Evaluation of General Health Status of Persons Living in Socio-Economically Disadvantaged Neighborhoods in a Large European Metropolitan City
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic Characteristics
3.2. Country of Origin
3.3. Social Integration and Housing Conditions
3.4. Smoking and Drinking Habits
3.5. COVID-19
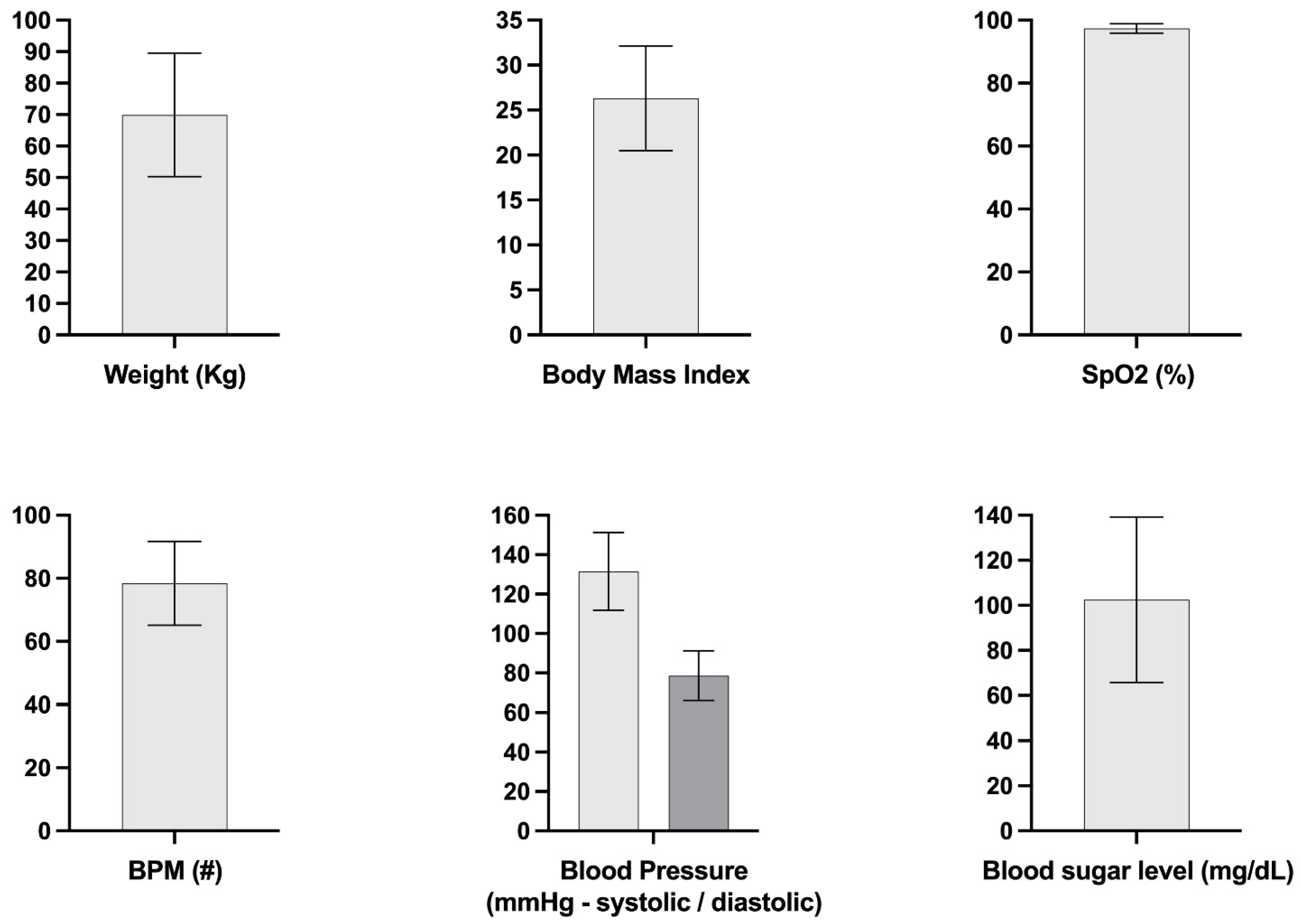
3.6. Health Assessment
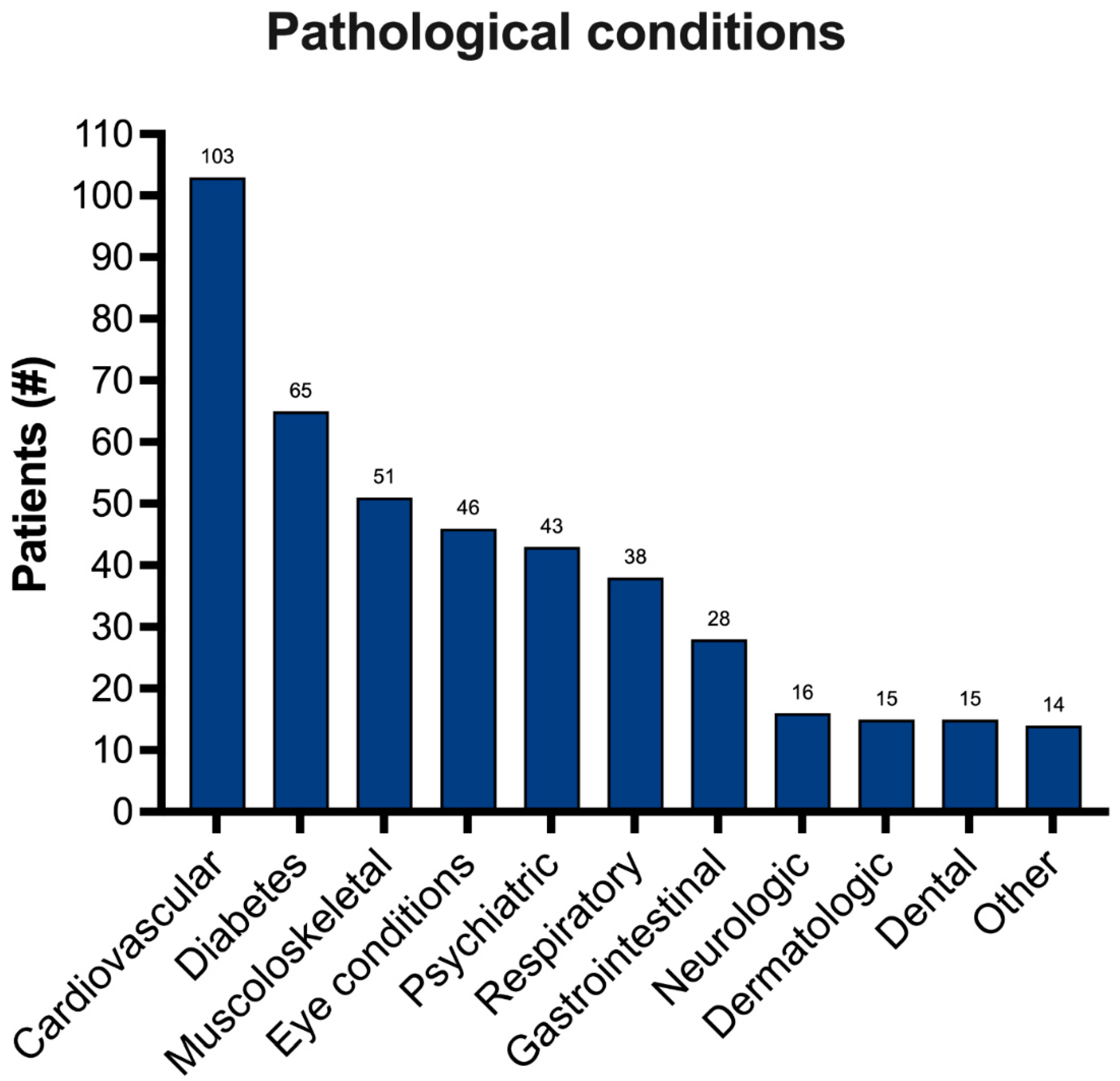
3.7. Specific Pathological Conditions
4. Discussion
Limits of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yerramilli, P.; Fernandez, O.; Thomson, S. Financial protection in Europe: A systematic review of the literature and mapping of data availability. Health Policy 2018, 122, 493–508. [Google Scholar] [CrossRef] [PubMed]
- Del Pozo-Rubio, R.; Minguez-Salido, R.; Pardo-Garcia, I.; Escribano-Sotos, F. Catastrophic long-term care expenditure: Associated socio-demographic and economic factors. Eur. J. Health Econ 2019, 20, 691–701. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Johnson, S.B.; Newman, S.; Riley, A.W. Residential mobility and long-term exposure to neighborhood poverty among children born in poor families: A U.S. longitudinal cohort study. Soc. Sci. Med. 2019, 226, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, A.M.; Aitken, Z.; Emerson, E.; Sahabandu, S.; Milner, A.; Bentley, R.; LaMontagne, A.D.; Pirkis, J.; Studdert, D. Inequalities in socio-economic characteristics and health and wellbeing of men with and without disabilities: A cross-sectional analysis of the baseline wave of the Australian Longitudinal Study on Male Health. BMC Public Health 2016, 16, 1042. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, D.; Jay, S.; McNamara, N.; Stevenson, C.; Muldoon, O.T. Perceived discrimination amongst young people in socio-economically disadvantaged communities: Parental support and community identity buffer (some) negative impacts of stigma. Br. J. Dev. Psychol. 2016, 34, 153–168. [Google Scholar] [CrossRef]
- Consolazio, D.; Murtas, R.; Tunesi, S.; Gervasi, F.; Benassi, D.; Russo, A.G. Assessing the Impact of Individual Characteristics and Neighborhood Socioeconomic Status During the COVID-19 Pandemic in the Provinces of Milan and Lodi. Int. J. Health Serv. 2021, 51, 311–324. [Google Scholar] [CrossRef]
- Gelormino, E.; Melis, G.; Marietta, C.; Costa, G. From built environment to health inequalities: An explanatory framework based on evidence. Prev. Med. Rep. 2015, 2, 737–745. [Google Scholar] [CrossRef]
