Novel Bathing Assist Device Decreases the Physical Burden on Caregivers and Difficulty of Bathing Activity in Care Recipients: A Pilot Study
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. BA Device
2.3. Experimental Paradigm
2.4. Data Recording and Analysis
3. Results
3.1. Change in Bathing Care with the Use of BA
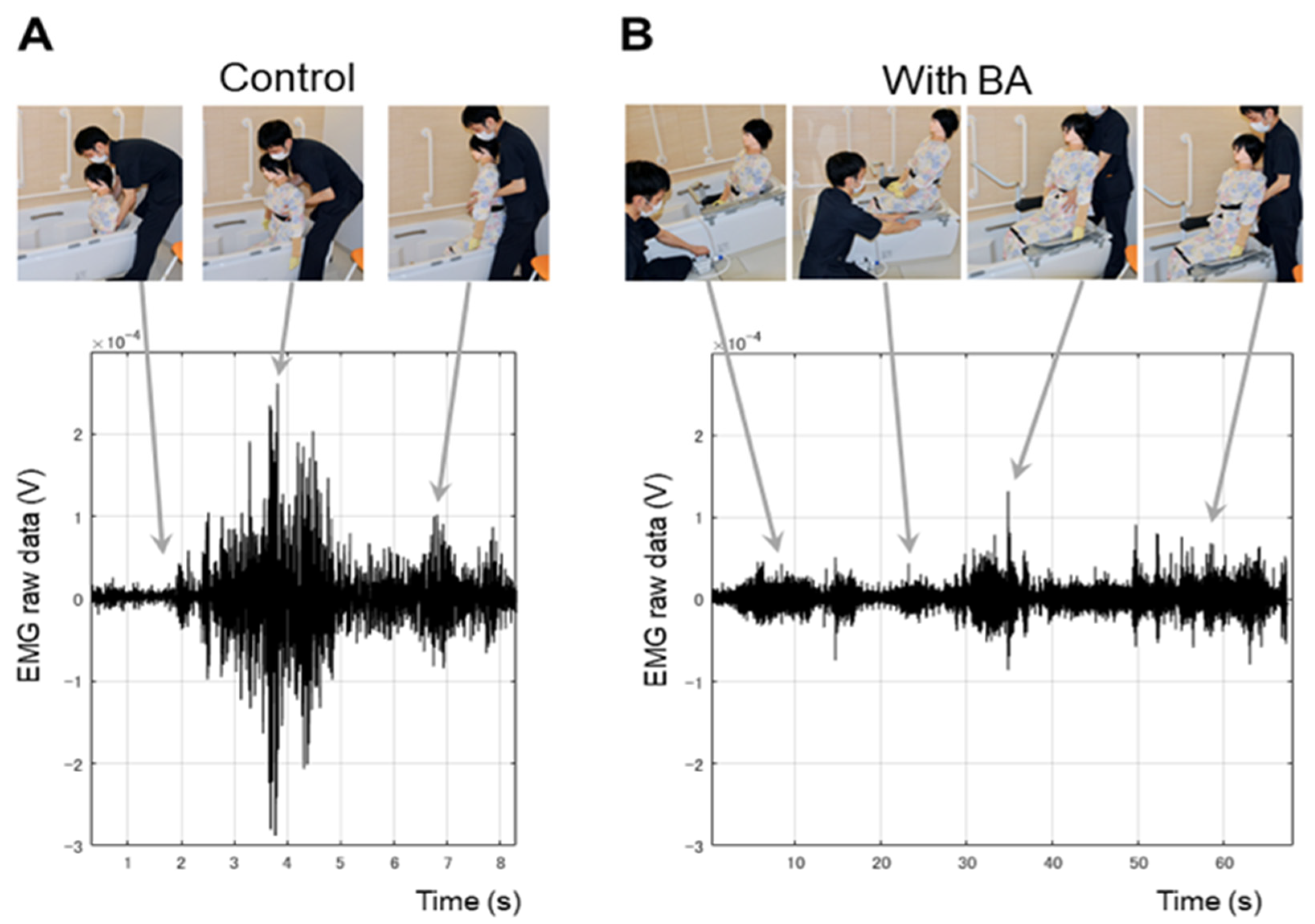
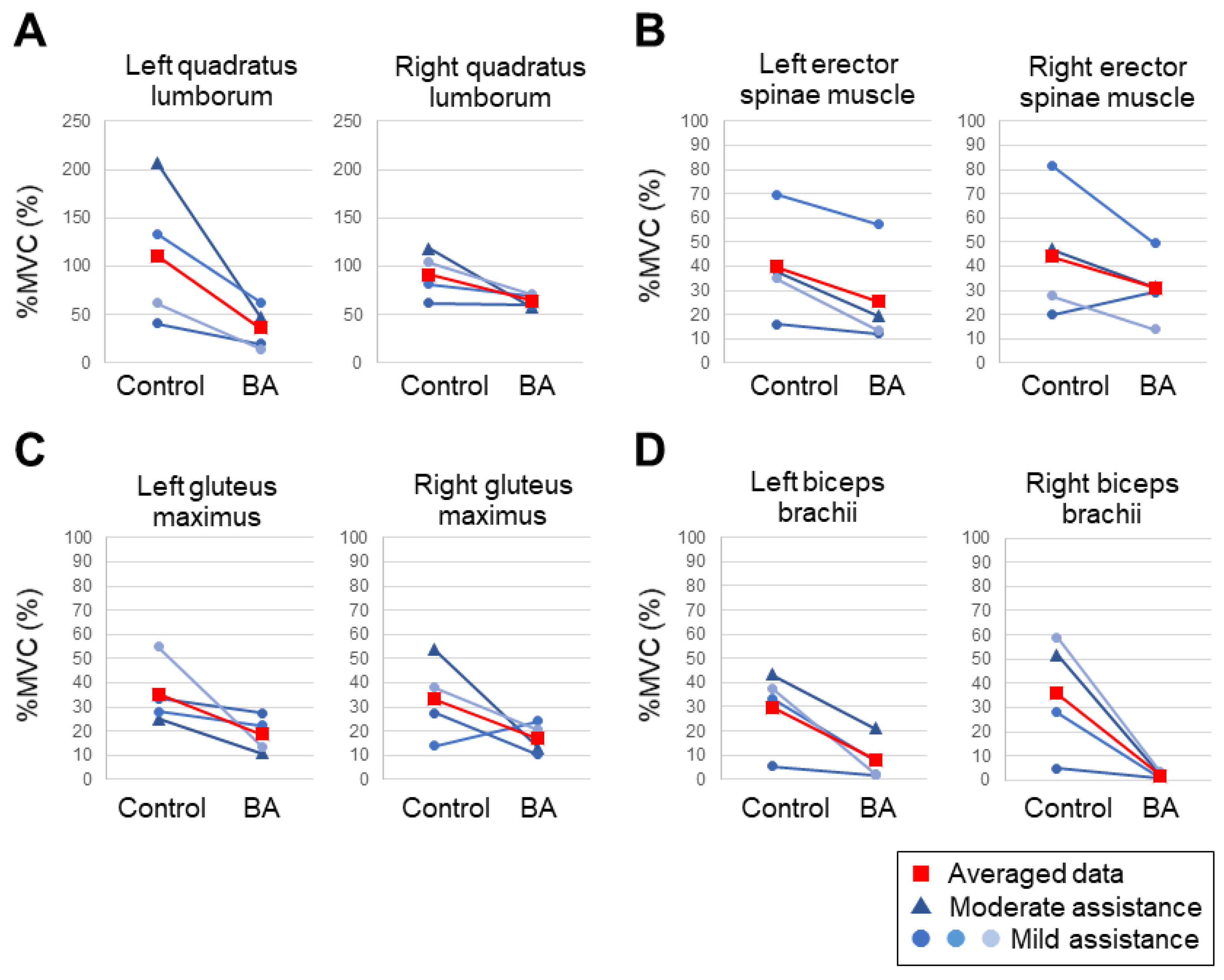
3.2. EMG when Assisting Patients out of the Bathub with and without the Use of BA
3.3. Assessment of Physical Burden with and without BA Using a Questionnaire
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nützi, M.; Koch, P.; Baur, H.; Elfering, A. Work–family conflict, task interruptions, and influence at work predict musculoskeletal pain in operating room nurses. Saf. Health Work 2015, 6, 329–337. [Google Scholar] [CrossRef]
- Sadeghian, F.; Coggon, D.; Ntani, G.; Hosseinzadeh, S. Predictors of low back pain in a longitudinal study of Iranian nurses and office workers. Work 2015, 51, 239–244. [Google Scholar] [CrossRef]
- Bejia, I.; Younes, M.; Jamila, H.B.; Khalfallah, T.; Salem, K.B.; Touzi, M.; Acrout, M.; Bergaoui, N. Prevalence and factors associated to low back pain among hospital staff. Jt. Bone Spine 2005, 72, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Bos, E.; Krol, B.; van der Star, L.; Groothoff, J. Risk factors and musculoskeletal complaints in non-specialized nurses, IC nurses, operation room nurses, and X-ray technologists. Int. Arch. Occup. Environ. Health 2007, 80, 198–206. [Google Scholar] [CrossRef]
- Dawson, A.P.; McLennan, S.N.; Schiller, S.D.; Jull, G.A.; Hodges, P.W.; Stewart, S. Interventions to prevent back pain and back injury in nurses: A systematic review. Occup. Environ. Med. 2007, 64, 642–650. [Google Scholar] [CrossRef]
