1. Introduction
Outcomes of total knee replacement (TKR) remain suboptimal, with 10–20% of patients continuing to experience pain or functional limitations after primary TKR [
1], despite good long-term survivorship [
2]. Approximately 45% of patients dissatisfied with TKR report anterior knee pain (AKP) affecting their daily activities [
3] which is likely related to patellofemoral complications. Patients suffering from AKP have difficulties with activities that increase patellofemoral joint (PFJ) forces such as walking up and down stairs, rising from a seated position, exiting a car or cycling [
4]. Patellofemoral complications are historically one of the most common reasons for poor TKR outcome [
5]. AKP appears to occur with equal incidence as patellofemoral complications, independent to whether the patella is resurfaced or left native [
6]. The patella itself is relatively poorly innervated, whereas the surrounding extensor hood of soft tissue is highly sensitive to increased strain.
Many factors affect the balance of the PJF during TKR including the amount of trochlea resection, the rotation and size of the femoral component. The distal femoral resection and tibial resection influence the joint line, which can change soft tissue tension of the extensor mechanism. When the patella is resurfaced, the amount of patella resection, size, shape and placement of the patella component influence patella tracking and soft tissue tension. Patella under-resection and thereby over-stuffing of the PFJ can cause chronic postoperative AKP and decreased range of motion due to higher than physiologic extensor mechanism forces [
7]. Patella over-resection increases the risk for fracture and may lead to under-tensioning the PFJ, resulting in lower than physiological extensor mechanism forces and muscle pain [
8]. Patella maltracking is multifactorial and is defined as abnormal tracking of the patella in the femoral groove during knee flexion and extension and can lead to increased wear of the patellar component, subluxation and dislocation [
9].
Despite these findings, the PFJ and extensor mechanism’s role as primary contributors to overall knee function is often overlooked, and limited attention has been paid to improving balancing and cutting techniques for the PFJ during TKR. Currently, with traditional surgical techniques, there is no method of quantifying or addressing patella compression forces. While prior studies have described changes in Q-angle and fluoroscopic patellar angle measurements to assess the PFJ postoperatively [
