The Effect of the Digital Manufacturing Technique, Preparation Taper, and Cement Type on the Retention of Aged Anterior Provisional Crowns: An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
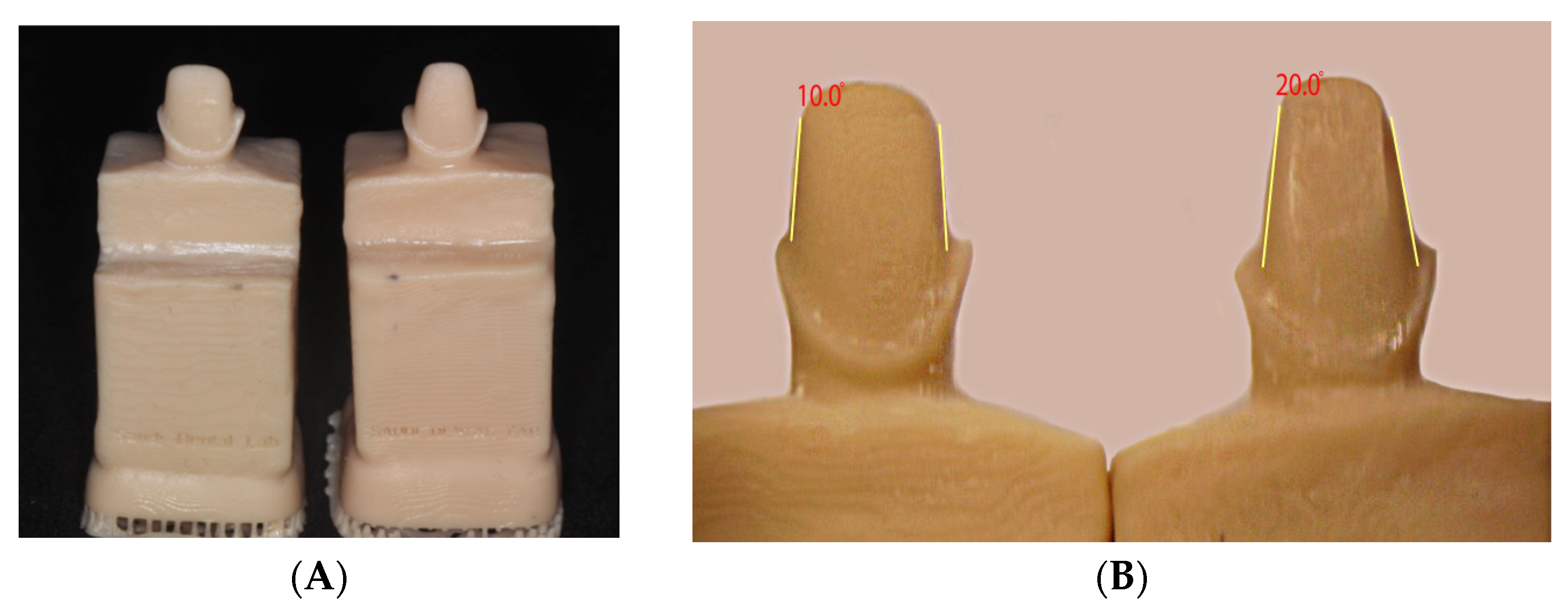
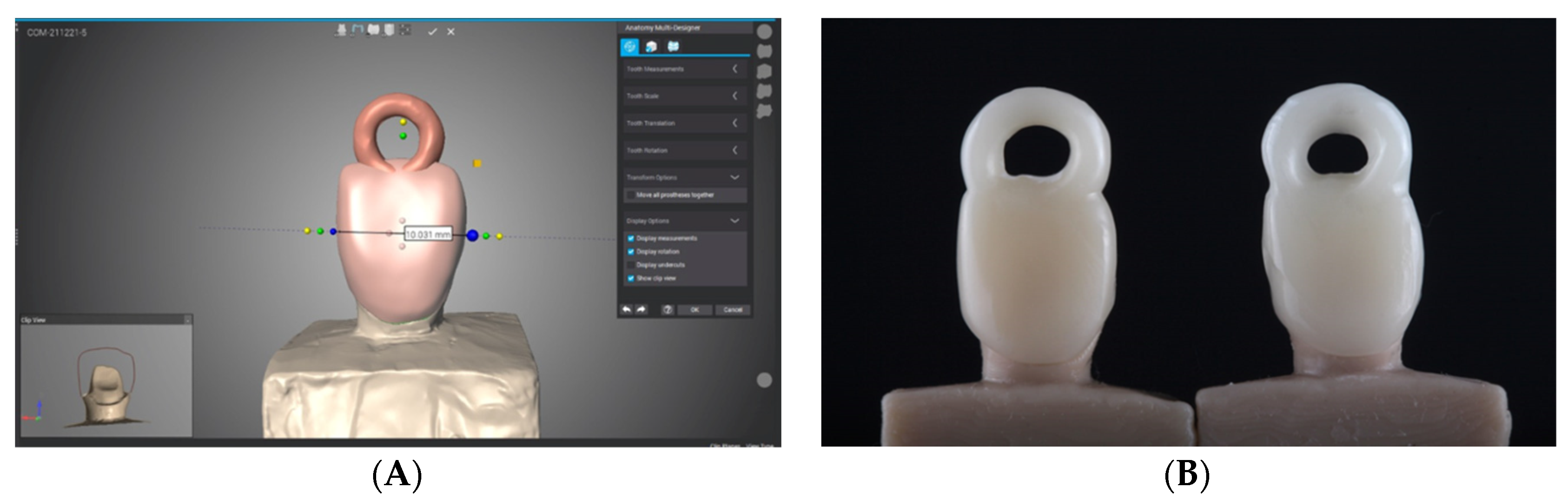
2.1. Fabrication of Test Samples
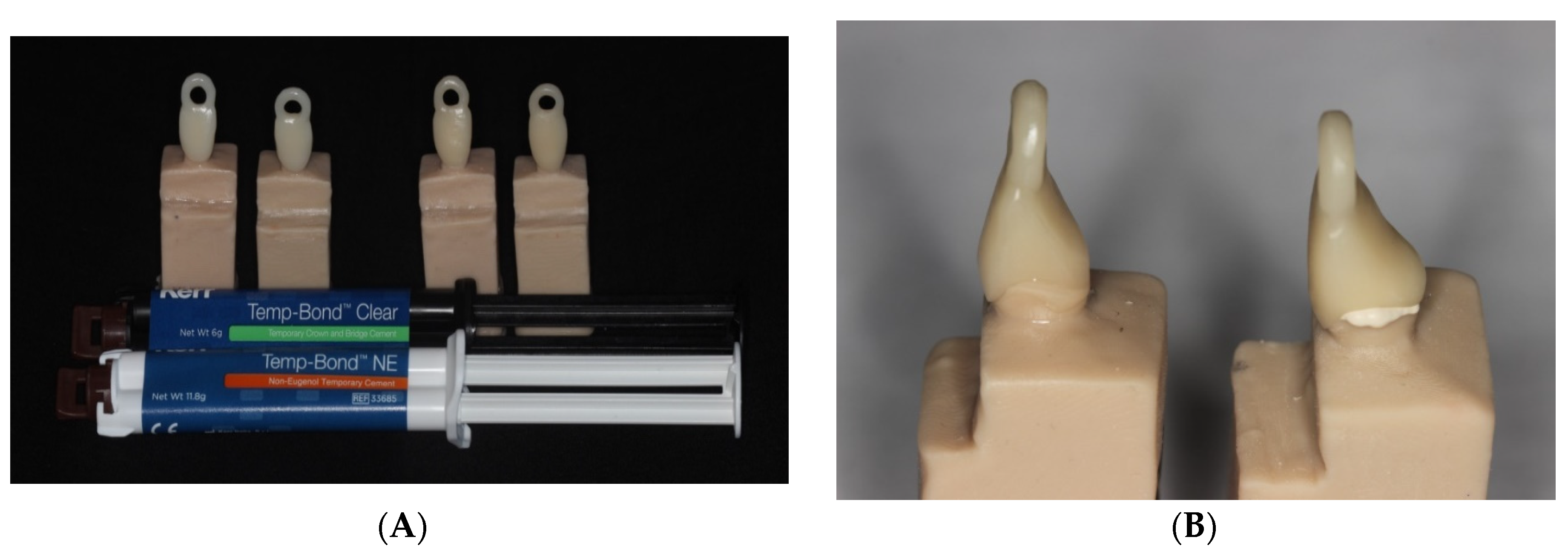
2.2. Cementation of Provisional Crowns
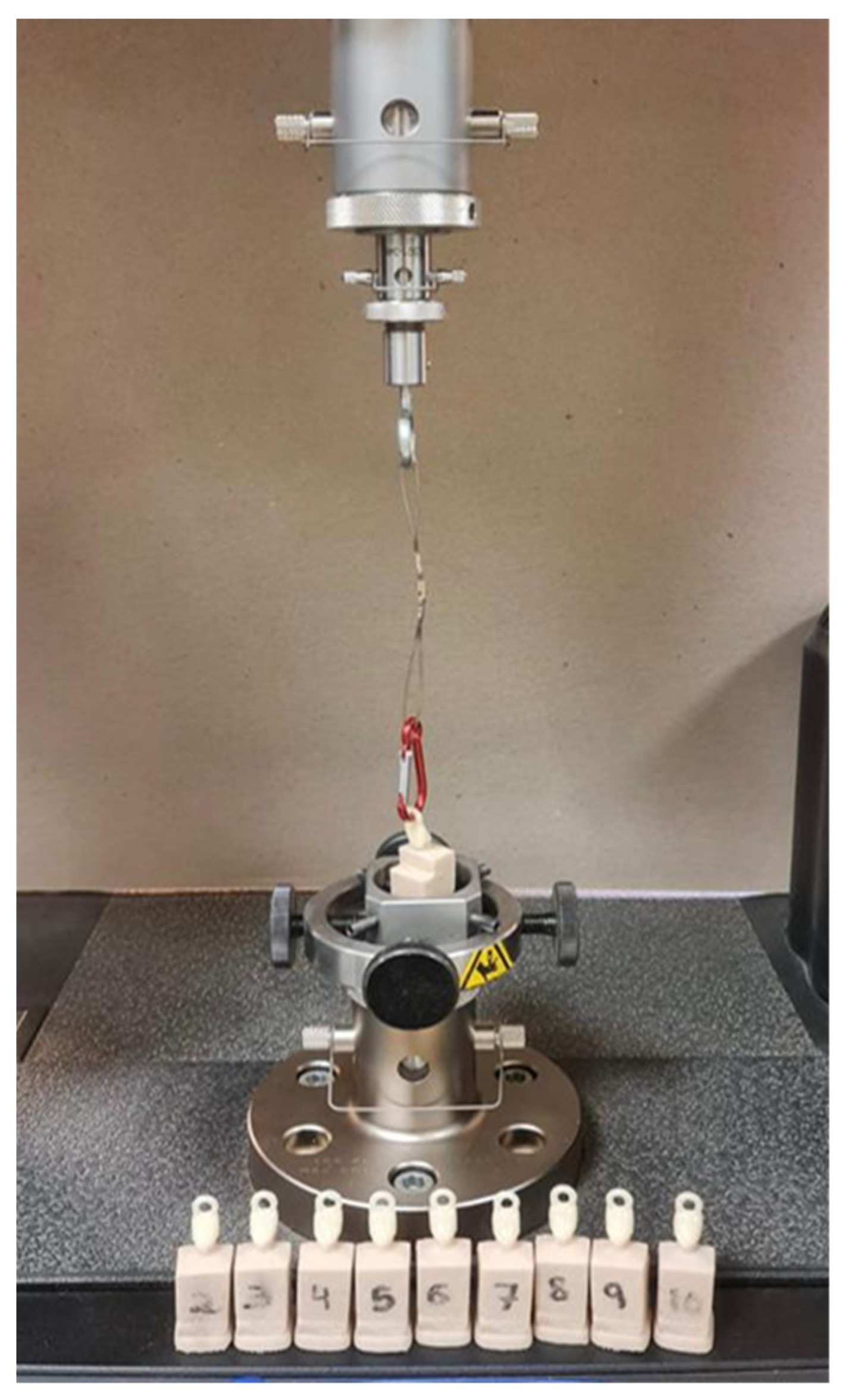
2.3. Aging and Pull-Off Testing with Universal Testing Machine
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abad-Coronel, C.; Carrera, E.; Córdova, N.M.; Fajardo, J.I.; Aliaga, P. Comparative Analysis of Fracture Resistance between CAD/CAM Materials for Interim Fixed Prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef] [PubMed]
- Mârțu, I.; Murariu, A.; Baciu, E.-R.; Savin, C.-N.; Foia, I.; Tatarciuc, M.; Diaconu-Popa, D. An Interdisciplinary Study Regarding the Characteristics of Dental Resins Used for Temporary Bridges. Medicina 2022, 58, 811. [Google Scholar] [CrossRef] [PubMed]
- Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Ripszky Totan, A.; Imre, M.; Țâncu, A.M.C.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison. Materials 2022, 15, 3075. [Google Scholar] [CrossRef] [PubMed]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef] [PubMed]
- Güth, J.F.; e Silva, J.A.; Edelhoff, D. Enhancing the predictability of complex rehabilitation with a removable CAD/CAM-fabricated long-term provisional prosthesis: A clinical report. J. Prosthodont. Dent. 2021, 107, 1–6. [Google Scholar] [CrossRef]
- Sampaio, C.S.; Niemann, K.D.; Schweitzer, D.D.; Hirata, R.; Atria, P.J. Microcomputed tomography evaluation of cement film thickness of veneers and crowns made with conventional and 3D printed provisional materials. J. Esthet. Restor. Dent. 2021, 33, 487–495. [Google Scholar] [CrossRef]
