Abstract
(1) Background: Total knee arthroplasty (TKA) is a well-established surgical treatment for end-stage osteoarthritis. While no leading factor can be identified, the high frequency of patient dissatisfaction (20%) pertains to several key features such as preoperative expectations and postoperative improvement in knee function. Bicruciate-retaining total knee arthroplasty (BCR-TKA) may improve kinematics and lead to improved clinical outcome in the higher-demanding patients. (2) Methods: A systematic review of the literature was performed to assess the best available preclinical and clinical literature on BCR-TKA for kinematics and clinical outcome and adverse events such as implant loosening. Articles were screened using predefined in- and exclusion criteria. The guidelines for Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) were used. (3) Results: The literature search resulted in 352 articles which were screened for title and abstract. After application of the in- and exclusion criteria, 13 preclinical and 30 clinical articles were included. The methodological quality of studies was low, including mainly level IV studies. (4) Conclusions: This is the first report that provides a systematic description of the broad available preclinical and clinical literature on BCR-TKA. It underlines the current interest in improving kinematics and clinical outcome based on a more anatomical TKA design. The current review demonstrates the low methodological quality of clinical trials that have investigated BCR-TKA. Currently, there are insufficient data to support broad (“state of the art”) implantation of BCR-TKA. Preclinical and clinical research suggest, however, that the design has a potential benefit to achieve improved kinematics in the young and active arthroplasty patient and warrants future research for new-generation designs with optimal (tibial) fixation and reproducible (robot or navigated) surgical placement.
1. Introduction
Total knee arthroplasty (TKA) is a well-established surgical treatment for end-stage osteoarthritis. Primary TKA is performed in over 200 per 100,000 inhabitants per year in large European countries such as Germany and Switzerland [1]. In the United States, the incidence of primary TKAs is expected to rise to 43% (299 per 100,000) inhabitants by 2050. Although successful in the majority of patients, up to 20% report dissatisfaction after treatment. While no leading factor can be identified, patient dissatisfaction pertains to several key factors such as preoperative expectations and the degree of postoperative improvement in knee function [2]. These factors can be attributed to the higher demand of young and active patients that are increasingly receiving primary TKA. In fact, it is expected that over 50% of patients receiving a TKA will be under the age of 65 years by 2030 [3]. As early TKA designs were primarily aimed at the elderly patient, new challenges for improvement in function and kinematics have arisen [3]. Primary TKA was designed to sacrifice the anterior cruciate ligament (ACL) and gain anteroposterior (AP) stability from the implant design in either posterior-cruciate-retaining (CR) or posterior-stabilized (PS) knee arthroplasties. The resulting loss of propriocepsis, along with the paradoxical anterior femoral translation commonly observed in mid- and terminal flexion, may lead to suboptimal kinematics and eventually to patient dissatisfaction [4,5,6,7,8]. Thus, in retaining the cruciate ligaments, bicruciate (BCR)-TKA may improve kinematics and lead to improved clinical outcome in the higher-demanding patients. Although BCR-TKA is expected to improve the performance of these patients as a result of the preserved ACL function, its clinical result remains controversial. The initial bicruciate design was introduced in the 1960s by Gunston [9]. Over the past decades, several newer designs have been introduced, which aim at better (tibial) fixation and range of motion. To date, the lack of improved clinical outcome and implant survival after BCR-TKA along with the low methodological quality of clinical trials have restricted broad implementation. Still, the proposed clinical and kinematic improvement that may be achieved by retaining the ACL has been supported by different kinematic and laboratory studies, along with early results of clinical trials [4]. The increase in the use of robotic-assisted TKA may further improve optimal implant placement, ligament balancing and alignment that may prove to be key factors in its possible success. The purpose of this review is to provide a comprehensive systematic overview of the literature on BCR-TKA to provide an in-depth view on available results and provide a basis for a future prospective.
2. Methods
A systematic review of the literature was performed to assess the best available clinical evidence after BCR-TKA kinematics and clinical outcome and implant survival. The search was conducted on 14 April 2022, in the electronic databases of MEDLINE and Embase, using the following parameters: “bicruciate retaining” OR “bi-cruciate retaining” OR “bicruciate-retaining” OR “bicruciate stabilized” OR “bicruciate-stabilized” OR “bicruciate stabilizing” OR “anterior cruciate ligament retaining” AND “knee arthroplasty” OR “knee replacement”. The articles were screened by title and abstract. The following inclusion criteria for relevant articles were used during the initial screening of titles and abstracts: clinical trials and case series that reported clinical outcome after bicruciate-retaining TKA and or preclinical kinematic laboratory/cadaveric studies. As there is variability in preclinical and clinical outcome measures, no main outcome domain could be used. Case reports, reviews and languages other than English, Dutch or German or non-retraceable articles were excluded. Levels of evidence were assigned to studies based on the methodological quality of their design. Where applicable, the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) were used [10].
3. Results
The literature search resulted in 352 articles which were screened for title and abstract. Of these articles, the majority did not fit the inclusion criteria. After application of the inclusion and exclusion criteria, 13 preclinical and 30 clinical articles could be included (Figure 1). Of the clinical trials, one randomized controlled trial was included; all other studies were of a retrospective design and qualified as level IV evidence.
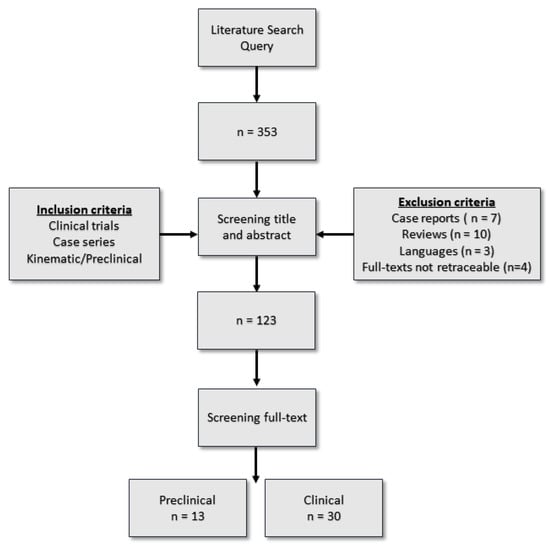
Figure 1.
