A Systematic Review of Positional Plagiocephaly Prevention Methods for Patients in Development
Abstract
1. Introduction
- (1)
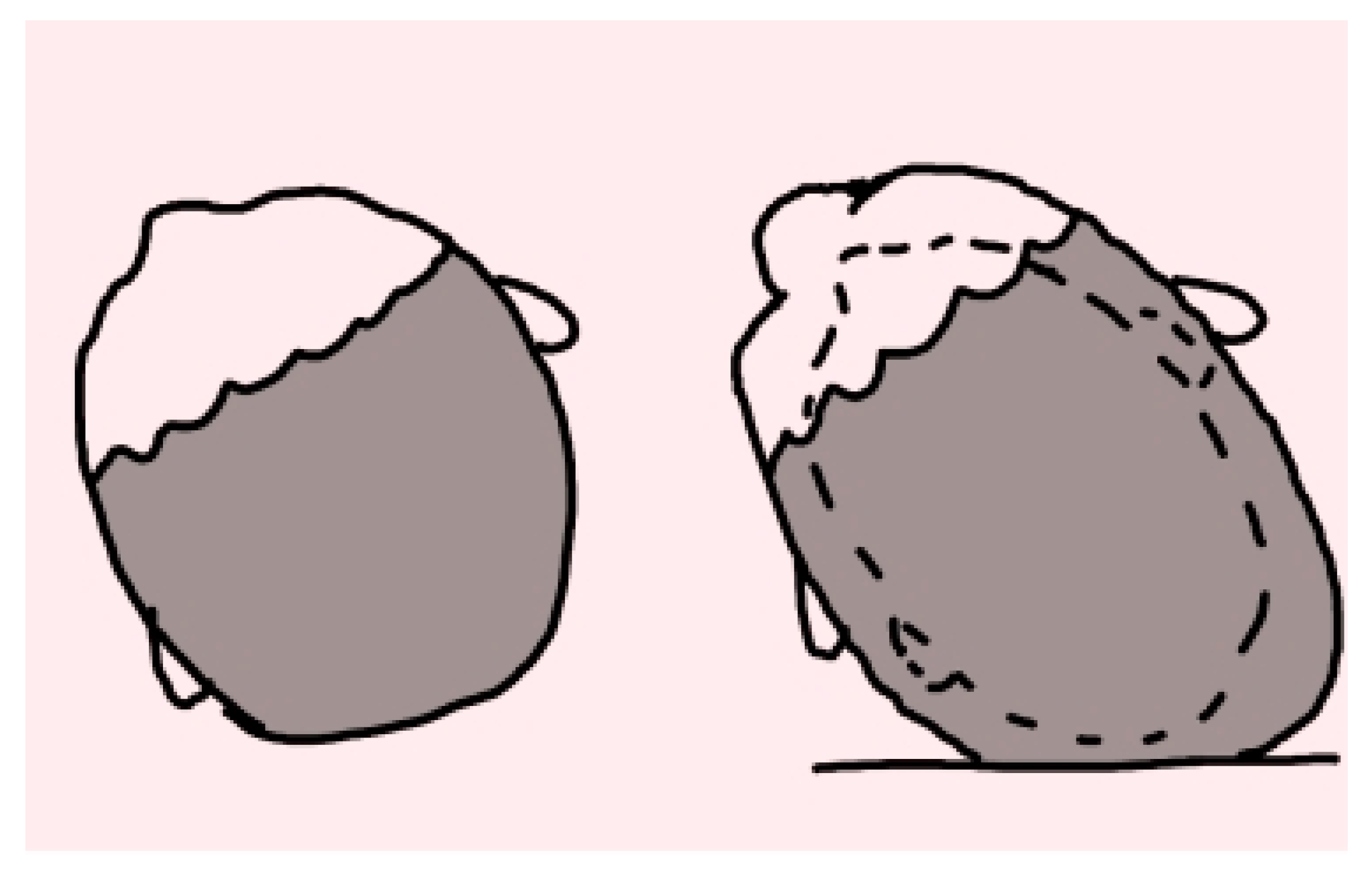
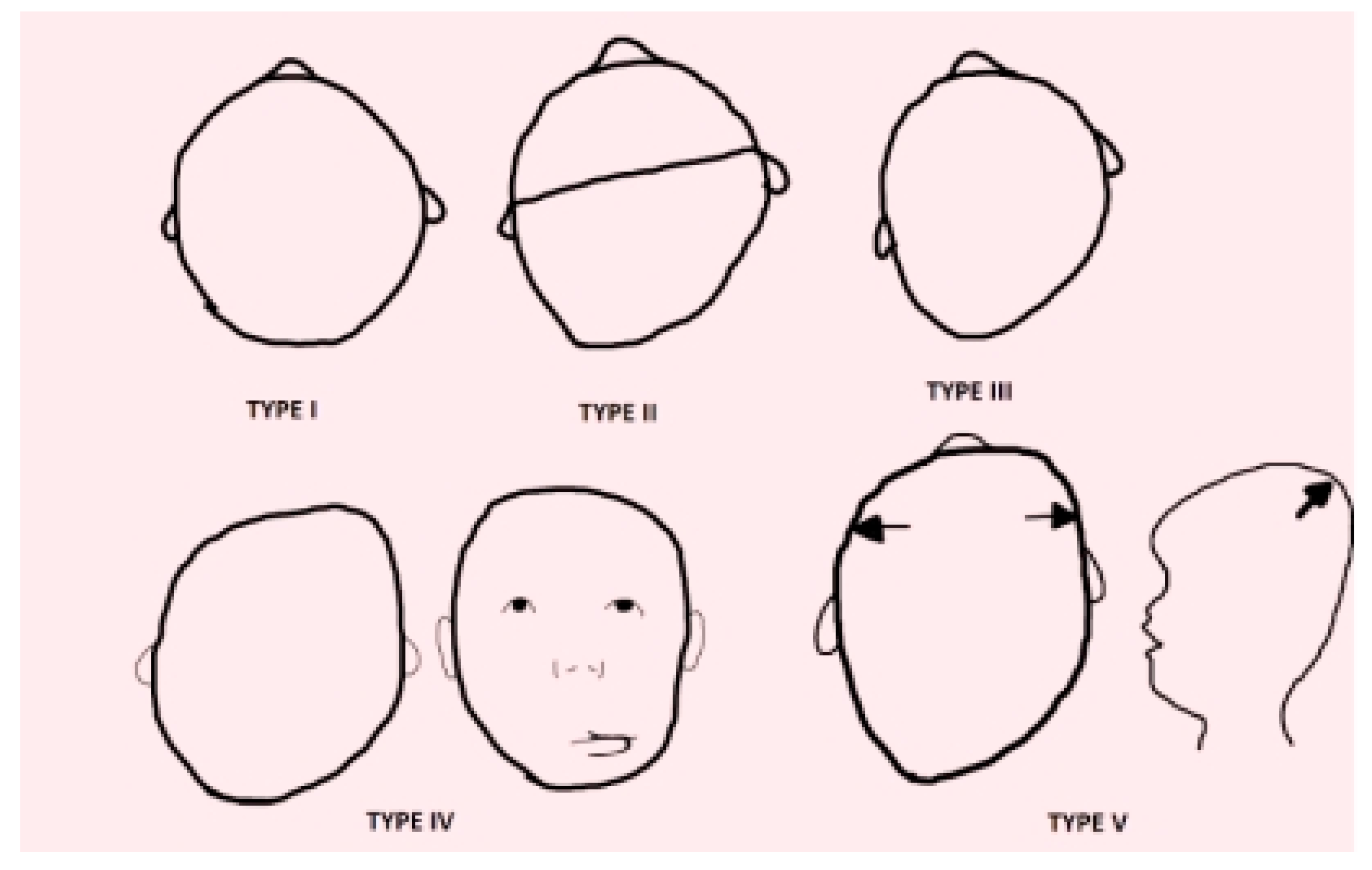
- Type I PP (PPI), the mildest form, in which asymmetry is present only in the back of the skull and whose depression may vary. There are no positional asymmetries at the ears level, deformities in the frontal region, or vertical changes (elongations) of the face.
- (2)
- Type II PP (PPII), a more advanced form of PP, in which various levels of posterior cranial asymmetry with involvement of the skull base and temporal fossa are recognized. The ear of the affected side is located forward and/or downward (visible when looking at the infant’s skull from above). The frontal squama (symmetrical forehead) is not involved. There is no facial asymmetry or vertical (compressive) changes in the skull.
- (3)
- Type III PP (PPIII), characterized by the typical parallelogram shape of the skull. There is posterior cranial deformation, changing of the ear from the affected part, and involvement of the frontal squama ipsilateral to the depression with a prominence of the same (visible from above). The face appears symmetrical.
- (4)
- Type IV PP (PPIV), characterized by posterior cranial deformity associated with facial asymmetry, frontal and ear swiveling ipsilateral to the cranial depression. Hyperplasia of the zygomatic process (less frequent) and displacement of cheek adipose tissue due to the progression of cranial deformation result in facial asymmetry.
- (5)
- Type V PP (PPV) in which, in addition to posterior cranial deformity associated with facial asymmetry, frontal and ear slippage ipsilateral to cranial depression, in the occipitoparietal area, there is altered vertical growth of the skull, as well as a protrusion in the temporal area [39].
2. Materials and Methods
2.1. Search Processing
2.2. Inclusion Criteria
2.3. Data Processing
3. Results
Characteristics of Included Articles
4. Discussion
4.1. Cranial Conformation-Related Positional Plagiocephaly
4.2. Prevention of Positional Plagiocephaly and Risk Factors
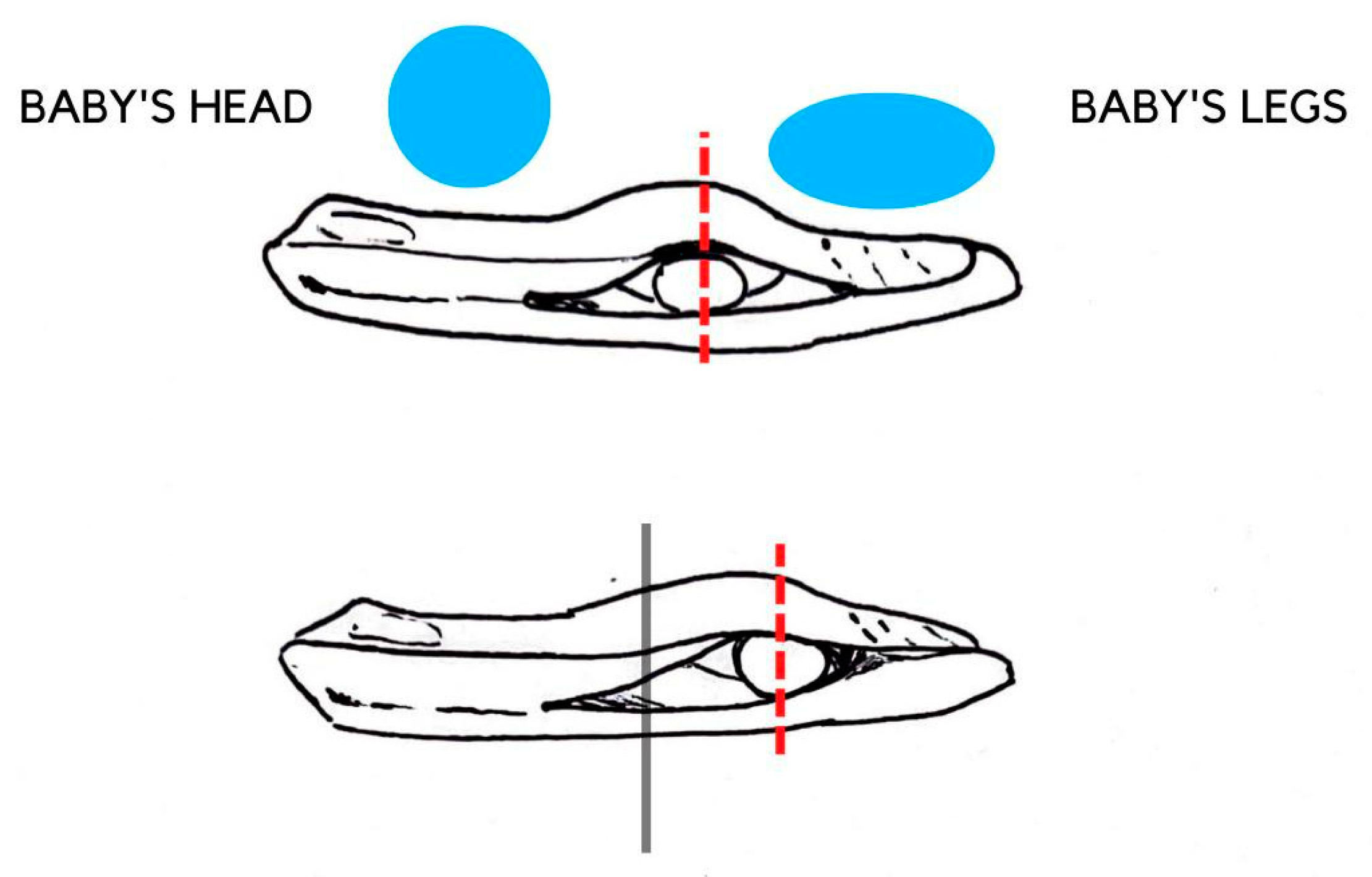
4.3. Positional Plagiocephaly and Mattress
4.4. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 3D | Three-Dimensional. |
| AAP | American Academy of Pediatrics. |
| AC | Asymmetry Of Cranium. |
| CA | Corrected Age. |
| CC | Cranial Circumference. |
| CI | Cephalic Index. |
| Crl | Cranial Length. |
| Crv | Cranial Volume. |
| Crw | Cranial Width. |
| CVA | Cranial Vault Asymmetry. |
| CVAI | Cranial Vault Asymmetry Index. |
| DB | Deformative Brachycephaly. |
| HT | Helmet Therapy. |
| LWR | Cranial Length–Width Ratio. |
| PP | Positional Plagiocephaly. |
| PPI | Positional Plagiocephaly Type I. |
| PPII | Positional Plagiocephaly Type II. |
| PPIII | Positional Plagiocephaly Type III. |
| PPIV | Positional Plagiocephaly Type IV. |
| PPV | Positional Plagiocephaly Type V. |
| PT | Positioning Therapy. |
| SE | Sellion. |
| SIDS | Sudden Infant Death Syndrome. |
| TAA | Thoraco-abdominal Asynchrony. |
| TEA | Term-Equivalent Age. |
| TR | Tragus Landmark. |
| ULS | Unilateral Lambdoid Synostosis. |
References
- Bruneteau, R.J.; Mulliken, J.B. Frontal Plagiocephaly: Synostotic, Compensational, or Deformational. Plast. Reconstr. Surg. 1992, 89, 21–31; discussion 32–33. [Google Scholar] [CrossRef] [PubMed]
- Naros, A.; Wolf, J.A.; Krimmel, M.; Kluba, S. Three-Dimensional Quantification of Facial Asymmetry in Children with Positional Cranial Deformity. Plast. Reconstr. Surg. 2021, 148, 1321–1331. [Google Scholar] [CrossRef]