- Mayer, J.; Stawarczyk, B.; Vogt, K.; Hickel, R.; Edelhoff, D.; Reymus, M. Influence of cleaning methods after 3D printing on two-body wear and fracture load of resin-based temporary crown and bridge material. Clin. Oral Investig. 2021, 25, 5987–5996. [Google Scholar] [CrossRef]
- Karaman, T.; Eser, B.; Altintas, E.; Atala, M.-H. Evaluation of the effects of finish line type and width on the fracture strength of provisional crowns. Odontology 2021, 109, 76–81. [Google Scholar] [CrossRef]
- Hensel, F.; Koenig, A.; Doerfler, H.-M.; Fuchs, F.; Rosentritt, M.; Hahnel, S. CAD/CAM Resin-Based Composites for Use in Long-Term Temporary Fixed Dental Prostheses. Polymers 2021, 13, 3469. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Sidhom, M.; Zaghloul, H.; Mosleh, I.E.-S.; Eldwakhly, E. Effect of Different CAD/CAM Milling and 3D Printing Digital Fabrication Techniques on the Accuracy of PMMA Working Models and Vertical Marginal Fit of PMMA Provisional Dental Prosthesis: An In Vitro Study. Polymers 2022, 14, 1285. [Google Scholar] [CrossRef] [PubMed]
- Parize, H.; Tardelli, J.D.C.; Bohner, L.; Sesma, N.; Muglia, V.A.; dos Reis, A.C. Digital versus conventional workflow for the fabrication of physical casts for fixed prosthodontics: A systematic review of accuracy. J. Prosthet. Dent. 2022, 128, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Al-Moaleem, M.M.; AlMakhloti, E.; Porwal, A.; Shariff, M.; Tikare, S. Evaluation of the degree of taper and convergence angle of full ceramo-metal crown preparations by different specialists centers at Assir Region, Saudi Arabia. Saudi J. Med. Med. Sci. 2015, 3, 198. [Google Scholar] [CrossRef]
- Alabdulkader, M.A.; Habib, S.R. Effect of cement application techniques on the adaptation and retention of provisional crowns. Technol. Health Care 2018, 6, 945–955. [Google Scholar] [CrossRef] [PubMed]
