DynamiChain: Development of Medical Blockchain Ecosystem Based on Dynamic Consent System
Abstract
1. Introduction
2. Related Works
2.1. Related Concept
2.2. Related Research
3. Proposed System
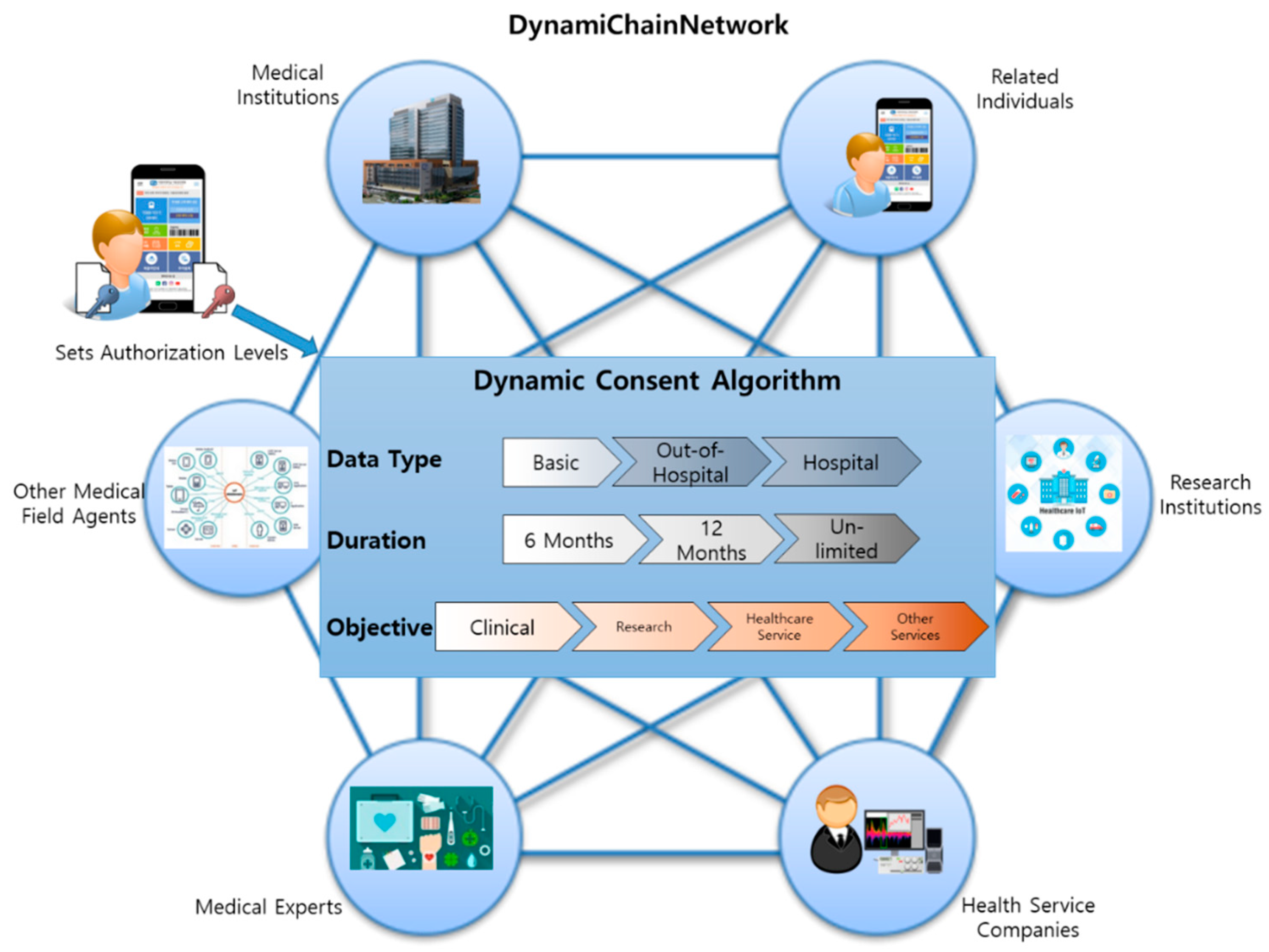
3.1. Overall System Architecture
3.2. Specific System Functions
3.3. Dynamic Consent Algorithm
3.4. Restricted Medical Data Policy Applied Work Flow Specifications
4. Implementation
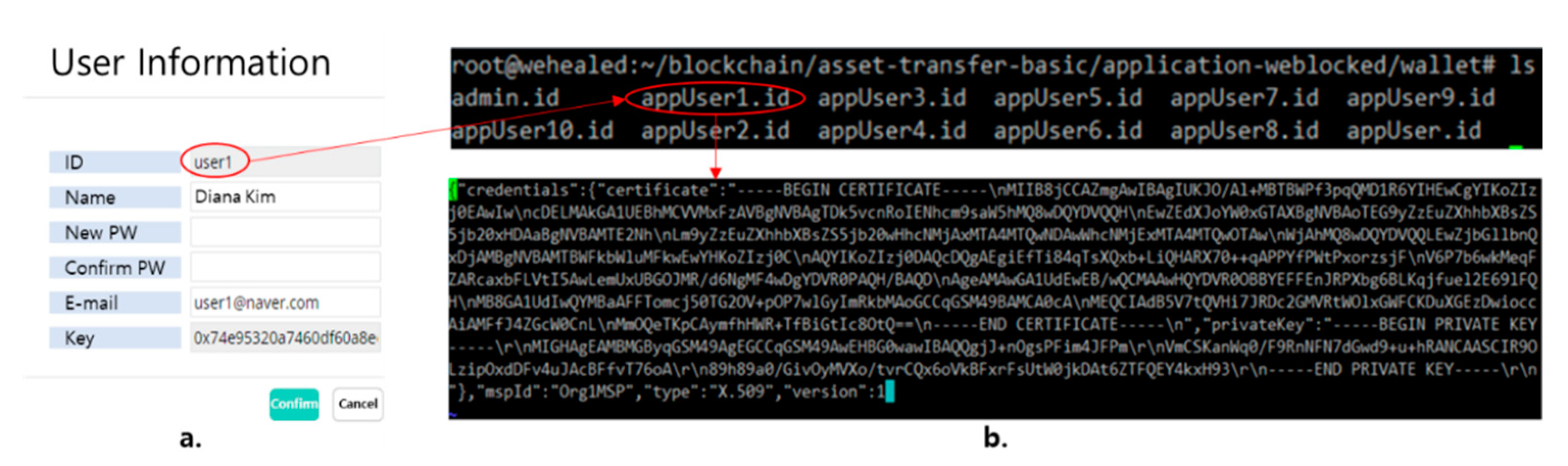
4.1. DynamiChain Network Based on Hyperledger Fabric
4.2. Dynamic Consent System
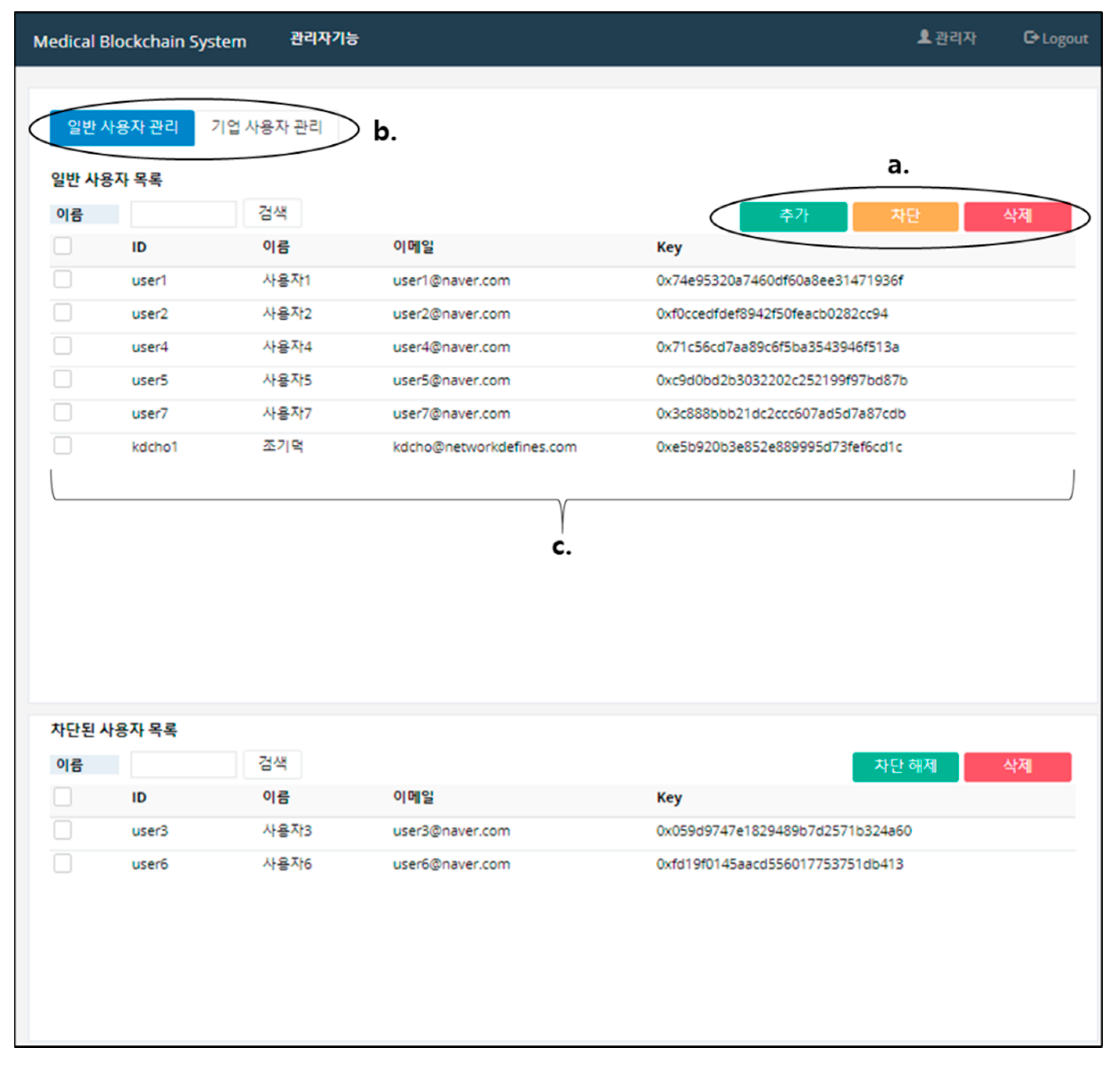
4.3. Security Management System
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wu, S.; Chen, Y.; Wang, Q.; Li, M.; Wang, C.; Luo, X. CReam: A smart contract enabled collusion-resistant e-auction. IEEE Trans. Inf. Forensics Secur. 2019, 14, 1687–1701. [Google Scholar] [CrossRef]