- Hansen, M.; Mulliken, J.B. Frontal Plagiocephaly. Diagnosis and Treatment. Clin. Plast. Surg. 1994, 21, 543–553. [Google Scholar] [CrossRef]
- Marinelli, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Limongelli, L.; Montenegro, V.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; et al. White Spot Lesions in Orthodontics: Prevention and Treatment. A Descriptive Review. J. Biol. Regul. Homeost. Agents 2021, 35, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Knight, S. Positional Plagiocephaly/Brachycephaly Is Associated with Later Cognitive and Academic Outcomes. J. Pediatr. 2019, 210, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Ruiz Colón, G.D.; Jin, M.C.; Grant, G.A.; Prolo, L.M. Increased Utilization of Healthcare Services in Children with Craniosynostosis. J. Neurosurg. Pediatr. 2022, 30, 52–59. [Google Scholar] [CrossRef]
- Park, K.M.; Tripathi, N.V.; Mufarrej, F.A. Quality of Life in Patients with Craniosynostosis and Deformational Plagiocephaly: A Systematic Review. Int. J. Pediatr. Otorhinolaryngol. 2021, 149, 110873. [Google Scholar] [CrossRef]
- Klausing, A.; Röhrig, A.; Lüchters, G.; Vogler, H.; Martini, M. Follow-up Study to Investigate Symmetry and Stability of Cranioplasty in Craniosynostosis—Introduction of New Pathology-Specific Parameters and a Comparison to the Norm Population. J. Craniomaxillofac Surg. 2019, 47, 1441–1448. [Google Scholar] [CrossRef]
- Haas-Lude, K.; Wolff, M.; Will, B.; Bender, B.; Krimmel, M. Clinical and Imaging Findings in Children with Non-Syndromic Lambdoid Synostosis. Eur. J. Pediatr. 2014, 173, 435–440. [Google Scholar] [CrossRef]
- Smartt, J.M.; Reid, R.R.; Singh, D.J.; Bartlett, S.P. True Lambdoid Craniosynostosis: Long-Term Results of Surgical and Conservative Therapy. Plast. Reconstr. Surg. 2007, 120, 993–1003. [Google Scholar] [CrossRef]
- Reardon, T.; Fiani, B.; Kosarchuk, J.; Parisi, A.; Shlobin, N.A. Management of Lambdoid Craniosynostosis: A Comprehensive and Systematic Review. Pediatr. Neurosurg. 2022, 57, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Dias, M.S.; Klein, D.M.; Backstrom, J.W. Occipital Plagiocephaly: Deformation or Lambdoid Synostosis? I. Morphometric Analysis and Results of Unilateral Lambdoid Craniectomy. Pediatr. Neurosurg. 1996, 24, 61–68. [Google Scholar] [CrossRef]
- De Bock, F.; Braun, V.; Renz-Polster, H. Deformational Plagiocephaly in Normal Infants: A Systematic Review of Causes and Hypotheses. Arch. Dis. Child. 2017, 102, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Cabrera-Martos, I.; Valenza, M.C.; Benítez-Feliponi, A.; Robles-Vizcaíno, C.; Ruiz-Extremera, A.; Valenza-Demet, G. Clinical Profile and Evolution of Infants with Deformational Plagiocephaly Included in a Conservative Treatment Program. Childs Nerv. Syst. 2013, 29, 1893–1898. [Google Scholar] [CrossRef] [PubMed]
- Adina, S.; Dipalma, G.; Bordea, I.R.; Lucaciu, O.; Feurdean, C.; Inchingolo, A.D.; Septimiu, R.; Malcangi, G.; Cantore, S.; Martin, D.; et al. Orthopedic Joint Stability Influences Growth and Maxillary Development: Clinical Aspects. J. Biol. Regul. Homeost. Agents 2020, 34, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Enlow, D.H.; Moyers, R.E.; Merow, W.W. Handbook of Facial Growth; Saunders: Philadelphia, PA, USA, 1982; ISBN 978-0-7216-3386-2. [Google Scholar]
- Patano, A.; Cirulli, N.; Beretta, M.; Plantamura, P.; Inchingolo, A.D.; Inchingolo, A.M.; Bordea, I.R.; Malcangi, G.; Marinelli, G.; Scarano, A.; et al. Education Technology in Orthodontics and Paediatric Dentistry during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6056. [Google Scholar] [CrossRef] [PubMed]
