The Relationship between the Ability to Cope with Unexpected Perturbations and Mechanical and Functional Ankle Instability
Abstract
1. Introduction
2. Methods
2.1. Participants
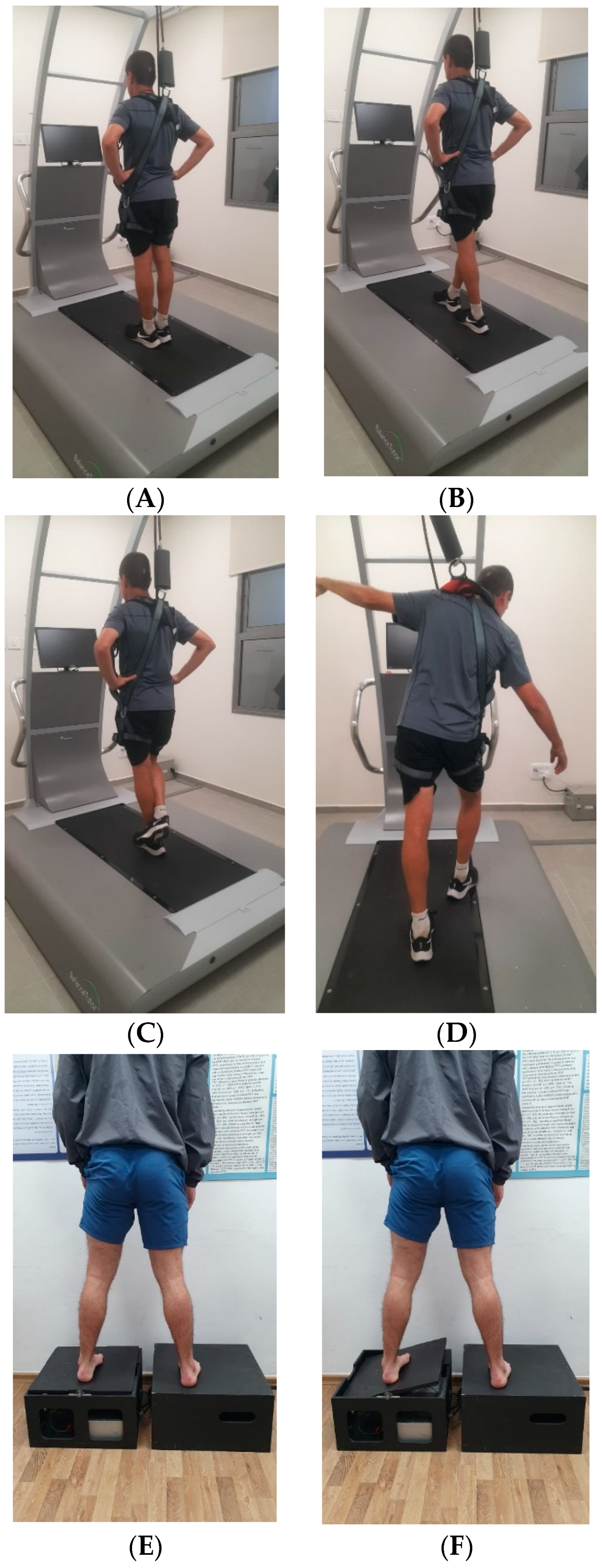
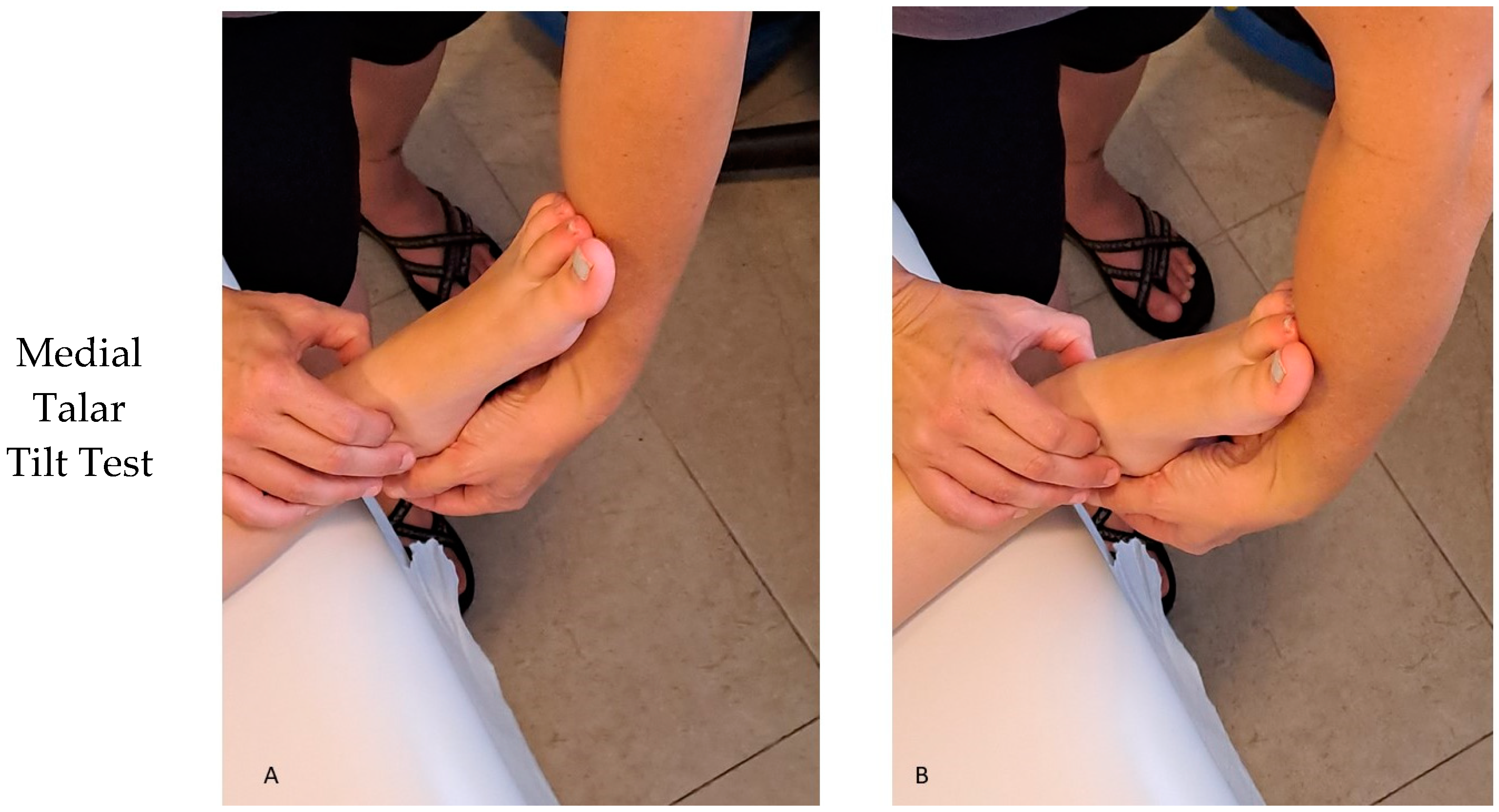
2.2. Procedure
2.3. Instruments
2.4. Statistical Analysis
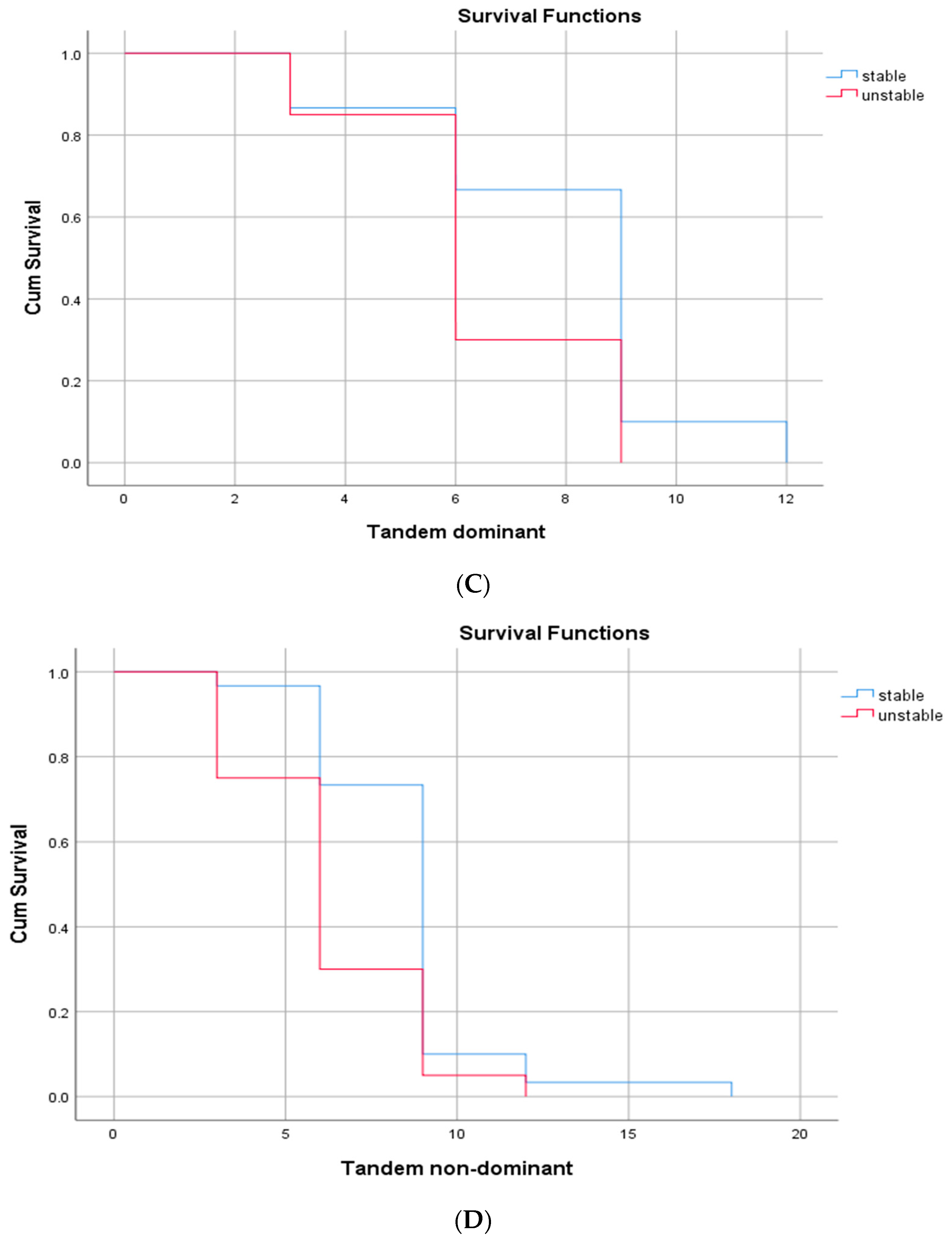
3. Results
4. Discussion
4.1. Limitations and Future Studies
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br. J. Sport. Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Kitamura, T.; Takasaki, H. Preseason Prognostic Factors for Injuries and Match Loss in Collision Sports: A Systematic Review. Int. J. Sport. Med. 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Gaddi, D.; Mosca, A.; Piatti, M.; Munegato, D.; Catalano, M.; Di Lorenzo, G.; Turati, M.; Zanchi, N.; Piscitelli, D.; Chui, K.; et al. Acute Ankle Sprain Management: An Umbrella Review of Systematic Reviews. Front. Med. 2022, 9, 868474. [Google Scholar] [CrossRef] [PubMed]
- Wikstrom, E.A.; Cain, M.S.; Chandran, A.; Song, K.; Regan, B.T.; Migel, D.K.; Kerr, Z.Y. Lateral Ankle Sprain and Subsequent Ankle Sprain Risk: A Systematic Review. J. Athl. Train. 2021, 56, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Esposito, E.R.; Farrokhi, S.; Shuman, B.R.; Sessoms, P.H.; Szymanek, E.; Hoppes, C.W.; Bechard, L.; King, D.; Fraser, J.J. Uneven Treadmill Training for Rehabilitation of Lateral Ankle Sprains and Chronic Ankle Instability: Protocol for a Pragmatic Randomized Controlled Trial. JMIR Res. Protoc. 2022, 11, e38442. [Google Scholar] [CrossRef]
- Fraser, J.J.; Hertel, J. Effects of a 4-Week Intrinsic Foot Muscle Exercise Program on Motor Function: A Preliminary Randomized Control Trial. J. Sport Rehabil. 2019, 28, 339–349. [Google Scholar] [CrossRef]
- Dolan, P.; Kenny, I.; Glynn, L.; Campbell, M.; Warrington, G.D.; Cahalan, R.; Harrison, A.; Lyons, M.; Comyns, T. Risk factors for acute ankle sprains in field-based, team contact sports: A systematic review of prospective etiological studies. Physician Sportsmed. 2022, 1–14. [Google Scholar] [CrossRef]