- Narula, S.; Punia, V.; KhaNdelWal, M.; Sharma, V.; Pamecha, S. Retention in Conventional Fixed Partial Dentures: A Review. J. Clin. Diagn. Res. 2011, 5, 1128–1133. [Google Scholar]
- Rodríguez, J.L.R.; Martínez, D.M.; Font, A.F.; Panadero, R.A.; Fernandez-Estevan, L. Traction test of temporary dental cements. J. Clin. Exp. Dent. 2017, 9, e564–e568. [Google Scholar] [CrossRef][Green Version]
- Lewinstein, I.; Stoleru-Baron, J.; Block, J.; Kfir, A.; Matalon, S.; Ormianer, Z. Antibacterial activity and tensile strength of provisional cements modified with fluoridecontaining varnish. Quintessence Int. 2013, 44, 107–112. [Google Scholar] [CrossRef]
- Zidan, O.; Ferguson, G.C. The retention of complete crowns prepared with three different tapers and luted with four different cements. J. Prosthet. Dent. 2003, 89, 565–571. [Google Scholar] [CrossRef]
- Chan, D.C.; Wilson, A.H., Jr.; Barbe, P.; Cronin, R.J., Jr.; Chung, C.; Chung, K. Effect of preparation convergence on retention and seating discrepancy of complete veneer crowns. J. Oral. Rehabil. 2005, 32, 58–64. [Google Scholar] [CrossRef]
- Ayad, M.F.; Johnston, W.-M.; Rosenstiel, S.-F. Influence of tooth preparation taper and cement type on recementation strength of complete metal crowns. J. Prosthet. Dent. 2009, 10, 354–361. [Google Scholar] [CrossRef]
- Lepe, X.; Bales, D.J.; Johnson, G.H. Retention of provisional crowns fabricated from two materials with the use of four temporary cements. J. Prosthet. Dent. 1999, 81, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D. Crown pull-off test (crown retention test) to evaluate the bonding effectiveness of luting agents. Dent. Mater. 2010, 26, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Graf, T.; Erdelt, K.-J.; Güth, J.-F.; Edelhoff, D.; Schubert, O.; Schweiger, J. Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns. Biomedicines 2022, 10, 2186. [Google Scholar] [CrossRef]