- Dimonte, M.; Inchingolo, F.; Minonne, A.; Arditi, G.; Dipalma, G. Bone SPECT in Management of Mandibular Condyle Hyperplasia. Report of a Case and Review of Literature. Minerva Stomatol. 2004, 53, 281–285. [Google Scholar]
- Hide, T. Dysmorphies Cranio-Faciales. Les Synostoses Prematures (Craniostenoses et Faciostenoses). J. Neurol. Neurosurg. Psychiatry 1978, 41, 387–388. [Google Scholar] [CrossRef]
- Collett, B.; Breiger, D.; King, D.; Cunningham, M.; Speltz, M. Neurodevelopmental Implications of “Deformational” Plagiocephaly. J. Dev. Behav. Pediatr. 2005, 26, 379–389. [Google Scholar] [CrossRef]
- Montenegro, V.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Compliance of Children with Removable Functional Appliance with Microchip Integrated during Covid-19 Pandemic: A Systematic Review. J. Biol. Regul. Homeost. Agents 2021, 35, 365–377. [Google Scholar] [CrossRef]
- Cirulli, N.; Ballini, A.; Cantore, S.; Farronato, D.; Inchingolo, F.; Dipalma, G.; Gatto, M.R.; Alessandri Bonetti, G. Mixed dentition space analysis of a southern italian population: New regression equations for unerupted teeth. J. Biol. Regul. Homeost. Agents 2015, 29, 515–520. [Google Scholar]
- Dunn, P.M. Congenital Postural Deformities. Br. Med. Bull. 1976, 32, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Pede, C.D.; et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. Int. J. Environ. Res. Public Health 2022, 19, 988. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Palmieri, G.; et al. Genetic Pattern, Orthodontic and Surgical Management of Multiple Supplementary Impacted Teeth in a Rare, Cleidocranial Dysplasia Patient: A Case Report. Medicina 2021, 57, 1350. [Google Scholar] [CrossRef] [PubMed]
- Mawji, A.; Vollman, A.R.; Fung, T.; Hatfield, J.; McNeil, D.A.; Sauvé, R. Risk Factors for Positional Plagiocephaly and Appropriate Time Frames for Prevention Messaging. Paediatr. Child Health 2014, 19, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Cappella, A.; Dolci, C.; Cagetti, M.G.; Inchingolo, F.; Sforza, C. Is Orthodontic Treatment with Microperforations Worth It? A Scoping Review. Children 2022, 9, 208. [Google Scholar] [CrossRef] [PubMed]
- Malcangi, G.; Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Garibaldi, M.; Inchingolo, A.M.; Piras, F.; Cardarelli, F.; Settanni, V.; et al. Impacted Central Incisors in the Upper Jaw in an Adolescent Patient: Orthodontic-Surgical Treatment—A Case Report. Appl. Sci. 2022, 12, 2657. [Google Scholar] [CrossRef]
- Turk, A.E.; McCarthy, J.G.; Thorne, C.H.; Wisoff, J.H. The “Back to Sleep Campaign” and Deformational Plagiocephaly: Is There Cause for Concern? J. Craniofac. Surg. 1996, 7, 12–18. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ceci, S.; Patano, A.; Inchingolo, A.M.; Montenegro, V.; Di Pede, C.; Malcangi, G.; Marinelli, G.; Coloccia, G.; Garibaldi, M.; et al. Elastodontic Therapy of Hyperdivergent Class II Patients Using AMCOP® Devices: A Retrospective Study. Appl. Sci. 2022, 12, 3259. [Google Scholar] [CrossRef]
- American Academy of Pediatrics AAP Task Force on Infant Positioning and SIDS: Positioning and SIDS. Pediatrics 1992, 89, 1120–1126. [CrossRef]
- Argenta, L.C.; David, L.R.; Wilson, J.A.; Bell, W.O. An Increase in Infant Cranial Deformity with Supine Sleeping Position. J. Craniofac. Surg. 1996, 7, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Kane, A.A.; Mitchell, L.E.; Craven, K.P.; Marsh, J.L. Observations on a Recent Increase in Plagiocephaly without Synostosis. Pediatrics 1996, 97, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Mulliken, J.B.; Vander Woude, D.L.; Hansen, M.; LaBrie, R.A.; Scott, R.M. Analysis of Posterior Plagiocephaly: Deformational versus Synostotic. Plast. Reconstr. Surg. 1999, 103, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Beuriat, P.-A.; Szathmari, A.; Di Rocco, F.; Mottolese, C. Deformational Plagiocephaly: State of the Art and Review of the Literature. Neurochirurgie 2019, 65, 322–329. [Google Scholar] [CrossRef]