Systematic literature review flowchart.
3.1. Implant Design and Clinical Outcome
3.1.1. First Generation
The design of BCR-TKA is especially important to ensure proper kinematics and implant survival. A primary concern for first-generation BCR-TKA includes tibial baseplate stability, as there is an absence of a tibial keel and reduced tibial coverage. First-generation BCR-TKA, for which the longest follow-up is available, included a femoral component with cobalt–chromium with an asymmetric trochlear groove requiring right and left components. The tibial component consisted of a flat symmetric polyethylene (PE) insert on a single-piece horseshoe-shaped titanium tibial tray with two round fixation pegs and a flat symmetric polyethylene (PE) bearing [4]. Pritchett presented the largest case series (214 arthroplasties in 160 patients) for this implant (Townley Anatomic, Biopro Inc, Port Huron, MI, USA) with clinical outcomes with a minimum follow-up of 20 years [11]. The Kaplan–Meier curve showed a revision-free survival of 89% (95% confidence interval (CI): 82–93%). Twenty-two knees in twenty-one patients (5.6%) were revised. Reasons for revision were polyethylene wear (n = 7), aseptic loosening of the femoral (n = 4) or tibial component (n = 3) and infection (n = 4). The Cloutier BCR-TKA (Ceraver Osteal, Paris, France), which included a tibial component with two flat symmetrical polyethylene (PE) bearings on a single-piece notched titanium tibial tray with two round 15 mm fixation pegs, showed a survivorship of 82% at 20 years with aseptic component loosening of 4.3% (7 of 163) [12].
3.1.2. Second Generation
Second-generation models were designed to improve implant stability based on an asymmetric-anatomical- or non-anatomical-perimeter-shaped tibial component with better tibial fixation and anterior stability [4].
LCS
In 1990, Buechel and Pappas presented a second-generation bicruciate-retaining meniscal-bearing TKA as part of a comprehensive, interchangeable knee prosthesis system New Jersey Low-Contact-Stress (LCS, DePuy Synthes, Warsaw, IN, USA), with both cemented and cementless options [13]. The bicruciate-retaining tibial component had a “U”-shaped metallic baseplate and separate medial and lateral polyethylene meniscal bearings with articulating surfaces curved to match the femoral geometry. The authors reported on the survival of 21 cemented and 25 cementless BCR-TKAs. In the cemented group, 12-year overall survival was 90.9%, and in the cementless group 6-year overall survival was 100%. Stiehl et al. presented 4743 TKAs that were performed between 1981 and 1997 using the LCS system with BCR (n = 324), CR (n = 2165) and PS (n = 2254) implants, and with a 14-year follow-up found the survivorship for BCR implants to be 79% (95% CI 72; 86); CR implants 82% (95% CI 78; 88); and PS knees 87% (95%CI 81; 94), respectively [14]. The overall 14-year survivorship for cementless fixation was 83% and for cemented fixation 84%. The aseptic loosening rate was the highest for the BCR system (6.1%). Conversely, in a retrospective analysis with a minimum follow-up of 15 years, a higher revision rate was found for an anterior–posterior glide CR-TKA (n = 916) compared to a BCR design (n = 180) with a hazard risk for BCR vs. PCR of 0.52 (0.34–0.80), p = 0.003 (adjusted model) [15]. Again, cemented fixation was preferred, as the 20-year cumulative revision incidence was higher at 2.9% (95% CI 1.7; 4.7) for cemented and 10.9% (95% CI 8.8; 13.4) for uncemented TKA. Table 1 provides a short overview of the clinical outcome studies for LCS BCR-TKA.

Table 1.
Clinical outcome studies for LCS BCR-TKA.
Vanguard XP
In our systematic search, the Vanguard XP (Vanguard XP Total Knee System, Zimmer Biomet, Warsaw, IN, United States) showed to be the BCR-TKA system with the most clinical data available. The design includes asymmetric condyles with a larger lateral condyle than medial to allow greater roll back laterally. The tibial tray consists of a U-shaped cobalt–chromium–molybdenum tray with two pegs and two keels and an asymmetrical PE bearing aimed at the difference in kinematics between the two compartments. Several authors reported promising short-term clinical outcome after performing BCR-TKA with this implant. Alnachoukati et al. found a high satisfaction rate of 94% in 146 BCR-TKAs, with an improvement in mean flexion (116° preoperative to 121° postoperative) and two revisions (1.4%) after a mean of one year follow-up [16]. Several other small case series in 20–50 patients found significant improvement in PROMs after BCR-TKA [17,18]. Of these studies, Peng et al. showed that PROMs were lower for those patients with a greater posterior tibial slope [18]. However, these level IV studies may be susceptible to reporting bias, as failure rates were not reported. Finally, one retrospective report on 107 patients with a mean follow-up of 3 years demonstrated an 88% (95% CI 82; 93) survival. Revisions were performed mainly for tibial loosening (5/19), ACL impingement (3/19) and pain (4/19) [19].
Comparative Studies of the Vanguard XP
A variety of clinical studies compared the Vanguard XP to other designs.