- Sathish, K.; Kumar, S.S.; Magal, R.T.; Selvaraj, V.; Narasimharaj, V.; Karthikeyan, R.; Sabarinathan, G.; Tiwari, M.; Kassa, A.E. A Comparative Study on Subtractive Manufacturing and Additive Manufacturing. Adv. Mater. Sci. Eng. 2022, 2022, 6892641. [Google Scholar] [CrossRef]
- Aldahian, N.; Khan, R.; Mustafa, M.; Vohra, F.; Alrahlah, A. Influence of Conventional, CAD-CAM, and 3D Printing Fabrication Techniques on the Marginal Integrity and Surface Roughness and Wear of Interim Crowns. Appl. Sci. 2021, 11, 8964. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applications in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Al-Halabi, M.N.; Bshara, N.; Nassar, J.A.; Comisi, J.C.; Rizk, C.K. Clinical Performance of Two Types of Primary Molar Indirect Crowns Fabricated by 3D Printer and CAD/CAM for Rehabilitation of Large Carious Primary Molars. Eur. J. Dent. 2021, 15, 463–468. [Google Scholar] [CrossRef]
- Muruppel, A.M.; Muruppel, A.M.; Nair, D.; Thomas, J.; Saratchandran, S.; Gladstone, S.; Rajeev, M.M. Assessment of Retention and Resistance Form of Tooth Preparations for All Ceramic Restorations using Digital Imaging Technique. J. Contemp. Dent. Pract. 2018, 19, 143–149. [Google Scholar] [CrossRef]
- Tiu, J.; Al-Amleh, B.; Waddell, J.N.; Duncan, W.J. Clinical tooth preparations and associated measuring methods: A systematic review. J. Prosthet. Dent. 2015, 113, 175–184. [Google Scholar] [CrossRef]
- Naidoo, N.; Moipolai, P.D.; Motloba, P. A Comparison of Convergence Angles of Crown preparations in an undergraduate programme at a Tertiary Institution. S. Afr. Dent. J. 2022, 76, 602–606. [Google Scholar] [CrossRef]
- Mack, P.J. A theoretical and clinical investigation into the taper achieved on crown and inlay preparations. J. Oral. Rehabil. 1980, 7, 255–265. [Google Scholar] [CrossRef] [PubMed]