- Kolokotsios, S.; Drousia, G.; Koukoulithras, I.; Plexousakis, M. Ankle Injuries in Soccer Players: A Narrative Review. Cureus 2021, 13, e17228. [Google Scholar] [CrossRef]
- Noronha, M.; França, L.C.; Haupenthal, A.; Nunes, G.S. Intrinsic predictive factors for ankle sprain in active university students: A prospective study. Scand. J. Med. Sci. Sport. 2012, 23, 541–547. [Google Scholar] [CrossRef]
- Hertel, J.; Corbett, R.O. An Updated Model of Chronic Ankle Instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic Ankle Instability: Evolution of the Model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.M.; Caulfield, B.; Docherty, C.L.; Fong, D.T.-P.; Fourchet, F.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; et al. Selection Criteria for Patients with Chronic Ankle Instability in Controlled Research: A Position Statement of the International Ankle Consortium. J. Athl. Train. 2014, 49, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Delahunt, E.; Coughlan, G.F.; Caulfield, B.; Nightingale, E.J.; Lin, C.-W.C.; Hiller, C.E. Inclusion Criteria When Investigating Insufficiencies in Chronic Ankle Instability. Med. Sci. Sport. Exerc. 2010, 42, 2106–2121. [Google Scholar] [CrossRef] [PubMed]
- Schneiders, A.; Gregory, K.; Karas, S.; Mündermann, A. Effect of foot position on balance ability in single-leg stance with and without visual feedback. J. Biomech. 2016, 49, 1969–1972. [Google Scholar] [CrossRef] [PubMed]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland Ankle Instability Tool: A Report of Validity and Reliability Testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- Docherty, C.L.; McLeod, T.C.V.; Shultz, S.J. Postural Control Deficits in Participants with Functional Ankle Instability as Measured by the Balance Error Scoring System. Clin. J. Sport Med. 2006, 16, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Gholizadeh, H.; Hill, A.; Nantel, J. The effect of various arm and walking conditions on postural dynamic stability when recovering from a trip perturbation. Gait Posture 2019, 76, 284–289. [Google Scholar] [CrossRef]
