Abstract
This practice-based study presents the clinical outcomes of a minimally invasive method for retrieving failed dental implants from elderly patients. Traditional removal methods for failed dental implants include trephination and other invasive procedures. That can be a special concern for the elderly, since aging exacerbates oral surgery-related morbidity and anxiety. This retrospective cohort study gathers data from 150 patients seen in a private clinic. Their implants (n = 199) failed due to biological, mechanical, or iatrogenic causes, and were removed as part of their treatment plan. Collected data included: (1) implant location (maxilla/mandible, anterior/posterior region), (2) reasons for implant retrieval, (3) connection type, (4) removal torque, and (5) operatory procedure—flapless and using a counter-torque removal kit, whenever possible. Flapless/minimally invasive retrieval was successful for 193 implants (97%). The remaining six implants demanded trephination (open-flap). The most common reasons for implant retrieval (81%) involved biological aspects, whereas iatrogenic (12%) and biomechanical (7%) reasons were less common. The surgical technique used was not associated to connection types or removal torque. Authors conclude that a counter-torque ratchet system is a minimally invasive technique with a high success rate in retrieving implants from elderly patients. Present findings support its use as a first-line approach for implant retrieval in that population.
1. Introduction
Treatment with dental implants has become routine for partially and completely edentulous elderly patients [1], with increased use in recent years [2,3]. Such a frequent use invariably leads to a large number of failed implants, i.e., a high absolute number of failures despite the high success rates of contemporary implant systems, as also reported for orthopedic and osteosynthesis implants [4,5].
It is noteworthy that dental implants are expected to remain in the oral cavity for a long time [6], exposing them to a series of biological and biomechanical challenges that may lead to failure. Moreover, there are cases of unsatisfactorily placed implants that need retrieval, i.e., removal due to iatrogenic reasons [7]. The decision whether to retrieve an implant must consider many factors, including its restorability, integrity and peri-implant health [8].
The wide variation in contemporary implant designs leads to varying failure rates. For instance, different alloys, macrogeometry, surface treatments, connection types and sizes may lead to varying odds of biomechanical failure [9,10]. Usually, a failed implant needs removal, regardless of being replaced or not. Traditional approaches for implant removal involve peri-implant osteotomy with burs or trephines, followed by extraction with forceps or an elevator [11]. The use of burs tends to be time consuming and especially disturbing for patients [11], and may leave implant fragments in the wound [12]. Trephination tends to be relatively traumatic [13], with significant damage to the bone around the implant. Moreover, straying from the long axis of the implant is a possibility, which can be critical with narrow ridges [11]. More recently, piezoelectric devices have become a popular choice for osteotomy [14]. Although invasiveness tends to be reduced, the latter method still results in the removal of healthy bone.
Traditional implant retrieval techniques are inadequate for many elderly patients. Preoperative anxiety may be overwhelming and healing may be impaired in many cases; therefore, surgical trauma should be minimal in the elderly [15]. Peculiarities of that population have driven the development of minimally invasive devices for implant retrieval and other procedures [6].
Less invasive approaches for implant retrieval include reverse screws and high torque wrenches. Their use may be more acceptable by the elderly, since those approaches do not demand osteotomy or even flap elevation. Those devices combine a more comfortable procedure for the patient with much lower tissue trauma. Moreover, better preservation of peri-implant tissues enables immediate placement of a new implant in many cases [12].
Previous attempts to retrieve implants conservatively have showed promising results, including the study by Anitua [16,17]. However, a large number of patients (13%) still needed traditional removal. That study used a reverse torque instrument that could reach a maximum of 200 Ncm, whereas a higher torque may still be safe. Moreover, there is no published data about a minimally invasive implant removal protocol for the elderly. Therefore, the aim of this study was to evaluate the success rate of a minimally invasive method of implant retrieval in elderly patients.
2. Materials and Methods
This study followed a retrospective cohort design. More specifically, a sample of patients treated in a private dental clinic (Santiago, Chile) had their data reviewed after receiving an indication for implant removal.
The following study was approved by the ethics committee of the Eastern Metropolitan Health Service (SSMO) of Santiago (Chile), and performed following the principles outlined in the Declaration of Helsinki. Since this study was based on data from patient forms, no research-specific consent form was applied. However, all patients had read and signed a consent form before dental treatment, agreeing with the possible confidential use of their clinical forms for research. Consent for clinical care was sought after notifying patients about implant failure, proposed treatment procedures, and risks/benefits.
