Do Psychogenic Erectile Dysfunction and Premature Ejaculation Share a Neural Circuit? Evidence from a fMRI Systematic Review and Meta-Analysis
Abstract
:1. Introduction
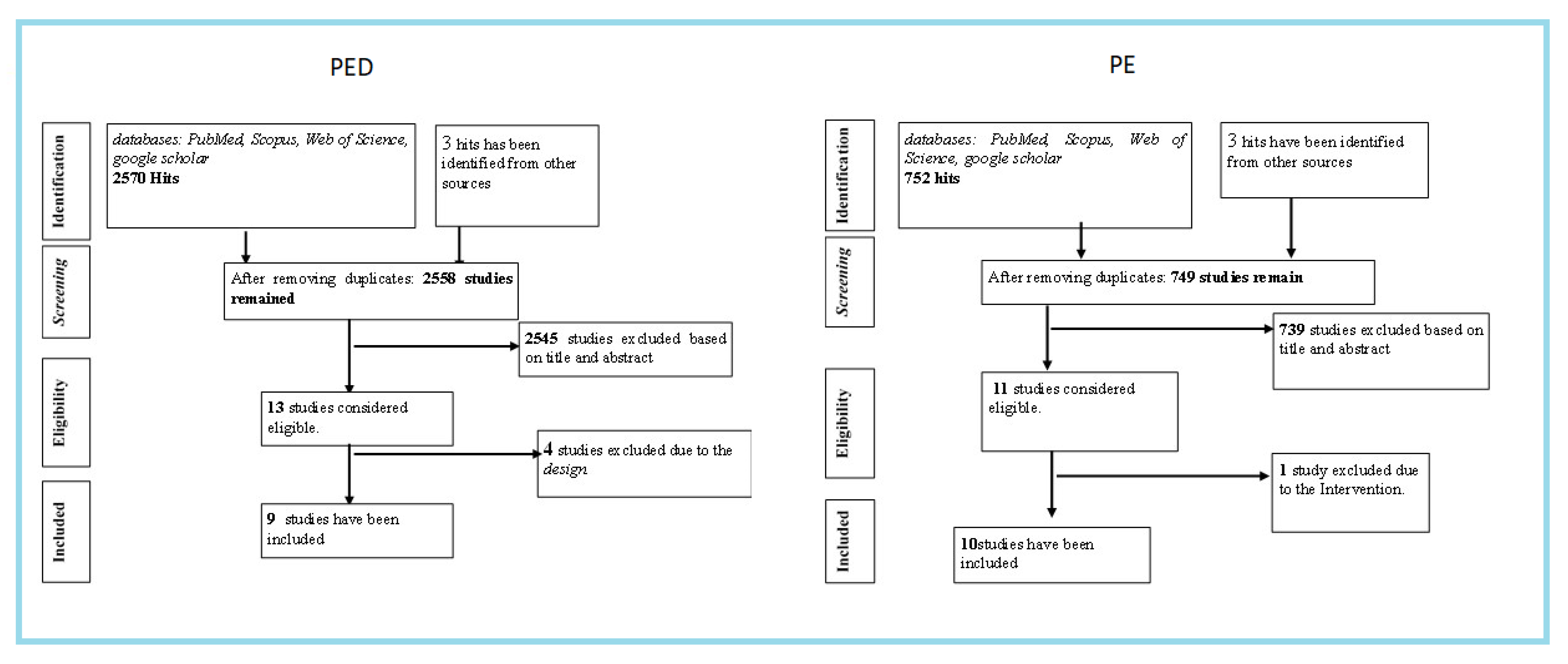
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Socio-Demographic and Behavioral Data Analysis
2.4. Brain-Clusters Data Extraction
3. Results
3.1. Characteristics of the Included Studies
3.2. Sociodemographic Results
3.3. Behavioral Results
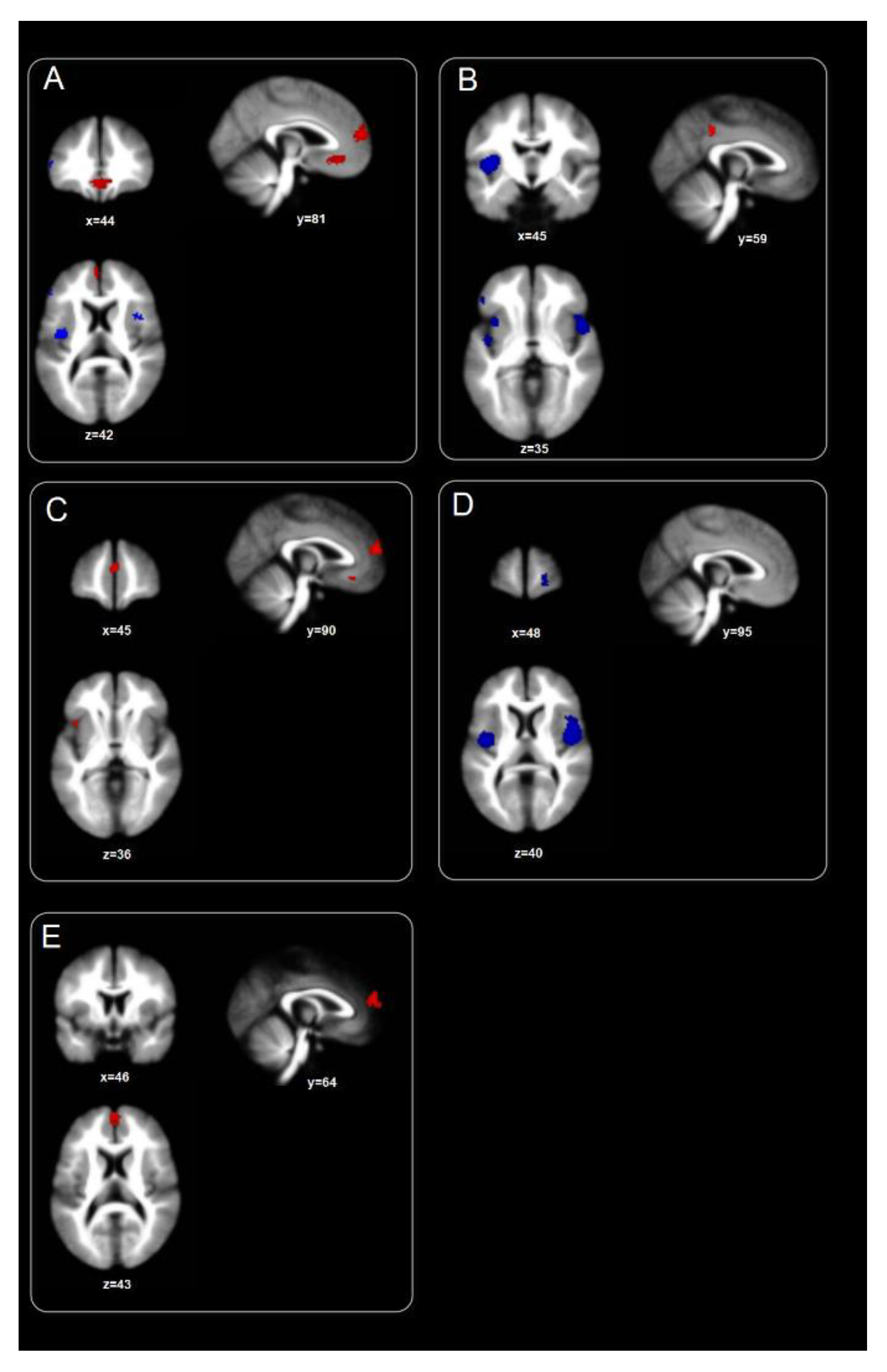
3.4. Homogeneity Maps Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- PICO Worksheet and Search Strategy Protocol
- 1.
- Define your question using PICO by identifying: Patient/Problem, Intervention, Comparison group and outcome:
- 2.
- Type of question/problem:
- 3.
- Type of studies/publications to include in the search:
- 4.
- List main topics and alternate terms from your PICO question that can be used for your search: “experimental studies”; “men”; “fMRI BOLD”; “erotic stimuli”; “Sexual behavior”; “Sexual dysfunction”; “Brain region activity”.
- 5.
- Write out your search strategy: “fMRI” AND “Psychogenic Erectile Dysfunction” OR “Psychogenic ED” OR” Neuroimaging” AND “fMRI” AND “premature ejaculation” Boolean search operators (AND) and (OR).
- 6.
- List any limits that may apply to your search: Gender: Male; Age: Adults; Year(s) of publication: 2003–2020; Language(s): English
- 7.
- List the databases you will search: Google Scholar, PubMed, Scopus, and Web of Science.
