Abdominal Adiposity Increases Lordosis and Doubles the Risk of Low Back Pain
Abstract
:1. Introduction
2. Subjects and Methods
2.1. Study Design and Sample Size
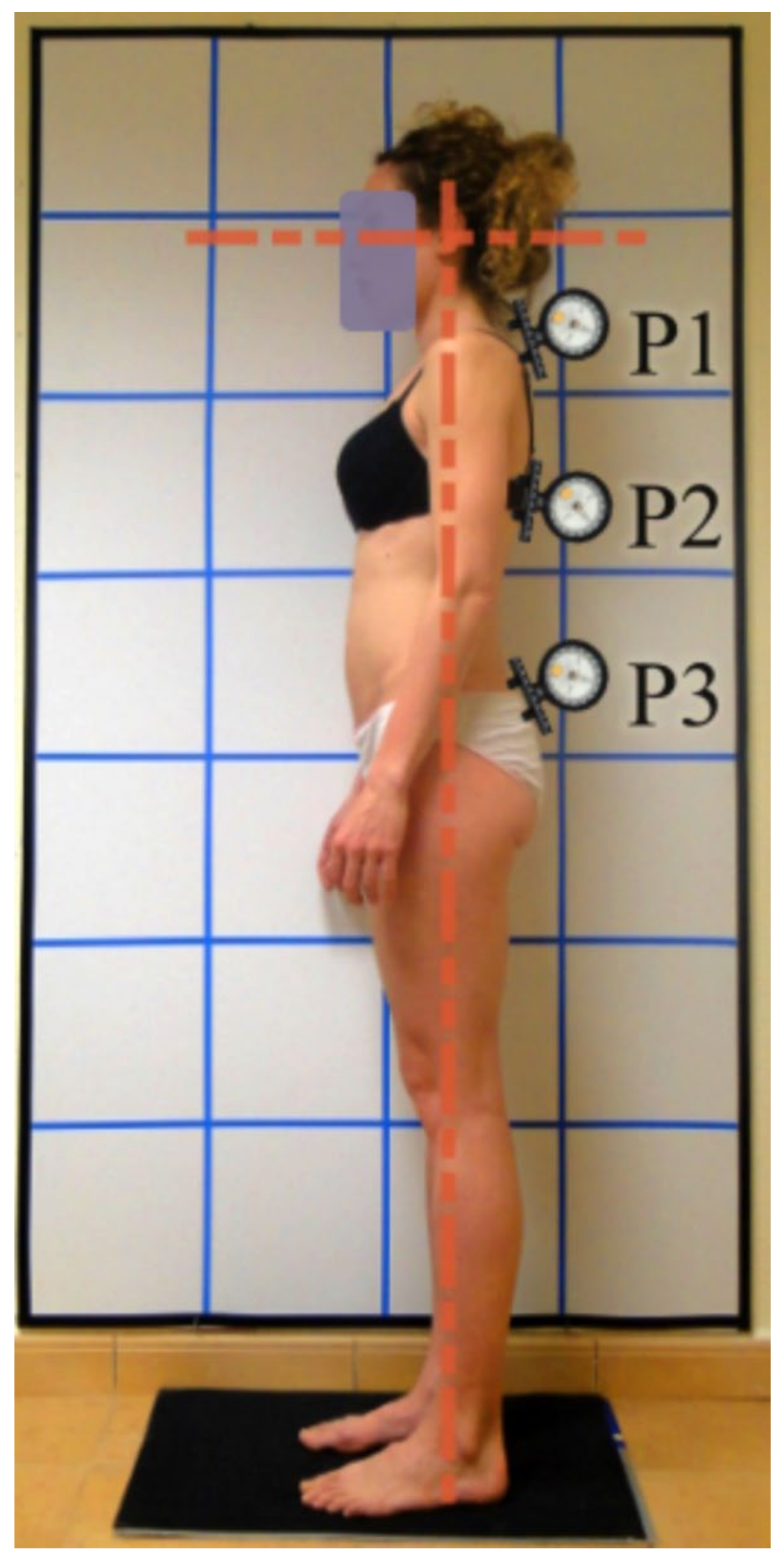
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Association between Obesity and Abdominal Obesity with Vertebral Curvatures
3.3. Association between Adiposity and Vertebral Curvatures with Vertebral Pain
4. Discussion
4.1. Sagittal Spinal Posture
4.2. Back Pain
5. Conclusions
Future Lines of Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Safiri, S.; Kolahi, A.A.; Smith, E.; Hill, C.; Bettampadi, D.; Mansournia, M.A.; Collins, G. Global, regional and national burden of osteoarthritis 1990–2017: A systematic analysis of the Global Burden of Disease Study 2017. Ann. Rheum. Dis. 2020, 79, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Hoy, D.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Bain, C.; Buchbinder, R. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Woolf, A. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [Green Version]
- Nestares, T.; Salinas, M.; de Teresa, C.; Díaz-Castro, J.; Moreno-Fernández, J.; López-Frías, M. Factores de riesgo relacionados con los hábitos de vida en pacientes con patología osteomuscular. Nutr. Hosp. 2017, 34, 444–453. [Google Scholar] [CrossRef]
- Blyth, F.M.; Briggs, A.M.; Schneider, C.H.; Hoy, D.G.; March, L.M. The global burden of musculoskeletal pain—Where to from here? Am. J. Public Health 2019, 109, 35–40. [Google Scholar] [CrossRef]
- Norberg, M.; Norberg, M.A. Lumbalgias comunes: Discapacidad y técnicas de evaluación, incidencias socioeconómicas. EMC Apar. Locomot. 2016, 49, 1–7. [Google Scholar] [CrossRef]