- Bates, A.V.; McGregor, A.; Alexander, C.M. Adaptation of balance reactions following forward perturbations in people with joint hypermobility syndrome. BMC Musculoskelet. Disord. 2021, 22, 123. [Google Scholar] [CrossRef]
- Tokur, D.; Grimmer, M.; Seyfarth, A. Review of balance recovery in response to external perturbations during daily activities. Hum. Mov. Sci. 2019, 69, 102546. [Google Scholar] [CrossRef]
- Munoz-Martel, V.; Santuz, A.; Bohm, S.; Arampatzis, A. Neuromechanics of Dynamic Balance Tasks in the Presence of Perturbations. Front. Hum. Neurosci. 2020, 14, 560630. [Google Scholar] [CrossRef]
- Picot, B.; Rémy-Neris, O.; Forestier, N. Proprioceptive postural control strategies differ among non-injured athletes. Neurosci. Lett. 2022, 769, 136366. [Google Scholar] [CrossRef]
- Jeon, W.; Jensen, J.L.; Griffin, L. Muscle activity and balance control during sit-to-stand across symmetric and asymmetric initial foot positions in healthy adults. Gait Posture 2019, 71, 138–144. [Google Scholar] [CrossRef]
- Talis, V.L.; Kazennikov, O.V. Effects of body turn on postural sway during symmetrical and asymmetrical standing. Exp. Brain Res. 2019, 237, 2231–2237. [Google Scholar] [CrossRef]
- Rodríguez-Sanz, D.; García-Sánchez, A.; Becerro-De-Bengoa-Vallejo, R.; Martínez-Jiménez, E.M.; Calvo-Lobo, C.; Fernández-Carnero, J.; Losa-Iglesias, M.E.; López-López, D. Eyes-Open Versus Eyes-Closed Somatosensory Motor Balance in Professional Soccer Players with Chronic Ankle Instability: A Case-Control Study. Orthop. J. Sport. Med. 2021, 9, 2325967120983606. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Dynamic balance deficits in individuals with chronic ankle instability compared to ankle sprain copers 1 year after a first-time lateral ankle sprain injury. Knee Surg. Sport. Traumatol. Arthrosc. 2016, 24, 1086–1095. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M. Recent developments on models and inclusion criteria for chronic ankle instability. J. Sport Health Sci. 2012, 1, 170–171. [Google Scholar] [CrossRef][Green Version]