- This form is adapted from: Miller, S.A. (2001). PICO worksheet and search strategy. US National Center for Dental Hygiene Research
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Dewitte, M.; Bettocchi, C.; Carvalho, J.; Corona, G.; Flink, I.; Limoncin, E.; van Lankveld, J. A psychosocial approach to erectile dysfunction: Position statements from the European Society of Sexual Medicine (ESSM). Sex. Med. 2021, 9, 100434. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Zhang, S.; Wei, Z.; Zhang, X.; Wang, Q. Prevalence of sexual dysfunction among the male populations who seeking medical care for infertility, pregnancy loss and preconception care: A cross-sectional study. Sci. Rep. 2022, 12, 12969. [Google Scholar] [CrossRef] [PubMed]
- Murtadha, M.; Raslan, M.; Fahmy, S.; Sabri, N. Changes in the Pharmacokinetics and Pharmacodynamics of Sildenafil in Cigarette and Cannabis Smokers. Pharmaceutics 2021, 13, 876. [Google Scholar] [CrossRef]
- Farre, J.M.; Fora, F.; Lasheras, M.G. Specific aspects of erectile dysfunction in psychiatry. Int. J. Impot. Res. 2004, 16, S46–S49. [Google Scholar] [CrossRef]
- Vargas-Cáceres, S.; Cera, N.; Nobre, P.; Ramos-Quiroga, J.A. The Impact of Psychosis on Sexual Functioning: A Systematic Review. J. Sex. Med. 2021, 18, 457–466. [Google Scholar] [CrossRef]
- Waldinger, M.D. Premature Ejaculation: State of the Art. Urol. Clin. N. Am. 2007, 34, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Braun, M.; Wassmer, G.; Klotz, T.; Reifenrath, B.; Mathers, M.; Engelmann, U. Epidemiology of erectile dysfunction: Results of the ‘Cologne Male Survey’. Int. J. Impot. Res. 2000, 12, 305–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teles, A.G.; Carreira, M.; Alarcão, V.; Sociol, D.; Aragüés, J.M.; Lopes, L.; Mascarenhas, M.; e Costa, J.G. Prevalence, Severity, and Risk Factors for Erectile Dysfunction in a Representative Sample of 3,548 Portuguese Men Aged 40 to 69 Years Attending Primary Healthcare Centers: Results of the Portuguese Erectile Dysfunction Study. J. Sex. Med. 2008, 5, 1317–1324. [Google Scholar] [CrossRef]
- Laumann, E.O.; Nicolosi, A.; Glasser, D.B.; Paik, A.; Gingell, C.; Moreira, E.; Wang, T. Sexual problems among women and men aged 40–80 y: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int. J. Impot. Res. 2005, 17, 39–57. [Google Scholar] [CrossRef]
- Lee, S.W.; Lee, J.H.; Sung, H.H.; Park, H.J.; Park, J.K.; Choi, S.K.; Kam, S.C. The prevalence of premature ejaculation and its clinical characteristics in Korean men according to different definitions. Int. J. Impot. Res. 2013, 25, 2–17. [Google Scholar] [CrossRef] [Green Version]
- Quintas-Gomes, A.L.; Nobre, P. Prevalence of Sexual Problems in Portugal: Results of a Population-Based Study Using a Stratified Sample of Men Aged 18 to 70 Years. J. Sex Res. 2014, 51, 13–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giuliano, F. Neurophysiology of erection and ejaculation. J. Sex. Med. 2011, 8, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Raveendran, A.V.; Agarwal, A. Premature ejaculation-current concepts in the management: A narrative review. Int. J. Reprod. BioMedicine 2021, 19, 5. [Google Scholar] [CrossRef] [PubMed]
- Gillman, N.; Gillman, M. Premature Ejaculation: Aetiology and Treatment Strategies. Med Sci. 2019, 7, 102. [Google Scholar] [CrossRef] [Green Version]
- Wolters, J.P.; Hellstrom, W.J. Current concepts in ejaculatory dysfunction. Rev. Urol. 2006, 8, S18–S25. [Google Scholar]
- Chéhensse, C.; Facchinetti, P.; Bahrami, S.; Andrey, P.; Soler, J.-M.; Chrétien, F.; Bernabé, J.; Clément, P.; Denys, P.; Giuliano, F. Human spinal ejaculation generator. Ann. Neurol. 2016, 81, 35–45. [Google Scholar] [CrossRef]
- Özdemir, O. Is premature ejaculation an impulse control disorder? Med. Hypotheses 2012, 79, 59–62. [Google Scholar] [CrossRef]