- Simonelli, N.; Gorini, A.; Giroli, M.; Amato, M.; Vigo, L.; Tremoli, E.; Werba, J.P. Barriers and facilitators for physical activity in sedentary people residing in a disadvantaged Italian neighbourhood. Epidemiol. Prev. 2018, 42, 226–234. [Google Scholar]
- Marinacci, C.; Demaria, M.; Melis, G.; Borrell, C.; Corman, D.; Dell’Olmo, M.M.; Rodriguez, M.; Costa, G. The Role of Contextual Socioeconomic Circumstances and Neighborhood Poverty Segregation on Mortality in 4 European Cities. Int. J. Health Serv. 2017, 47, 636–654. [Google Scholar] [CrossRef]
- Materia, E.; Spadea, T.; Rossi, L.; Cesaroni, G.; Area, M.; Perucci, C.A. Health care inequalities: Hospitalization and socioeconomic position in Rome. Epidemiol. Prev. 1999, 23, 197–206. [Google Scholar]
- van Vuuren, C.L.; Reijneveld, S.A.; van der Wal, M.F.; Verhoeff, A.P. Neighborhood socioeconomic deprivation characteristics in child (0–18 years) health studies: A review. Health Place 2014, 29, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Tanggaard Andersen, P.; Holst Algren, M.; Fromsejer Heiberg, R.; Joshi, R.; Kronborg Bak, C. Social network resources and self-rated health in a deprived Danish neighborhood. Health Promot. Int. 2018, 33, 999–1009. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Cedola, C.; Russo, L.; Urbano, S.; Cimino, M.; Fonte, E.; Morrone, A.; Arcangeli, A.; Ercoli, L. Health and social conditions of children living in disadvantaged neighborhoods in the city of Rome, Italy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 12350–12357. [Google Scholar] [PubMed]
- Ralli, M.; Urbano, S.; Gobbi, E.; Shkodina, N.; Mariani, S.; Morrone, A.; Arcangeli, A.; Ercoli, L. Health and Social Inequalities in Women Living in Disadvantaged Conditions: A Focus on Gynecologic and Obstetric Health and Intimate Partner Violence. Health Equity 2021, 5, 408–413. [Google Scholar] [CrossRef]
- Timberlake, J.M. Effects of household and neighborhood characteristics on children’s exposure to neighborhood poverty and affluence. Soc. Sci. Res. 2009, 38, 458–476. [Google Scholar] [CrossRef]
- Nau, C.; Schwartz, B.S.; Bandeen-Roche, K.; Liu, A.; Pollak, J.; Hirsch, A.; Bailey-Davis, L.; Glass, T.A. Community socioeconomic deprivation and obesity trajectories in children using electronic health records. Obesity 2015, 23, 207–212. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129 (Suppl. S2), 19–31. [Google Scholar] [CrossRef]
- Cockerham, W.C.; Hamby, B.W.; Oates, G.R. The Social Determinants of Chronic Disease. Am. J. Prev. Med. 2017, 52, S5–S12. [Google Scholar] [CrossRef]