- Onyemaechi, N.O.; Anyanwu, G.E.; Obikili, E.N.; Onwuasoigwe, O.; Nwankwo, O.E. Impact of overweight and obesity on the musculoskeletal system using lumbosacral angles. Patient Prefer. Adherence 2016, 10, 291. [Google Scholar] [CrossRef] [Green Version]
- Raza, A.; Jamshaid, M.; Riaz, T.; Bashir, I.; Majeed, I.; Akram, W. Correlation of back pain with obesity and posture among teenagers. Anaesth. Pain Intensive Care 2019, 2019, 112–116. [Google Scholar]
- Pagnotti, G.M.; Haider, A.; Yang, A.; Cottell, K.E.; Tuppo, C.M.; Tong, K.Y.; Chan, M.E. Postural Stability in Obese Preoperative Bariatric Patients Using Static and Dynamic Evaluation. Obes. Facts 2020, 13, 499–513. [Google Scholar] [CrossRef]
- Yelmaiza, M.; Susanti, R.; Indra, S. The Risk Factors Affecting Disability Level of Lumbar Disc Herniation. Biosci. Med. J. Biomed. Transl. Res. 2022, 6, 1275–1280. [Google Scholar] [CrossRef]
- Brito-Hernández, L.; Espinoza-Navarro, O.; Díaz-Gamboa, J.; Lizana, P.A. Evaluación postural y prevalencia de hipercifosis e hiperlordosis en estudiantes de enseñanza básica. Int. J. Morphol. 2018, 36, 290–296. [Google Scholar] [CrossRef] [Green Version]
- Tatsumi, M.; Mkoba, E.M.; Suzuki, Y.; Kajiwara, Y.; Zeidan, H.; Harada, K.; Aoyama, T. Risk factors of low back pain and the relationship with sagittal vertebral alignment in Tanzania. BMC Musculoskelet. Disord. 2019, 20, 1–5. [Google Scholar] [CrossRef] [Green Version]
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull. World Health Organ. 2001, 79, 373. [Google Scholar]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Lohman, T.G.; Roche, A.F.; Martorell, R. (Eds.) Anthropometric standardization reference manual. In Human Kinetics Books; Agris: Rome, Italy, 1991; Available online: https://agris.fao.org/agris-search/search.do?recordID=US201300683431 (accessed on 2 July 2022).