10,
11], a dynamic, intraoperative assessment of PFJ forces during TKR has not been described. An intraoperative means of assessing PFJ forces during TKR could allow adjustments of the patella cut depth and angle to more closely replicate native PFJ kinematics, which may improve overall patient outcomes and decrease PFJ-related complications.
The current study utilized a novel PFJ load sensor device that resembles a patella implant component. When applied to the patella, the sensor is capable of dynamically assessing PFJ forces before and after placement of tibial and femoral TKR components, which can allow for patella cut adjustments and reproduction of physiologic PFJ and extensor mechanism forces. The aims of this study were (1) to characterize changes in PFJ forces in an experimental in vitro setup and in a human cadaveric model before and after TKR component placement and (2) to assess whether the use of novel PFJ cutting guides can reproduce physiologic PFJ forces in a cadaveric model. The study hypothesized that native and postoperative resection PFJ forces can be measured and differ based on patella implant thickness and angulation of the patella cut. The goal of this translational research is to develop a system that can improve TKR outcomes by balancing the PFJ and extensor mechanism as an integral but often overlooked part of TKR surgery. Significant patient benefits might result, based on data that patella over/under-loading is closely associated with poor functional outcome [
12,
13,
14].
2. Materials and Methods
2.1. Patellofemoral Joint Load Sensor
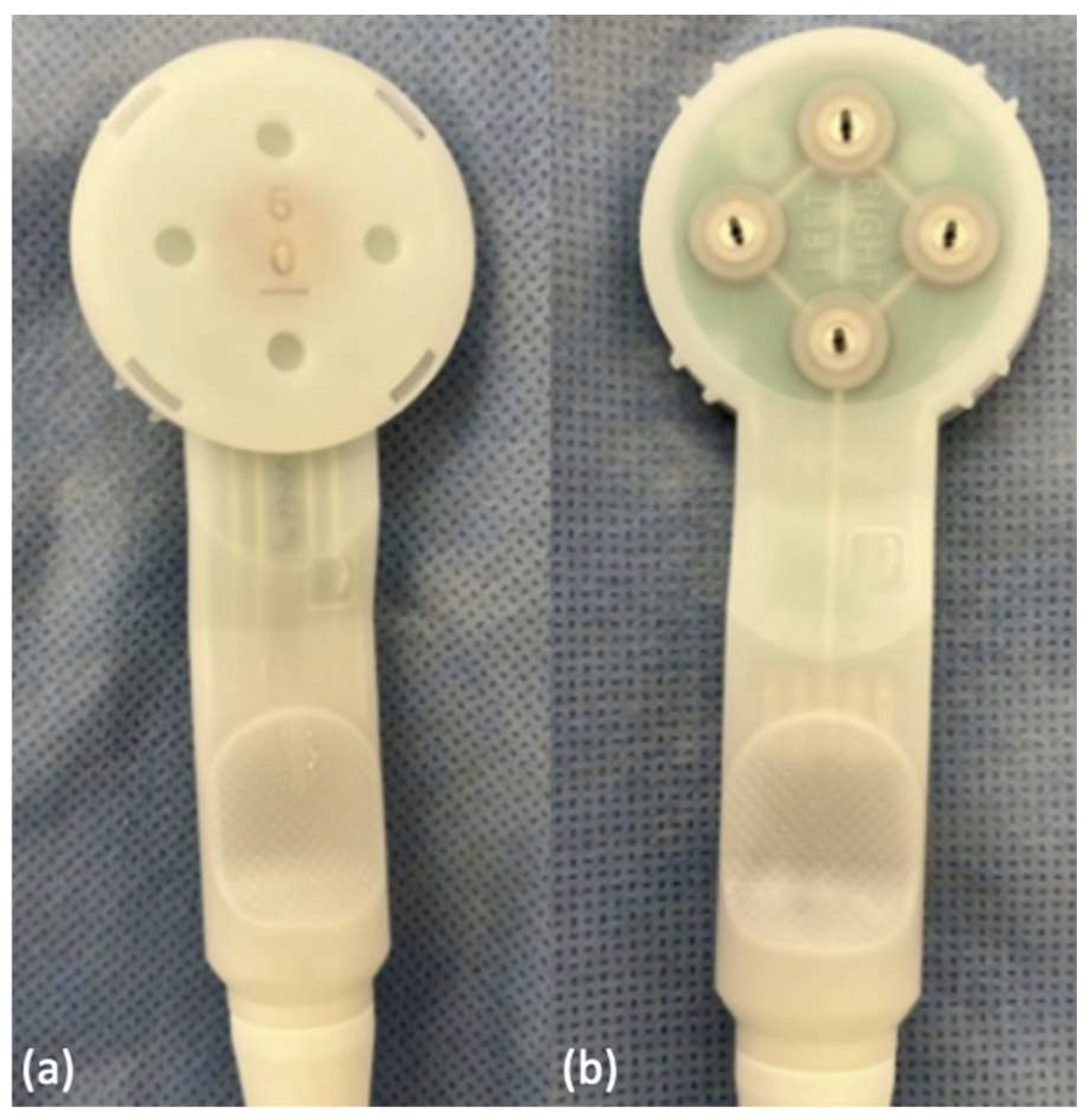
The novel PFJ load sensor (quad sense, Eventum Orthopaedics Ltd., Ilkley, UK) was initially developed in 2021 and consists of a paddle with four evenly placed pressure sensors in the superior, inferior, medial and lateral quadrants (
Figure 1a) that can be attached to the underside of the everted patella via four stainless steel tines (
Figure 1b). The sensor itself is constructed from ABS resin contoured into a disc matching the shape of the patellar undersurface, and is designed to measure compressive forces in four separate quadrants of the patellofemoral joint (
Figure 2). Adjustment shims with different thicknesses (6 mm, 7 mm, 8 mm, 9 mm) and angles (neutral, 1.25 degrees, 2.5 degrees) can be attached to the underside of the sensor paddle. Sensor data is captured after a trial of knee flexion-extension is generated, and usually three trials can be performed in a single 12 s recording period. This sensor data is recorded and a visual plot of sensor force against time can be generated in real time and displayed on a panel PC, with four lines shown corresponding to each of the four quadrant sensors, respectively.