Christensen et al. found that a non-anatomical design BCR-TKA (Vanguard XP) had inferior short-term survivorship and radiolucent lines (RLLs) on X-rays when compared to a conventional CR implant [20]. Indeed, in their study including 78 BCR and 294 CR implants with a mean follow-up of 18 months (range, 2–32 months), knees in the BCR group had a higher frequency of all-cause revision (5% vs. 1.3%; hazard ratio (HR), 7.44; 95% CI 1.24; 44.80) and a greater proportion of RLLs of the tibial component (HR 2.93; 95% CI 1.62; 5.32; p < 0.001). The authors concluded that these results may be explained by learning curves or truly inferior outcomes resulting from the BCR design. Similarly, a large retrospective cohort that compared BCR-TKA (n = 195) with anterior-stabilized (AS) CR-TKA design (n = 1253) at a mid-term follow-up (mean 5.2 years) found a higher revision rate for BCR-TKA of 11.3% vs. 1.6% [21]. Nineteen (9.7%) BCR-TKA knees were revised for aseptic tibial loosening; only one (0.1%) of the AS knees was revised for the same reason (p < 0.001). Compared with AS knees, BCR-TKA had significantly lower improvement in range of motion (3.2 deg vs. 2.2 deg, p < 0.001), Knee Society Score (KSS) pain subscore (39 vs. 35.7, p = 0.014), KSS clinical subscore (52.4 vs. 46, p < 0.001) and KSS functional subscore (20.9 vs. 15.5, p = 0.01).
In a single-blinded randomized controlled trial (n = 50) comparing the Vanguard BCR and CR design, Troelsen et al. found no differences between the two designs in terms of stable fixation on RSA or patient-reported outcome measure scores (PROMs) at 2 years [22]. However, while no reoperations were performed in the CR group, three patients required a reintervention for stiffness and one for a tibial island fracture in the BCR group. Another two case–control studies of the same cohort compared 61 BCR-TKAs with 61 CR TKAs and found no difference in joint awareness and clinical improvement [23,24]. The survival rate of both groups was 98.4% at three years. Both revisions were insert changes due to persistent pain in the CR-TKA group and valgus thrust in the BCR-TKA group. The clinical and comparative studies in which clinical outcome and revision rates were reported for the Vanguard XP design are summarized in Table 2.

Table 2.
Clinical outcome studies for Vanguard XP BCR-TKA.
3.1.3. Third Generation
Journey XR
The Journey II XR (Smith and Nephew plc, Watford, United Kingdom) system was designed to overcome ongoing concerns of loosening and improve kinematics. The design consists of an anatomical tibial component that includes a metal tibia tray with two independent and uniquely designed concave medial and convex lateral bearings together with a natural 3° oblique joint line [4]. One kinematic clinical study in 17 knees of 15 patients found the in vivo kinematics of BCR-TKA knees reproduced native knee kinematics to a lower extent compared 20 patients that received unicompartimental knee arthroplasty (UKA) [25]. Larger clinical trials exploring this design are currently underway (https://clinicaltrials.gov/ct2/show/NCT03136887, accessed on 14 April 2022).
Intraoperative Technique, Design, Balancing and Alignment
Tibial base plate design has proven to have an important effect on the risk of aseptic tibial loosening, a severe adverse event which has been described in early BCR-TKA designs. For example, linking of two separate baseplates appears to provide increased primary stability in terms of bony fixation, comparable to that of a conventional single tibial baseplate [26].
Computational modeling has been used to identify the most sensitive components of knee joint laxity and suggest a sequence for balancing ligament tensions during knee arthroplasty with a preserved ACP and PCL. Based on the findings of one study, an optimal sequence for adjusting strains of ligament bundles during surgery were identified using a variety of laxity examinations [27]. For example, the anteroposterior laxity has been found to be sensitive to the tension of the ACL ligament in early flexion [27,28]. What is more, a significant correlation was found between extension joint gap change and the change in ACL elongation in 29 patients, highlighting the importance of precise joint line restoration and soft tissue balancing during BCR-TKA [29]. Although concerns exist regarding an increase in patellofemoral compressive forces after BCR-TKA, no significant correlations between intraoperative patellofemoral compressive force and anterior knee pain after anatomical BCR-TKA have been found in 22 patients at short-term follow-up (1.5 years) [30]. Posterior tibial slope (PTS) may also be an important factor that determines postoperative kinematics and clinical outcome, as one study demonstrated that it has a significant impact on the stress experienced by the ACL during weight-bearing sit-to-stand and single-leg deep lunge. This suggests that avoiding excessive PTS may be one of the surgical implant alignment factors to consider during surgery to minimize increased preserved ACL tension [31]. This has been supported by computer modeling as well [18]. In addition, in the setting of tibial cuts reproducing the native medial PTS, patients with larger PTS may be at risk of trauma to the posteromedial structures [32]. These findings may emphasize the value of precise robot-assisted surgery and aid in future designs of BCR-TKA.
Preclinical Kinematics
Kinematics of the human knee are a result of an interconnected system of bones, soft tissue structures and muscles resulting in a motion in all six degrees of freedom, with a complex set of translations and rotations. BCR-TKA aims to restore pain-free motion of the joint, based on these physiological kinematics [33]. To achieve this goal, optimal anatomic design, implant position and use of native proprioception are key factors. Several studies have aimed to assess the kinematics of BCR-TKA to better understand how to achieve its theoretical improvement in kinematics. Indeed, during simulated deep knee bend, chair-sit and walking, a biomimetic BCR implant showed activity-dependent kinematics similar to healthy knees in vivo [34]. Restoring native knee geometry together with ACL preservation may thus provide these desired kinematics over contemporary ACL-preserving and ACL-sacrificing implants. Indeed, in 14 cadaveric knee specimens tested under passive conditions with and without external loads, the width of the varus/valgus and internal/external laxity envelope for the native knee and the bicruciate-retaining knee were almost the same. However, in the native knee, a difference in laxity was seen between the stable medial side and the more mobile lateral side [35]. With an image-free navigation system in six fresh-frozen whole-body cadavers, one study found that the amount of tibial internal rotation throughout knee flexion was more similar to that in a native knee if a medial constrained insert was used compared to a flat insert [36]. Others showed that lateral joint laxity was potentially decreased in BCR-TKA, limiting native flexion kinematics. The loss of internal rotation in deep flexion may be compensated by using a lateral insert with a posterior slope of +3° [37].