- Ribeiro, A.I.; Fraga, S.; Severo, M.; Kelly-Irving, M.; Delpierre, C.; Stringhini, S.; Kivimaki, M.; Joost, S.; Guessous, I.; Severi, G.; et al. Association of neighbourhood disadvantage and individual socioeconomic position with all-cause mortality: A longitudinal multicohort analysis. Lancet Public Health 2022, 7, e447–e457. [Google Scholar] [CrossRef]
- Alagna, E.; Santangelo, O.E.; Raia, D.D.; Gianfredi, V.; Provenzano, S.; Firenze, A. Health status, diseases and vaccinations of the homeless in the city of Palermo, Italy. Ann. Ig. 2019, 31, 21–34. [Google Scholar]
- Llerena, K.; Gabrielian, S.; Green, M.F. Clinical and cognitive correlates of unsheltered status in homeless persons with psychotic disorders. Schizophr. Res. 2018, 197, 421–427. [Google Scholar] [CrossRef]
- Paiva, I.K.; Lira, C.D.; Justino, J.M.; Miranda, M.G.; Saraiva, A.K. Homeless people’s right to health: Reflections on the problems and components. Cien. Saude. Colet. 2016, 21, 2595–2606. [Google Scholar] [CrossRef] [PubMed]
- Neisler, J.; Reitzel, L.R.; Garey, L.; Kenzdor, D.E.; Hebert, E.T.; Vijayaraghavan, M.; Businelle, M.S. Concurrent nicotine and tobacco product use among homeless smokers and associations with cigarette dependence and other factors related to quitting. Drug Alcohol Depend. 2018, 185, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Arcangeli, A.; Ercoli, L. Homelessness and COVID-19: Leaving No-One Behind. Ann. Glob. Health 2021. [CrossRef] [PubMed]
- Ralli, M.; Cedola, C.; Urbano, S.; Morrone, A.; Ercoli, L. Homeless persons and migrants in precarious housing conditions and COVID-19 pandemic: Peculiarities and prevention strategies. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9765–9767. [Google Scholar]
- Ralli, M.; Cedola, C.; Urbano, S.; Latini, O.; Shkodina, N.; Morrone, A.; Arcangeli, A.; Ercoli, L. Assessment of SARS-CoV-2 infection through rapid serology testing in the homeless population in the City of Rome, Italy. Preliminary results. J. Public Health Res. 2020, 9, 1986. [Google Scholar] [CrossRef]
- van Laere, I.R.; de Wit, M.A.; Klazinga, N.S. Pathways into homelessness: Recently homeless adults problems and service use before and after becoming homeless in Amsterdam. BMC Public Health 2009, 9, 3. [Google Scholar] [CrossRef]
- Romaszko, J.; Kuchta, R.; Opalach, C.; Bertrand-Bucinska, A.; Romaszko, A.M.; Giergielewicz-Januszko, B.; Bucinski, A. Socioeconomic Characteristics, Health Risk Factors and Alcohol Consumption among the Homeless in North-Eastern Part of Poland. Cent. Eur. J. Public Health 2017, 25, 29–34. [Google Scholar] [CrossRef][Green Version]
