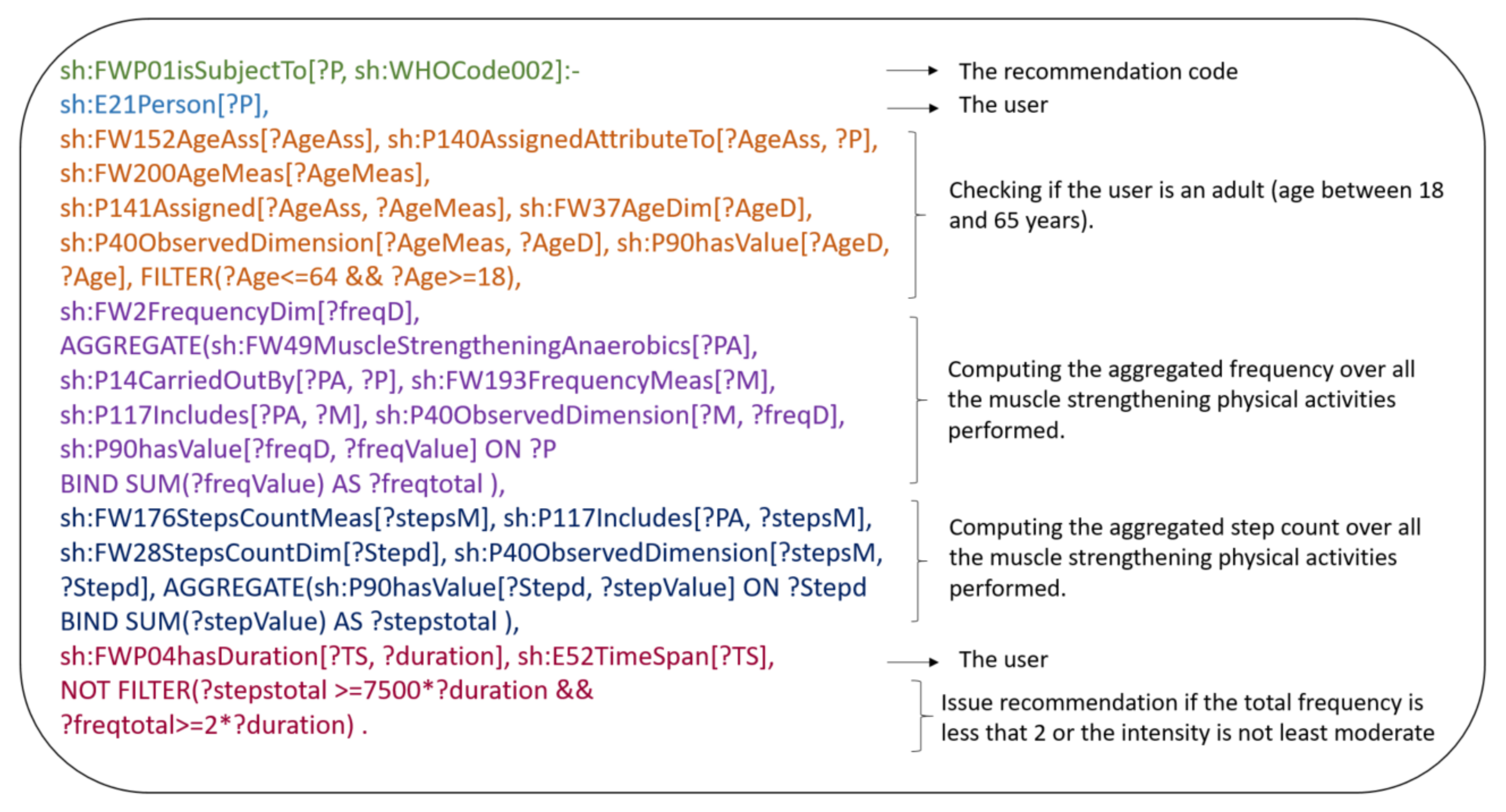
- Rule to issue WHO/ACSM recommendations: Rules are triggered according to the user’s age, the frequency, the modality, the duration (typically a week), and the intensity of the physical activity. While frequency, modality, and duration are given explicitly, intensity needs to be calculated. Once we have computed the intensity of all the physical activities that a user has performed over a specific time window, using the above rule, we aggregate them and, based on the results, one or more recommendations are triggered. As an example, we show the rule that codifies the following WHO guideline:WHO Recommendation: Adults(18–64 years) should also do muscle-strengthening activities at moderate or greater intensity that involve all major muscle groups on 2 or more days a week, as these provide additional health benefits.The