2.2. In Vitro Experimental Set-Up
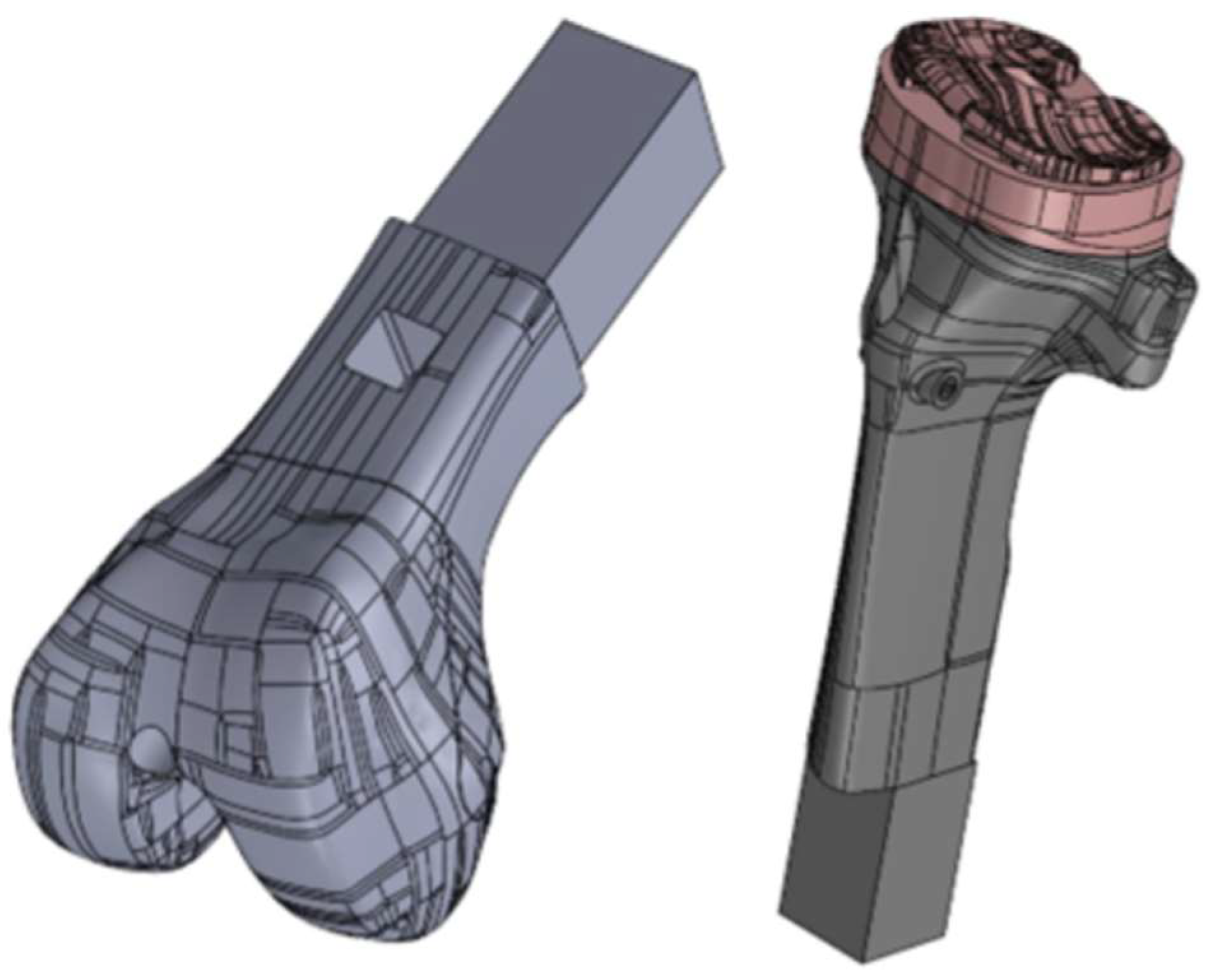
An in vitro evaluation of the sensor was conducted utilizing a model knee. A model Left Cadaver Leg Version 3 (Medical Models, Bristol, UK) with custom 3D printed femoral and tibial component inserts was used (
Figure 3). A simulated patella with tendons was attached to the model knee, with a spring used to simulate the quadriceps tension. The spring had a free length of 107 mm and a 1.64 mm wire gauge diameter. To accommodate the sensor, the patella was resected by 6 mm, using the lateral facet as reference. Sensor readings were taken using the 6 mm, 7 mm, 8 mm, 9 mm and 6 mm 2.5° shims, following a methodology of moving the model knee through full flexion and extension three times, at a consistent pace and flexion angle.
2.3. Cadaveric Patella Load Assessment
The current study utilized two pelvis-to-toe, unpreserved cadaveric specimens (Specimen 1: 75 year old male, body mass index 22 kg/m
2, no previous knee surgery, mild bilateral medial compartment arthritis; Specimen 2: 76 year old male, body mass index 26 kg/m
2, no previous knee surgery, mild right medial compartment arthritis, moderate left tricompartmental arthritis) to test whether the quad sense device was able to capture PFJ forces in a proposed TKR workflow to adjust the patella cut with a custom patella clamp to reproduce more physiologic PFJ forces during TKR. On each extremity, a standard medial arthrotomy approach to the knee was performed. The patella was mobilized and everted. A preliminary 6 mm patella cut was made using a patella clamp (Enztec, Premium Patella Saw Guide, Christchurch, New Zealand) with a custom cutting guide attached to the clamp for a 6 mm resection depth and a standard oscillating saw (
Figure 4). The quad sense sensor with 6 mm neutral shim was then attached to the cut undersurface of the patella using four metal tines as part of the sensor paddle. Force data of the native PFJ was then recorded from three range of motion trials from full extension to full flexion in all four quadrants of the sensor. A standardized flowsheet was followed, with the intention to record native PFJ load measurements and compare them to TKR PFJ load measurements to see if differences in these measurements could inform whether an adjustment cut was warranted (