Although the importance of retaining the ACL was underlined within the BCR-TKA group, no difference was found in contact forces, rotations, translations and ligament forces when BCR-TKA was compared to CR-TKA during a normal walking pattern [38]. Furthermore, Okada et al. found that the preserved ACL in the BCR-TKA cadaveric knees had a 2-fold to 6-fold higher strain than that in intact knees at 0°, 15°, 90° and 120° of passive motion [39]. Computer modeling has also suggested that restoring native knee geometry together with ACL preservation may provide kinematic superiority over contemporary ACL-sacrificing implants [34]. More precisely, computational simulation results suggested that BCR-TKA improves the posterior movement of the lateral condyle, medial condyle and tibial internal rotation through a full range of flexion when compared to CR-TKA and PS-TKA [40]. However, one computer model suggests that surgeons using symmetric BCR-TKA may consider using a kinematic alignment method to achieve sufficient ligament laxity throughout knee flexion to prevent a conflict between the retained ACL and the replaced joint surface [41]. Moreover, the loss of the conforming anatomy of menisci and tibial cartilage and replacement by a relatively flat polyethylene insert may account for the loss of tibial internal rotation and the slight paradoxical anterior motion of the medial femoral condyle [42]. In a cadaveric model, Halewoord et al. found BCR-TKA (Unity KneeTM 77, Corin Ltd., Cirencester, UK) reduced AP laxity versus CR-TKA, and may improve knee stability without using conforming geometry in the implant design. When compared to an implant design with a bridge between the two tibial bearing trays, the use of two components akin as used in UKA prevented tibial avulsion fractures in extension in this model [43]. Still, a cadaveric model showed that the rotational kinematics may be lost once the tibial replacement is performed [44].
In Vivo (Clinical) Kinematics
A variety of small clinical studies have analyzed in vivo kinematics after BCR-TKA to better understand the advantages of this design. Several studies have confirmed BCR-TKAs to have good AP stability throughout the range of knee flexion, regardless of the weight-bearing condition [45,46]. Furthermore, using fluoroscopy while performing a deep knee bend activity, subjects having a BCR-TKA (n = 10) exhibited a more normal-like kinematic pattern in early and late flexion compared to CR-TKAs (n = 40) [47].
Kono et al. matched kinematic data from BCR-TKA (Journey II XR, Smith and Nephew plc), UKA and healthy controls during squatting motion, under fluoroscopy [25]. Here, there was a lower extension angle of UKA knees than healthy and BCR-TKA knees (p < 0.01) and lower flexion of BCR-TKA knees compared to healthy and UKA knees (p < 0.01). In a separate study, it was found that BCR-TKA reduced femoral external rotation and AP translation with flexion. In addition, while preoperatively ACL forces correlated highly with AP translation of the femur during squatting, postoperatively only posterior cruciate ligament (PCL) forces correlated with AP translation of the lateral femoral condyle during squatting. These findings indicate that kinematic changes correlate with changes in cruciate ligament forces, thus underlining the lack of achieving native kinematics [48]. This has been supported by a validated computer tomography and fluoroscopic imaging system in 29 patients who underwent unilateral BCR-TKA. Again, during a single-leg deep lunge, BCR-TKAs showed significantly less posterior femoral translation during terminal flexion, compared with the contralateral native knee. Similarly, BCR-TKAs showed significantly less mean femoral rollback during sit-to-stand. BCR-TKAs also demonstrated significantly reduced internal rotation during high-flexion lunge and sit-to-stand. Even further, while Tsai et al. showed no statistical significant differences in AP translation as well as varus rotation for BCR-TKA (Vanguard XP) (n = 30) compared to normal healthy knees during the stance phase, sagittal plane motion and tibiofemoral articular contact characteristics including pivoting patterns were not fully restored in BCR-TKA patients during gait [49]. Together with the lack of restored sagittal plane motions and tibiofemoral articular contact characteristics during gait, these findings suggest that BCR-TKA does not restore native tibiofemoral articular contact kinematics [50]. Hennessy et al. analyzed kinematic gait in females and males (15/14) after BCR-TKA implantation (Vanguard XP). The authors demonstrated significant increase in the KSS (58.1 ± 11.8 preoperative to 86.6 ± 16.7 postoperative, p < 0.001). In a nine-month follow-up case–control study that compared BCR-TKA to PS-TKA and UKA in groups of twenty patients each, BCR-TKA showed a superior static balance ability on a single-leg test compared to the other techniques [51]. Motion and electromyography (EMG) data were also used to show that ACL retention led to altered muscle recruitment during downhill walking in 12 BCR-TKA subjects compared with 12 CR-TKA subjects; the authors concluded that BCR-TKA may offer some neuromuscular benefits for stabilizing the knee joint [52]. However, despite maintaining AP stability, asymmetric knee motion persisted in unilateral BCR-TKA patients during gait as assessed by a combined computer tomography and dual fluoroscopic imaging system in 29 patients. The results of this study suggested that the knee motion symmetry during gait was not restored in patients with unilateral BCR-TKA [46]. Finally, at a short-term follow-up of 6 weeks, in 15 knees that received BCR-TKA (Journey II XR), improved gait ability (walking time (p < 0.01), number of steps (p < 0.05), velocity (p < 0.01) and stride length (p < 0.01) was shown compared to those who received bicruciate-stabilized (BCS)-TKA [53].