- El-Mubarak, N.; Abu-Bakr, N.; Omer, O.; Ibrahim, Y. Assessment of undergraduate students’ tooth preparation for full veneer cast restorations. Open J. Stomatol. 2014, 4, 43–48. [Google Scholar] [CrossRef]
- Rafeek, R.N.; Marchan, S.M.; Seymour, K.G.; Zou, L.F.; Samarawickrama, D.Y. Abutment taper of full cast crown preparations by dental students in the UWI School of Dentistry. Eur. J. Prosthodont. Restor. Dent. 2006, 14, 63–66. [Google Scholar] [PubMed]
- Dorriz, H.; Nokar, S.; Naini, R.B.; Madadi, A. The convergence angle of full-coverage crown preparations made by dental students. J. Dent. Med. Tehran Univ. Med. Sci. 2008, 5, 37–41. [Google Scholar]
- Tripathi, S.; Amarnath, G.S.; Muddugangadhar, B.C.; Sharma, A.; Choudhary, S. Effect of Preparation Taper, Height and Marginal Design Under Varying Occlusal Loading Conditions on Cement Lute Stress: A Three Dimensional Finite Element Analysis. J. Indian Prosthodont. Soc. 2014, 14, 110–118. [Google Scholar] [CrossRef]
- Lee, W.-S.; Lee, D.-H.; Lee, K.-B. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J. Adv. Prosthodont. 2017, 9, 265–270. [Google Scholar] [CrossRef]
- Al Wadei, M.H.D.; Sayed, M.E.; Jain, S.; Aggarwal, A.; Alqarni, H.; Gupta, S.G.; Alqahtani, S.M.; Alahmari, N.M.; Alshehri, A.H.; Jain, M.; et al. Marginal Adaptation and Internal Fit of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM-Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Coatings 2022, 12, 1777. [Google Scholar] [CrossRef]
- Nakamura, T.; Dei, N.; Kojima, T.; Wakabayashi, K. Marginal and internal fit of Cerec 3 CAD/CAM all-ceramic crowns. Int. J. Prosthodont. 2003, 16, 244–248. [Google Scholar]
- Iwai, T.; Komine, F.; Kobayashi, K.; Saito, A.; Matsumura, H. Influence of convergence angle and cement space on adaptation of zirconium dioxide ceramic copings. Acta Odontol. Scand. 2008, 4, 214–218. [Google Scholar] [CrossRef]