- Larkins, L.W.; Baker, R.T.; Baker, J.G. Physical Examination of the Ankle: A Review of the Original Orthopedic Special Test Description and Scientific Validity of Common Tests for Ankle Examination. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100072. [Google Scholar] [CrossRef] [PubMed]
- Vuurberg, G.; Kluit, L.; van Dijk, C.N. The Cumberland Ankle Instability Tool (CAIT) in the Dutch population with and without complaints of ankle instability. Knee Surg. Sport. Traumatol. Arthrosc. 2018, 26, 882–891. [Google Scholar] [CrossRef]
- MadehKhaksar, F.; Klenk, J.; Sczuka, K.; Gordt, K.; Melzer, I.; Schwenk, M. The effects of unexpected mechanical perturbations during treadmill walking on spatiotemporal gait parameters, and the dynamic stability measures by which to quantify postural response. PLoS ONE 2018, 13, e0195902. [Google Scholar] [CrossRef]
- Witchalls, J.B.; Waddington, G.; Adams, R.; Blanch, P. Chronic ankle instability affects learning rate during repeated proprioception testing. Phys. Ther. Sport 2014, 15, 106–111. [Google Scholar] [CrossRef]
- Cho, J.H.; Lee, D.; Song, H.K.; Bang, J.Y.; Lee, K.T.; Park, Y.U. Value of stress ultrasound for the diagnosis of chronic ankle instability compared to manual anterior drawer test, stress radiography, magnetic resonance imaging, and arthroscopy. Knee Surg. Sport. Traumatol. Arthrosc. 2016, 24, 1022–1028. [Google Scholar] [CrossRef]
- Donahue, M.; Simon, J.; Docherty, C.L. Critical Review of Self-Reported Functional Ankle Instability Measures. Foot Ankle Int. 2011, 32, 1140–1146. [Google Scholar] [CrossRef] [PubMed]
- Pourkazemi, F.; Hiller, C.E.; Raymond, J.; Nightingale, E.J.; Refshauge, K. Predictors of chronic ankle instability after an index lateral ankle sprain: A systematic review. J. Sci. Med. Sport 2014, 17, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Hiller, C.E.; Refshauge, K.; Herbert, R.; Kilbreath, S. Balance and Recovery from a Perturbation are Impaired in People with Functional Ankle Instability. Clin. J. Sport Med. 2007, 17, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Hirai, D.; Docherty, C.L.; Schrader, J. Severity of Functional and Mechanical Ankle Instability in an Active Population. Foot Ankle Int. 2009, 30, 1071–1077. [Google Scholar] [CrossRef]