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; Technical Report Series 894; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Durnin, J.V.; Womersley, J.V.G.A. Body fat assessed from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 years. Br. J. Nutr. 1974, 32, 77–97. [Google Scholar] [CrossRef] [Green Version]
- Siri, W.E. Body composition from fluid spaces and density: Analysis of methods. Tech. Meas. Body Compos. 1961, 61, 223–244. [Google Scholar]
- Aranceta, J.; Foz, M.; Moreno, B.; Gil, B.; Jover, E.; Millán, J.; Monereo, S. Documento de consenso: Obesidad y riesgo cardiovascular. Clín. Investig. Arterioscler. 2003, 15, 196–232. [Google Scholar] [CrossRef]
- Han, T.S.; Seidell, J.C.; Currall, J.E.P.; Morrison, C.E.; Deurenberg, P.; Lean, M.E.J. The influences of height and age on waist circumference as an index of adiposity in adults. Int. J. Obes. 1997, 21, 83–90. [Google Scholar] [CrossRef] [Green Version]
- Hsieh, S.D.; Yoshinaga, H.; Muto, T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int. J. Obes. 2003, 27, 610–616. [Google Scholar] [CrossRef] [Green Version]
- Bullock-Saxton, J. Postural alignment in standing: A repeatability study. Aust. J. Physiother. 1993, 39, 25–29. [Google Scholar] [CrossRef] [Green Version]
- Saur, P.M.; Ensink, F.B.M.; Frese, K.; Seeger, D.; Hildebrandt, J. Lumbar range of motion: Reliability and validity of the inclinometer technique in the clinical measurement of trunk flexibility. Spine 1996, 21, 1332–1338. [Google Scholar] [CrossRef]
- Santonja, F.; Pastor, A.; Andújar, P. Cifosis y lordosis. Cirugía Menor Proced. Med. Fam. 2000, 1, 783–792. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Oja, P. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orozco, C.A.T.; Sánchez, J.R.B. Influencia de la asimetría en el tamaño de la muestra para el cumplimiento del teorema central del límite en distribuciones continúas. Sci. Tech. 2017, 22, 398–402. [Google Scholar]
- Damasceno, L.H.F.; Catarin, S.R.G.; Campos, A.D.; Defino, H.L.A. Lumbar lordosis: A study of angle values and of vertebral bodies and intervertebral discs role. Acta Ortop. Bras. 2006, 14, 193–198. [Google Scholar] [CrossRef]
- Takeda, N.; Kobayashi, T.; Atsuta, Y.; Matsuno, T.; Shirado, O.; Minami, A. Changes in the sagittal spinal alignment of the elderly without vertebral fractures: A minimum 10-year longitudinal study. J. Orthop. Sci. 2009, 14, 748–753. [Google Scholar] [CrossRef]
- Araújo, F.A.; Simões, D.; Silva, P.; Alegrete, N.; Lucas, R. Sagittal standing posture and relationships with anthropometrics and body composition during childhood. Gait Posture 2019, 73, 45–51. [Google Scholar] [CrossRef]
- Tatsumi, Y.; Watanabe, M.; Kokubo, Y.; Nishimura, K.; Higashiyama, A.; Okamura, T.; Miyamoto, Y. Effect of age on the association between waist-to-height ratio and incidence of cardiovascular disease: The Suita study. J. Epidemiol. 2013, 23, 351–359. [Google Scholar] [CrossRef] [Green Version]
- Jankowicz-Szymańska, A.; Bibro, M.; Wodka, K.; Smola, E. Does excessive body weight change the shape of the spine in children? Child. Obes. 2019, 15, 346–352. [Google Scholar] [CrossRef]