The study included all 150 patients treated between 2017 and 2020, wherein 199 implants were considered as failed. A dentist with 15 years of experience in oral implantology examined the patients and decided on implant removal based on biological, mechanical, or iatrogenic causes. Removal was indicated as part of the treatment plan.
Among patients with an indication for implant removal, we included only independent elderly adults (60 years or more). Participants had a pretreatment history of osseointegrated implants exposed to the oral environment. Moreover, inclusion depended on having implants with at least one of the three conditions: (1) horizontal bone loss observed through routine oral radiographs, greater than the first three threads of the implant and associated with signs of peri-implant inflammation; (2) implants without the possibility of predictable prosthetic rehabilitation or with possible aesthetic implications, and (3) defective retention system, i.e., damaged hexagon, deformed internal thread or fractured abutment screw with no possibility of removal. Furthermore, the exclusion criteria were (1) radiographic image compatible with lack of osseointegration, (2) implant mobility, and (3) implants with pain to percussion test.
Retrieval of all implants was initiated by using a reverse torque implant removal toolkit (Neo Fixture Remover, Neobiotech, Seoul, Korea; Figure 1), without the requirement of raising a flap. Implant retrieval begins by inserting a torqued stem at 40–80 Ncm into the internal implant thread, followed by the attachment of an implant extractor device (Figure 1A), which is screwed to the initial stem in the opposite direction. When both devices were assembled, counter-torque is performed using a torque ratchet (Figure 1B), at which the removal device is firmly fixed to the implant. In turn, removal occurs consequently to reverse torque oscillating between 100 and 500 Ncm (Figure 1C,D).
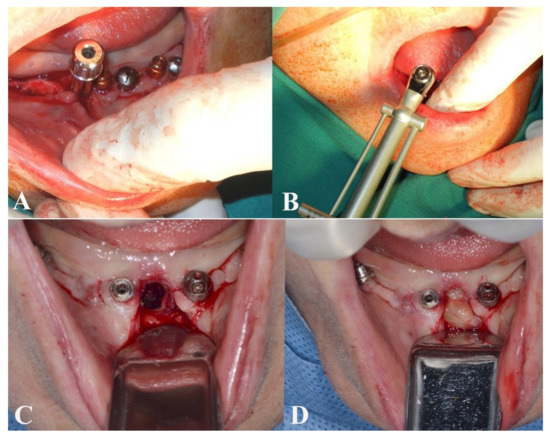
Figure 1.
Both methods used for implant retrieval. (A). The device screwed to the initial stem in the opposite direction. (B). Torque ratchet to perform counter-torque for implant removal. (C). Bone defect after removal with trephine bur. (D). Defect healing with L-PRF clot.
Traditional trephination took place whenever implant removal was not viable by the previous technique. In those cases, a flap was raised to expose the failed implant. In turn, peri-implant osteotomy was performed by using a trephine of the same diameter as the implants (Figure 2A). Those cases counted as failed use of the reverse torque system (Figure 2B).

Figure 2.
Implants removed through both methods. (A). Trephine bur, observing a bone ring surrounding the removed implant. (B). Implant removal with the counter-torque system, noting a less invasive procedure.
Data collected from patient forms for this study included: (1) implant location, by arch (maxilla/mandible) and region (anterior/posterior); (2) cause of failure, classified as iatrogenic (wrong location or impossibility to be rehabilitated), biological (peri-implantitis with poor prognosis in the short/medium term), and mechanical (fractured implant or damaged internal connection); (3) implant connection, external/internal, and (4) removal torque (Ncm).
Regarding sample size, this study used a convenience sample corresponding to all potentially eligible patients of the study clinic. That clinic has used the tested implant removal equipment since its clearance for patient use in Chile in 2017.
Statistical analysis was performed using SPSS version 22.0 (SPSS Inc, Chicago, IL, USA) with a significance level of 0.05. The Shapiro–Wilk test was used to evaluate data distribution. One-way ANOVA was used to determine the association between removal torque and the cause of failure (post-hoc test: Scheffé), while a two-tailed t test was applied for independent samples to compare the values between the two connection types and the difference in the anterior and posterior region of the mandible/maxilla.
3. Results
Our participant sample was composed of 94 women and 56 men, with a mean age (SD) of 68 (3) years. They had 199 implants indicated for removal, with most (n = 134, 67.3%) being used to retain single crowns. The remaining implants were used for the treatment of fully edentulous arches by fixed prostheses (n = 29, 14.6%) or overdentures (n = 36, 18.1%).