- Watabe, T.; Takabayashi, T.; Tokunaga, Y.; Kubo, M. Copers adopt an altered dynamic postural control compared to individuals with chronic ankle instability and controls in unanticipated single-leg landing. Gait Posture 2021, 92, 378–382. [Google Scholar] [CrossRef]
- Eechaute, C.; De Ridder, R.; Maes, T.; Beckwée, D.; Swinnen, E.; Buyl, R.; Vaes, P. Evidence of a different landing strategy in subjects with chronic ankle instability. Gait Posture 2017, 52, 62–67. [Google Scholar] [CrossRef]
- Hiller, C.E.; Blair, S.; Nightingale, E.J.; Simic, M.; Burns, J. People with recurrent ankle sprains do not change their ankle strategy in anticipation of a perturbation event. J. Foot Ankle Res. 2014, 7, A33. [Google Scholar] [CrossRef]
- Brown, C.N.; Mynark, R. Balance deficits in recreational athletes with chronic ankle instability. J. Athl. Train. 2007, 42, 367–373. [Google Scholar]
- Steinberg, N.; Adams, R.; Ayalon, M.; Dotan, N.; Bretter, S.; Waddington, G. Recent Ankle Injury, Sport Participation Level, and Tests of Proprioception. J. Sport Rehabil. 2019, 28, 824–830. [Google Scholar] [CrossRef]
- Sousa, A.S.P.; Leite, J.; Costa, B.; Santos, R. Bilateral Proprioceptive Evaluation in Individuals with Unilateral Chronic Ankle Instability. J. Athl. Train. 2017, 52, 360–367. [Google Scholar] [CrossRef]
- Xue, X.; Ma, T.; Li, Q.; Song, Y.; Hua, Y. Chronic ankle instability is associated with proprioception deficits: A systematic review and meta-analysis. J. Sport Health Sci. 2021, 10, 182–191. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Iqbal, Z.A.; Iqbal, A.; Ahmed, H.; Ramteke, S.U. Effect of Chronic Ankle Sprain on Pain, Range of Motion, Proprioception, and Balance among Athletes. Int. J. Environ. Res. Public Health 2020, 17, 5318. [Google Scholar] [CrossRef]