- Filisetti, M.; Cattarelli, D.; Bonomi, S. Positional Plagiocephaly from Structure to Function: Clinical Experience of the Service of Pediatric Osteopathy in Italy. Early Hum. Dev. 2020, 146, 105028. [Google Scholar] [CrossRef]
- Peitsch, W.K.; Keefer, C.H.; LaBrie, R.A.; Mulliken, J.B. Incidence of Cranial Asymmetry in Healthy Newborns. Pediatrics 2002, 110, e72. [Google Scholar] [CrossRef]
- Dec, W.; Warren, S.M. Current Concepts in Deformational Plagiocephaly. J. Craniofac. Surg. 2011, 22, 6–8. [Google Scholar] [CrossRef]
- Mawji, A.; Vollman, A.R.; Hatfield, J.; McNeil, D.A.; Sauvé, R. The Incidence of Positional Plagiocephaly: A Cohort Study. Pediatrics 2013, 132, 298–304. [Google Scholar] [CrossRef]
- Argenta, L.; David, L.; Thompson, J. Clinical Classification of Positional Plagiocephaly. J. Craniofac. Surg. 2004, 15, 368–372. [Google Scholar] [CrossRef]
- Leung, A.Y.F.; Mandrusiak, A.; Watter, P.; Gavranich, J.; Johnston, L.M. Clinical Assessment of Head Orientation Profile Development and Its Relationship with Positional Plagiocephaly in Healthy Term Infants—A Prospective Study. Early Human Dev. 2016, 96, 31–38. [Google Scholar] [CrossRef]
- Di Venere, D.; Pettini, F.; Nardi, G.M.; Laforgia, A.; Stefanachi, G.; Notaro, V.; Rapone, B.; Grassi, F.R.; Corsalini, M. Correlation between Parodontal Indexes and Orthodontic Retainers: Prospective Study in a Group of 16 Patients. Oral Implantol. 2017, 10, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Kluba, S.; Kraut, W.; Reinert, S.; Krimmel, M. What Is the Optimal Time to Start Helmet Therapy in Positional Plagiocephaly? Plast. Reconstr. Surg. 2011, 128, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Freudlsperger, C.; Steinmacher, S.; Saure, D.; Bodem, J.P.; Kühle, R.; Hoffmann, J.; Engel, M. Impact of Severity and Therapy Onset on Helmet Therapy in Positional Plagiocephaly. J. Craniomaxillofac Surg. 2016, 44, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Di Venere, D.; Laforgia, A.; Azzollini, D.; Barile, G.; De Giacomo, A.; Inchingolo, A.D.; Rapone, B.; Capodiferro, S.; Kazakova, R.; Corsalini, M. Calcification of the Atlanto-Occipital Ligament (Ponticulus Posticus) in Orthodontic Patients: A Retrospective Study. Healthcare 2022, 10, 1234. [Google Scholar] [CrossRef]
- Wilbrand, J.-F.; Wilbrand, M.; Malik, C.Y.; Howaldt, H.-P.; Streckbein, P.; Schaaf, H.; Kerkmann, H. Complications in Helmet Therapy. J. Craniomaxillofac Surg. 2012, 40, 341–346. [Google Scholar] [CrossRef]
- Gump, W.C.; Mutchnick, I.S.; Moriarty, T.M. Complications Associated with Molding Helmet Therapy for Positional Plagiocephaly: A Review. FOC 2013, 35, E3. [Google Scholar] [CrossRef]
- Miyabayashi, H.; Nagano, N.; Kato, R.; Noto, T.; Hashimoto, S.; Saito, K.; Morioka, I. Reference Values for Cranial Morphology Based on Three-Dimensional Scan Analysis in 1-Month-Old Healthy Infants in Japan. Neurol. Med. Chir. 2022, 62, 246–253. [Google Scholar] [CrossRef]
- Yang, W.; Chen, J.; Shen, W.; Wang, C.; Wu, Z.; Chang, Q.; Li, W.; Lv, K.; Pan, Q.; Li, H.; et al. Prevalence of Positional Skull Deformities in 530 Premature Infants with a Corrected Age of up to 6 Months: A Multicenter Study. BMC Pediatr. 2019, 19, 520. [Google Scholar] [CrossRef]