The implant removal system had a success rate of 97%, i.e., 193 implants were removed without requiring flap elevation. However, six implants demanded trephination. Of these six implants, there were four cases of implant fracture during use of the removal kit, whereas two implants could not be removed even with maximum torque (i.e., 500 Ncm).
With respect to the cause of failure, 12% were identified as iatrogenic, whereas 81% and 7% were attributed to biological and mechanical causes, respectively. There was no case with more than one cause of failure. The mean removal torque was 220 Ncm, with significantly higher torque for the anterior mandible (mean: 308 Ncm) compared to the other areas (Table 1). Removal torque achieved at least 450 Ncm in four cases. The type of connection did not influence removal torque values significantly (Table 2). There was no significant difference between the three possible causes of failure either (mean torque, iatrogenic: 219 Ncm, biological: 222 Ncm, mechanical: 250 Ncm).

Table 1.
Mean removal torque according to implant location.

Table 2.
Mean and ranges of removal torque according to implant connection.
4. Discussion
This practice-based clinical study discloses the success rate of a novel instrument kit for implant retrieval, with promising use for elderly patients. We found a remarkably high success rate with that kit, which simply acts by the direct application of reverse torque on the implant platform. Few cases needed the elevation of a flap and other surgical procedures, which followed traditional protocols. Complications were rare and could be managed by routine procedures.
The successful removal of almost all implants (97%) is likely due to well-distributed shear stresses in the implant-bone junction. For our participants, the counter-torque ratchet system preserved hard and soft tissues, and prevented the relatively large defects produced by the trephine-bur technique. Those advantages favored the immediate placement of a new implant whenever indicated. The study by Anitua et al. [16,17] reported close success rates with a comparable device, i.e., between 86% and 88% of implant removal, with 12–14% of implants removed by trephination. The tested device explains those slightly lower success rates, since it allows a maximum removal torque of 200 Ncm. Applying the same cutoff in this study would impact the observed success rate, since 54% of implants required a higher removal torque. This would be critical for the anterior mandible. Although torque values are significantly higher in that region, it is the preferred place for implant placement in edentulous patients.
Present results imply that counter-torque removal of implants can use higher torques than previously thought. Previous studies recommended avoiding torque values above 120–190 Ncm, which are supposed to increase the risk of bone fracture [18,19]. Previous implant removal instructions included piezoelectric osteotomy around the coronal third of the implant whenever the torque reached 200 Ncm [20]. Reviewing that cutoff can certainly make removal procedures more conservative, since well-distributed stress may lead to the safe use of high torque values.
Since a counter-torque device allows minimal or no bone damage for implant removal, this can be critical for the elderly. Firstly, aging tends to diminish bone quantity and quality, making peri-implant ridge preservation even more important [1]. Moreover, many elderly patients are not good candidates for oral surgery [21], partly due to associated systemic comorbidities and eventual frailty [1,22]. Minimally invasive approaches (such as counter-torque devices) may enable elective implant removal in cases for which it would be contraindicated otherwise, by reducing postoperative morbidity as well as healing and treatment time. In other words, our results imply that the tested device can be a first choice for the elderly rather than trephination, due to its high success rate and less invasive nature.
There is an inherent need to prioritize immediate implant installation following the removal of a failed fixture [16,23], if the biological and patient-centered aspects favor it. Thus, the device tested in this study would meet this objective and allow the implant installation immediately upon removal.
The removal torque values are known to depend on the bone quality [24], implant diameter [12,25], shape, and surface type [26] among others. As expected, the highest removal torque values were identified in the anterior mandible, due to the highest bone density of this region [27,28]. Four implants required nearly 450 Ncm for the removal from that region. Despite the development of new implant designs with improvements in their biomechanics [10], the type of connection (internal or external) had no influence on removal torque, even if implant design is expected to influence removal values [20]. Probably both connections were robust enough to transmit stress efficiently with the tested device.
Whereas the most common reasons for the removal of orthopedic implants and osteosynthesis screws are iatogrenic and biomechanical [5], the most common cause of dental implant failure was observed to be biological. This finding is concurrent with previous research [11,16,21], given the constant exposure of dental implants to the oral microbiota. Iatrogenic factors were the second cause of implant failure, i.e., non-restorable positions [8], concurring with the rate (12–14%) of other studies [16,17]. This shows that the sample is representative since the most frequent causes of implant failure are consistent with what was previously reported.
Different from the study of Anitua et al. [17], which compared the surface of removed implants, this study was unable to identify specific surface treatments. Studied patients had their implants placed by other dentists. Different treatments may influence surface energy, improve the osteoblast proliferation and the bone-implant contact [29,30,31], and consequently, the osseointegration, which can be related or not with the torque values during the removal procedure. However, authors understand that present findings reflect a pragmatic sample, and thus can be applied to elderly patients needing implant removal.