- lthof, S.E.; McMahon, C.G.; Waldinger, M.D.; Serefoglu, E.C.; Shindel, A.W.; Adaikan, P.G.; Becher, E.; Dean, J.; Giuliano, F.; Hellstrom, W.J.; et al. An update of the International Society of Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation [PE]. J. Sex. Med. 2014, 11, 1392–1422. [Google Scholar] [CrossRef] [Green Version]
- Sansone, A.; Aversa, A.; Corona, G.; Fisher, A.D.; Isidori, A.M.; La Vignera, S.; Limoncin, E.; Maggi, M.; Merico, M.; Jannini, E.A. Management of premature ejaculation: A clinical guideline from the Italian Society of Andrology and Sexual Medicine (SIAMS). J. Endocrinol. Investig. 2021, 44, 1103–1118. [Google Scholar] [CrossRef]
- Stoléru, S.; Mouras, H. Brain Functional Imaging Studies of Sexual Desire and Arousal in Human Males. In The Psychophysiology of Sex; Janssen, E., Ed.; The Kinsey Institute for Research in Sex, Gender, and Reproduction, Inc.: Bloomington, IN, USA, 2007; p. 334. [Google Scholar]
- Park, K.; Kang, K.H.; Seo, J.J.; Kim, H.J.; Ryu, S.B.; Jeong, G.W. Blood-oxygenation-level-dependent functional magnetic resonance imaging for evaluating cerebral regions of female sexual arousal response. Urology 2001, 57, 1189–1194. [Google Scholar] [CrossRef]
- Sumich, A.; Kumari, V.; Sharma, T. Neuroimaging of sexual arousal: Research and clinical utility. Hosp. Med. 2003, 64, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Stoleru, S.; Gregoire, M.-C.; Gerard, D.; Decety, J.; Lafarge, E.; Cinotti, L.; Lavenne, F.; Le Bars, D.; Vernet-Maury, E.; Rada, H.; et al. Neuroanatomical Correlates of Visually Evoked Sexual Arousal in Human Males. Arch. Sex. Behav. 1999, 28, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Stoléru, S.; Fonteille, V.; Cornélis, C.; Joyal, C.; Moulier, V. Functional neuroimaging studies of sexual arousal and orgasm in healthy men and women: A review and meta-analysis. Neurosci. Biobehav. Rev. 2012, 36, 1481–1509. [Google Scholar] [CrossRef] [PubMed]
- Georgiadis, J.R.; Kringelbach, M.L.; Pfaus, J.G. Sex for fun: A synthesis of human and animal neurobiology. Nat. Rev. Urol. 2012, 9, 486–498. [Google Scholar] [CrossRef]
- Murray, L.; Waller, R.; Hyde, L.W. A systematic review examining the link between psychopathic personality traits, antisocial behavior, and neural reactivity during reward and loss processing. Pers. Disord. Theory Res. Treat. 2018, 9, 497–509. [Google Scholar] [CrossRef]
- Goldstein, R.Z.; Volkow, N.D. Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. Nat. Rev. Neurosci. 2011, 12, 652–669. [Google Scholar] [CrossRef] [Green Version]
- Golec, K.; Draps, M.; Stark, R.; Pluta, A.; Gola, M. Aberrant orbitofrontal cortex reactivity to erotic cues in Compulsive Sexual Behavior Disorder. J. Behav. Addict. 2021, 10, 646–656. [Google Scholar] [CrossRef]
- Gola, M.; Draps, M. Ventral Striatal Reactivity in Compulsive Sexual Behaviors. Front. Psychiatry 2018, 9, 546. [Google Scholar] [CrossRef] [Green Version]
- Kowalewska, E.; Grubbs, J.B.; Potenza, M.N.; Gola, M.; Draps, M.; Kraus, S.W. Neurocognitive Mechanisms in Compulsive Sexual Behavior Disorder. Curr. Sex. Heal. Rep. 2018, 10, 255–264. [Google Scholar] [CrossRef]
- Georgiadis, J.; Kringelbach, M. The human sexual response cycle: Brain imaging evidence linking sex to other pleasures. Prog. Neurobiol. 2012, 98, 49–81. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wells, G.; Shea, B.; O‘Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. NewcastleOttawa Quality Assessment Scale Cohort Studies. 2020. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.Asp (accessed on 15 September 2020).