4. Discussion
This is the first report that provides a systematic description of the broad available preclinical and clinical literature on BCR-TKA. It underlines the current interest in improving kinematics and clinical outcome based on a more anatomical TKA design. Indeed, a recent survey amongst 346 experienced knee surgeons confirmed that there is a strong interest to perform BCR-TKA and the percentage of potentially eligible patients is high [54]. In our view, the current systematic review is especially insightful, as for the first time, the extensive preclinical models can be compared to the available clinical data. The importance of implant design with adequate tibial fixation to prevent aseptic loosening was highlighted. In addition, because the rationale behind BCR-TKA aims at native kinematics, intraoperative precise joint line restoration and soft tissue balancing during BCR-TKA, as well as adequate PTS, are important factors to consider during surgery to minimize increased loading and impingement of the preserved ACL. An important challenge to overcome for the implant design is the difference in laxity that is observed between the stable medial side and the more mobile lateral side in the native knee. Indeed, preclinical data suggest that using a medial constrained insert and a lateral insert with a posterior slope of +3° may aid in this challenge [36,37]. Nevertheless, the preclinical data that compare the BCR-TKA design to the CR-TKA design are conflicting, and optimal ligament balancing for an ACL- and PCL-preserved knee has yet to be defined. Thus, while these data suggest ACL retention to have theoretical kinematic advantages in TKA, the heterogenicity in the described models creates difficulty in optimal implant design. What is more, newer anatomical bearing designs with more constrained (concave) medial and convex lateral surfaces may be as important for anterior–posterior stability and kinematics as ACL retention. Unfortunately, while such designs have been described, their exact influence on kinematics is yet to be determined [25].
Several clinical studies suggest BCR-TKA may provide kinematic improvements over contemporary implants with superior movement of the lateral condyle, medial condyle and tibial internal rotation through a full range of flexion, as well as reduce AP laxity. Again, while newer-generation BCR-TKAs seem to show promising results, there are no clinical data that show superior results compared to other designs. This may be attributed to several patient, implant, surgical and methodological factors. For example, the implant which has been explored in the most clinical trials to date, i.e., the Vanguard XP, showed similar clinical and RSA results compared to a CR design in a single-blinded randomized controlled trial (n = 50) at 2 years [22].This has been confirmed by several smaller (retrospective) cohort studies in the short term up to three years (Table 1). However, at an intermediate follow-up of 5 years, a large retrospective cohort study including 1253 patients raised concerns regarding the performance of BCR-TKA, as a higher revision rate for aseptic loosening was found compared to an AS CR-TKA design of 9.7% vs. 0.1%, respectively [21]. While surgical experience was suggested to be a confounder, a later report showed a revision-free survival of 88% at 3 years, which is lower than traditional TKA designs [19]. Furthermore, lower postoperative range of motion and stiffness have been reported [20,55]. Here, it is important to stress that these findings need to be interpreted with care, as the majority of these studies are of low (level IV) methodological quality which is prone to patient and surgeon bias. Interestingly, to the best of our knowledge, the rational of improving propriocepsis due to ACL retention has yet to be confirmed in the literature. Similarly, while the young and active patient would have a theoretical advantage in the BCR-TKA design, no comparative clinical data between the older (>65 years) and younger (<65 years) were identified. In fact, the majority of studies included in this review reported on patients aged 65 years and older.
Although kinematic studies found advantages of BCR-TKA, its design does not achieve native knee function, as forces to the ACL may be increased and posterior femoral translation and internal rotation decreased. In addition, sagittal plane motion and tibiofemoral articular contact characteristics including pivoting patterns were not fully restored [25,48,49,50]. Nevertheless, kinematic analyses suggest superior static balance ability on a single-leg test of BCR-TKA compared to PS-TKA and UKA designs [51], and that compared to the CR-TKA design, ACL retention may lead to improved muscle recruitment during (downhill) walking and increased neuromuscular control
Recently, a BCS-TKA design was introduced which uses a dual-post-cam mechanism as a substitute for the ACL and PCL, with due to the design provides guidance for axial rotation and posterior translation. One kinematic analysis that compared this system to BCR-TKA found that BCR-TKA (n = 10) improved gait ability more than BCS-TKA (Journey II XR) (n = 15) at a short-term follow-up of 6 weeks [53]. As BCS-TKA may be less prone to native ACL strain, aseptic loosening and surgeon experience, future (randomized) controlled trials comparing these designs would be of great interest [56]. Moreover, as retention of the native ACL seems to have kinematic advantages over the other designs, third-generation BCR-TKA designs with an optimal (robotic or navigated) placement may prove to achieve the unmet need for a TKA design for the younger and active patient.
In conclusion, the current systematic review underlines the low methodological quality of clinical trials investigating BCR-TKA. Currently, there are insufficient data to support broad (“state of the art”) implantation of BCR-TKA, and its utility remains to be assessed [57]. Preclinical and clinical (kinematic) research suggests, however, that the design has a potential benefit to achieve improved kinematics in the young and active arthroplasty patient and warrants future research for new-generation designs with optimal (tibial) fixation and reproducible (robot or navigated) surgical placement.