- Kajita, H.; Sakamoto, Y.; Takenouchi, T.; Miwa, T.; Takahashi, T. Is That Cranial Deformity Really Due to Sleeping Position? Pediatrics Int. 2017, 59, 494–496. [Google Scholar] [CrossRef]
- Ifflaender, S.; Rüdiger, M.; Konstantelos, D.; Wahls, K.; Burkhardt, W. Prevalence of Head Deformities in Preterm Infants at Term Equivalent Age. Early Human Dev. 2013, 89, 1041–1047. [Google Scholar] [CrossRef]
- Hutchison, B.L.; Hutchison, L.A.D.; Thompson, J.M.D.; Mitchell, E.A. Plagiocephaly and Brachycephaly in the First Two Years of Life: A Prospective Cohort Study. Pediatrics 2004, 114, 970–980. [Google Scholar] [CrossRef]
- Najarian, S.P. Infant Cranial Molding Deformation and Sleep Position: Implications for Primary Care. J. Pediatr. Health Care 1999, 13, 173–177. [Google Scholar] [CrossRef]
- Yorifuji, J.; Yorifuji, T.; Tachibana, K.; Nagai, S.; Kawai, M.; Momoi, T.; Nagasaka, H.; Hatayama, H.; Nakahata, T. Craniotabes in Normal Newborns: The Earliest Sign of Subclinical Vitamin D Deficiency. J. Clin. Endocrinol. Metab. 2008, 93, 1784–1788. [Google Scholar] [CrossRef] [PubMed]
- Weernink, M.G.M.; van Wijk, R.M.; Groothuis-Oudshoorn, C.G.M.; Lanting, C.I.; Grant, C.C.; van Vlimmeren, L.A.; Boere-Boonekamp, M.M. Insufficient Vitamin D Supplement Use during Pregnancy and Early Childhood: A Risk Factor for Positional Skull Deformation: Vitamin D: A Risk Factor for Skull Deformation. Matern. Child. Nutr. 2016, 12, 177–188. [Google Scholar] [CrossRef]
- Michels, A.C.; Van Den Elzen, M.E.; Vies, J.S.H.; Van Der Hulst, R.R. Positional Plagiocephaly and Excessive Folic Acid Intake during Pregnancy. Cleft Palate-Craniofacial J. 2012, 49, 1–4. [Google Scholar] [CrossRef]
- Nuysink, J.; van Haastert, I.C.; Eijsermans, M.J.C.; Koopman-Esseboom, C.; van der Net, J.; de Vries, L.S.; Helders, P.J.M. Prevalence and Predictors of Idiopathic Asymmetry in Infants Born Preterm. Early Human Dev. 2012, 88, 387–392. [Google Scholar] [CrossRef] [PubMed]
- de Walle, H.E.K.; de Jong-van den Berg, L.T.W. Ten Years after the Dutch Public Health Campaign on Folic Acid: The Continuing Challenge. Eur. J. Clin. Pharmacol. 2008, 64, 539–543. [Google Scholar] [CrossRef]
- Littlefield, T.R.; Kelly, K.M.; Pomatto, J.K.; Beals, S.P. Multiple-Birth Infants at Higher Risk for Development of Deformational Plagiocephaly: II. Is One Twin at Greater Risk? Pediatrics 2002, 109, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, B.L.; Thompson, J.M.D.; Mitchell, E.A. Determinants of Nonsynostotic Plagiocephaly: A Case-Control Study. Pediatrics 2003, 112, e316. [Google Scholar] [CrossRef]
- van Vlimmeren, L.A.; van der Graaf, Y.; Boere-Boonekamp, M.M.; L’Hoir, M.P.; Helders, P.J.M.; Engelbert, R.H.H. Risk Factors for Deformational Plagiocephaly at Birth and at 7 Weeks of Age: A Prospective Cohort Study. Pediatrics 2007, 119, e408–e418. [Google Scholar] [CrossRef]
- McKinney, C.M.; Cunningham, M.L.; Holt, V.L.; Leroux, B.; Starr, J.R. Characteristics of 2733 Cases Diagnosed with Deformational Plagiocephaly and Changes in Risk Factors over Time. Cleft Palate-Craniofacial J. 2008, 45, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Lennartsson, F. Developing Guidelines for Child Health Care Nurses to Prevent Nonsynostotic Plagiocephaly: Searching for the Evidence. J. Pediatric Nurs. 2011, 26, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Boere-Boonekamp, M.M.; van der Linden-Kuiper, L.T. Positional Preference: Prevalence in Infants and Follow-Up After Two Years. Pediatrics 2001, 107, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Ricci, D.; Romeo, D.M.M.; Haataja, L.; van Haastert, I.C.; Cesarini, L.; Maunu, J.; Pane, M.; Gallini, F.; Luciano, R.; Romagnoli, C.; et al. Neurological Examination of Preterm Infants at Term Equivalent Age. Early Human Dev. 2008, 84, 751–761. [Google Scholar] [CrossRef]