- Smith, O.M.; Chant, C.; Burns, K.E.A.; Kaur, M.; Ashraf, S.; DosSantos, C.C.; Hwang, S.W.; Friedrich, J.O. Characteristics, clinical course, and outcomes of homeless and non-homeless patients admitted to ICU: A retrospective cohort study. PLoS ONE 2017, 12, e0179207. [Google Scholar] [CrossRef]
- Matteoli, M.; Scaringi, C.; Carella, P.; Fruttaldo, L.; Angeloni, U.; Laurenza, M. A Mobile Health Service to Manage Diabetic Foot in Homeless Patients. J. Am. Podiatr. Med. Assoc. 2015, 105, 424–428. [Google Scholar] [CrossRef]
- Pacelli, B.; Zengarini, N.; Broccoli, S.; Caranci, N.; Spadea, T.; Di Girolamo, C.; Cacciani, L.; Petrelli, A.; Ballotari, P.; Cestari, L.; et al. Differences in mortality by immigrant status in Italy. Results of the Italian Network of Longitudinal Metropolitan Studies. Eur. J. Epidemiol. 2016, 31, 691–701. [Google Scholar] [CrossRef] [PubMed]
- Baggett, T.P.; Tobey, M.L.; Rigotti, N.A. Tobacco use among homeless people--addressing the neglected addiction. N. Engl. J. Med. 2013, 369, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Baggett, T.P.; Chang, Y.; Singer, D.E.; Porneala, B.C.; Gaeta, J.M.; O’Connell, J.J.; Rigotti, N.A. Tobacco-, alcohol-, and drug-attributable deaths and their contribution to mortality disparities in a cohort of homeless adults in Boston. Am. J. Public Health 2015, 105, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Baggett, T.P.; Rigotti, N.A. Cigarette smoking and advice to quit in a national sample of homeless adults. Am. J. Prev. Med. 2010, 39, 164–172. [Google Scholar] [CrossRef]
- Snyder, L.D.; Eisner, M.D. Obstructive lung disease among the urban homeless. Chest 2004, 125, 1719–1725. [Google Scholar] [CrossRef]
- Weinreb, L.; Goldberg, R.; Perloff, J. Health characteristics and medical service use patterns of sheltered homeless and low-income housed mothers. J. Gen. Intern. Med. 1998, 13, 389–397. [Google Scholar] [CrossRef][Green Version]
- Holowatyj, A.N.; Heath, E.I.; Pappas, L.M.; Ruterbusch, J.J.; Gorski, D.H.; Triest, J.A.; Park, H.K.; Beebe-Dimmer, J.L.; Schwartz, A.G.; Cote, M.L.; et al. The Epidemiology of Cancer Among Homeless Adults in Metropolitan Detroit. JNCI Cancer Spectr. 2019, 3, pkz006. [Google Scholar] [CrossRef]
- Hwang, S.W. Homelessness and health. CMAJ 2001, 164, 229–233. [Google Scholar]
- Crowe, C.; Hardill, K. Nursing research and political change: The street health report. Can. Nurse 1993, 89, 21–24. [Google Scholar]