- Iwakiri, K.; Takahashi, M.; Sotoyama, M.; Hirata, M.; Hisanaga, N. Usage Survey of Care Equipment in Care Service Facilities for the Elderly. Sangyo Eiseigaku Zasshi 2007, 49, 12–20. Available online: https://mol.medicalonline.jp/library/journal/download?GoodsID=cf8sangy/2007/004901/003&name=0012-0020j (accessed on 5 October 2022). [CrossRef]
- Mukai, M. Relations between nursing care workers’ lower back pain and their professional work and practices. Jpn. J. Gerontol. 2011, 33, 426–435. [Google Scholar] [CrossRef]
- Asakura, H.; Bishu, N.; Kanadani, C.; Yamada, T. Recognition of transfer tools by staff at care health centers for the elderly and its association with lumbago. Rigakuryoho Kagaku 2013, 28, 329–334. [Google Scholar] [CrossRef]
- Septarina, L.; Sumii, H.; Kunisada, M.; Matsumoto, Y. Comparative study of stress and burnout among nurses and caregivers during end-of-life care. Humanit. Sci. J. Fac. Health Welf. 2017, 17, 65–71. Available online: http://harp.lib.hiroshima-u.ac.jp/pu-hiroshima/metadata/12487 (accessed on 13 July 2022).
- Iwakiri, K.; Takahashi, M.; Sotoyama, M.; Liu, X.; Koda, S. Priority approaches of occupational safety and health activities for preventing low back pain among caregivers. J. Occup. Health 2019, 61, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Matsudaira, K.; Konishi, H.; Miyoshi, K.; Isomura, T.; Inuzuka, K. Potential risk factors of persistent low Back pain developing from mild low Back pain in urban Japanese workers. PLoS ONE 2014, 9, e93924. [Google Scholar] [CrossRef] [PubMed]
- Robotic Care Devices Portal. Available online: https://robotcare.jp/en/home/index (accessed on 13 July 2022).
- Yoshimi, T.; Kato, K.; Tsuchimoto, S.; Mizuguchi, N.; Kondo, I. Increase of verbal communication by long-term use of transfer-support robots in nursing facilities. Geriatr. Gerontol. Int. 2021, 21, 276–277. [Google Scholar] [CrossRef] [PubMed]