user, assumed to be between 18 and 65 years, will get this recommendation in two cases:Case 1: she/he performed any muscle-strengthening physical activity but the intensity of the physical activity is lower than moderate or the frequency is less than two. This case is covered in Figure 9 below:Case 2: she/he did not do any muscle-strengthening physical activity. This case is covered in Figure 10:
3. Results
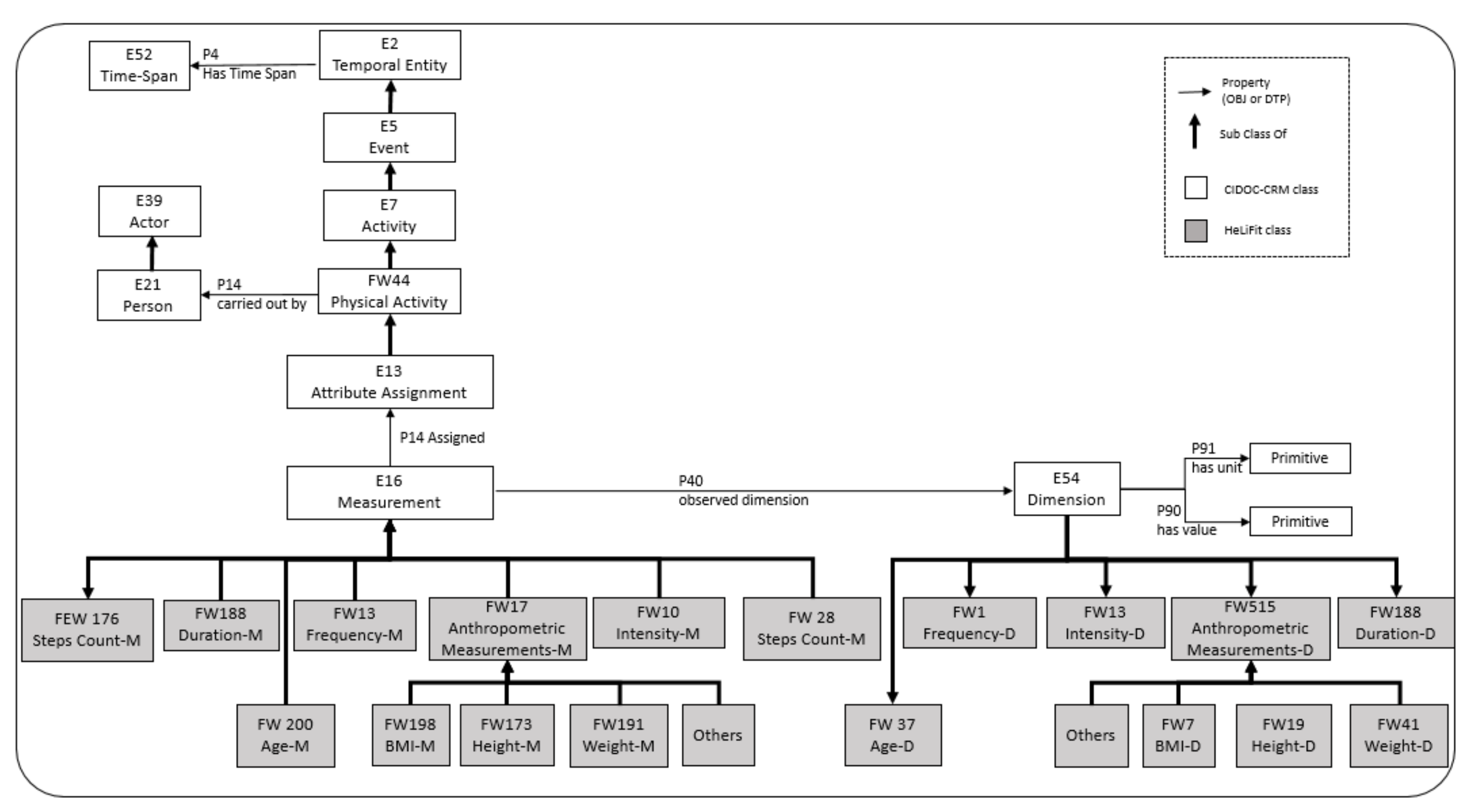
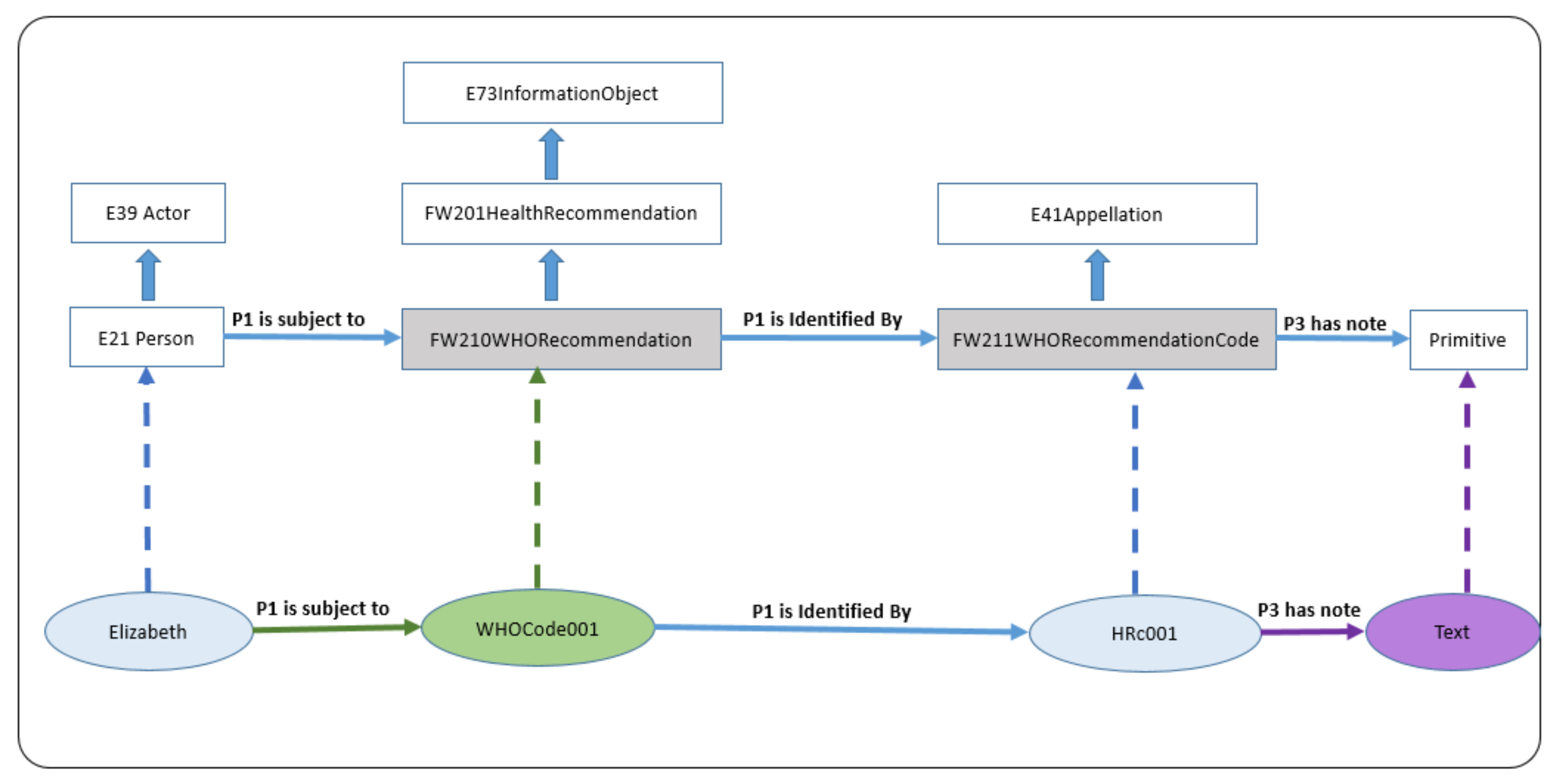
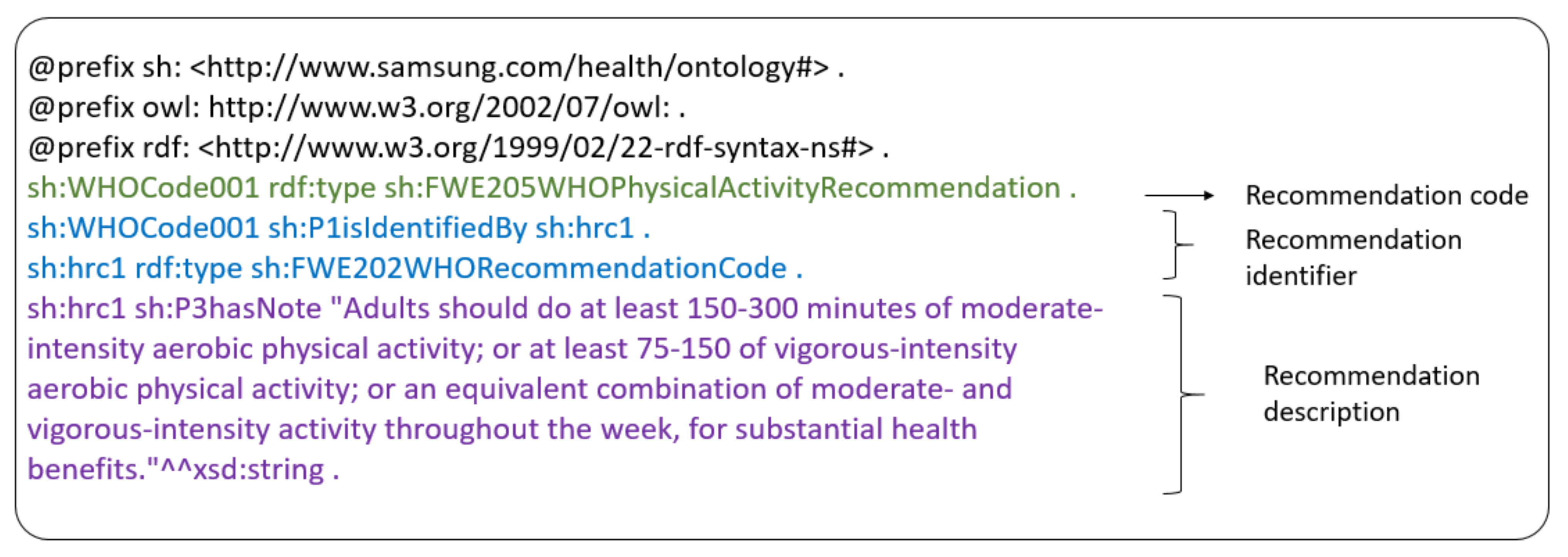
3.1. Description of HeLiFit Ontology
3.2. Evaluation of HeLiFit and HeLiFit-Rule
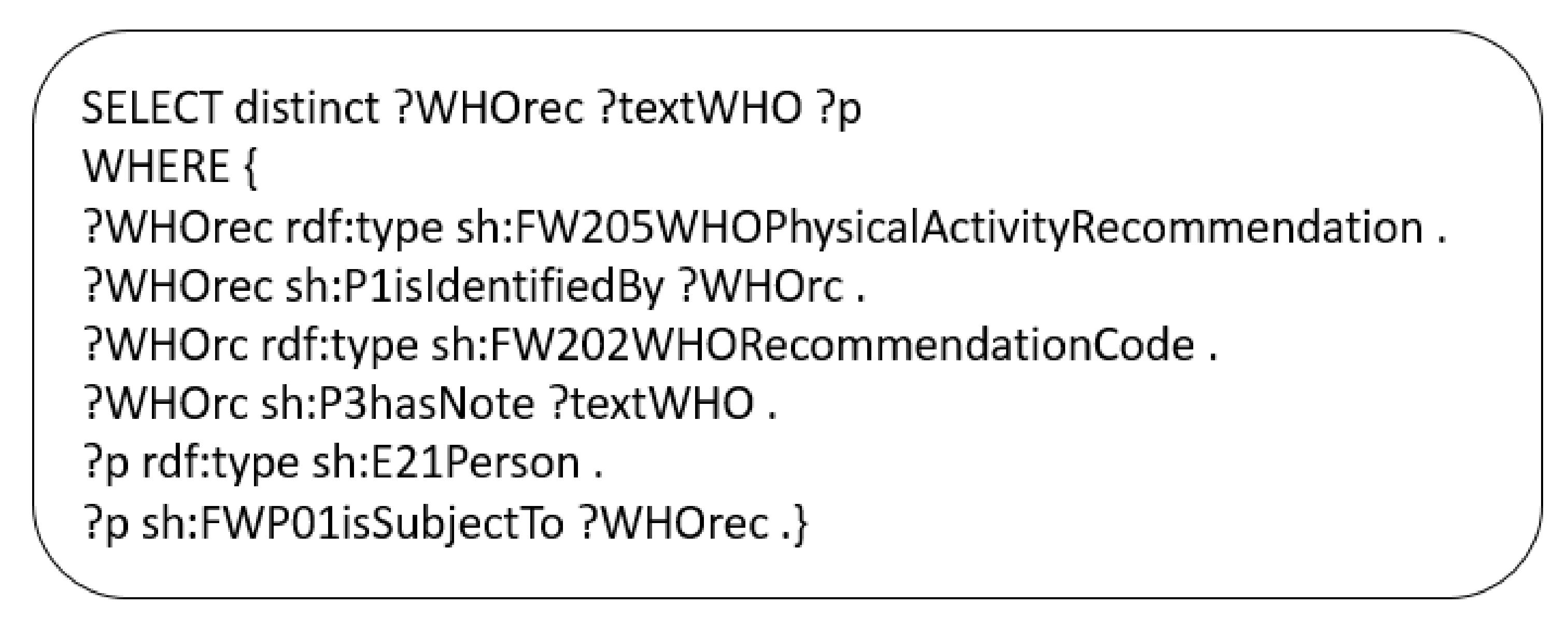
3.3. Health Knowledge Graph with HeLiFit and Reasoning with Rules
4. Concluding Discussion and Future Work
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WHO | World Health Organization |
| ACSM | The American College of Sports Medicine |
| OWL | Web Ontology Language |
| KR&R | Knowledge representation and reasoning |
| HeLiFit | Health Lifestyle Fitness Ontology |
| HeLiFit-Rule | Set of rules based on Health Lifestyle Fitness Ontology |
| SWRL | Semantic Web Rule Language |
| RDFox | A scalable in-memory RDF triple store and semantic reasoning engine |
| FHIR | Fast Healthcare Interoperability Resources |
Appendix A. Set of Rules Used in This Paper
- Rule 1: Checking if the user has a sedentary behavior based on the step count.sh:P2hasType[?P,sh:sedentarybehavior]:-sh:E21Person[?P],sh:FW44PhysicalActivity[?PA],sh:P14CarriedOutBy[?PA,?P],sh:FW176StepsCountMeas[?M],sh:P117Includes[?PA,?M],sh:FW28StepsCountDim[?Stepd], sh:P40ObservedDimension[?M,?Stepd],AGGREGATE(sh:P90hasValue[?Stepd,?stepValue]ON ?Stepd BIND SUM(?stepValue) AS ?total) FILTER(?total<=5000) .