- Ralli, M.; Arcangeli, A.; Morrone, A.; Ercoli, L. Characteristics of COVID-19 in Homeless Shelters: The Importance of Asymptomatic Transmission. Ann. Intern. Med. 2020, 174, 42–49. [Google Scholar]
- Ralli, M.; Morrone, A.; Arcangeli, A.; Ercoli, L. Asymptomatic patients as a source of transmission of COVID-19 in homeless shelters. Int. J. Infect Dis. 2020, 103, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Opalach, C.; Romaszko, J.; Jaracz, M.; Kuchta, R.; Borkowska, A.; Bucinski, A. Coping Styles and Alcohol Dependence among Homeless People. PLoS ONE 2016, 11, e0162381. [Google Scholar] [CrossRef]
- Ngo, A.N.; Islam, M.A.; Aoyagi, J.; Sandor, Z.; Sandor, S. Prevalence of Hypertension in Homeless Adults: An Interprofessional Education Community-Based Health Fairs Cross-Sectional Study in Urban Long Beach, California. High Blood Press Cardiovasc. Prev. 2021, 28, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Reitzel, L.R.; Chinamuthevi, S.; Daundasekara, S.S.; Hernandez, D.C.; Chen, T.A.; Harkara, Y.; Obasi, E.M.; Kendzor, D.E.; Businelle, M.S. Association of Problematic Alcohol Use and Food Insecurity among Homeless Men and Women. Int. J. Environ. Res. Public Health 2020, 17, 3631. [Google Scholar] [CrossRef] [PubMed]
- Fischer, P.J.; Breakey, W.R. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am. Psychol. 1991, 46, 1115–1128. [Google Scholar] [CrossRef]
- Drake, M.A. The nutritional status and dietary adequacy of single homeless women and their children in shelters. Public Health Rep. 1992, 107, 312–319. [Google Scholar]
- Bernstein, R.S.; Meurer, L.N.; Plumb, E.J.; Jackson, J.L. Diabetes and hypertension prevalence in homeless adults in the United States: A systematic review and meta-analysis. Am. J. Public Health 2015, 105, e46–e60. [Google Scholar] [CrossRef]
- Asgary, R.; Sckell, B.; Alcabes, A.; Naderi, R.; Schoenthaler, A.; Ogedegbe, G. Rates and Predictors of Uncontrolled Hypertension Among Hypertensive Homeless Adults Using New York City Shelter-Based Clinics. Ann. Fam. Med. 2016, 14, 41–46. [Google Scholar] [CrossRef]
- Chen, C.L.; Chen, M.; Liu, C.K. The Effects of Obesity-Related Anthropometric Factors on Cardiovascular Risks of Homeless Adults in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 6833. [Google Scholar] [CrossRef]
- Yamamoto, M.; Horita, R.; Sado, T.; Nishio, A. Non-communicable Disease among Homeless Men in Nagoya, Japan: Relationship between Metabolic Abnormalities and Sociodemographic Backgrounds. Intern. Med. 2020, 59, 1155–1162. [Google Scholar] [CrossRef]