Author Contributions
T.S.D.W.: Systematic search, analysis of manuscripts, manuscript writing. S.N.V.L.: Manuscript writing. G.G.V.H.: Manuscript writing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Klug, A.; Gramlich, Y.; Rudert, M.; Drees, P.; Hoffmann, R.; Weißenberger, M.; Kutzner, K.P. The Projected Volume of Primary and Revision Total Knee Arthroplasty Will Place an Immense Burden on Future Health Care Systems over the next 30 Years. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3287–3298. [Google Scholar] [CrossRef] [PubMed]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.J.K.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Lau, E.; Ong, K.; Zhao, K.; Kelly, M.; Bozic, K.J. Future Young Patient Demand for Primary and Revision Joint Replacement: National Projections from 2010 to 2030. Clin. Orthop. Relat. Res. 2009, 467, 2606–2612. [Google Scholar] [CrossRef] [PubMed]
- Sabatini, L.; Barberis, L.; Centola, M.; Bistolfi, A.; Camazzola, D.; Capella, M.; Massè, A.; Schiraldi, M. Bicruciate-Retaining Total Knee Arthroplasty: What’s New? World J. Orthop. 2021, 12, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Cherian, J.J.; Kapadia, B.H.; Banerjee, S.; Jauregui, J.J.; Harwin, S.F.; Mont, M.A. Bicruciate-Retaining Total Knee Arthroplasty: A Review. J. Knee Surg. 2014, 27, 199–205. [Google Scholar] [CrossRef]
- Dennis, D.A.; Komistek, R.D.; Colwell, C.E.; Ranawat, C.S.; Scott, R.D.; Thornhill, T.S.; Lapp, M.A. In Vivo Anteroposterior Femorotibial Translation of Total Knee Arthroplasty: A Multicenter Analysis. Clin. Orthop. Relat. Res. 1998, 356, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Boese, C.K.; Ebohon, S.; Ries, C.; De Faoite, D. Bi-Cruciate Retaining Total Knee Arthroplasty: A Systematic Literature Review of Clinical Outcomes. Arch. Orthop. Trauma Surg. 2021, 141, 293–304. [Google Scholar] [CrossRef]
- Komistek, R.D.; Allain, J.; Anderson, D.T.; Dennis, D.A.; Goutallier, D. In Vivo Kinematics for Subjects with and without an Anterior Cruciate Ligament. Clin. Orthop. Relat. Res. 2002, 404, 315–325. [Google Scholar] [CrossRef]
- Gunston, F.H. Polycentric Knee Arthroplasty: Prosthetic Simulation of Normal Knee Movement. 1971. Clin. Orthop. Relat. Res. 2006, 446, 11–12. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009, 339, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Pritchett, J.W. Bicruciate-Retaining Total Knee Replacement Provides Satisfactory Function and Implant Survivorship at 23 Years. Clin. Orthop. Relat. Res. 2015, 473, 2327–2333. [Google Scholar] [CrossRef] [PubMed]
- Sabouret, P.; Lavoie, F.; Cloutier, J.M. Total Knee Replacement with Retention of Both Cruciate Ligaments: A 22-Year Follow-up Study. Bone Joint J. 2013, 95-B, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Buechel, F.F.; Pappas, M.J. Long-Term Survivorship Analysis of Cruciate-Sparing versus Cruciate-Sacrificing Knee Prostheses Using Meniscal Bearings. Clin. Orthop. Relat. Res. 1990, 260, 162–169. [Google Scholar] [CrossRef]
- Stiehl, J.B.; Hamelynck, K.J.; Voorhorst, P.E. International Multi-Centre Survivorship Analysis of Mobile Bearing Total Knee Arthroplasty. Int. Orthop. 2006, 30, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Van Ooij, B.; de Keijzer, D.R.; Hoornenborg, D.; Sierevelt, I.N.; Haverkamp, D. Lower Revision Rates for Cemented Fixation in a Long-Term Survival Analysis of Three Different LCS Designs. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2707–2713. [Google Scholar] [CrossRef] [PubMed]
- Alnachoukati, O.K.; Emerson, R.H.; Diaz, E.; Ruchaud, E.; Ennin, K.A. Modern Day Bicruciate-Retaining Total Knee Arthroplasty: A Short-Term Review of 146 Knees. J. Arthroplast. 2018, 33, 2485–2490. [Google Scholar] [CrossRef]
- Hennessy, D.; Arauz, P.; Klemt, C.; An, S.; Kwon, Y.M. Gender Influences Gait Asymmetry Following Bicruciate-Retaining Total Knee Arthroplasty. J. Knee Surg. 2020, 33, 582–588. [Google Scholar] [CrossRef]
- Peng, Y.; Arauz, P.; An, S.; Limmahakhun, S.; Klemt, C.; Kwon, Y.M. Does Component Alignment Affect Patient Reported Outcomes Following Bicruciate Retaining Total Knee Arthroplasty? An In Vivo Three-Dimensional Analysis. J. Knee Surg. 2020, 33, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Pelt, C.E.; Sandifer, P.A.; Gililland, J.M.; Anderson, M.B.; Peters, C.L. Mean Three-Year Survivorship of a New Bicruciate-Retaining Total Knee Arthroplasty: Are Revisions Still Higher Than Expected? J. Arthroplasty 2019, 34, 1957–1962. [Google Scholar] [CrossRef]
- Christensen, J.C.; Brothers, J.; Stoddard, G.J.; Anderson, M.B.; Pelt, C.E.; Gililland, J.M.; Peters, C.L. Higher Frequency of Reoperation with a New Bicruciate-Retaining Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 2017, 475, 62–69. [Google Scholar] [CrossRef]
- Eggenberger, E.E.; Hurst, J.M.; Morris, M.J.; Berend, K.R.; Lombardi, A.V.; Crawford, D.A. Midterm Outcomes of a Bicruciate-Retaining Compared with the Bicruciate-Sacrificing Knee System. J. Arthroplast. 2022, 37, S245–S249. [Google Scholar] [CrossRef] [PubMed]