- Rule 2: Checking if the user has done at least 150–300 min of moderate-intensity aerobic physical activity; or at least 75–150 of vigorous-intensity aerobic physical activity, if not, a recommendation will be issued.sh:FWP01isSubjectTo[?P,sh:WHOCode001]:-sh:E21Person[?P],sh:FW152AgeAss[?AgeAss], h:P140AssignedAttributeTo[?AgeAss,?P],sh:FW200AgeMeas[?AgeMeas],sh:P141Assigned[?AgeAss,?AgeMeas],sh:FW37AgeDim[?AgeD],sh:P40ObservedDimension[?AgeMeas,?AgeD],sh:P90hasValue[?AgeD,?Age],FILTER(?Age<=64&&?Age>=18),sh:FW4DurationDim[?durd],AGGREGATE(sh:FW51CardioAerobics[?PA],sh:P14CarriedOutBy[?PA,?P],sh:FW188DurationMeas[?M],sh:P117Includes[?PA,?M],sh:P40ObservedDimension[?M,?durd],sh:P90hasValue[?durd,?durValue] ON ?P BIND SUM(?durValue)AS ?durtotal),sh:FW176StepsCountMeas[?stepsM],sh:P117Includes[?PA,?stepsM],sh:FW28StepsCountDim[?Stepd],sh:P40ObservedDimension[?stepsM,?Stepd],AGGREGATE(sh:P90hasValue[?Stepd,?stepValue] ON ?Stepd BINDSUM(?stepValue) AS ?stepstotal ),sh:FW40TimeWindowDim[?TW],sh:P90hasValue[?TW,?TWvalue],NOT FILTER(?stepstotal >=7500*?TWvalue && ?stepstotal <10000*?TWvalue &&?durtotal>150*?TWvalue && ?durtotal<=300*?TWvalue),NOTFILTER(?stepstotal>10000*?TWvalue&&?durtotal>75*?TWvalue&&?durtotal<=150*?TWvalue).
- Rule 3: Checking if the user has performed any muscle-strengthening activities, if not, a recommendation will be issued.sh:FWP01isSubjectTo[?P,sh:WHOCode002]:-sh:E21Person[?P],sh:FW152AgeAss[?AgeAss],sh:P140AssignedAttributeTo[?AgeAss,?P],sh:FW200AgeMeas[?AgeMeas],sh:P141Assigned[?AgeAss,?AgeMeas],sh:FW37AgeDim[?AgeD],sh:P40ObservedDimension[?AgeMeas,?AgeD],sh:P90hasValue[?AgeD,?Age],FILTER(?Age<=64&&?Age>=18),sh:FW44PhysicalActivity[?PA],sh:P14CarriedOutBy[?PA,?P],NOTEXISTS ?PA IN sh:FW49MuscleStrengtheningAnaerobics[?PA].
- Rule 4: Checking if the user has performed muscle-strengthening activities at moderate or greater intensity that involve all major muscle groups on 2 or more days a week, if not, a recommendation will be issued.sh:FWP01isSubjectTo[?P,sh:WHOCode002]:-sh:E21Person[?P],sh:FW152AgeAss[?AgeAss],sh:P140AssignedAttributeTo[?AgeAss,?P],sh:FW200AgeMeas[?AgeMeas],sh:P141Assigned[?AgeAss,?AgeMeas],sh:FW37AgeDim[?AgeD],sh:P40ObservedDimension[?AgeMeas,?AgeD],sh:P90hasValue[?AgeD, ?Age],FILTER(?Age<=64&&?Age>=18),sh:FW2FrequencyDim[?freqD],AGGREGATE(sh:FW49MuscleStrengtheningAnaerobics[?PA],sh:P14CarriedOutBy[?PA, ?P],sh:FW193FrequencyMeas[?M],sh:P117Includes[?PA, ?M],sh:P40ObservedDimension[?M, ?freqD],sh:P90hasValue[?freqD,?freqValue] ON ?P BIND SUM(?freqValue)AS ?freqtotal ),sh:FW176StepsCountMeas[?stepsM],sh:P117Includes[?PA,?stepsM],sh:FW28StepsCountDim[?Stepd],sh:P40ObservedDimension[?stepsM,?Stepd],AGGREGATE(sh:P90hasValue[?Stepd,?stepValue] ON ?Stepd BINDSUM(?stepValue) AS ?stepstotal ),sh:FW40TimeWindowDim[?TW],sh:P90hasValue[?TW,?TWvalue],NOT FILTER(?stepstotal>=7500*?TWvalue&&?freqtotal>=2*?TWvalue) .
- Rule 5: Checking if the user has done at least 150–300 min of moderate-intensity aerobic physical activity; or at least 75–150 of vigorous-intensity aerobic physical activity, if so, a congratulations message will be issued.sh:FWP01isSubjectTo[?P,sh:WHOCode101]:-sh:E21Person[?P],sh:FW152AgeAss[?AgeAss],sh:P140AssignedAttributeTo[?AgeAss,?P],sh:FW200AgeMeas[?AgeMeas],sh:P141Assigned[?AgeAss,?AgeMeas],sh:FW37AgeDim[?AgeD],sh:P40ObservedDimension[?AgeMeas,?AgeD],sh:P90hasValue[?AgeD,?Age],FILTER(?Age<=64&&?Age>=18),sh:FW4DurationDim[?durd],AGGREGATE(sh:FW51CardioAerobics[?PA],sh:P14CarriedOutBy[?PA,?P],sh:FW188DurationMeas[?M],sh:P117Includes[?PA,?M],sh:P40ObservedDimension[?M,?durd],sh:P90hasValue[?durd,?durValue] ON ?P BIND SUM(?durValue)AS ?durtotal),sh:FW176StepsCountMeas[?stepsM],sh:P117Includes[?PA,?stepsM],sh:FW28StepsCountDim[?Stepd],sh:P40ObservedDimension[?stepsM,?Stepd],AGGREGATE(sh:P90hasValue[?Stepd,?stepValue] ON ?StepdBIND SUM(?stepValue) AS ?stepstotal),sh:FW40TimeWindowDim[?TW],sh:P90hasValue[?TW,?TWvalue],FILTER(?stepstotal>=7500*?TWvalue && ?stepstotal<10000*?TWvalue&&?durtotal>150*?TWvalue&&?durtotal<=300*?TWvalue).