- Gozdzik, A.; Salehi, R.; O’Campo, P.; Stergiopoulos, V.; Hwang, S.W. Cardiovascular risk factors and 30-year cardiovascular risk in homeless adults with mental illness. BMC Public Health 2015, 15, 165. [Google Scholar] [CrossRef] [PubMed]
- Baggett, T.P.; Liauw, S.S.; Hwang, S.W. Cardiovascular Disease and Homelessness. J. Am. Coll. Cardiol. 2018, 71, 2585–2597. [Google Scholar] [CrossRef] [PubMed]
- Al-Shakarchi, N.J.; Evans, H.; Luchenski, S.A.; Story, A.; Banerjee, A. Cardiovascular disease in homeless versus housed individuals: A systematic review of observational and interventional studies. Heart 2020, 106, 1483–1488. [Google Scholar] [CrossRef]
- Shiue, I. Is being homeless or worried about housing associated with allergies and skin problems? Ann. Allergy Asthma. Immunol. 2014, 112, 384–386. [Google Scholar] [CrossRef] [PubMed]
- Huynh, M.; Gupta, R.; Koo, J.Y. Emotional stress as a trigger for inflammatory skin disorders. Semin. Cutan. Med. Surg. 2013, 32, 68–72. [Google Scholar] [CrossRef]
- Orion, E.; Wolf, R. Psychological factors in skin diseases: Stress and skin: Facts and controversies. Clin. Dermatol. 2013, 31, 707–711. [Google Scholar] [CrossRef]
- Ayano, G.; Assefa, D.; Haile, K.; Chaka, A.; Solomon, H.; Hagos, P.; Yohannis, Z.; Haile, K.; Bekana, L.; Agidew, M.; et al. Mental, neurologic, and substance use (MNS) disorders among street homeless people in Ethiopia. Ann. Gen. Psychiatry 2017, 16, 40. [Google Scholar] [CrossRef]
- Fazel, S.; Khosla, V.; Doll, H.; Geddes, J. The prevalence of mental disorders among the homeless in western countries: Systematic review and meta-regression analysis. PLoS Med. 2008, 5, e225. [Google Scholar] [CrossRef]
- Hadland, S.E.; Marshall, B.D.; Kerr, T.; Qi, J.; Montaner, J.S.; Wood, E. Depressive symptoms and patterns of drug use among street youth. J. Adolesc. Health 2011, 48, 585–590. [Google Scholar] [CrossRef]
- Scott, J. Homelessness and mental illness. Br. J. Psychiatry 1993, 162, 314–324. [Google Scholar] [CrossRef]
- Breakey, W.R.; Fischer, P.J.; Kramer, M.; Nestadt, G.; Romanoski, A.J.; Ross, A.; Royall, R.M.; Stine, O.C. Health and mental health problems of homeless men and women in Baltimore. JAMA 1989, 262, 1352–1357. [Google Scholar] [CrossRef] [PubMed]