- Stagnara, P.; De Mauroy, J.C.; Dran, G.; Gonon, G.P.; Costanzo, G.; Dimnet, J.; Pasquet, A. Reciprocal angulation of vertebral bodies in a sagittal plane: Approach to references for the evaluation of kyphosis and lordosis. Spine 1982, 7, 335–342. [Google Scholar] [CrossRef] [Green Version]
- Zaina, F.; Atanasio, S.; Ferraro, C.; Fusco, C.; Negrini, A.; Romano, M.; Negrini, S. Review of rehabilitation and orthopedic conservative approach to sagittal plane diseases during growth: Hyperkyphosis, junctional kyphosis, and Scheuermann disease. Eur. J. Phys. Rehabil. Med. 2009, 45, 595–603. [Google Scholar]
- Chun, S.W.; Lim, C.Y.; Kim, K.; Hwang, J.; Chung, S.G. The relationships between low back pain and lumbar lordosis: A systematic review and meta-analysis. Spine J. 2017, 17, 1180–1191. [Google Scholar] [CrossRef]
- Segarra, V.; Heredia, J.R.; Peña, G.; Sampietro, M.; Moyano, M.; Mata, F.; Silva-Grigoletto, M.E.D. Core y sistema de control neuro-motor: Mecanismos básicos para la estabilidad del raquis lumbar. Rev. Bras. Educ. Fís. Esporte 2014, 28, 521–529. [Google Scholar] [CrossRef] [Green Version]
- Perera, R.S.; Chen, L.; Hart, D.J.; Spector, T.D.; Arden, N.K.; Ferreira, M.L.; Radojčić, M.R. Effects of body weight and fat mass on back pain–direct mechanical or indirect through inflammatory and metabolic parameters? In Seminars in Arthritis and Rheumatism; WB Saunders: Amsterdam, The Netherlands, 2022; Volume 52, p. 151935. [Google Scholar]
- Ávila-Ramírez, J.; Reyes-Rodríguez, V.A. La obesidad y el sobrepeso, su efecto sobre la columna lumbar. Rev. Mex. Neurocienc. 2009, 10, 220–223. [Google Scholar]
| Total Population (n = 301) | Men (n = 122) | Women (n = 179) | p Value | |
|---|---|---|---|---|
| Age m(sd) | 47.0 (20.5) | 41.9 (20.7) | 50.5 (19.7) | <0.001 |
| Studies level m (%) | 0.063 | |||
| Low | 105 (34.9) | 35 (28.7) | 70 (39.1) | |
| High | 196 (65.1) | 87 (71.3) | 109 (60.9) | |
| METs m (sd) | 2647.7 (2402.1) | 3449.2 (3073.7) | 2101.5 (1600.6) | <0.001 |
| BMI (kg/m2) m (sd) | 25.6 (4.2) | 25.6 (3.7) | 25.6 (4.5) | 0.986 |
| n (%)Normal | 148 (49.2) | 56 (45.9) | 90 (50.3) | 0.586 |
| Overweight | 106 (35.2) | 47 (39.3) | 60 (33.5) | |
| Obesity | 47 (15.6) | 18 (14.8) | 29 (16.2) | |
| BF% m (sd) | 30.4 (9.2) | 22.9 (7.5) | 35.6 (6.4) | <0.001 |
| n (%)Normal | 93 (30.9) | 49 (40.2) | 44 (24.6) | <0.001 |
| Limit | 38 (12.6) | 22 (18.0) | 16 (8.9) | |
| Obesity | 170 (56.5) | 51 (41.8) | 119 (66.5) | |
| WC (cm) m (sd) | 84.4 (12.3) | 88.7 (11.9) | 81.4 (11.8) | <0.001 |
| n (%)Normal | 231 (76.7) | 102 (83.6) | 129 (72.1) | 0.020 |
| Abdominal obesity | 70 (23.3) | 20 (16.4) | 50 (27.9) | |
| WHR (cm) m (sd) | 0.86 (0.10) | 0.92 (0.09) | 0.82 (0.09) | <0.001 |
| n (%)Normal | 204 (67.8) | 96 (78.7) | 108 (60.3) | 0.001 |
| Risk value | 97 (32.2) | 26 (21.3) | 71 (39.7) | |
| W/HT (cm) m (sd) | 0.51 (0.08) | 0.51 (0.07) | 0.51 (0.08) | 0.995 |
| n (%)Normal | 144 (47.8) | 60 (49.2) | 84 (46.9) | 0.701 |
| Risk value | 157 (52.2) | 62 (50.8) | 95 (53.1) | |
| Cervical curvature (rad) m (sd) | 37.2 (8.9) | 37.1 (9.0) | 37,2 (8.9) | 0.964 |
| Dorsal curvature (rad) m (sd) | 51.9 (11.4) | 50.5 (11.2) | 53.0 (11.6) | 0.066 |
| Lumbar curvature (rad) m (sd) | 36.4 (11.9) | 33.3 (12.0) | 38.5 (11.5) | <0.001 |
| Neck pain n (%) | ||||