Among the limitations of the study, one can mention the elderly population, which precludes extrapolation to young adults. However, answering questions specifically for this population is paramount, since they need minimally invasive procedures the most. In addition, other limitations were that the level of satisfaction between groups (trephine vs. removal kit) was not compared, as well as potential selection bias since it was a convenience sample. However, our practice-based study provides realistic results of our daily clinical routine, as stated by Emami et al. [32]. Furthermore, a systematic review [20] reported that most of the studies regarding implant removal have considerable issues, including small sample sizes, no disclosure of complications and misuse of statistical methods. We tackled those issues by reaching a considerable sample size, careful statistical analysis and reporting adversities. However, randomized clinical trials considering patient-reported outcomes studies are still needed to determine the best implant removal method for elderly patients.
In conclusion, the use of a counter-torque ratchet system is a minimally invasive technique with a high success rate, which reduces the postoperative morbidity and the time of healing/treatment in elderly individuals.
Author Contributions
Conceptualization, Y.L. and E.B.; methodology, B.W.; formal analysis, J.M. and R.F.d.S.; investigation, Y.L., E.B., R.F.d.S.; data curation, J.M., R.F.d.S.; writing—original draft preparation, R.F.d.S., B.W. and E.B.; writing—review and editing, Y.L., E.B., R.F.d.S., B.W. and J.M.; supervision, E.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Eastern Metropolitan Health Service (SSMO) of Santiago (Chile).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to data include some names of the clinicians that placed previously the implants (including iatrogenic) as well as the brands of retrieved implants.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Park, J.C.; Baek, W.S.; Choi, S.H.; Cho, K.S.; Jung, U.W. Long-term outcomes of dental implants placed in elderly patients: A retrospective clinical and radiographic analysis. Clin. Oral Implant. Res. 2017, 28, 186–191. [Google Scholar] [CrossRef]
- Elani, H.W.; Starr, J.R.; Da Silva, J.D.; Gallucci, G.O. Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026. J. Dent. Res. 2018, 97, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Gaviria, L.; Salcido, J.P.; Guda, T.; Ong, J.L. Current trends in dental implants. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Yeakley, B.; Goswami, T. Orthopedic implant retrieval—Imperatives and possibilities. Ann. Biomed. Eng. 2009, 37, 2326–2336. [Google Scholar] [CrossRef]
- Nica, N.; Cretu, B.; Ene, D.; Antoniac, I.; Gheorghita, D.; Ene, R. Failure analysis of retrieved osteosynthesis implants. Materials 2020, 13, 1201. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, M.; Muller, F.; Suter, V.; Buser, D. Implants for elderly patients. Periodontol. 2000 2017, 73, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Coelho, P.G.; Marin, C.; Granato, R.; Suzuki, M. Histomorphologic analysis of 30 plateau root form implants retrieved after 8 to 13 years in function. A human retrieval study. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 91, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Tarnow, D.P.; Chu, S.J. When to save or remove implants in the smile zone: A clinical report of maxillary lateral incisor implants in malposition. J. Esthet. Restor. Dent. 2021. [Google Scholar] [CrossRef]
- Hasan, I.; Heinemann, F.; Aitlahrach, M.; Bourauel, C. Biomechanical finite element analysis of small diameter and short dental implant. Biomed. Tech. 2010, 55, 341–350. [Google Scholar] [CrossRef]
- Borie, E.; Orsi, I.A.; de Araujo, C.P. The influence of the connection, length and diameter of an implant on bone biomechanics. Acta Odontol. Scand. 2015, 73, 321–329. [Google Scholar] [CrossRef]
- Stajcic, Z.; Stojcev Stajcic, L.J.; Kalanovic, M.; Dinic, A.; Divekar, N.; Rodic, M. Removal of dental implants: Review of five different techniques. Int. J. Oral Maxillofac. Surg. 2016, 45, 641–648. [Google Scholar] [CrossRef]