- Witchalls, J.; Waddington, G.; Blanch, P.; Adams, R. Ankle Instability Effects on Joint Position Sense When Stepping Across the Active Movement Extent Discrimination Apparatus. J. Athl. Train. 2012, 47, 627–634. [Google Scholar] [CrossRef]
- Hiller, C.E.; Nightingale, E.J.; Lin, C.-W.C.; Coughlan, G.F.; Caulfield, B.; Delahunt, E. Characteristics of people with recurrent ankle sprains: A systematic review with meta-analysis. Br. J. Sport. Med. 2011, 45, 660–672. [Google Scholar] [CrossRef]
- DeJong, M.A.F.; Koldenhoven, R.; Hertel, J. Proximal Adaptations in Chronic Ankle Instability: Systematic Review and Meta-analysis. Med. Sci. Sport. Exerc. 2020, 52, 1563–1575. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, U.; Melzer, I.; Zeilig, G.; Plotnik, M. Muscle activation profile is modulated by unexpected balance loss in walking. Gait Posture 2022, 93, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.S.; Silva, M.; Gonzalez, S.; Santos, R. Bilateral compensatory postural adjustments to a unilateral perturbation in subjects with chronic ankle instability. Clin. Biomech. 2018, 57, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Rieger, M.; Papegaaij, S.; Pijnappels, M.; Steenbrink, F.; van Dieën, J. Transfer and retention effects of gait training with anterior-posterior perturbations to postural responses after medio-lateral gait perturbations in older adults. Clin. Biomech. 2020, 75, 104988. [Google Scholar] [CrossRef] [PubMed]
- Caldemeyer, L.E.; Brown, S.M.; Mulcahey, M.K. Neuromuscular training for the prevention of ankle sprains in female athletes: A systematic review. Physician Sportsmed. 2020, 48, 363–369. [Google Scholar] [CrossRef]
- Riva, D.; Bianchi, R.; Rocca, F.; Mamo, C. Proprioceptive Training and Injury Prevention in a Professional Men’s Basketball Team: A Six-Year Prospective Study. J. Strength Cond. Res. 2016, 30, 461–475. [Google Scholar] [CrossRef] [PubMed]
- Mosca, M.; Caravelli, S.; Massimi, S.; Fuiano, M.; Catanese, G.; Barone, G.; Bragonzoni, L.; Benedetti, M.G. Evaluation of proprioception and postural control at a minimum 1 year follow-up after ankle capsuloligamentous lateralplasty with Brostrom technique: A cohort study. Medicine 2020, 99, e19862. [Google Scholar] [CrossRef] [PubMed]