| No | 129 (42.9) | 68 (55.7) | 61 (34.1) | <0.001 |
| Yes | 172 (57.1) | 54 (44.3) | 118 (65.9) | |
| Dorsal pain n (%) | ||||
| No | 200 (66.4) | 89 (73.0) | 111 (62.0) | 0.048 |
| Yes | 101 (33.6) | 33 (27.0) | 68 (38.0) | |
| Low back pain n (%) | ||||
| No | 102 (33.9) | 50 (41.0) | 52 (29.1) | 0.032 |
| Yes | 199 (66.1) | 72 (59.0) | 128 (70.9) |
| Cervical Curvature β (95% CI) | Dorsal Curvature β (95% CI) | Lumbar Curvature β (95% CI) | |
|---|---|---|---|
| BMI (kg/m2) | 0.376 (0.136–0.617) ** | 0.599 (0.274–0.924) *** | 0.336 (0.003–0.670) * |
| BF% | 0.260 (0.072–0.448) ** | 0.459 (0.206–0.712) *** | 0.175 (−0.086–0.435) |
| WC (cm) | 0.187 (0.100–0.274) *** | 0.264 (0.146–0.382) *** | 0.143 (0.021–0.265) * |
| WHR | 17.192 (6.058–28.325) ** | 21.525 (6.354–36.697) ** | 3.324 (−12.228–18.877) |
| W/HT | 0.298 (0.151–0.446) *** | 0.447 (0.247–0.646) *** | 0.215 (0.008–0.422) * |
| Neck Pain OR (95% CI) | Dorsal Pain OR (95% CI) | Low Back Pain OR (95% CI) | |
|---|---|---|---|
| BMI (kg/m2) (ref: normal) | |||
| overweight | 0.659 (0.376–1.157) | 0.855 (0.4817–1.520) | 0.864 (0.483–1.546) |
| obesity | 0.544 (0.262–1.132) | 1.466 (0.710–3.026) | 1.507 (0.662–3.428) |
| BF% (ref: normal) | |||
| limit | 1.319 (0.552–3.150) | 1.434 (0.596–3.451) | 1.646 (0.683–3.966) |
| obesity | 0.889 (0.425–1.860) | 1.433 (0.675–3.042) | 1.761 (0.826–3.757) |
| WC (cm) (ref: normal) | |||
| abdominal obesity | 0.595 (0.326–1.085) | 1.139 (0.621–2.088) | 2.172 (1.067–4.419) * |
| WHR (ref: normal) | |||
| Risk | 0.932 (0.532–1.616) | 0.840 (0.481–1.467) | 0.995 (0.554–1.787) |
| W/HT (ref: normal) | |||
| Risk | 0.552 (0.307–0.993) * | 1.082 (0.670–1.747) | 0.923 (0.505–1.687) |
| Cervical curvature (rad) | 0.998 (0.968–1.028) | 1.004 (0.974–1.035) | 1.002 (0.971–1.034) |
| Dorsal curvature (rad) | 0.990 (0.969–1.012) | 1.009 (0.987–1.032) | 1.004 (0.981–1.028) |
| Lumbar curvature (rad) | 1.006 (0.985–1.028) | 0.997 (0.975–1.019) | 1.031 (1.007–1.055) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saludes, R.; Acevedo, P.; García, I.Z.; Gómez Carrión, Á.; Martínez Sebastián, C.; Núñez Fernández, A.; Seco-Armell, I.; Sánchez-Gómez, R. Abdominal Adiposity Increases Lordosis and Doubles the Risk of Low Back Pain. Appl. Sci. 2022, 12, 7616. https://doi.org/10.3390/app12157616
Saludes R, Acevedo P, García IZ, Gómez Carrión Á, Martínez Sebastián C, Núñez Fernández A, Seco-Armell I, Sánchez-Gómez R. Abdominal Adiposity Increases Lordosis and Doubles the Risk of Low Back Pain. Applied Sciences. 2022; 12(15):7616. https://doi.org/10.3390/app12157616
Chicago/Turabian StyleSaludes, Rebeca, Paula Acevedo, Ignacio Zaragoza García, Álvaro Gómez Carrión, Carlos Martínez Sebastián, Almudena Núñez Fernández, Isabel Seco-Armell, and Rubén Sánchez-Gómez. 2022. "Abdominal Adiposity Increases Lordosis and Doubles the Risk of Low Back Pain" Applied Sciences 12, no. 15: 7616. https://doi.org/10.3390/app12157616
APA StyleSaludes, R., Acevedo, P., García, I. Z., Gómez Carrión, Á., Martínez Sebastián, C., Núñez Fernández, A., Seco-Armell, I., & Sánchez-Gómez, R. (2022). Abdominal Adiposity Increases Lordosis and Doubles the Risk of Low Back Pain. Applied Sciences, 12(15), 7616. https://doi.org/10.3390/app12157616