- Gelberg, L.; Linn, L.S. Demographic differences in health status of homeless adults. J. Gen. Intern. Med. 1992, 7, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Jun, J.S.; Kim, Y.J.; Roh, S.; Moon, S.S.; Bukonda, N.; Hines, L. Mental Health, Substance Abuse, and Suicide Among Homeless Adults. J. Evid. Inf. Soc. Work 2017, 14, 229–242. [Google Scholar] [CrossRef] [PubMed]
- Berg, J.; Nyamathi, A.; Christiani, A.; Morisky, D.; Leake, B. Predictors of screening results for depressive symptoms among homeless adults in Los Angeles with latent tuberculosis. Res. Nurs. Health 2005, 28, 220–229. [Google Scholar] [CrossRef]
- Brown, R.T.; Kiely, D.K.; Bharel, M.; Mitchell, S.L. Factors associated with geriatric syndromes in older homeless adults. J. Health Care Poor Underserved 2013, 24, 456–468. [Google Scholar] [CrossRef]
- Coohey, C.; Easton, S.D.; Kong, J.; Bockenstedt, J.K. Sources of psychological pain and suicidal thoughts among homeless adults. Suicide Life Threat. Behav. 2015, 45, 271–280. [Google Scholar] [CrossRef]
- Crawford, D.M.; Trotter, E.C.; Hartshorn, K.J.; Whitbeck, L.B. Pregnancy and mental health of young homeless women. Am. J. Orthopsychiatry 2011, 81, 173–183. [Google Scholar] [CrossRef]
- Hynes, F.; Kilbride, K.; Fenton, J. A survey of mental disorder in the long-term, rough sleeping, homeless population of inner Dublin. Ir. J. Psychol. Med. 2019, 36, 19–22. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iacoella, C.; De-Giorgio, F.; Palaia, G.; Ferraioli, M.; Arcangeli, A.; Ralli, M. Evaluation of General Health Status of Persons Living in Socio-Economically Disadvantaged Neighborhoods in a Large European Metropolitan City. Appl. Sci. 2022, 12, 7428. https://doi.org/10.3390/app12157428
Iacoella C, De-Giorgio F, Palaia G, Ferraioli M, Arcangeli A, Ralli M. Evaluation of General Health Status of Persons Living in Socio-Economically Disadvantaged Neighborhoods in a Large European Metropolitan City. Applied Sciences. 2022; 12(15):7428. https://doi.org/10.3390/app12157428
Chicago/Turabian StyleIacoella, Claudia, Fabio De-Giorgio, Gaspare Palaia, Mario Ferraioli, Andrea Arcangeli, and Massimo Ralli. 2022. "Evaluation of General Health Status of Persons Living in Socio-Economically Disadvantaged Neighborhoods in a Large European Metropolitan City" Applied Sciences 12, no. 15: 7428. https://doi.org/10.3390/app12157428
APA StyleIacoella, C., De-Giorgio, F., Palaia, G., Ferraioli, M., Arcangeli, A., & Ralli, M. (2022). Evaluation of General Health Status of Persons Living in Socio-Economically Disadvantaged Neighborhoods in a Large European Metropolitan City. Applied Sciences, 12(15), 7428. https://doi.org/10.3390/app12157428