| CAIT D | CAITN D | Ankle Sprains | AII D | AII ND | Clinical ass. D | Clinical ass. ND | AMEDA D | |
|---|---|---|---|---|---|---|---|---|
| CAIT D | - | |||||||
| CAIT ND | 0.762 * | - | ||||||
| Ankle sprains | −0.626 * | −0.710 * | - | |||||
| AII D | −0.833 * | −0.555 * | 0.670 * | - | ||||
| AII ND | −0.434 * | −0.733 * | 0.662 * | 0.378 * | - | |||
| Clinical ass. D | −0.497 * | −0.386 * | 0.283 * | 0.563 * | 0.383 * | - | ||
| Clinical ass. ND | −0.379 * | −0.560 * | 0.363 * | 0.281 * | 0.420 * | 0.452 * | - | |
| AUC D | 0.453 * | 0.273 * | −0.418 * | −0.434 * | −0.215 | −0.199 | −0.086 | - |
| AUC ND | 0.211 | 0.196 | −0.762 * | 0.153 | −0.285 * | −0.138 | −0.183 | 0.646 * |
| SO | SC | TD | TND | SLSS | SLOS | Walk | ||
|---|---|---|---|---|---|---|---|---|
| CAIT D | ≤25 | 15 (3) | 12 (6) | 6 (3) * | 6 (3) * | 6 (4) | 6 (0) | 12 (3) |
| >25 | 15 (6) | 12 (6) | 9 (3) * | 9 (3) * | 6 (6) | 6 (2) | 12 (3) | |
| CAIT ND | ≤25 | 15 (6) | 12 (8) | 6 (3) * | 6 (3) * | 6 (6) | 6 (0) | 12 (3) |
| >25 | 15 (6) | 12 (6) | 9 (3) * | 9 (2) * | 9 (4) | 6 (1) | 14 (3) | |
| AII D | ≥5 | 14 (3) * | 12 (6) * | 6 (3) * | 6 (6) * | 6 (6) | 6 (0) | 12 (3) * |
| <5 | 15 (6) * | 14 (6) * | 9 (3) * | 9 (3) * | 6 (4) | 6 (0) | 15 (6) * | |
| AII ND | ≥5 | 12 (3) * | 9 (6)* | 6 (0) * | 6 (6) * | 6 (7) | 6 (2) | 9 (6) * |
| <5 | 15 (6) * | 12 (6) * | 9 (3) * | 9 (3) * | 6 (4) | 6 (0) | 12 (3) * | |
| Clinical ass. D | ≥2 | 15 (6) | 12 (6) | 8 (3) | 9 (3) | 6 (6) | 6 (1) | 12 (3) |
| <2 | 15 (5) | 15 (6) | 9 (3) | 9 (3) | 6 (4) | 6 (0) | 15 (9) | |
| Clinical ass. ND | ≥2 | 15 (3) | 12 (6) | 6 (3) | 9 (3) | 6 (6) | 6 (0) | 12 (3) |
| <2 | 15 (6) | 15 (9) | 9 (3) | 9 (3) | 6 (4) | 6 (0) | 12 (3) | |
| Ankle sprains | =5 | 12 (6) * | 9 (6) * | 6 (3) * | 6 (3) * | 4 (6) | 6 (0) | 12 (6) * |
| ≤4 | 15 (6) * | 15 (6) * | 9 (3) * | 9 (3) * | 6 (4) | 6 (0) | 15 (6) * |
| Ankle Sprains (0 ≤ 4; 1 = 5) | ALL (0 < 5; 1 ≥ 5) | Clinical ass. (0 < 2; 1 ≥ 2) | CAIT (0 > 25; 1 ≤ 25) | AUC (0 = Low. Tertile 1 = Upp. Tertile) | n (%) | |