- Troelsen, A.; Ingelsrud, L.H.; Thomsen, M.G.; Muharemovic, O.; Otte, K.S.; Husted, H. Are There Differences in Micromotion on Radiostereometric Analysis Between Bicruciate and Cruciate-Retaining Designs in TKA? A Randomized Controlled Trial. Clin. Orthop. Relat. Res. 2020, 478, 2045–2053. [Google Scholar] [CrossRef] [PubMed]
- Kalaai, S.; Bemelmans, Y.F.L.; Scholtes, M.; Boonen, B.; van Haaren, E.H.; Schotanus, M.G.M. A Short-Term Radiological and Clinical Comparison between the Bi-Cruciate and Cruciate Retaining Total Knee Arthroplasty a Retrospective Case Controlled Study. J. Clin. Orthop. Trauma 2021, 18, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Kalaai, S.; Scholtes, M.; Borghans, R.; Boonen, B.; van Haaren, E.; Schotanus, M. Comparable Level of Joint Awareness between the Bi-Cruciate and Cruciate Retaining Total Knee Arthroplasty with Patient-Specific Instruments: A Case-Controlled Study. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1835–1841. [Google Scholar] [CrossRef]
- Kono, K.; Inui, H.; Tomita, T.; Yamazaki, T.; Taketomi, S.; Tanaka, S. Bicruciate-Retaining Total Knee Arthroplasty Reproduces in vivo Kinematics of Normal Knees to a Lower Extent than Unicompartmental Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3007–3015. [Google Scholar] [CrossRef]
- Nowakowski, A.M.; Stangel, M.; Grupp, T.M.; Valderrabano, V. Comparison of the Primary Stability of Different Tibial Baseplate Concepts to Retain Both Cruciate Ligaments during Total Knee Arthroplasty. Clin. Biomech. 2013, 28, 910–915. [Google Scholar] [CrossRef]
- Amiri, S.; Wilson, D.R. A Computational Modeling Approach for Investigating Soft Tissue Balancing in Bicruciate Retaining Knee Arthroplasty. Comput. Math. Methods Med. 2012, 2012, 652865. [Google Scholar] [CrossRef]
- Fleming, B.; Beynnon, B.; Howe, J.; McLeod, W.; Pope, M. Effect of Tension and Placement of a Prosthetic Anterior Cruciate Ligament on the Anteroposterior Laxity of the Knee. J. Orthop. Res. 1992, 10, 177–186. [Google Scholar] [CrossRef]
- Tsai, T.Y.; Liow, M.H.L.; Peng, Y.; Arauz, P.; Li, G.; Kwon, Y.M. In-Vivo Elongation of Anterior and Posterior Cruciate Ligament in Bi-Cruciate Retaining Total Knee Arthroplasty. J. Orthop. Res. 2018, 36, 3239–3246. [Google Scholar] [CrossRef]
- Toyoda, S.; Kaneko, T.; Igarashi, T.; Takada, K.; Yoshizawa, S. Higher Patellofemoral Compressive Force Does Not Affect Anterior Knee Pain in Anatomical Bi-Cruciate Retaining Total Knee Arthroplasty: In Vivo Prospective Analysis of Guided Motion Prosthesis. Clin. Biomech. 2021, 88, 105444. [Google Scholar] [CrossRef]
- Klemt, C.; Bounajem, G.; Tirumala, V.; Xiong, L.; Oganesyan, R.; Kwon, Y.M. Posterior Tibial Slope Increases Anterior Cruciate Ligament Stress in Bi-Cruciate Retaining Total Knee Arthroplasty: In Vivo Kinematic Analysis. J. Knee Surg. 2022, 35, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Yamagami, R.; Inui, H.; Taketomi, S.; Kono, K.; Kawaguchi, K.; Sameshima, S.; Kage, T.; Tanaka, S. Proximal Tibial Morphology Is Associated with Risk of Trauma to the Posteromedial Structures during Tibial Bone Resection Reproducing the Anatomical Posterior Tibial Slope in Bicruciate-Retaining Total Knee Arthroplasty. Knee 2022, 36, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Postolka, B.; Schütz, P.; Fucentese, S.F.; Freeman, M.A.R.; Pinskerova, V.; List, R.; Taylor, W.R. Tibio-Femoral Kinematics of the Healthy Knee Joint throughout Complete Cycles of Gait Activities. J. Biomech. 2020, 110, 109915. [Google Scholar] [CrossRef] [PubMed]
- Zumbrunn, T.; Varadarajan, K.M.; Rubash, H.E.; Malchau, H.; Li, G.; Muratoglu, O.K. Regaining Native Knee Kinematics Following Joint Arthroplasty: A Novel Biomimetic Design with ACL and PCL Preservation. J. Arthroplast. 2015, 30, 2143–2148. [Google Scholar] [CrossRef] [PubMed]
- Arnout, N.; Victor, J.; Vermue, H.; Pringels, L.; Bellemans, J.; Verstraete, M.A. Knee Joint Laxity Is Restored in a Bi-Cruciate Retaining TKA-Design. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2863–2871. [Google Scholar] [CrossRef]
- Wada, K.; Hamada, D.; Takasago, T.; Nitta, A.; Goto, T.; Tonogai, I.; Tsuruo, Y.; Sairyo, K. The Medial Constrained Insert Restores Native Knee Rotational Kinematics after Bicruciate-Retaining Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1621–1627. [Google Scholar] [CrossRef]
- Takasago, T.; Hamada, D.; Wada, K.; Nitta, A.; Tamaki, Y.; Goto, T.; Tsuruo, Y.; Sairyo, K. Insufficient Lateral Joint Laxity after Bicruciate-Retaining Total Knee Arthroplasty Potentially Influences Kinematics during Flexion: A Biomechanical Cadaveric Study. Knee 2021, 28, 311–318. [Google Scholar] [CrossRef]
- Zhang, Q.; Chen, Z.; Zhang, Z.; Jin, Z.; Muratoglu, O.K.; Varadarajan, K.M. Leveraging Subject-Specific Musculoskeletal Modeling to Assess Effect of Anterior Cruciate Ligament Retaining Total Knee Arthroplasty during Walking Gait. Proc. Inst. Mech. Eng. H. 2020, 234, 1445–1456. [Google Scholar] [CrossRef]