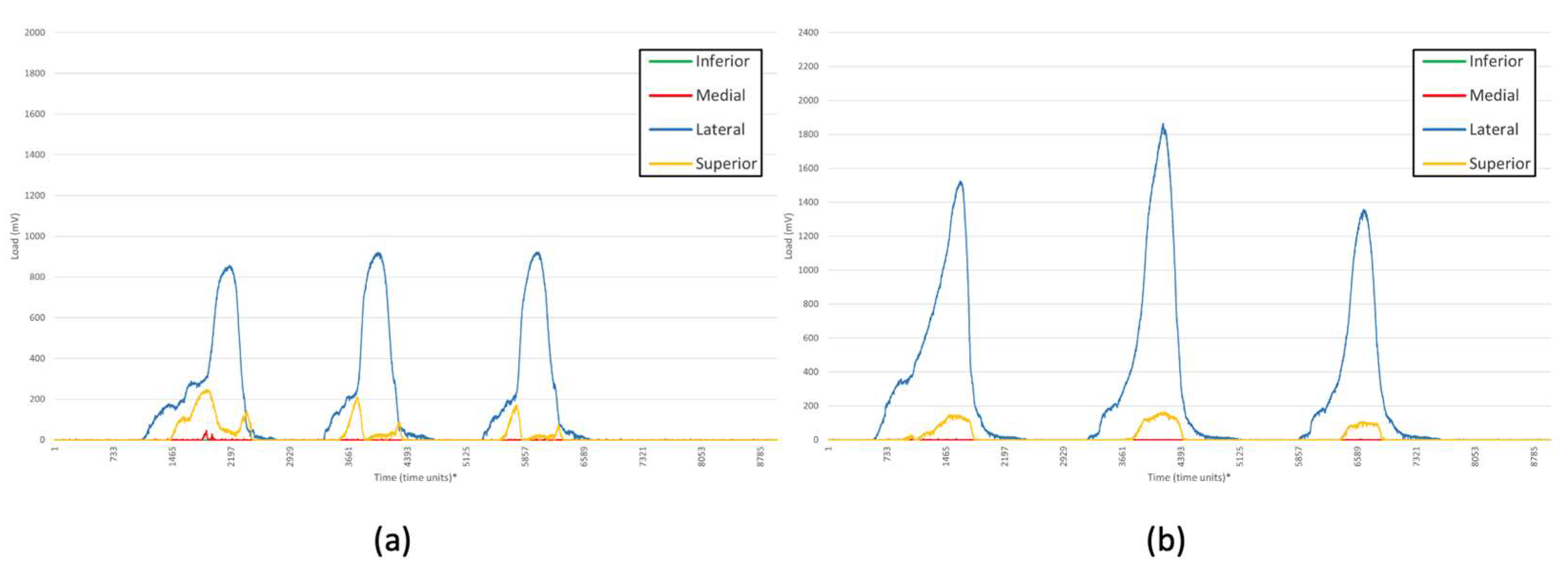
Figure 5).
TKR surgery was then performed, with a posterior stabilized TKR (Legion, posterior stabilized, Smith & Nephew, Memphis, TN). The quad sense sensor was re-attached to the underside of the patella in the same location and orientation. PFJ load data was then collected during three range of motion trials utilizing each of the respective shim-angle combinations in the following order: 6 mm neutral, 7 mm neutral, 8 mm neutral, 9 mm neutral, 6 mm 1.25° angle, 6 mm 2.5° angle, 7 mm 1.25° angle, 7 mm 2.5° angle, 8 mm 1.25° angle, 8 mm 2.5° angle, 9 mm 1.25° angle, 9 mm 2.5° angle, with the angled shim orientations recorded in the following order: (1) facing medial (thicker side on inferior aspect of patella), (2) facing lateral (thicker superiorly), (3) facing superior (thicker medially), and (4) facing inferiorly (thicker laterally). Upon completion of range of motion trials for each of these shim-angle combinations, a total of 37 measurements of PFJ load were obtained beginning with the native knee neutral 6 mm measurement, and ending with the post-TKR 9 mm 2.5° angle inferior measurement.
2.4. Cadaveric Patella Adjustment Cut
Upon completion of the previous measurements, load data from the quad sense device were reviewed on the panel PC. The load profile of the native measurement obtained prior to TKR instrumentation was compared to the load profile with trial components in place and with different shim angle combinations. Appropriate adjustment cuts were made utilizing the patella clamp with custom cutting guides matching the thickness and orientation of the adjustment shims (
Figure 6). For the left knee in Specimen 1, forces were remeasured and compared, and a 3 mm 2.5° laterally angled adjustment cut, with more bone taken superiorly, was made. Forces were then measured with a shim angle combination set to 9 mm neutral for comparison. For the right knee in Specimen 1, a 4 mm neutral adjustment cut was made to evaluate for over-stuffing, and forces were remeasured after the adjustment cut utilizing shim angle combinations set to 6 mm neutral, 7 mm neutral, 8 mm neutral, and 9 mm neutral. For both the left and right knee in Specimen 2, after forces were measured, a 4 mm 1.25° inferiorly angled adjustment cut, with more bone taken laterally, was performed. Forces present after the adjustment cut were measured utilizing a 9 mm neutral shim.