- Dusing, S.C.; Kyvelidou, A.; Mercer, V.S.; Stergiou, N. Infants Born Preterm Exhibit Different Patterns of Center-of-Pressure Movement Than Infants Born at Full Term. Phys. Ther. 2009, 89, 1354–1362. [Google Scholar] [CrossRef]
- de Groot, L. Posture and Motility in Preterm Infants. Dev. Med. Child Neurol. 2000, 42, 65–68. [Google Scholar] [CrossRef]
- Samsom, J.F.; de Groot, L. The Influence of Postural Control on Motility and Hand Function in a Group of ‘High Risk’ Preterm Infants at 1 Year of Age. Early Hum. Dev. 2000, 60, 101–113. [Google Scholar] [CrossRef]
- Mercuri, E.; Guzzetta, A.; Laroche, S.; Ricci, D.; vanHaastert, I.; Simpson, A.; Luciano, R.; Bleakley, C.; Frisone, M.F.; Haataja, L.; et al. Neurologic Examination of Preterm Infants at Term Age: Comparison with Term Infants. J. Pediatrics 2003, 142, 647–655. [Google Scholar] [CrossRef]
- American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome The Changing Concept of Sudden Infant Death Syndrome: Diagnostic Coding Shifts, Controversies Regarding the Sleeping Environment, and New Variables to Consider in Reducing Risk. Pediatrics 2005, 116, 1245–1255. [CrossRef]
- Rowland, K.; Das, N. PURLs: Helmets for Positional Skull Deformities: A Good Idea, or Not? J. Fam. Pract. 2015, 64, 44–46. [Google Scholar]
- Jenny, B.; Smoll, N.R.; Rilliet, B.; Gautschi, O.P. Management of Positional Plagiocephaly—Helmet or No Helmet? Childs Nerv. Syst. 2014, 30, 1153–1154. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sillifant, P.; Vaiude, P.; Bruce, S.; Quirk, D.; Sinha, A.; Burn, S.C.; Richardson, D.; Duncan, C. Positional Plagiocephaly: Experience with a Passive Orthotic Mattress. J. Craniofacial Surg. 2014, 25, 1365–1368. [Google Scholar] [CrossRef] [PubMed]
- Gajewska, E.; Moczko, J.; Kroll, P.; Naczk, M.; Naczk, A.; Sobieska, M. How Motor Elements at 3 Months Influence Motor Performance at the Age of 6 Months. Medicine 2021, 100, e27381. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.W.; Landenberger, M.; Jung, T.; Lindenthal, T.; Philippi, H. Vojta Therapy and Neurodevelopmental Treatment in Children with Infantile Postural Asymmetry: A Randomised Controlled Trial. J. Phys. Ther. Sci. 2017, 29, 301–306. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Chaput, J.-P.; Adamo, K.B.; Aubert, S.; Barnes, J.D.; Choquette, L.; Duggan, M.; Faulkner, G.; Goldfield, G.S.; Gray, C.E.; et al. Canadian 24-Hour Movement Guidelines for the Early Years (0–4 Years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep. BMC Public Health 2017, 17, 874. [Google Scholar] [CrossRef]
- Carson, V.; Zhang, Z.; Predy, M.; Pritchard, L.; Hesketh, K.D. Longitudinal Associations between Infant Movement Behaviours and Development. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 10. [Google Scholar] [CrossRef]
- Tremblay, M.S. Introducing 24-Hour Movement Guidelines for the Early Years: A New Paradigm Gaining Momentum. J. Phys. Act. Health 2020, 17, 92–95. [Google Scholar] [CrossRef]
- Pin, T.; Eldridge, B.; Galea, M.P. A Review of the Effects of Sleep Position, Play Position, and Equipment Use on Motor Development in Infants. Dev. Med. Child. Neurol. 2007, 49, 858–867. [Google Scholar] [CrossRef]
- Sudden Infant Death Syndrome Prevention|BMC Pediatrics|Full Text. Available online: https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-021-02536-z (accessed on 19 July 2022).