- Rule 6: Checking if the user has performed muscle-strengthening activities at moderate or greater intensity that involve all major muscle groups on 2 or more days a week, if so, a congratulations message will be issued.sh:FWP01isSubjectTo[?P,sh:WHOCode102]:-sh:E21Person[?P],sh:FW152AgeAss[?AgeAss],sh:P140AssignedAttributeTo[?AgeAss,?P]sh:FW200AgeMeas[?AgeMeas],sh:P141Assigned[?AgeAss,?AgeMeas],sh:FW37AgeDim[?AgeD],sh:P40ObservedDimension[?AgeMeas,?AgeD],sh:P90hasValue[?AgeD,?Age],FILTER(?Age<=64&&?Age>=18),sh:FW2FrequencyDim[?freqD],AGGREGATE(sh:FW49MuscleStrengtheningAnaerobics[?PA],sh:P14CarriedOutBy[?PA,?P],sh:FW193FrequencyMeas[?M],sh:P117Includes[?PA,?M],sh:P40ObservedDimension[?M,?freqD],sh:P90hasValue[?freqD,?freqValue] ON ?P BINDSUM(?freqValue) AS?freqtotal),sh:FW176StepsCountMeas[?stepsM],sh:P117Includes[?PA,?stepsM],sh:FW28StepsCountDim[?Stepd],sh:P40ObservedDimension[?stepsM,?Stepd],AGGREGATE(sh:P90hasValue[?Stepd,?stepValue] ON ?Stepd BINDSUM(?stepValue) AS ?stepstotal),sh:FW40TimeWindowDim[?TW],sh:P90hasValue[?TW,?TWvalue],FILTER(?stepstotal>=7500*?TWvalue&& ?freqtotal>=2*?TWvalue) .
- Rule 7: Checking if the user has a sedentary behavior, if so, a recommendation will be issued.sh:FWP01isSubjectTo[?P,sh:WHOCode005]:-sh:E21Person[?P],sh:FW152AgeAss[?AgeAss],sh:P140AssignedAttributeTo[?AgeAss,?P],sh:FW200AgeMeas[?AgeMeas],sh:P141Assigned[?AgeAss,?AgeMeas],sh:FW37AgeDim[?AgeD],sh:P40ObservedDimension[?AgeMeas,?AgeD],sh:P90hasValue[?AgeD,?Age],FILTER(?Age<=64&&?Age>=18),sh:P2hasType[?P,sh:sedentarybehavior].
References
- Briazgounov, I.P. The role of physical activity in the prevention and treatment of noncommunicable diseases. World Health Stat. Q. 1988, 41, 242–250. [Google Scholar] [PubMed]
- World Health Organization. The Global Action Plan on Physical Activity 2018–2030. 2018. Available online: http://www.who.int/ncds/prevention/physical-activity/gappa (accessed on 28 November 2021).
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sport. Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- Abdi, S.; Spann, A.; Borilovic, J.; de Witte, L.; Hawley, M. Understanding the care and support needs of older people: A scoping review and categorisation using the WHO international classification of functioning, disability and health framework (ICF). BMC Geriatr. 2019, 19, 195, Erratum in BMC Geriatr. 2020, 20, 23. [Google Scholar] [CrossRef]
- Fischer, F.; Lange, K.; Klose, K.; Greiner, W.; Kraemer, A. Barriers and Strategies in Guideline Implementation—A Scoping Review. Healthcare 2016, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- Grol, R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001, 39 (Suppl. 2), II46–II54. [Google Scholar] [CrossRef] [PubMed]
- Cabana, M.D.; Rand, C.S.; Powe, N.R.; Wu, A.W.; Wilson, M.H.; Abboud, P.A.; Rubin, H.R. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999, 282, 1458–1465. [Google Scholar] [CrossRef] [PubMed]
- Storm-Versloot, M.N.; Knops, A.M.; Ubbink, D.T.; Goossens, A.; Legemate, D.A.; Vermeulen, H. Long-term adherence to a local guideline on postoperative body temperature measurement: Mixed methods analysis. J. Eval. Clin. Pract. 2012, 18, 841–847. [Google Scholar] [CrossRef]
- Russell, S.; Norvig, P. Artificial Intelligence: A Modern Approach, 4th ed.; University of California: Berkeley, CA, USA, 2020. [Google Scholar]
- Wiesner, M.; Pfeifer, D. Health recommender systems: Concepts, requirements, technical basics and challenges. Int. J. Environ. Res. Public Health 2014, 11, 2580–2607. [Google Scholar] [CrossRef]
- Council of Europe Development Bank (CEB). Ageing Populations in Europe: Challenges and Opportunities for the CEB. JAMA 2014. Available online: https://coebank.org/media/documents/Study_Ageing.pdf (accessed on 28 November 2021).