- Albajes-Eizagirre, A.; Solanes, A.; Vieta, E.; Radua, J. Voxel-based meta-analysis via permutation of subject images (PSI): Theory and implementation for SDM. NeuroImage 2019, 186, 174–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radua, J.; Mataix-Cols, D. Meta-analytic methods for neuroimaging data explained. Biol. Mood Anxiety Disord. 2012, 2, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radua, J.; Mataix-Cols, D.; Phillips, M.L.; El-Hage, W.; Kronhaus, D.M.; Cardoner, N.; Surguladze, S. A new meta-analytic method for neuroimaging studies that combines reported peak coordinates and statistical parametric maps. Eur. Psychiatry 2012, 27, 605611. [Google Scholar] [CrossRef]
- Eradua, J.; Erubia, K.; Canales-Rodríguez, E.J.; Epomarol-Clotet, E.; Efusar-Poli, P.; Emataix-Cols, D. Anisotropic Kernels for Coordinate-Based Meta-Analyses of Neuroimaging Studies. Front. Psychiatry 2014, 5, 13. [Google Scholar] [CrossRef] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Zung, W.W. A rating instrument for anxiety disorders. Psychosomatics 1971, 371, 10. [Google Scholar] [CrossRef]
- Zung, W.W. A Self-Rating Depression Scale. Arch. Gen. Psychiatry 1965, 12, 63–70. [Google Scholar] [CrossRef]
- Rosen, R.C.; Riley, A.; Wagner, G.; Osterloh, I.H.; Kirkpatrick, J.; Mishra, A. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology 1997, 49, 822–830. [Google Scholar] [CrossRef] [Green Version]
- Rosen, R.; Cappelleri, J.; Smith, M.D.; Lipsky, J.; Peña, B. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int. J. Impot. Res. 1999, 11, 319–326. [Google Scholar] [CrossRef]
- Waldinger, M.D.; Hengeveld, M.; Zwinderman, A.H.; Olivier, B. An empirical operationalization study of DSM-IV diagnostic criteria for premature ejaculation. Int. J. Psychiatry Clin. Pract. 1998, 2, 287–293. [Google Scholar] [CrossRef]
- Symonds, T.; Perelman, M.A.; Althof, S.; Giuliano, F.; Martin, M.; May, K.; Abraham, L.; Crossland, A.; Morris, M. Development and Validation of a Premature Ejaculation Diagnostic Tool. Eur. Urol. 2007, 52, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Cera, N.; Castelhano, J.; Oliveira, C.; Carvalho, J.; Gomes, A.L.Q.; Peixoto, M.M.; Pereira, R.; Janssen, E.; Castelo-Branco, M.; Nobre, P. The role of anterior and posterior insula in male genital response and in visual attention: An exploratory multimodal fMRI study. Sci. Rep. 2020, 10, 18463. [Google Scholar] [CrossRef] [PubMed]
- Duerden, E.G.; Arsalidou, M.; Lee, M.; Taylor, M.J. Lateralization of affective processing in the insula. NeuroImage 2013, 78, 159–175. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, R.P.; Kumaran, A.K. The Association of Anxiety with the Subtypes of Premature Ejaculation: A Chart Review. Prim. Care Companion CNS Disord. 2014, 16, 26666. [Google Scholar] [CrossRef] [Green Version]
- Mourikis, I.; Antoniou, M.; Matsouka, E.; Vousoura, E.; Tzavara, C.; Ekizoglou, C.; Papadimitriou, G.N.; Vaidakis, N.; Zervas, I.M. Anxiety and depression among Greek men with primary erectile dysfunction and premature ejaculation. Ann. Gen. Psychiatry 2015, 14, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Crespi, B.J. Oxytocin, testosterone, and human social cognition. Biol. Rev. 2015, 91, 390–408. [Google Scholar] [CrossRef]
- Hull, E.M.; Lorrain, D.S.; Du, J.; Matuszewich, L.; A Lumley, L.; Putnam, S.K.; Moses, J. Hormone-neurotransmitter interactions in the control of sexual behavior. Behav. Brain Res. 1999, 105, 105–116. [Google Scholar] [CrossRef]
- Graziottin, A. Sexual arousal: Similarities and differences between men and women. J. Men’s Health Gend. 2004, 1, 215–223. [Google Scholar] [CrossRef]
- Baskerville, T.; Douglas, A. Interactions between dopamine and oxytocin in the control of sexual behaviour. Prog. Brain Res. 2008, 170, 277–290. [Google Scholar] [CrossRef]