2.5. Data Collection and Presentation
After each range of motion trial, PFJ load measurements were obtained and the raw data was collected in the form of CSV files which were converted to Microsoft Excel Workbook files (.xlsx) for data processing (Microsoft Excel version 2207, Microsoft, Redmond, WA). Load data was collected over a 12 s time period, during which three trials of knee flexion extension cycling were performed. Load data was recorded initially by the sensor in units of millivolts (mV), which were calibrated or converted into Newtons (N) utilizing a sensor-specific conversion factor of 20:1 (or division by 20). The initial graphs reviewed on the panel PC are shown using mV. Within the 12 s time period the trial is performed, 8785 time units of data were collected, such that there were 8785 corresponding points where load data was measured. Therefore, 1 s of real time contained 732 time units of data. A line graph was created from the raw data for each sensor reading, such that four line plots were visualized representing load plotted against time, corresponding to the four respective pressure sensors. From a qualitative perspective, these plotted graphs could be compared visually in real time by the surgeon to interpret changes in PFJ load measurements for different shim-angle combinations which were obtained.
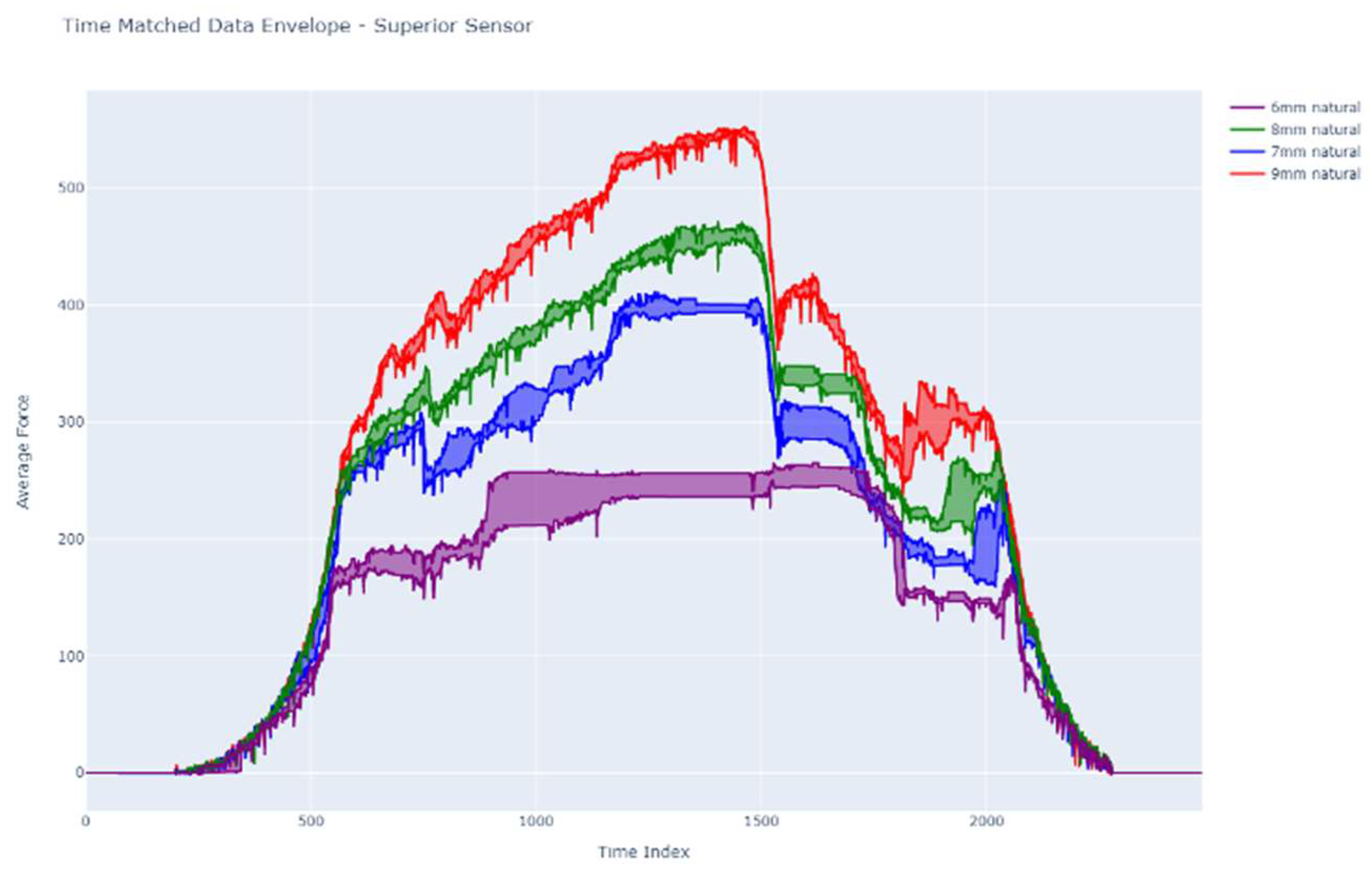
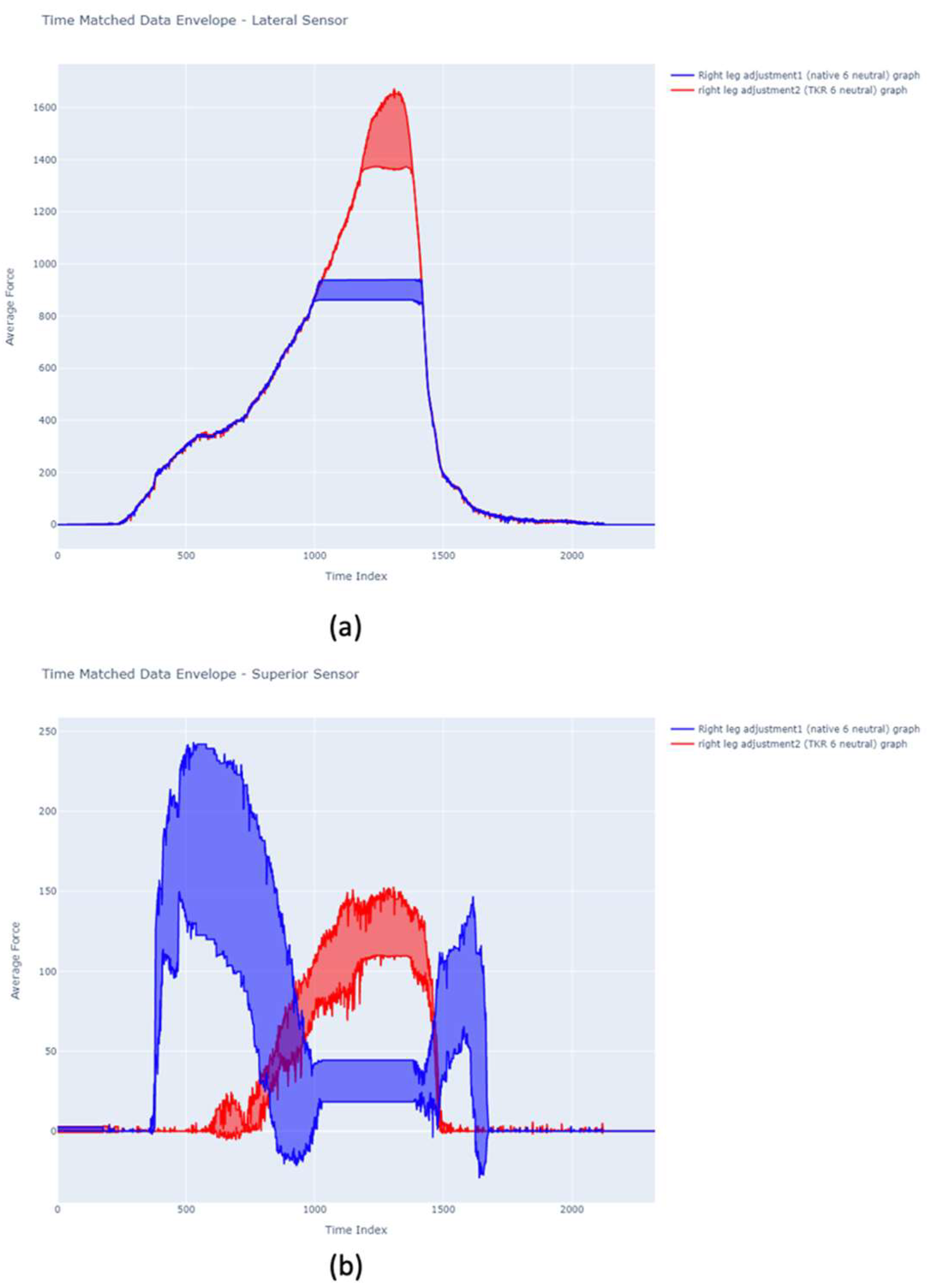
2.6. Dynamic Time Warping Comparison
In order to clearly compare the measurements between different shim-angle combinations, a dynamic time warping algorithm was applied to the data for Specimen 1. The purpose of performing this dynamic time warping was to allow for clearer comparison of data during each trial and to assess the uncertainty that operational differences may have contributed to the data. The main purpose was to compare the measurements obtained in different trials (e.g., for different shim sizes) and standardize them by time, since variation was expected in how long it would take a surgeon to cycle the knee through flexion and extension. The algorithm implemented included the following steps:
Data for time periods without movement (during which the knee was actively being flexed or extended) were detected and filtered out.
Troughs in the values obtained for the combined summed load sensors were detected using a peak detection algorithm with specified prominence.
The signal was segmented into single movement pieces, and labeled based on the different test conditions.
Dynamic time warping was implemented to match each segmented signal in time. In doing so, this reduced the need for the surgeon performing the trial to move the knee at exactly the same speed each time by dynamically stretching or compressing the signal, to achieve optimal Euclidean distance matching.
Time matched signals from each test were combined to provide an average and standard deviation for each point in the knee motion, including the maximal load obtained for each trial.
2.7. Statistical Analysis
Quad sense data was obtained from all four quadrants of the sensor during the range of motion trials for the cadaveric experiment and was recorded in the system. The raw data was obtained as mentioned above and line graphs plotting load against time were created. Dynamic time warping was also performed using the aforementioned algorithm, and from this data peak maximal load was recorded from each of the three respective range of motion trials performed within each recording. The mean maximal load ± standard deviation during these three range of motion trials for each respective shim-angle combination was calculated and compared utilizing either a one-way ANOVA (alpha = 0.05), or in the setting of multiple shim-angle combinations a two-way ANOVA with multiple comparisons (alpha = 0.05) was performed. For comparisons between two shim-angle combinations, such as comparing the native versus TKR 6 mm neutral shim measurements, a paired t-test (alpha = 0.05) was performed.