- Xue, Q.-L. The frailty syndrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G. Cardiovascular Health Study Collaborative Research Group. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Higueras-Fresnillo, S.; Cabanas-Sánchez, V.; Lopez-Garcia, E.; Esteban-Cornejo, I.; Banegas, J.R.; Sadarangani, K.P.; Rodríguez-Artalejo, F.; Martinez-Gomez, D. Physical Activity and Association Between Frailty and All-Cause and Cardiovascular Mortality in Older Adults: Population-Based Prospective Cohort Study. J. Am. Geriatr. Soc. 2018, 66, 2097–2103. [Google Scholar] [CrossRef] [PubMed]
- McGilton, K.S.; Vellani, S.; Yeung, L.; Chishtie, J.; Commisso, E.; Ploeg, J.; Andrew, M.K.; Ayala, A.P.; Gray, M.; Morgan, D.; et al. Identifying and understanding the health and social care needs of older adults with multiple chronic conditions and their caregivers: A scoping review. BMC Geriatr. 2018, 18, 231. [Google Scholar] [CrossRef]
- Young, M.E.; Thomas, A.; Lubarsky, S.; Gordon, D.; Gruppen, L.D.; Rencic, J.; Ballard, T.; Holmboe, E.; Da Silva, A.; Ratcliffe, T.; et al. Mapping clinical reasoning literature across the health professions: A scoping review. BMC Med. Educ. 2020, 20, 107. [Google Scholar] [CrossRef]
- Tzitzikas, Y.; Allocca, C.; Bekiari, C.; Marketakis, Y.; Fafalios, P.; Doerr, M.; Minadakis, N.; Patkos, T.; Candela, L. Integrating Heterogeneous and Distributed Information about Marine Species through a Top Level Ontology. In Proceedings of the Research Conference on Metadata and Semantic Research, Thessaloniki, Greece, 19–22 November 2013. [Google Scholar]
- Tjoa, E.; Guan, C. A Survey on Explainable Artificial Intelligence (XAI): Toward Medical XAI. IEEE Trans. Neural Netw. Learn. Syst. 2021, 32, 4793–4813. [Google Scholar] [CrossRef] [PubMed]
- Tsiouris, K.M.; Tsakanikas, V.D.; Gatsios, D.; Fotiadis, D.I. A Review of Virtual Coaching Systems in Healthcare: Closing the Loop With Real-Time Feedback. Front. Digit. Health 2020, 2, 567502. [Google Scholar] [CrossRef] [PubMed]
- Kulyk, O.; op den Akker, R.; Klaassen, R.; van Gemert-Pijnen, L.J. Personalized virtual coaching for lifestyle support: Principles for design and evaluation. Int. J. Adv. Life Sci. 2014, 6, 300. [Google Scholar]
- Op den Akker, H.; Klaassen, R.; op den Akker, R.; Jones, V.M.; Hermens, H.J. Opportunities for smart & tailored activity coaching. In Proceedings of the 26th IEEE International Symposium on Computer-Based Medical Systems, Porto, Portugal, 20–22 June 2013; pp. 546–547. [Google Scholar] [CrossRef]
- DiPietro, L.; Al-Ansari, S.S.; Biddle, S.J.; Borodulin, K.; Bull, F.C.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.; Chastin, S.; et al. Advancing the global physical activity agenda: Recommendations for future research by the 2020 WHO physical activity and sedentary behavior guidelines development group. Int. J. Behav. Nutr. Phys. Act. 2019, 17, 143. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Mentzer, J.; Taira, R. Developing a Physical Activity Ontology to Support the Interoperability of Physical Activity Data. J. Med. Internet Res. 2019, 21, e12776. [Google Scholar] [CrossRef]
- Dragoni, M.; Bailoni, T.; Maimone, R.; Eccher, C. HeLiS: An Ontology for Supporting Healthy Lifestyles. In Proceedings of the Semantic Web—International Semantic Web Conference, ISWC 2018, Monterey, CA, USA, 8–12 October 2018; Lecture Notes in Computer Science. Springer: Cham, Switzerland, 2018; Volume 11137. [Google Scholar]
- Peleg, M. Computer-interpretable clinical guidelines: A methodological review. J. Biomed. Inform. 2013, 46, 744–763. [Google Scholar] [CrossRef]
- Peleg, M.; Boxwala, A.A.; Ogunyemi, O.; Zeng, Q.; Tu, S.; Lacson, R.; Bernstam, E.; Ash, N.; Mork, P.; Ohno-Machado, L.; et al. GLIF3: The evolution of a guideline representation format. In Proceedings of the AMIA Symposium; American Medical Informatics Association: Rockville, MD, USA, 2000; p. 645. [Google Scholar]
- Wang, D.; Peleg, M.; Tu, S.W.; Boxwala, A.A.; Ogunyemi, O.; Zeng, Q.; Greenes, R.A.; Patel, V.L.; Shortliffe, E.H. Design and implementation of the GLIF3 guideline execution engine. J. Biomed. Inform. 2004, 37, 305–318. [Google Scholar] [CrossRef] [PubMed]
- Boxwala, A.A.; Peleg, M.; Tu, S.; Ogunyemi, O.; Zeng, Q.T.; Wang, D.; Patel, V.L.; Greenes, R.A.; Shortliffe, E.H. GLIF3: A representation format for sharable computer-interpretable clinical practice guidelines. J. Biomed. Inform. 2004, 37, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Peleg, M.; Keren, S.; Denekamp, Y. Mapping computerized clinical guidelines to electronic medical records: Knowledge-data ontological mapper (KDOM). J. Biomed. Inform. 2008, 41, 180–201. [Google Scholar] [CrossRef]
- Grando, M.A.; Glasspool, D.; Boxwala, A. Argumentation logic for the flexible enactment of goal-based medical guidelines. J. Biomed. Inform. 2012, 45, 938–949. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Grando, A.; Peleg, M.; Glasspool, D. A goal-oriented framework for specifying clinical guidelines and handling medical errors. J. Biomed. Inform. 2010, 43, 287–299. [Google Scholar] [CrossRef]
- Wilk, S.; Michalowski, W.; Michalowski, M.; Farion, K.; Hing, M.M.; Mohapatra, S. Mitigation of adverse interactions in pairs of clinical practice guidelines using constraint logic programming. J. Biomed. Inform. 2013, 46, 341–353. [Google Scholar] [CrossRef]
- Miller, P.L.; Frawley, S.J.; Sayward, F.G. Maintaining and incrementally revalidating a computer-based clinical guideline: A case study. J. Biomed. Inform. 2001, 34, 99–111. [Google Scholar] [CrossRef][Green Version]
- Pérez, B.; Porres, I. Authoring and verification of clinical guidelines: A model driven approach. J. Biomed. Inform. 2010, 43, 520–536. [Google Scholar] [CrossRef]