- Froum, S.; Yamanaka, T.; Cho, S.C.; Kelly, R.; James, S.S.; Elian, N. Techniques to remove a failed integrated implant. Compend. Contin. Educ. Dent. 2011, 32, 22–26. [Google Scholar]
- Watanabe, F.; Hata, Y.; Mataga, I.; Yoshie, S. Retrieval and replacement of a malpositioned dental implant: A clinical report. J. Prosthet. Dent. 2002, 88, 255–258. [Google Scholar] [CrossRef]
- Kwon, Y.D.; Pae, A. Piezoelectric Trapezoidal Osteotomy for the Retrieval of a Displaced Dental Implant in the Osteoporotic Mandibular Body. Implant. Dent. 2016, 25, 703–706. [Google Scholar] [CrossRef] [PubMed]
- Müller, F.; Salem, K.; Barbezat, C.; Herrmann, F.R.; Schimmel, M. Knowledge and attitude of elderly persons towards dental implants. Gerodontology 2012, 29, e914–e923. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Orive, G. A new approach for atraumatic implant explantation and immediate implant installation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, e19–e25. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Murias-Freijo, A.; Alkhraisat, M.H. Conservative Implant Removal for the Analysis of the Cause, Removal Torque, and Surface Treatment of Failed Nonmobile Dental Implants. J. Oral Implantol. 2016, 42, 69–77. [Google Scholar] [CrossRef]
- Bozkaya, D.; Muftu, S.; Muftu, A. Evaluation of load transfer characteristics of five different implants in compact bone at different load levels by finite elements analysis. J. Prosthet. Dent. 2004, 92, 523–530. [Google Scholar] [CrossRef]
- Frost, H.M. Bone’s mechanostat: A 2003 update. Anat. Rec. A Discov. Mol. Cell. Evol. Biol. 2003, 275, 1081–1101. [Google Scholar] [CrossRef]
- Roy, M.; Loutan, L.; Garavaglia, G.; Hashim, D. Removal of osseointegrated dental implants: A systematic review of explantation techniques. Clin. Oral Investig. 2020, 24, 44–60. [Google Scholar] [CrossRef]
- Greenstein, G.; Cavallaro, J. Failed dental implants: Diagnosis, removal and survival of reimplantations. J. Am. Dent. Assoc. 2014, 145, 835–842. [Google Scholar] [CrossRef]
- Müller, F. Interventions for edentate elders—What is the evidence? Gerodontology 2014, 31 (Suppl. 1), 44–51. [Google Scholar]
- Covani, U.; Barone, A.; Cornelini, R.; Crespi, R. Clinical outcome of implants placed immediately after implant removal. J. Periodontol. 2006, 77, 722–727. [Google Scholar] [CrossRef]
- Anil, S.; Aldosari, A.A. Impact of bone quality and implant type on the primary stability: An experimental study using bovine bone. J. Oral Implantol. 2015, 41, 144–148. [Google Scholar] [CrossRef]
- Ivanoff, C.J.; Sennerby, L.; Johansson, C.; Rangert, B.; Lekholm, U. Influence of implant diameters on the integration of screw implants. An experimental study in rabbits. Int. J. Oral Maxillofac. Surg. 1997, 26, 141–148. [Google Scholar] [CrossRef]
- Elias, C.N.; Oshida, Y.; Lima, J.H.; Muller, C.A. Relationship between surface properties (roughness, wettability and morphology) of titanium and dental implant removal torque. J. Mech. Behav. Biomed. Mater. 2008, 1, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Norton, M.R.; Gamble, C. Bone classification: An objective scale of bone density using the computerized tomography scan. Clin. Oral Implant. Res. 2001, 12, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Shapurian, T.; Damoulis, P.D.; Reiser, G.M.; Griffin, T.J.; Rand, W.M. Quantitative evaluation of bone density using the Hounsfield index. Int. J. Oral Maxillofac. Implantol. 2006, 21, 290–297. [Google Scholar]
- Bosshardt, D.; Chappuis, V.; Buser, D. Osseointegration of titanium, titanium alloy and zirconia dental implants: Current knowledge and open questions. Periodontol. 2000 2017, 73, 22–40. [Google Scholar] [CrossRef]
- Rupp, F.; Liang, L.; Geis-Gerstorfer, J.; Scheideler, L.; Hüttig, F. Surface characteristics of dental implants: A review. Dent. Mater. 2018, 34, 40–57. [Google Scholar] [CrossRef]
- Dias, F.J.; Fuentes, R.; Navarro, P.; Weber, B.; Borie, E. Assessment of the Chemical Composition in Diferent Dental Implant Types: An Analysis through EDX System. Coatings 2020, 10, 882. [Google Scholar] [CrossRef]
- Emami, E.; de Souza, R.F.; Bernier, J.; Rompré, P.; Feine, J.S. Patient perceptions of the mandibular three-implant overdenture: A practice-based study. Clin. Oral Implant. Res. 2015, 26, 639–643. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).