- Rolls, E.T.; Cheng, W.; Feng, J. The orbitofrontal cortex: Reward, emotion and depression. Brain Commun. 2020, 2, fcaa196. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Qin, W.; Liu, H.; Fan, L.; Wang, J.; Jiang, T.; Yu, C. Subregions of the human superior frontal gyrus and their connections. NeuroImage 2013, 78, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, S.J.; Spengler, S.; Simons, J.S.; Steele, J.D.; Lawrie, S.M.; Frith, C.D.; Burgess, P.W. Functional Specialization within Rostral Prefrontal Cortex (Area 10): A Meta-analysis. J. Cogn. Neurosci. 2006, 18, 932–948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Argembeau, A.; Ruby, P.; Collette, F.; Degueldre, C.; Balteau, E.; Luxen, A.; Maquet, P.; Salmon, E. Distinct Regions of the Medial Prefrontal Cortex Are Associated with Self-referential Processing and Perspective Taking. J. Cogn. Neurosci. 2007, 19, 935–944. [Google Scholar] [CrossRef]
- Seidel, E.-M.; Pfabigan, D.M.; Hahn, A.; Sladky, R.; Grahl, A.; Paul, K.; Kraus, C.; Küblböck, M.; Kranz, G.S.; Hummer, A.; et al. Uncertainty during pain anticipation: The adaptive value of preparatory processes. Hum. Brain Mapp. 2015, 36, 744–755. [Google Scholar] [CrossRef]
- Simmons, A.; Strigo, I.; Matthews, S.C.; Paulus, M.P.; Stein, M.B. Anticipation of Aversive Visual Stimuli Is Associated with Increased Insula Activation in Anxiety-Prone Subjects. Biol. Psychiatry 2006, 60, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, R.P.; Kirlic, N.; Misaki, M.; Bodurka, J.; Rhudy, J.L.; Paulus, M.P.; Drevets, W.C. Increased anterior insula activity in anxious individuals is linked to diminished perceived control. Transl. Psychiatry 2015, 5, e591. [Google Scholar] [CrossRef] [Green Version]
- Lee, T.M.; Chan, C.C.; Han, S.-H.; Leung, A.W.; Fox, P.T.; Gao, J.-H. An event-related fMRI study on risk taking by healthy individuals of high or low impulsiveness. Neurosci. Lett. 2008, 438, 138–141. [Google Scholar] [CrossRef]
- Rodriguez, G.; Sack, A.T.; Dewitte, M.; Schuhmann, T. Inhibit My Disinhibition: The Role of the Inferior Frontal Cortex in Sexual Inhibition and the Modulatory Influence of Sexual Excitation Proneness. Front. Hum. Neurosci. 2018, 12, 300. [Google Scholar] [CrossRef] [Green Version]
- Deng, W.; Rolls, E.T.; Ji, X.; Robbins, T.; Banaschewski, T.; Bokde, A.L.; Bromberg, U.; Buechel, C.; Desrivières, S.; Conrod, P.; et al. Separate neural systems for behavioral change and for emotional responses to failure during behavioral inhibition. Hum. Brain Mapp. 2017, 38, 3527–3537. [Google Scholar] [CrossRef]
- Northoff, G.; Heinzel, A.; de Greck, M.; Bermpohl, F.; Dobrowolny, H.; Panksepp, J. Selfreferential processing in our brain—A meta-analysis of imaging studies on the self. Neuroimage 2006, 31, 440–457. [Google Scholar] [CrossRef] [PubMed]
- Tops, M.; Boksem, M.A.S. A Potential Role of the Inferior Frontal Gyrus and Anterior Insula in Cognitive Control, Brain Rhythms, and Event-Related Potentials. Front. Psychol. 2011, 2, 330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oei, N.Y.L.; Rombouts, S.A.; Soeter, R.P.; van Gerven, J.M.; Both, S. Dopamine Modulates Reward System Activity During Subconscious Processing of Sexual Stimuli. Neuropsychopharmacology 2012, 37, 1729–1737. [Google Scholar] [CrossRef] [Green Version]
- Rolls, E.T. The cingulate cortex and limbic systems for emotion, action, and memory. Brain Struct. Funct. 2019, 224, 3001–3018. [Google Scholar] [CrossRef] [Green Version]
- Vogt, B.A. Pain and emotion interactions in subregions of the cingulate gyrus. Nat. Rev. Neurosci. 2005, 6, 533–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreno, S.G.; Sutton, A.J.; E Ades, A.; Stanley, T.D.; Abrams, K.R.; Peters, J.L.; Cooper, N.J. Assessment of regression-based methods to adjust for publication bias through a comprehensive simulation study. BMC Med Res. Methodol. 2009, 9, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Design | |
|
|
| Population | |
|
|
| Intervention | |
|
|
| Topic | |
|
|
| Psychogenic Erectile Dysfunction Studies | |||