- Okada, Y.; Teramoto, A.; Takagi, T.; Yamakawa, S.; Sakakibara, Y.; Shoji, H.; Watanabe, K.; Fujimiya, M.; Fujie, H.; Yamashita, T. ACL Function in Bicruciate-Retaining Total Knee Arthroplasty. J. Bone Joint Surg. Am. 2018, 100, E114. [Google Scholar] [CrossRef]
- Liu, H.W.; Ni, M.; Zhang, G.Q.; Li, X.; Chen, H.; Zhang, Q.; Chai, W.; Zhou, Y.G.; Chen, J.Y.; Liu, Y.L.; et al. Kinematic Analysis of Anterior Cruciate Ligament Reconstruction in Total Knee Arthroplasty. Am. J. Transl. Res. 2016, 8, 2275. [Google Scholar]
- Watanabe, M.; Kuriyama, S.; Nakamura, S.; Nishitani, K.; Tanaka, Y.; Sekiguchi, K.; Ito, H.; Matsuda, S. Abnormal Knee Kinematics Caused by Mechanical Alignment in Symmetric Bicruciate-Retaining Total Knee Arthroplasty Are Alleviated by Kinematic Alignment. Knee 2020, 27, 1385–1395. [Google Scholar] [CrossRef] [PubMed]
- Heyse, T.J.; Slane, J.; Peersman, G.; Dirckx, M.; van de Vyver, A.; Dworschak, P.; Fuchs-Winkelmann, S.; Scheys, L. Kinematics of a Bicruciate-Retaining Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1784–1791. [Google Scholar] [CrossRef]
- Halewood, C.; Traynor, A.; Bellemans, J.; Victor, J.; Amis, A.A. Anteroposterior Laxity After Bicruciate-Retaining Total Knee Arthroplasty Is Closer to the Native Knee Than ACL-Resecting TKA: A Biomechanical Cadaver Study. J. Arthroplast. 2015, 30, 2315–2319. [Google Scholar] [CrossRef] [PubMed]
- Hamada, D.; Wada, K.; Takasago, T.; Goto, T.; Nitta, A.; Higashino, K.; Fukui, Y.; Sairyo, K. Native Rotational Knee Kinematics Are Lost in Bicruciate-Retaining Total Knee Arthroplasty When the Tibial Component Is Replaced. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3249–3256. [Google Scholar] [CrossRef] [PubMed]
- Kono, K.; Inui, H.; Tomita, T.; Yamazaki, T.; Taketomi, S.; Yamagami, R.; Kawaguchi, K.; Kage, T.; Arakawa, T.; Tanaka, S. Effect of Weight-Bearing in Bicruciate-Retaining Total Knee Arthroplasty during High-Flexion Activities. Clin. Biomech. 2022, 92, 105569. [Google Scholar] [CrossRef]
- Arauz, P.; Peng, Y.; Kwon, Y.M. Knee Motion Symmetry Was Not Restored in Patients with Unilateral Bi-Cruciate Retaining Total Knee Arthroplasty-in Vivo Three-Dimensional Kinematic Analysis. Int. Orthop. 2018, 42, 2817–2823. [Google Scholar] [CrossRef]
- Smith, L.A.; Nachtrab, J.; LaCour, M.; Cates, H.; Freeman, M.G.; Komistek, R.D. In Vivo Knee Kinematics: How Important Are the Roles of Femoral Geometry and the Cruciate Ligaments? J. Arthroplast. 2021, 36, 1445–1454. [Google Scholar] [CrossRef]
- Kono, K.; Inui, H.; Tomita, T.; Yamazaki, T.; Konda, S.; Taketomi, S.; Tanaka, S.; D’Lima, D.D. In Vivo Kinematics and Cruciate Ligament Forces in Bicruciate-Retaining Total Knee Arthroplasty. Sci. Rep. 2021, 11, 5645. [Google Scholar] [CrossRef]
- Tsai, T.Y.; Liow, M.H.L.; Li, G.; Arauz, P.; Peng, Y.; Klemt, C.; Kwon, Y.M. Bi-Cruciate Retaining Total Knee Arthroplasty Does Not Restore Native Tibiofemoral Articular Contact Kinematics During Gait. J. Orthop. Res. 2019, 37, 1929–1937. [Google Scholar] [CrossRef]
- Kwon, Y.M.; Arauz, P.; Peng, Y.; Klemt, C. In Vivo Kinematics of Deep Lunges and Sit-to-Stand Activities in Patients with Bicruciate-Retaining Total Knee Arthroplasty. Bone Joint J. 2020, 102-B, 59–65. [Google Scholar] [CrossRef]
- Baumann, F.; Bahadin, Ö.; Krutsch, W.; Zellner, J.; Nerlich, M.; Angele, P.; Tibesku, C.O. Proprioception after Bicruciate-Retaining Total Knee Arthroplasty Is Comparable to Unicompartmental Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1697–1704. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.C.; Della Valle, C.J.; Wimmer, M.A. Level and Downhill Walking to Assess Implant Functionality in Bicruciate- and Posterior Cruciate-Retaining Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 2884–2889. [Google Scholar] [CrossRef] [PubMed]
- Amemiya, K.; Kaneko, T.; Omata, M.; Igarashi, T.; Takada, K.; Ikegami, H.; Musha, Y. Anatomical Bi-Cruciate Retaining TKA Improves Gait Ability Earlier than Bi-Cruciate Stabilized TKA Based on Triaxial Accelerometery Data: A Prospective Cohort Study. Asia-Pacific J. Sport. Med. Arthrosc. Rehabil. Technol. 2021, 25, 35–41. [Google Scholar] [CrossRef] [PubMed]
- De Faoite, D.; Ries, C.; Foster, M.; Boese, C.K.; Boese, C.K. Indications for Bi-Cruciate Retaining Total Knee Replacement: An International Survey of 346 Knee Surgeons. PLoS ONE 2020, 15, e0234616. [Google Scholar] [CrossRef]
- Lavoie, F.; Al-Shakfa, F.; Moore, J.R.; Mychaltchouk, L.; Iguer, K. Postoperative Stiffening after Bicruciate-Retaining Total Knee Arthroplasty. J. Knee Surg. 2018, 31, 453–458. [Google Scholar] [CrossRef]
- Clarke, C.; Pomeroy, V.; Clark, A.; Creelman, G.; Hancock, N.; Horton, S.; Killett, A.; Mann, C.; Payerne, E.; Toms, A.; et al. CAPAbility: Comparison of the JOURNEY II Bi-Cruciate Stabilised and GENESIS II Total Knee Arthroplasty in Performance and Functional Ability: Protocol of a Randomised Controlled Trial. Trials 2020, 21, 222. [Google Scholar] [CrossRef]
- Osmani, F.A.; Thakkar, S.C.; Collins, K.; Schwarzkopf, R. The Utility of Bicruciate-Retaining Total Knee Arthroplasty. Arthroplast. Today 2016, 3, 61–66. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).