- Fernandez-Lopez, M.; Gomez-Perez, A.; Juristo, N. Methontology: From ontological art towards ontological engineering. In Proceedings of the Symposium on Ontological Engineering of AAAI, Rhode Island, Greece, 24–26 March 1997. [Google Scholar]
- Pinto, H.S.; Staab, S.; Tempich, C. DILIGENT: Towards a fine-grained methodology for distributed, loosely-controlled and evolving engineering of ontologies. In Proceedings of the 16th Eureopean Conference on Artificial Intelligence, ECAI’2004, including Prestigious Applicants of Intelligent Systems, PAIS 2004, Valencia, Spain, 22–27 August 2004. [Google Scholar]
- Suarez-Figueroa, M.C. NeOn Methodology for Building Ontology Networks: Specification, Scheduling and Reuse. Ph.D. Thesis, Technical University of Madrid, Madrid, Spain, 2012. [Google Scholar]
- Gangemi, A.; Nicola Guarino, C.M.; Alessandro, O. Understanding Top-Level Ontological Distinctions. In Proceedings of the Seventeenth International Joint Conference on Artificial Intelligence, Menlo Park, CA, USA, 4–10 August 2001. [Google Scholar]
- Allocca, C.; d’Aquin, M.; Motta, E. DOOR: Towards a formalization of ontology relations. In Proceedings of the International Conference on Knowledge Engineering and Ontology Development (KEOD), Madera, Portugal, 6–8 October 2009. [Google Scholar]
- Silva, P.; Andrade, M.T.; Carvalho, P.; Mota, J. A Structured and Flexible Language for Physical Activity Assessment and Characterization. J. Sports Med. 2013, 2013, 420916. [Google Scholar] [CrossRef]
- Gangemi, A.; Guarino, N.; Masolo, C.; Oltramari, A.; Schneider, L. Sweetening ontologies with dolce. In Proceedings of the 13th International Conference on Knowledge Engineering and Knowledge Management, Siguenza, Spain, 1–4 October 2002; Ontologies and the Semantic Web. Springer: Berlin/Heidelberg, Germany, 2002; pp. 166–181. [Google Scholar]
- Doerr, M. The CIDOC CRM—An Ontological Approach to Semantic Interoperability of Metadata. AI Mag. 2003, 24, 75–92. [Google Scholar] [CrossRef]
- Niles, I.; Pease, A. Towards a standard upper ontology. In Proceedings of the International Conference on Formal Ontology in Information Systems-Volume, Ogunquit, ME, USA, 17–19 October 2001; pp. 2–9. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Bamparopoulos, G.; Konstantinidis, E.; Bratsas, C.; Bamidis, P.D. Towards exergaming commons: Composing the exergame ontology for publishing open game data. J. Biomed. Semant. 2016, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Partridge, C.; Mitchell, A.; Cook, A.; Sullivan, J.; West, M. A Survey of Top-Level Ontologies—To inform the ontological choices for a Foundation Data Model. Available online: https://www.repository.cam.ac.uk/handle/1810/313452 (accessed on 28 November 2021).
- Trojahn, C.; Vieira, R.; Schmidt, D.; Pease, A.; Guizzardi, G. Foundational ontologies meet ontology matching: A survey. Semant. Web 2021. [Google Scholar] [CrossRef]
- Nenov, Y.; Piro, R.; Motik, B.; Horrocks, I.; Wu, Z.; Banerjee, J. RDFox: A Highly-Scalable RDF Store. In Proceedings of the Semantic Web—International Semantic Web Conference, Bethlehem, PA, USA, 11–15 October 2015; Lecture Notes in Computer Science. Springer: Cham, Switzerland, 2015; Volume 9367. [Google Scholar] [CrossRef]
- McAvoy, C.R.; Moore, C.C.; Aguiar, E.J.; Ducharme, S.W.; Schuna, J.M., Jr.; Barreira, T.V.; Chase, C.J.; Gould, Z.R.; Amalbert-Birriel, M.A.; Chipkin, S.R.; et al. Cadence (steps/min) and relative intensity in 21 to 60-year-olds: The CADENCE-adults study. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 27. [Google Scholar] [CrossRef] [PubMed]
- W3C OWL Working Group. OWL 2 Web Ontology Language Document Overview, 2nd ed.; W3C Recommendation 11 December 2012; World Wide Web Consortium (W3C): Cambridge, MA, USA, 2012. [Google Scholar]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Lutz, C. The Complexity of Description Logics with Concrete Domains. Ph.D. Thesis, RWTH Aachen University, Computer Science Center, Aachen, Germany, 2002. [Google Scholar]
- Shearer, R.; Motik, B.; Horrocks, I. HermiT: A Highly-Efficient OWL Reasoner. In Proceedings of the Fifth Owled Workshop on Owl: Experiences & Directions, Gaithersburg, MD, USA, 1 January 2008. [Google Scholar]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32 (Suppl. 9), S498–S504. [Google Scholar] [CrossRef]
- Pan, J.Z.; Stoilos, G.; Stamou, G.; Tzouvaras, V.; Horrocks, I. f-SWRL: A Fuzzy Extension of SWRL. In Journal on Data Semantics VI; Spaccapietra, S., Aberer, K., Cudré-Mauroux, P., Eds.; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2006; Volume 4090. [Google Scholar] [CrossRef]
- Amato, F.; Casola, V.; Cozzolino, G.; De Benedictis, A.; Mazzocca, N.; Moscato, F. A Security and Privacy Validation Methodology for e-Health Systems. ACM Trans. Multimed. Comput. Commun. Appl. 2021, 17, 67. [Google Scholar] [CrossRef]






| Intensity category | The purpose of HeLiFit and HeLiFit-Rule is to represent and reason upon the WHO/ACSM guidelines on physical activity and sedentary behavior. |
| Scope | The HeLiFit ontology should focus on characterizing the notion of physical activity as used in the context of WHO/ACSM guidelines and allowing a mean to measure it, whereas HeLiFit focuses on reasoning over the different levels of adherence and issue recommendations to users. |
| Implementation language | Web Ontology Language (OWL) for HeLiFit and RDFox Rule Language for HeLiFit-Rule. |