|---|---|---|---|
| Source | Selection | Comparability | Exposition |
| Cera et al., 2012 | **** | ** | ** |
| Cera et al., 2014 | **** | ** | ** |
| Chen et al., 2017 | **** | ** | * |
| Jin et al., 2018 | **** | ** | ** |
| Liu et al., 2015 | **** | ** | ** |
| Montorsi et al., 2003a | *** | -- | * |
| Montorsi et al., 2003b | *** | -- | * |
| Wang et al., 2017 | **** | ** | ** |
| Yin et al., 2020 | **** | ** | *** |
| Premature Ejaculation Studies | |||
| Source | Selection | Comparability | Exposition |
| Chen et al., 2020a | **** | ** | ** |
| Chen et al., 2020b | **** | ** | *** |
| Gao et al., 2020a | *** | ** | *** |
| Gao et al., 2020b | *** | ** | ** |
| Geng et al., 2021 | *** | ** | ** |
| Lu et al., 2018 | *** | ** | *** |
| Xu et al., 2019 | *** | ** | *** |
| Yang et al., 2018 | *** | ** | *** |
| Zhang et al., 2017 | *** | ** | ** |
| Zhang et al., 2020 | **** | ** | ** |
| Source | Nr. Participants | Age | Diagnostic Criteria | Clinical Interview | Psychological Assessment (Tests) | Uro-Andrologic Assessment | Tasks |
|---|---|---|---|---|---|---|---|
| § Cera et al., 2012 | PED:17 HC: 19 | PED: M = 34.3; SD = 11 HC: M = 33.6; SD = 11.5 | DSM-IV | MINI | IIEF; SAI; SCL-90-R; STAI;BIS/BAS scale | Yes | VSS |
| § Cera et al., 2014 | PED:16 HC: 19 | PED: M = 33.4; SD = 10.7 HC: M = 33.5; SD = 11.4 | DSM-IV | MINI | IIEF; SAI; SCL-90-R; STAI;BIS/BAS scale | Yes | Long VSS |
| § Chen et al., 2017 | PED:24 HC: 26 | PED: M = 29.8; SD = 4.62 HC: M = 32.81; SD = 8.38 | Medical Clinical anamnesis. | IIEF; HAM-A; HAM-D | Yes | Resting state | |
| § Jin et al., 2018 | PED: 26 HC: 26 | PED: M = 26.8; SD = 5 HC: M = 28.5; SD = 3.2 | Neuropsychiatric anamnesis; Sexual/psychosocial interview | IIEF;SAS;SDS | Yes | Resting state | |
| § Liu et al., 2015 | PED: 27 HC: 27 | PED: M = 33.22; SD = 5.92 HC: M = 31.41; SD = 5.82 | Medical Clinical anamnesis | IIEF; QEQ; SEARQ | Yes | Resting state | |
| § Montorsi et al., 2003 | PED:8 HC: 4 | PED: M = 43; SD = N/A HC: M = 25; SD = N/A | Neuropsychiatric anamnesis; | N/A | Yes | VSS | |
| § Montorsi et al., 2003 | PED:8 HC: 4 | PED: M = 49; SD = N/A HC: M = 25; SD = N/A | Neuropsychiatric anamnesis; | N/A | Yes | VSS | |
| § Wang et al., 2017 | PED: 27 HC: 27 | PED:M = 26.58; SD = 4.89 HC: M = 28.39; SD = 3.53 | DSM-5 | Neuropsychiatric anamnesis; Sexual/psychosocial interview | IIEF; SAS; SDS | Yes | Resting state |
| § Yin et al., 2020 | PED: 31 HC: 24 | PED: M = 13.97; SD = 3.6 HC: M = 22.21; SD = 0.98 | Neuropsychiatric anamnesis; Sexual/psychosocial interview | IIEF; QEQ; SEARQ; SAS; SDS | Yes | Resting state | |
| ♦Chen et al., 2020 | PE:17 HC:23 | PE: M = 22.88; SD = 0.99; HC: M = 23.26; SD = 0.81 | Medical Clinical anamnesis. | IIEF; IELT; PEDT | N/A | Resting state | |
| ♦Chen et al., 2021 | PE:17 HC:24 | PE:M = 21.47; SD = 0.62; HC: M = 21.72; SD = 0.74 | Medical Clinical anamnesis. | IIEF-5; PEDT | N/A | Resting state | |
| ♦Gao et al., 2020(a) | PE:47 HC: 30 | PE:M = 31.3; SD = 4.83 HC: M = 31.10; SD = 2.88 | Medical Clinical anamnesis | IIEF-5; IELT PEDT; SAS; SDS | N/A | Resting state | |
| ♦Gao et al., 2020(b) | PE:45 HC: 37 | PE:M = 30.90; SD = 5.31 HC:M = 30.84; SD = 3.23 | Medical Clinical anamnesis | IIEF-5; IELT PEDT; SAS; SDS | N/A | Resting state | |
| ♦Geng et al., 2021 | PE: 44 HC: 31 | PE: M = 23.95; SD = 0.11 HC: M = 24.29; SD = 0.24 | Medical Clinical anamnesis | IIEF-5; IELT; SAS; SDS | N/A | Resting state | |
| ♦Lu et al., 2018 | PE:20 HC:15 | PE:M = 27.95; SD = 4.52 HC: M = 27.87; SD = 3.78 | IIEF-5; IELT; CIPE-5 | N/A | Resting state | ||
| ♦Xu et al., 2019 | PE:20 HC:15 | PE:M = 30.52; SD = 5.06 HC: M = 31.33; SD = 2.77 | IIEF-5; IELT PEDT; | N/A | Resting state | ||
| ♦Yang et al., 2018 | PE:20 HC:15 | PE:M = 30.52; SD = 5.06 HC: M = 31.33; SD = 2.77 | IIEF-5; IELT PEDT; | N/A | Resting state | ||