- Gumus, H.-O.; Kurtulus, I.-L.; Kuru, E. Evaluation and comparison of the film thicknesses of six temporary cements before and after thermal cycling. Niger. J. Clin. Pract. 2018, 21, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Peixoto, R.F.; De Aguiar, C.R.; Jacob, E.S.; Macedo, A.P.; Mattos, M.D.G.C.D.; Antunes, R.P.D.A. Influence of Temporary Cements on the Bond Strength of Self-Adhesive Cement to the Metal Coronal Substrate. Braz. Dent. J. 2015, 26, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Sound, S. ADA Professional Product Review. Tempor. Cem. 2011, 6, 13–16. [Google Scholar]
- Arwatchanakan, S.; Phatomworachad, S.; Kosuwon, P.; Phetpranomporn, S.; Luansritisakul, P. The Comparison of Temporary Crown Retention Among Three Temporary Cements. In Proceedings of the Continental European Division Meeting, Florence, Italy, 9 June 2013. [Google Scholar]
- Sarfaraz, H.; Hassan, A.; Shenoy, K.K.; Shetty, M. An in vitro study to compare the influence of newer luting cements on retention of cement-retained implant-supported prosthesis. J. Indian Prosthodont. Soc. 2019, 19, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Cuellar, A.R.; Donmez, M.B.; Schimmel, M.; Abou-Ayash, S.; Lu, W.-E.; Yilmaz, B. Effect of Printing Layer Thickness on the Trueness and Margin Quality of 3D-Printed Interim Dental Crowns. Appl. Sci. 2021, 11, 9246. [Google Scholar] [CrossRef]


| Group 1 | Milled—10°—Non-eugenol conventional cement |
| Group 2 | Milled—10°—Clear cement |
| Group 3 | Milled—20°—Non-eugenol conventional cement |
| Group 4 | Milled—20°—Clear cement |
| Group 5 | Printed—10°—Non-eugenol conventional cement |
| Group 6 | Printed—10°—Clear cement |
| Group 7 | Printed—20°—Non-eugenol conventional cement |