- Yoshimi, T.; Kato, K.; Tsuchimoto, S.; Mizuguchi, N.; Aimoto, K.; Itoh, N.; Kondo, I. Investigating proficiency using a lift-type transfer support device for effective care: Comparison of skilled and unskilled nursing homes. Disabil. Rehabil. Assist. Technol. 2022, 30, 1–10. [Google Scholar] [CrossRef]
- Yoshimi, T.; Kato, K.; Aimoto, K.; Sato, K.; Itoh, N.; Kondo, I. Utilization of transfer support equipment for meeting with family members in a nursing home during the COVID-19 pandemic: A case report. Geriatr. Gerontol. Int. 2021, 21, 741–742. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Yoshimi, T.; Aimoto, K.; Sato, K.; Itoh, N.; Kondo, I. Reduction of multiple-caregiver assistance through the long-term use of a transfer support robot in a nursing facility. Assist. Technol. 2022, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Yoshimi, T.; Tsuchimoto, S.; Mizuguchi, N.; Aimoto, K.; Itoh, N.; Kondo, I. Identification of care tasks for the use of wearable transfer support robots—An observational study at nursing facilities using robots on a daily basis. BMC Health Serv. Res. 2021, 21, 652. [Google Scholar] [CrossRef]
- Hignett, S.; Crumpton, E.; Ruszala, S.; Alexander, P.; Fray, M.; Fletcher, B. Evidence-based patient handling: Systematic review. Nurs. Stand. 2003, 17, 33–36. [Google Scholar] [CrossRef]
- Vieira, E.R.; Miller, L. Facing the challenge of patient transfers: Using ceiling lifts in healthcare facilities. HERD 2008, 2, 6–16. [Google Scholar] [CrossRef]
- Safe Lifting and Movement of Nursing Home Residents; NIOSH: Washington, DC, USA, 2006. Available online: https://www.cdc.gov/niosh/docs/2006-117/default.html (accessed on 13 July 2022).