4. Discussions
Although TKR has become a well-established treatment for end stage degenerative disease of the knee with good survivorship [
2], a great number of patients remain dissatisfied following the procedure [
1]. AKP represents a leading cause of dissatisfaction that can be associated with PFJ complications which ultimately require revision surgery [
3,
4]. Restoring physiologic soft tissue tension and balance of the PFJ during TKR and thereby avoiding patella “over-stuffing” or “under-tensioning” should be a primary objective during surgery; however, few if any advancements in surgical strategies to address PFJ balancing have been made. At present, limited understanding exists on how to address the specific PFJ anatomy of each individual patient, and significant variation exists by surgeon on whether patellar resurfacing is performed. Furthermore, there is limited agreement on what constitutes adequate patellar resurfacing, with many surgeons performing the procedure using a freehand technique [
15]. The findings of this preliminary cadaveric study revealed that a novel force sensor device is capable of recording PFJ loads in four quadrants intraoperatively. No previously published studies have assessed the feasibility of utilizing this device, and we present findings validating its use in both a knee model and cadaveric specimen. Furthermore, we demonstrated how these measurements can guide surgical planning, with the ability to adjust the patella resection to achieve more physiologic, native loading and balance during TKR. Following assessment of the native PFJ loads in this study compared with TKR trial components in place, PFJ loads increased significantly with use of greater thickness adjustment shims. Angled adjustment shims revealed differential loads in the superior and lateral quadrant, which could guide adjustment cuts to “fine-tune” the preliminary patella using custom cutting guides with adjustable thickness and angles. Furthermore, we observed in our left knee study that performing an angled adjustment cut based on shim measurements could reproduce expected loads when re-measured with a neutral shim matched in resection thickness. Our study also observed the effects of under-stuffing or under-tensioning the patella, as uniformly reduced PFJ loads were measured after a large 4 mm adjustment cut was made in our right knee study.
PFJ loads increased significantly with greater shim thickness with TKR trial components in place compared to the native PFJ load measurements. Soft tissue tension in the extensor hood of the soft tissue structures surrounding the patella, quadriceps muscle and tendon, medial and lateral retinaculum and patella tendon, have been implicated in AKP [
7]. Patella resection remains one of the least controlled aspects of TKR and it is widely acknowledged in the literature that improved surgical accuracy would reduce the risk of postoperative patella complications [
16]. Amongst experienced surgeons, errors in patella resection occur in 10% of cases [
17]
, with increased patellar resection angle reported to be the sole independent risk factor for AKP [
18]. Inaccurate surgical patella resection, which is confounded by a lack of consensus, is responsible for a high incidence of patella-related complications, with some studies reporting that up to 80% of resurfaced patella are greater in size than their pre-surgical measurement with associated post-operative AKP [
19]. “Over-stuffing” the PFJ through under-resection of the patella can lead to AKP following TKR [
20]. While over-resection of the patella should be avoided due to the risk of fracture, [
8] the quad sense device allowed for characterization of PFJ loads for comparison to the patient-specific native PFJ loads. This provides the surgeon with the ability to make adjustments in resection depth and angle of the patella resection, which could decrease the risk for patella under-resection and “over-stuffing”. Pre-operative alignment may also play a role in PFJ loads which are encountered. Notably, within the two cadaveric experiments conducted, we noted increased lateral PFJ loads. While the reason these lateral PFJ loads were observed is not immediately evident, this increase may be due to overall valgus alignment of the specimens, as lateral patella tracking was appreciable pre-operatively. Altered loads of the PFJ and extensor hood, even after an optimally implanted TKR may explain why patients rarely experience the “forgotten knee” [
21].
Various methods for evaluating the quality of PFJ management following TKR have been studied, particularly to predict excessive PFJ loads and patellar maltracking which contribute to complications including anterior knee pain [
12,
13,
14]. Q-angle, lateral patellar tilt, and patellar displacement have been measured in the post-operative or intraoperative setting to assess adequate patellar tracking [
3,
14]. An increase in Q-angle is associated with complications such as anterior knee pain following TKR, and this increase can be multifactorial occurring due to malrotated femoral or tibial components as well as an inadequately managed patella [
3]. Lateral patellar tilt and patellar displacement, measured on a skyline axial radiograph, have also been implicated as important factors in patellar tracking, with lateral patellar tilt > 10° and patellar displacement > 3 mm associated with patellar maltracking [
13,
22]. Lateral patellar tilt and patellar displacement are determined by patellar resection angle, patellar component medialization, as well as positioning of the femoral component [
14]. A prior study has also used surgical navigation systems to assess patellar tracking intraoperatively, as well as use of a force transducer to quantify patellofemoral contact pressures [
23]. Compared to these prior techniques implemented to improve patellar tracking and reduce PFJ loads, none have implemented a technique where dynamic measurements are obtained intraoperatively to guide adjustment resection of the patella in a patient-specific fashion.