| Group 8 | Printed—20°—Clear cement |
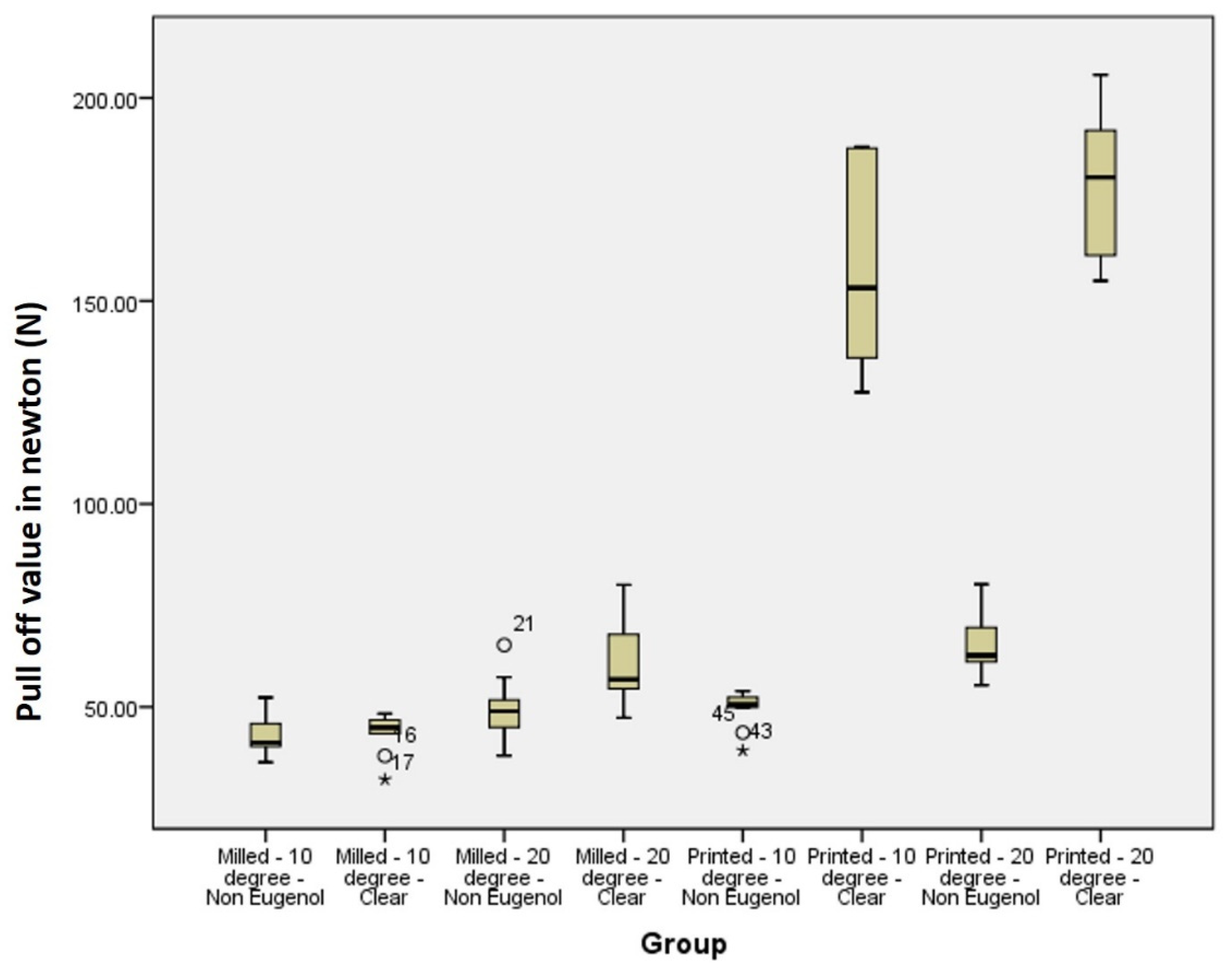
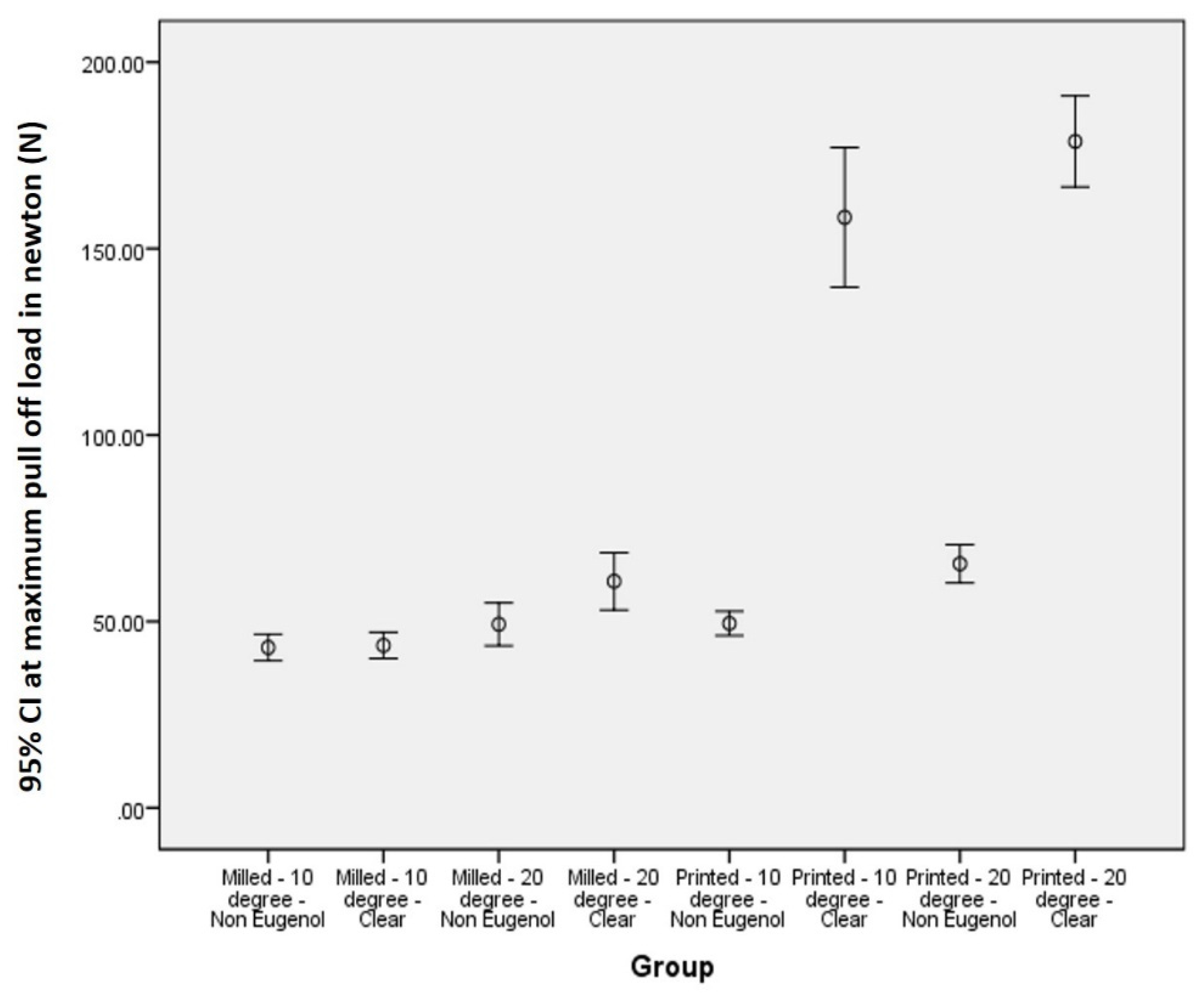
| Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | Group 6 | Group 7 | Group 8 | |
|---|---|---|---|---|---|---|---|---|
| n—number of samples per group | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| Maximum (N) | 52.34 | 48.35 | 65.25 | 80.10 | 53.88 | 188.02 | 80.24 | 205.65 |
| Mean (N) | 43.01 | 43.48 | 49.24 | 60.76 | 49.15 | 158.37 | 65.48 | 178.74 |
| Median (N) | 41.27 | 45.46 | 48.94 | 56.79 | 50.56 | 153.23 | 62.69 | 180.44 |
| Minimum(N) | 36.38 | 32.14 | 37.98 | 47.31 | 39.28 | 127.50 | 55.31 | 154.95 |
| Standard deviation (N) | 4.93 | 5.20 | 8.04 | 10.77 | 4.64 | 26.19 | 7.16 | 17.09 |
| Group | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| MD/p-Value | MD/p-Value | MD/p-Value | MD/p-Value | MD/p-Value | MD/p-Value | MD/p-Value | MD/p-Value | |
| 1 | X | −0.56/0.921 | −6.23/0.274 | 17.75/0.002 * | −6.46/0.257 | 115.36/0.000 * | 115.36/0.000 * | −135.73 */0.000 * |
| 2 | −0.56/0.921 | X | −5.67/0.319 | −17.19 */0.003 * | −5.90/0.301 | −114.80 */0.000 * | −21.91/0.000 * | 135.17 */0.000 * |
| 3 | −6.23/0.274 | −5.67/0.319 | X | −11.52/0.045 * | −0.23/0.968 | −109.13/0.000 * | −16.24 */0.005 * | −129.50 */0.000 * |
| 4 | 17.75/0.002 * | −17.19 */0.003 * | −11.52/0.045 * | X | 11.30 */0.050 * | −109.13/0.000 * | −16.24 */0.005 * | −129.50 */0.000 * |
| 5 | −6.46/0.257 | −5.90/0.301 | −0.23/0.968 | 11.30 */0.050 * | X | −108.91 */0.000 * | −16.01 */0.006 * | −129.27 */0.000 * |
| 6 | −115.36/0.000 * | −114.80 */0.000 * | −109.13/0.000 * | −97.61 */0.000 * | −108.91 */0.000 * | X | 92.90 */0.000 * | −20.36 */0.001 * |
| 7 | −22.47 */0.000 * | −21.91/0.000 * | −16.24 */0.005 * | −4.72/0.407 | −16.01 */0.006 * | 92.90 */0.000 * | X | −113.26 */0.000 * |