- Ronald, L.A.; Yassi, A.; Spiegel, J.; Tate, R.B.; Tait, D.; Mozel, M.R. Effectiveness of installing overhead ceiling lifts. Reducing musculoskeletal injuries in an extended care hospital unit. AAOHN J. 2002, 50, 120–127. [Google Scholar] [CrossRef]
- Engst, C.; Chhokar, R.; Miller, A.; Tate, R.B.; Yassi, A. Effectiveness of overhead lifting devices in reducing the risk of injury to care staff in extended care facilities. Ergonomics 2005, 48, 187–199. [Google Scholar] [CrossRef]
- Fact-Finding Survey on Long-Term Care Works by Care Work Foundation. 2020. Available online: http://www.kaigo-center.or.jp/report/2021r01_chousa_01.html (accessed on 5 October 2022).
- Hayasaka, S.; Shibata, Y.; Goto, Y.; Noda, T.; Ojima, T. Bathing in a bathtub and health status: A cross-sectional study. Complement. Ther. Clin. Pract. 2010, 16, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Traphagan, J.W. Culture and long-term care: The bath as social service in Japan. Care Manag. J. 2004, 5, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Bathing Aid Device (Bath Assist), HI-LEX CORPORATION. Available online: http://www.hi-lex.co.jp/e/cable/house/house03.html (accessed on 13 July 2022).
- Hides, J.A.; Richardson, C.A.; Jull, G.A. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine 1996, 21, 2763–2769. [Google Scholar] [CrossRef] [PubMed]
- Sions, J.M.; Elliott, J.M.; Pohlig, R.T.; Hicks, G.E. Trunk muscle characteristics of the Multifidi, Erector Spinae, Psoas, and Quadratus Lumborum in older adults with and without chronic low back pain. J. Orthop. Sports Phys. Ther. 2017, 47, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Perotto, A.O.; Delagi, E.F.; Iazzetti, J.M.; Morrison, D. Anatomical Guide for the Electromyographer: The Limbs and Trunk, 4th ed.; Charles, C., Ed.; Thomas Publisher: Springfield, IL, USA, 2005. [Google Scholar]
- Avers, D.; Brown, M. Daniels and Worthingham’s Muscle Testing E-Book: Techniques of Manual Examination and Performance Testing, 10th ed.; Saunders; Elsevier Health Sciences: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Guidelines for Nursing Homes: Ergonomics for the Prevention of Musculoskeletal Disorders. Available online: https://www.osha.gov/ergonomics (accessed on 2 September 2022).