|---|---|---|---|---|---|---|
| No-CAI in ≥4/5 assessments (“Stable” group) | 0 | 0 | 0 | 0 | 0 | 13 (22.0) |
| 0 | 0 | 0 | 0 | 1 | 8 (13.6) | |
| 0 | 0 | 0 | 1 | 0 | 1 (1.7) | |
| 0 | 0 | 1 | 0 | 0 | 7 (11.9) | |
| 1 | 0 | 0 | 0 | 0 | 1 (1.7) | |
| CAI/no-CAI in <4 assessments | 0 | 0 | 1 | 1 | 0 | 4 (6.8) |
| 0 | 0 | 1 | 1 | 1 | 1 (1.7) | |
| 1 | 0 | 0 | 0 | 1 | 1 (1.7) | |
| 1 | 0 | 0 | 1 | 0 | 1 (1.7) | |
| 1 | 0 | 0 | 1 | 1 | 1 (1.7) | |
| 1 | 0 | 1 | 1 | 0 | 1 (1.7) | |
| CAI in ≥4/5 assessments (“Unstable” group) | 1 | 0 | 1 | 1 | 1 | 2 (3.4) |
| 1 | 1 | 1 | 1 | 0 | 6 (10.2) | |
| 1 | 1 | 1 | 1 | 1 | 12 (20.3) |
| SO | SC | TD | TND | SLSS | SLOS | Walk | |
|---|---|---|---|---|---|---|---|
| (A) “stable” group | 15 (0.55) | 12 (0.96) | 9 (0.31) | 9 (0.23) | 6 (0.65) | 6 (0.22) | 15 (0.70) |
| (B) “unstable” group | 15 (0.98) | 9 (1.43) | 6 (0.57) | 6 (0.68) | 4 (1.19) | 6 (0.8) | 12 (1.18) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steinberg, N.; Tenenbaum, G.; Zeev, A.; Witchalls, J.; Waddington, G. The Relationship between the Ability to Cope with Unexpected Perturbations and Mechanical and Functional Ankle Instability. Appl. Sci. 2022, 12, 11119. https://doi.org/10.3390/app122111119
Steinberg N, Tenenbaum G, Zeev A, Witchalls J, Waddington G. The Relationship between the Ability to Cope with Unexpected Perturbations and Mechanical and Functional Ankle Instability. Applied Sciences. 2022; 12(21):11119. https://doi.org/10.3390/app122111119
Chicago/Turabian StyleSteinberg, Nili, Galit Tenenbaum, Aviva Zeev, Jeremy Witchalls, and Gordon Waddington. 2022. "The Relationship between the Ability to Cope with Unexpected Perturbations and Mechanical and Functional Ankle Instability" Applied Sciences 12, no. 21: 11119. https://doi.org/10.3390/app122111119
APA StyleSteinberg, N., Tenenbaum, G., Zeev, A., Witchalls, J., & Waddington, G. (2022). The Relationship between the Ability to Cope with Unexpected Perturbations and Mechanical and Functional Ankle Instability. Applied Sciences, 12(21), 11119. https://doi.org/10.3390/app122111119