| 8 | −135.73 */0.000 * | 135.17 */0.000 * | −129.50 */0.000 * | −117.98 */0.000 * | −129.27 */0.000 * | −20.36 */0.001 * | −113.26 */0.000 * | X |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lunkad, H.; Sayed, M.E.; Alhazmi, A.E.; Alwadani, B.; Shafei, A.M.; Ayoub, M.N.; Shabi, M.M.A.; Mesawa, S.A.; Abdulfatah, B.A.; Alqarni, H.; et al. The Effect of the Digital Manufacturing Technique, Preparation Taper, and Cement Type on the Retention of Aged Anterior Provisional Crowns: An In Vitro Study. Appl. Sci. 2022, 12, 12714. https://doi.org/10.3390/app122412714
Lunkad H, Sayed ME, Alhazmi AE, Alwadani B, Shafei AM, Ayoub MN, Shabi MMA, Mesawa SA, Abdulfatah BA, Alqarni H, et al. The Effect of the Digital Manufacturing Technique, Preparation Taper, and Cement Type on the Retention of Aged Anterior Provisional Crowns: An In Vitro Study. Applied Sciences. 2022; 12(24):12714. https://doi.org/10.3390/app122412714
Chicago/Turabian StyleLunkad, Honey, Mohammed E. Sayed, Abdullah Essa Alhazmi, Bandar Alwadani, Ameen Marwei Shafei, Muath Naji Ayoub, Maan Mohammed A. Shabi, Sara Ahmad Mesawa, Basmah Alhassan Abdulfatah, Hatem Alqarni, and et al. 2022. "The Effect of the Digital Manufacturing Technique, Preparation Taper, and Cement Type on the Retention of Aged Anterior Provisional Crowns: An In Vitro Study" Applied Sciences 12, no. 24: 12714. https://doi.org/10.3390/app122412714
APA StyleLunkad, H., Sayed, M. E., Alhazmi, A. E., Alwadani, B., Shafei, A. M., Ayoub, M. N., Shabi, M. M. A., Mesawa, S. A., Abdulfatah, B. A., Alqarni, H., Alqahtani, S. M., Alamoudi, A., Almalki, M. S., Jethlia, A., & Jain, S. (2022). The Effect of the Digital Manufacturing Technique, Preparation Taper, and Cement Type on the Retention of Aged Anterior Provisional Crowns: An In Vitro Study. Applied Sciences, 12(24), 12714. https://doi.org/10.3390/app122412714