| Target user | The primary target users are health care professionals (User 1) working with aging frailty users (user 2), aiming to recommend or coach them on physical activity and exercise. Another group of target users (user 3) is professionals involved in the development of digital coach solutions to support physical activity and exercise recommendation, i.e., |
| User 1—Health care professionals dealing with frailty | |
| User 2—Aging frailty users trainer | |
| User 3—Software developer or researcher working in the domain of digital coach for adherence in physical activity domain | |
| Intended uses | User 1: The intended uses of the ontology include: (1) supporting the process of physical activity regimen recommendation to a patient and (2) modifying current physical activity regimen for better adherence. |
| User 2: The intended use is to support the process of modification of user adherence based on changes in the user profile. | |
| User 3: The intended use is to support the development of personalized solutions for physical activity maintenance and modification based on the user’s need. |
| Children and Adolescents |
|---|
| Children and adolescents should do at least an average of 60 min per day of moderate- to vigorous-intensity, mostly aerobic physical activity across the week. |
| Vigorous-intensity aerobic activities, as well as those that strengthen muscle and bone, should be incorporated at least 3 days a week. |
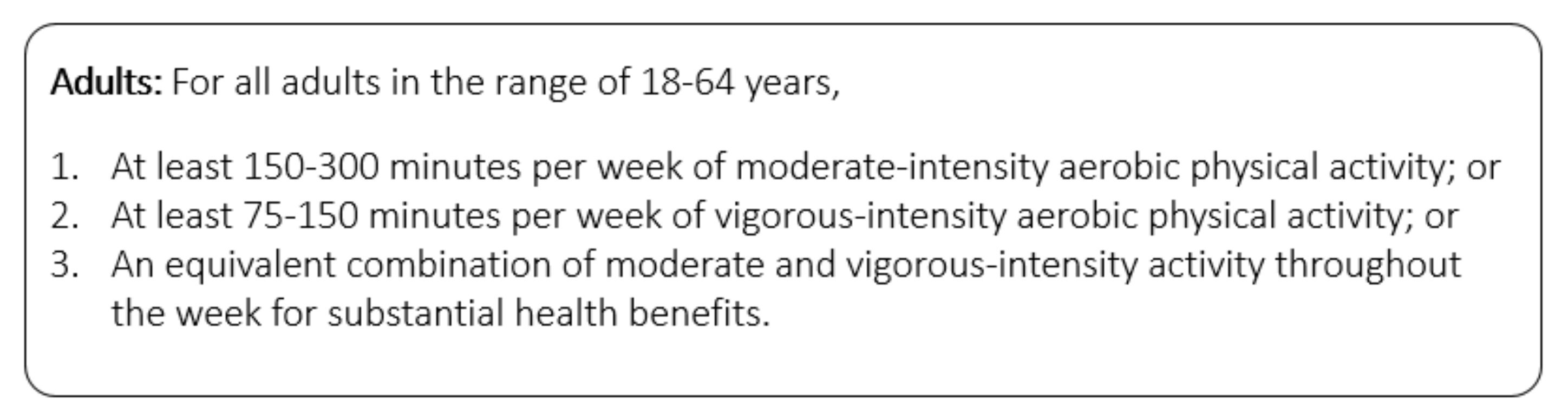
| Adults (aged 18–64 years) |
| All adults should undertake regular physical activity. |
| Adults should do at least 150–300 min of moderate-intensity aerobic physical activity; or at least 75–150 min of vigorous-intensity aerobic physical activity; or an equivalent combination of moderate- and vigorous-intensity activity throughout the week, for substantial health benefits. |
| Adults should also do muscle-strengthening activities at moderate or greater intensity that involve all major muscle groups on 2 or more days a week, as these provide additional health benefits. |
| Adults should limit the amount of time spent being sedentary. Replacing sedentary time with physical activity of any intensity (including light intensity) provides health benefits. |
| Older adults (aged 65 years and older) |
| Older adults should do at least 150–300 min of moderate-intensity aerobic physical activity; or at least 75–150 min of vigorous-intensity aerobic physical activity; or an equivalent combination of moderate- and vigorous intensity activity throughout the week, for substantial health benefits. |
| Older adults may increase moderate intensity aerobic physical activity to more than 300 min; or do more than 150 min of vigorous-intensity aerobic physical activity; or an equivalent combination of moderate- and vigorous intensity activity throughout the week, for additional health benefits. |
| To help reduce the detrimental effects of high levels of sedentary behavior on health, older adults should aim to do more than the recommended levels of moderate to vigorous-intensity physical activity. |
| Pregnant and postpartum women |
| All pregnant and postpartum women without contraindication should do at least 150 min of moderate-intensity aerobic physical activity throughout the week for substantial health benefits. |
| All pregnant and postpartum women without contraindication should incorporate a variety of aerobic and muscle-strengthening activities. Adding gentle stretching may also be beneficial |
| Pregnant and postpartum women should limit the amount of time spent being sedentary. Replacing sedentary time with physical activity of any intensity (including light intensity) provides health benefits. |
| Intensity Category | Objective Measures |
|---|---|
| Sedentary | |
| per minute [51] | |
| Moderate | |
| per minute [51] | |
| Vigorous | 6<MET<9 |
| per minute [51] | |
| High | 9<MET |
| R | |
| Steps > 140.7 per minute [51] |
| Metrics | |||
|---|---|---|---|
| Axiom | 770 | Logical axiom count | 308 |
| Declaration axiom count | 289 | Class count | 250 |
| Object property count | 12 | Data property count | 5 |
| Individual count | 23 | Annotation property count | 1 |
| DL expressivity | ALHI(D) | SubClassOf | 246 |
| SubObjectPropertyOf | 2 | InverseObjectPropertiesf | 3 |
| ObjectPropertyDomain | 10 | ObjectPropertyRange | 10 |
| SubDataPropertyOf | 2 | DataPropertyDomain | 6 |
| DataPropertyRange | 6 | ClassAssertion | 23 |
| AnnotationAssertion | 173 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allocca, C.; Jilali, S.; Ail, R.; Lee, J.; Kim, B.; Antonini, A.; Motta, E.; Schellong, J.; Stieler, L.; Haleem, M.S.; et al. Toward a Symbolic AI Approach to the WHO/ACSM Physical Activity & Sedentary Behavior Guidelines. Appl. Sci. 2022, 12, 1776. https://doi.org/10.3390/app12041776
Allocca C, Jilali S, Ail R, Lee J, Kim B, Antonini A, Motta E, Schellong J, Stieler L, Haleem MS, et al. Toward a Symbolic AI Approach to the WHO/ACSM Physical Activity & Sedentary Behavior Guidelines. Applied Sciences. 2022; 12(4):1776. https://doi.org/10.3390/app12041776
Chicago/Turabian StyleAllocca, Carlo, Samia Jilali, Rohit Ail, Jaehun Lee, Byungho Kim, Alessio Antonini, Enrico Motta, Julia Schellong, Lisa Stieler, Muhammad Salman Haleem, and et al. 2022. "Toward a Symbolic AI Approach to the WHO/ACSM Physical Activity & Sedentary Behavior Guidelines" Applied Sciences 12, no. 4: 1776. https://doi.org/10.3390/app12041776
APA StyleAllocca, C., Jilali, S., Ail, R., Lee, J., Kim, B., Antonini, A., Motta, E., Schellong, J., Stieler, L., Haleem, M. S., Georga, E., Pecchia, L., Gaeta, E., & Fico, G. (2022). Toward a Symbolic AI Approach to the WHO/ACSM Physical Activity & Sedentary Behavior Guidelines. Applied Sciences, 12(4), 1776. https://doi.org/10.3390/app12041776