Patella maltracking occurring in the setting of too little tension or “under-tensioning” of the patella leads to reduced function and mechanical disadvantage as well [
8]. Maltracking or malorientation of the extensor hood produces soft tissue pain and reduction in function as well as the prospect of increased wear in the patella resurfacing implant [
9]. Important factors which contribute to patellar instability are component malposition. Oversized femoral components and/or its rotation are thought to cause patella tilting onto the trochlear grove, and resultant complications including AKP and instability. Rotation of the femoral component varies based on the alignment strategy used (mechanical or anatomical), with internal rotation of the femoral component demonstrated to correlate with poorer outcomes [
15], and whilst less common, internal rotation of the tibial component, can cause increased strain on the PFJ. The quad sense allows characterization of loads in four quadrants of the patella that can alert the surgeon during trialing if non-physiologic forces in the lateral quadrant occur that can be related to femoral component malposition. Rotating platforms were hypothesized as a means of compensating for malrotation, although TKRs using these have shown no improved outcomes as compared to fixed bearing implants [
24]. In the most recent designs of TKR, increased emphasis has been placed on a patella and soft tissue friendly design of the trochlea and on redesigns of the patella implant [
25]. There is increasing focus on the amount of trochlea resection at TKR and the positioning and sizing of the femoral component, in addition to the establishment of the femoral implant accurately on the joint line [
26]. While the importance of the extensor mechanism and reproduction of adequate PFJ loads appears to have received more attention, further clinical investigations are needed to assess whether the quad sense device can lead to improved patient functional outcomes.
The study we performed had several limitations. For one, the findings were limited by the use and number of cadaveric specimens. Native PFJ loading patterns were also obtained in knees with mild degenerative disease in the medial compartment, which cannot be generalizable as native loading patterns in healthy, non-painful knees. The technique we discuss may not provide a true assessment of native PFJ dynamic loading given these initial measurements were made in knees that were already arthritic. However, with traditional patella surgery techniques, no method for assessing PFJ loading exists, and this technique offers a considerable step forward. In particular, the measurement of “native”, patient-specific PFJ loading patterns prior to TKR cuts may allow for individualized adjustments of patella loading using the described device and workflow. While the diseased joint state must be taken into account when obtaining “native” PFJ loading patterns, no other strategies to make intraoperative adjustments have been proposed and developed. Currently, surgeons rely on reproducing the measured thickness of the native patella and substitute a polyethylene implant with the assumption that this will reproduce PFJ loading. The results of this study show this is conclusively not the case, and in every example, PFJ loading is significantly altered by TKR with patella resurfacing carried out with this method. Comparatively, this technique actually offers real-time evaluation of PFJ loading, such that the resurfaced patella can be adjusted as needed in response to observed PFJ loads. Gaining data on the abnormal loading forces following TKR using this method will allow the surgeon to alter the patella resection to address these changes. Abnormal tissue loading has been shown to relate strongly to extensor hood pain and function [
12,
13,
14], and further evaluations of native PFJ loading without degenerative disease may be needed to establish true normal PFJ loading patterns.
Additional limitations included that PFJ force measurements were time based and not associated with knee flexion angle during range of motion trials. However, all knee range of motion trials were performed by the senior author and were consistent throughout the study. During range of motion trials, the arthrotomy performed was provisionally closed with two towel clamps approximating the superior pole of the patella and medial retinaculum, which were marked prior to incision with a skin marker. Under these circumstances, PFJ loads were measured. However, even small changes in arthrotomy closure positioning may have an effect on patella tracking which can differ from the loads measured during these intraoperative trials [
27]. While the time warp function was used to fit knee flexion angles to load measurements, future investigations and iterations of the device may include flexion angle measurements associated with PFJ loads. Patella resection adjustments were made based on evaluation of PFJ loading characteristics with different thickness shim and angles by the senior author.
In summary, the method detailed in our study for evaluation of PFJ loads presents a technique for improving management of patella resection and could be easily incorporated into the existing work flow of TKR. A planned work flow would involve first performing a patella resection and then obtaining native PFJ loads. Subsequently, evaluation of PFJ load after TKR was performed, as well as the effect of a potential secondary patella resection. A secondary patella resection might then be required to normalize loading of the PFJ. Based on the cadaveric experience, this might add 4–5 min to the procedure but does not require extra steps in the knee procedure and therefore will not materially add to the risk associated with the operation. Significant benefit in outcomes would accrue if PFJ loading forces can be normalized with this proposed method. Future studies will evaluate the use of pattern recognition algorithms to help surgeons identify PFJ loading patterns and to make choices on appropriate adjustment cuts intraoperatively. Furthermore, expanding to measure PFJ loads in a larger sample size, as well as in non-arthritic knees, will provide surgeons with a better representative understanding of what optimal PFJ load patterns should be achieved based on healthy native knees.