| ♦Zang et al., 2017 | PE:20 HC:15 | PE:M = 27.95; SD = 4.52 HC: M = 27.87; SD = 3.78 | IIEF-5; IELT; CIPE-5 | Yes | VSS Resting state | ||
| ♦Zhang et al., 2020 | PE:25 HC:21 | PE:M = 30.44; SD = 5.59 HC: M = 32.29; SD = 6.60 | PEDT; BDI | N/A | Resting state |
| Cluster | Hemisphere | Coordinates (X, Y, Z) | Z Values | p Values | Nr. Voxels | BA |
|---|---|---|---|---|---|---|
| Global Map: Blobs ≥ 234 voxels Z ≥ 2.576; peaks Z ≥ 3.142. | ||||||
| Anterior Prefrontal cortex | L | 0, 52, 13 | 3.996 | 0.000 | 234 | 10 |
| Anterior Prefrontal cortex | R | −4, 28, −10 | 3.142 | 0.000 | 305 | 11 |
| Global Map: Blobs ≥ 3 voxels Z ≤ −2.577; Peaks Z ≤ −2.711 | ||||||
| Posterior insula/claustrum | L | −34, −7, 10 | −3.442 | 0.000 | 176 | 13 |
| Inferior frontal gyrus (Broca’s Area) | R | 43, 10, 11 | −3.292 | 0.000 | 53 | 44 |
| Inferior frontal gyrus, pars triangularis | L | −51, 34, 9 | −2.732 | 0.003 | 16 | 45 |
| Dorsal anterior cingulate cortex | R | 6, 0, 37 | −2.856 | 0.002 | 13 | 24 |
| Anterior prefrontal cortex | R | 19, 57, −6 | −3.078 | 0.001 | 12 | 10 |
| Task Map: Blobs ≥ 215 voxels Z ≥ 2.577; peaks Z ≥ 3.611. | ||||||
| Anterior prefrontal cortex/ Ventromedial Prefrontal cortex | L | −2, 52, 17 | 3.611 | 0.000 | 215 | 10 |
| Resting-State Map: Blobs ≥ 45 voxels Z ≤ −2.576; peaks Z ≤ −3.417 | ||||||
| Insula | R | 47, 6, 0 | −5.504 | 0.000 | 1678 | 13 |
| Insula | L | −36, −7, 8 | −4.245 | 0.000 | 404 | 13 |
| Temporal pole | L | −41, 11, −12 | −3.560 | 0.000 | 109 | 38 |
| Anterior Prefrontal cortex | R | 19, 57, 0 | −3.417 | 0.000 | 45 | 10 |
| PED Map: Blobs ≥ 1 voxel Z ≥ 2.578; peaks Z ≥ 2.599. | ||||||
| Anterior Prefrontal cortex | L | −2, 52, 13 | 3.253 | 0.000 | 122 | 10 |
| Orbitofrontal cortex | L | −6, 27, −12 | 2.909 | 0.001 | 39 | 11 |
| Anterior insula | L | −40, 12, 1 | 2.864 | 0.002 | 22 | 13 |
| Anterior Prefrontal cortex | L | −2, 55, 22 | 2.643 | 0.004 | 2 | 10 |
| Ventromedial Prefrontal cortex | L | −8, 20, −9 | 2.599 | 0.004 | 2 | 25 |
| PE Map: Blobs ≥ 54 voxels Z ≤ 2.579; peaks Z ≤ −3.279 | ||||||
| Posterior cingulate cortex/retrosplenial cortex | R | 0, −38, 36 | 3.279 | 0.000 | 54 | 23 |
| PE Map: Blobs ≥ 256 voxels Z ≤ −2.576; peaks Z ≤ −3.718 | ||||||
| Anterior insula | R | 45, 8, −6 | −5.102 | 0.000 | 849 | 13 |
| Posterior insula | L | −40, −6, 6 | −4.685 | 0.000 | 583 | 13 |
| Orbital part of inferior frontal gyrus | L | −39, 13, −9 | −4.520 | 0.000 | 453 | 47 |
| Orbital part of inferior frontal gyrus | L | −49, 33, 2 | −3.528 | 0.000 | 195 | 47 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monteiro, J.; Castelhano, J.; Pignatelli, D.; Tartaro, A.; Cera, N. Do Psychogenic Erectile Dysfunction and Premature Ejaculation Share a Neural Circuit? Evidence from a fMRI Systematic Review and Meta-Analysis. Appl. Sci. 2022, 12, 11249. https://doi.org/10.3390/app122111249
Monteiro J, Castelhano J, Pignatelli D, Tartaro A, Cera N. Do Psychogenic Erectile Dysfunction and Premature Ejaculation Share a Neural Circuit? Evidence from a fMRI Systematic Review and Meta-Analysis. Applied Sciences. 2022; 12(21):11249. https://doi.org/10.3390/app122111249
Chicago/Turabian StyleMonteiro, Jéssica, João Castelhano, Duarte Pignatelli, Armando Tartaro, and Nicoletta Cera. 2022. "Do Psychogenic Erectile Dysfunction and Premature Ejaculation Share a Neural Circuit? Evidence from a fMRI Systematic Review and Meta-Analysis" Applied Sciences 12, no. 21: 11249. https://doi.org/10.3390/app122111249
APA StyleMonteiro, J., Castelhano, J., Pignatelli, D., Tartaro, A., & Cera, N. (2022). Do Psychogenic Erectile Dysfunction and Premature Ejaculation Share a Neural Circuit? Evidence from a fMRI Systematic Review and Meta-Analysis. Applied Sciences, 12(21), 11249. https://doi.org/10.3390/app122111249