- Hershenson, M.B.; Colin, A.A.; Wohl, M.E.; Stark, A.R. Changes in the Contribution of the Rib Cage to Tidal Breathing during Infancy. Am. Rev. Respir. Dis. 1990, 141, 922–925. [Google Scholar] [CrossRef]
- Papastamelos, C.; Panitch, H.B.; England, S.E.; Allen, J.L. Developmental Changes in Chest Wall Compliance in Infancy and Early Childhood. J. Appl. Physiol. 1995, 78, 179–184. [Google Scholar] [CrossRef]
- Sieck, G.C.; Fournier, M.; Blanco, C.E. Diaphragm Muscle Fatigue Resistance during Postnatal Development. J. Appl. Physiol. 1991, 71, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Skatvedt, O.; Grøgaard, J. Infant Sleeping Position and Inspiratory Pressures in the Upper Airways and Oesophagus. Arch. Dis. Child. 1994, 71, 138–140. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dassios, T.; Vervenioti, A.; Dimitriou, G. Respiratory Muscle Function in the Newborn: A Narrative Review. Pediatr. Res. 2022, 91, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, M.R.; Greenspan, J.S.; Deoras, K.S.; Allen, J.L.; Shaffer, T.H. Effect of Position on the Mechanical Interaction between the Rib Cage and Abdomen in Preterm Infants. J. Appl. Physiol. 1992, 72, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Lipsett, B.J.; Reddy, V.; Steanson, K. Anatomy, Head and Neck, Fontanelles. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Rothman, S.M.; Lee, B.C. What Bulges under a Bulging Fontanel? Arch. Pediatr. Adolesc. Med. 1998, 152, 100–101. [Google Scholar] [PubMed]
- A Bologna c’è il Materassino Che ‘Protegge’ i Neonati, il Primo in Italia. Available online: https://www.ordineinfermieribologna.it/2017/a-bologna-ce-il-materassino-che-protegge-i-neonati-il-primo-in-italia.html (accessed on 3 October 2022).


| Articles screening strategy | KEYWORDS: A: “positional plagiocephaly”; B: “prevention”; |
| Boolean Indicators: “A” AND “B” | |
| Timespan: from January 2012 up to October 2022. | |
| Language: only ENGLISH | |
| Electronic Databases: PubMed, Web of Science, Google Scholar, Scopus, Cochrane Library, ScienceDirect |
| Ref | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
| [48] | Miyabayashi et al., 2022 | Observational study | 3D scanner evaluation of values for cranial morphological features in 1-month-old Japanese infants, to have the prevalence of PP. | In 153 healthy infants, a 3D scanner and image analysis software was used to evaluate cranial form. | The CVAI (Cranial Vault Asymmetry Index) >3.5% or ≥10% were diagnosed as deformational (64.7%) or severe PP (6.6%). |
| [49] | Wang Yang et al., 2019 | Multicenter study | Evaluation of PP in premature infants to have an early diagnosis. | In 530 preterm infants, the head shape was evaluated by a simple manual method based on Wilbrand’s standardized scheme. | PP was 3.0%, and those of right and left plagiocephaly were 69.4 and 30.6%, respectively. The PP was highest in newborns with a gestational period < 32 weeks. |
| [50] | Kajita et al., 2017 | Case report | Evaluation of ULS with typical cranium characteristics of PP. | 10-month girl; 3-year-old boy. | Collaboration with craniofacial surgeons is fundamental in the case of infant cranial deformity to avoid simply diagnosing PP and missing craniosynostosis. |
| [41] | Amy Y.F. Leung et al., 2016 | Prospective study | Evaluation of skull orientation and how PP relates to it in full-term newborns with no congenital problems. | 94 newborns were observed at 3, 6, and 9 weeks to control head orientation, including head orientation length, strength, and turning latency. At three weeks, the direction of the head on one side duration was most prevalent (right: 40, left: 41, midline: 19). | After the side was taken into consideration, head orientation force was comparable throughout the three ages, although from 3 to 9 weeks, the vigor of head orientation to the left declined. |
| [14] | Cabrera-Martos et al., 2013 | Prospective clinical trial | According to their unique clinical profile, the effectiveness of a conservative strategy in plagiocephaly-affected infants is evaluated. | 104 newborns with nonsynostotic plagiocephaly accompanied or not by congenital or positional torticollis. | The suggested physiotherapy regimen can successfully treat Plagiocephaly. |
| [51] | Ifflaender et al., 2013 | observational study | Prevalence of symmetrical and AC abnormalities and to pinpoint potential risk factors, data on the head shape of preterm newborns at TEA (Term-Equivalent Age) are evaluated. | 195 newborn scans were gained using a 3D laser shape digitizer. | At TEA, preterm newborns had a significant frequency of symmetrical and AC abnormalities. |