- Klein, B.; Schlömer, I. A robotic shower system: Acceptance and ethical issues. Z. Gerontol. Geriatr. 2018, 51, 25–31. [Google Scholar] [CrossRef]
- Satoh, H.; Kawabata, T.; Sankai, Y. Bathing care assistance with robot suit HAL. In Proceedings of the 2009 IEEE International Conference on Robotics and Biomimetics (ROBIO), Guilin, China, 19–23 December 2009; pp. 498–503. [Google Scholar] [CrossRef]
- Tan, C.K.; Kadone, H.; Miura, K.; Abe, T.; Koda, M.; Yamazaki, M.; Sankai, Y.; Suzuki, K. Muscle synergies during repetitive stoop lifting with a bioelectrically-controlled lumbar support exoskeleton. Front. Hum. Neurosci. 2019, 13, 142. [Google Scholar] [CrossRef]
- Burden, A. How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25 years of research. J. Electromyogr. Kinesiol. Review 2010, 20, 1023–1035. [Google Scholar] [CrossRef]
- Ekstrom, R.A.; Soderberg, G.L.; Donatelli, R.A. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J. Electromyogr. Kinesiol. 2005, 15, 418–428. [Google Scholar] [CrossRef]
- Hunter, A.M.; St Clair Gibson, A.; Lambert, M.; Noakes, T.D. Electromyographic (EMG) Normalization Method for Cycle Fatigue Protocols. Med. Sci. Sports Exerc. 2002, 34, 857–861. [Google Scholar] [CrossRef]

| ID1 | ID2 | ID3 | ID4 | ||
|---|---|---|---|---|---|
| Diagnosis | Right Middle Cerebral Artery Infarction | Femoral Neck Fracture (Right Artificial Head Replacement) | Right Femoral Supraclavicular Fracture (Plate Fixation) | Right Parietal Lobe Infarction | |
| Height (cm) | 172.8 | 166.1 | 146.1 | 152.0 | |
| Weight (kg) | 70.5 | 53.5 | 56.6 | 44.2 | |
| FIMTM | Motor subscale | 60 | 78 | 70 | 76 |
| Cognitive subscale | 29 | 31 | 32 | 33 | |
| Welfare equipment used for transportation in hospital wards | Wheelchair | Walkers | Wheelchair (For weight exemption) | Walkers | |
| ID 1 | ID 2 | ID 3 | ID 4 | |
|---|---|---|---|---|
| Transfer to shower seat | Moderate Assistance | Monitoring | Monitoring | Monitoring |
| Transfer from the shower chair to the bathtub | Moderate Assistance | Monitoring | Monitoring | Mild Assistance |
| Getting into the bathtub | Moderate Assistance | Monitoring | Monitoring | Mild Assistance |
| Getting out the bathtub | Moderate Assistance | Mild Assistance | Mild Assistance | Mild Assistance |
| ID 1 | ID 2 | ID 3 | ID 4 | |
|---|---|---|---|---|
| Transfer to shower seat | Moderate Assistance | Monitoring | Monitoring | Monitoring |
| Transfer from the shower chair to the bathtub | Moderate Assistance | Monitoring | Monitoring | Monitoring |
| Getting into the bathtub | Monitoring | Monitoring | Monitoring | Monitoring |
| Getting out the bathtub | Monitoring | Monitoring | Monitoring | Monitoring |
| Caregiver ID | 1 | 2 | 3 | 4 | Median | |
|---|---|---|---|---|---|---|
| Physical burden (min: 1, max: 7) | Control | 5 | 5 | 4 | 3 | 4.5 |
| BA | 2 | 1 | 1 | 1 | 1 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kato, K.; Aimoto, K.; Kawamura, K.; Yoshimi, T.; Itoh, N.; Kondo, I. Novel Bathing Assist Device Decreases the Physical Burden on Caregivers and Difficulty of Bathing Activity in Care Recipients: A Pilot Study. Appl. Sci. 2022, 12, 10131. https://doi.org/10.3390/app121910131
Kato K, Aimoto K, Kawamura K, Yoshimi T, Itoh N, Kondo I. Novel Bathing Assist Device Decreases the Physical Burden on Caregivers and Difficulty of Bathing Activity in Care Recipients: A Pilot Study. Applied Sciences. 2022; 12(19):10131. https://doi.org/10.3390/app121910131
Chicago/Turabian StyleKato, Kenji, Keita Aimoto, Koki Kawamura, Tatsuya Yoshimi, Naoki Itoh, and Izumi Kondo. 2022. "Novel Bathing Assist Device Decreases the Physical Burden on Caregivers and Difficulty of Bathing Activity in Care Recipients: A Pilot Study" Applied Sciences 12, no. 19: 10131. https://doi.org/10.3390/app121910131
APA StyleKato, K., Aimoto, K., Kawamura, K., Yoshimi, T., Itoh, N., & Kondo, I. (2022). Novel Bathing Assist Device Decreases the Physical Burden on Caregivers and Difficulty of Bathing Activity in Care Recipients: A Pilot Study. Applied Sciences, 12(19), 10131. https://doi.org/10.3390/app121910131