| Ref | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
| [55] | Weernink et al., 2014 | Observational case–control study | Analyzing the relationship between intake of vitamin D supplements during the third trimester of pregnancy (mother) and during the newborn period (child) and the emergence of positional skull deformation in infants aged 2 to 4 months. | 548 matched controls and 275 babies with positional cranial deformation aged 2–4 months were compared. | An increased risk of positional deformation of the skull is linked to the pregnant woman’s inadequate vitamin D consumption. |
| [56] | Michels et al., 2012 | Retrospective case–control study | Evaluation of the connection between elevated folic acid intake and PP. | Participants in the study were 94 mothers (PP group: children with PP) and 94 mothers (CO group: children without PP). Some subjects were excluded from the study, so the PP group consisted of 75 mothers and the CO group of 54. | 20% of PP patients took the recommended double dose of folic acid, while only 6% of the CO group % did the same. |
| [57] | Nuysink et al., 2012 | Retrospective longitudinal study | Examine the frequency of an idiopathic asymmetry in 192 newborns (gestational age ≤ 32.0 weeks) at TEA and 6 months CA (Corrected age). | 192 infants born ≤ 32.0 weeks of gestation | At TEA, positioning preferences for the head were present in 44.8% of cases; in 10.4% of PP cases, and 13 percent of cases at 6 months CA. In preventing the onset of a PP, special care must be taken, given the high frequency of a positional preference in children delivered preterm at TEA. |
| [26] | Mawji et al., 2014 | Prospective cohort study | Identify possible causes of PP in newborns between the ages of seven and twelve weeks. | 384 healthy-term babies aged 7 to 12 weeks | It was calculated that 46.6% of children had PP. The identified risk factors are a right-sided head positional preference, supine in sleep, part positioned by vacuum/forceps, and male sex. |
| Ref | Authors (Year) | Type of the Study/Days | Aim of the Study | Materials | Results |
|---|---|---|---|---|---|
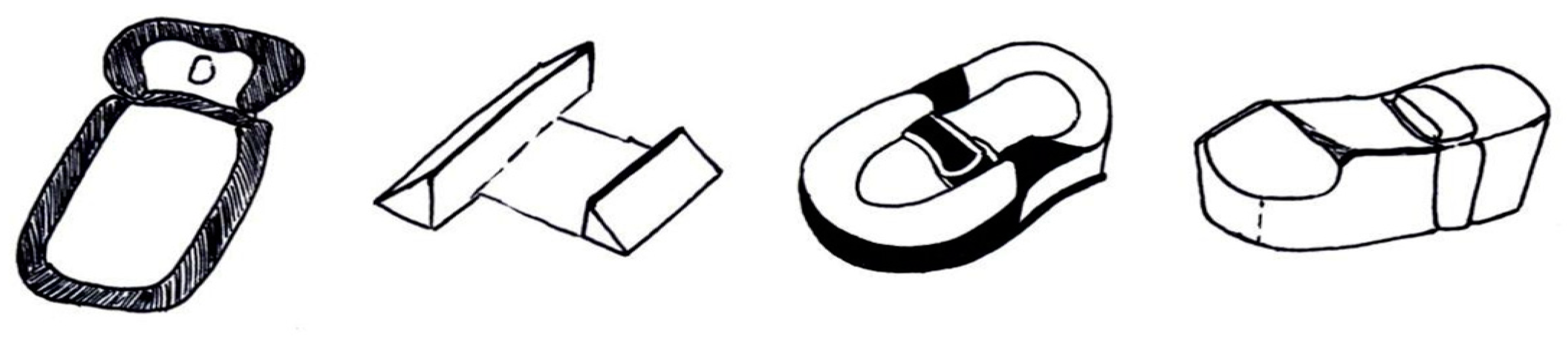
| [73] | Sillifant et al., 2014 | Clinical study | The objective is a comparison of cranial deformity of infants affected by PP before and after the adoption of a Sleepcurve mattress. | 30 patients with a mean age of five months were included. The grade of asymmetry was assessed with CVA and was classified into three ranges: clinically insignificant (CVA 6 mm), moderate (CVA 6–12 mm), and high (CVA > 12 mm). | The improvement of cranial symmetry was statistically relevant (p value of 0.001). The average asymmetry was 5 mm, compared to the 16 mm at the start. The symmetry enhancement was 11 mm. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Malcangi, G.; Patano, A.; Di Pede, C.; Netti, A.; Ciocia, A.M.; Corriero, A.; Semjonova, A.; et al. A Systematic Review of Positional Plagiocephaly Prevention Methods for Patients in Development. Appl. Sci. 2022, 12, 11172. https://doi.org/10.3390/app122111172
Inchingolo AD, Inchingolo AM, Piras F, Malcangi G, Patano A, Di Pede C, Netti A, Ciocia AM, Corriero A, Semjonova A, et al. A Systematic Review of Positional Plagiocephaly Prevention Methods for Patients in Development. Applied Sciences. 2022; 12(21):11172. https://doi.org/10.3390/app122111172
Chicago/Turabian StyleInchingolo, Alessio Danilo, Angelo Michele Inchingolo, Fabio Piras, Giuseppina Malcangi, Assunta Patano, Chiara Di Pede, Anna Netti, Anna Maria Ciocia, Alberto Corriero, Alexandra Semjonova, and et al. 2022. "A Systematic Review of Positional Plagiocephaly Prevention Methods for Patients in Development" Applied Sciences 12, no. 21: 11172. https://doi.org/10.3390/app122111172
APA StyleInchingolo, A. D., Inchingolo, A. M., Piras, F., Malcangi, G., Patano, A., Di Pede, C., Netti, A., Ciocia, A. M., Corriero, A., Semjonova, A., Azzollini, D., De Ruvo, E., Viapiano, F., Ferrara, I., Palmieri, G., Campanelli, M., Mancini, A., De Leonardis, N., Avantario, P., ... Dipalma, G. (2022). A Systematic Review of Positional Plagiocephaly Prevention Methods for Patients in Development. Applied Sciences, 12(21), 11172. https://doi.org/10.3390/app122111172




