- Wang, S.; Ouyang, L.; Yuan, Y.; Ni, X.; Han, X.; Wang, F.-Y. Blockchain-enabled smart contracts: Architecture, applications, and future trends. IEEE Trans. Syst. Man Cybern. 2019, 49, 2266–2277. [Google Scholar] [CrossRef]
- Gao, F. Data encryption algorithm for e-commerce platform based on blockchain technology. Discret. Contin. Dyn. Syst. S 2019, 12, 1457–1470. [Google Scholar] [CrossRef]
- Christidis, K.; Devetsikiotis, M. Blockchains and smart contracts for the Internet of Things. IEEE Access 2016, 4, 2292–2303. [Google Scholar] [CrossRef]
- Zheng, X.; Sun, S.; Mukkamala, R.R.; Vatrapu, R.; Ordieres-Mere, J. Accelerating health data sharing: A solution based on the Internet of Things and distributed ledger technologies. J. Med. Internet Res. 2019, 21, e13583. [Google Scholar] [CrossRef]
- Khan, F.A.; Asif, M.; Ahmad, A.; Alharbi, M.; Aljuaid, H. Blockchain technology, improvement suggestions, security challenges on smart grid and its application in healthcare for sustainable development. Sustain. Cities Soc. 2020, 55, 102018. [Google Scholar] [CrossRef]
- Meiklejohn, S.; Pomarole, M.; Jordan, G.; Levchenko, K.; McCoy, D.; Voelker, G.M.; Savage, S. A fistful of bitcoins: Characterizing payments among men with no names. In Proceedings of the 2013 Conference on Internet Measurement Conference, Barcelona, Spain, 23–25 October 2013; pp. 127–140. [Google Scholar]
- Kosba, A.; Miller, A.; Shi, E.; Wen, Z.; Papamanthou, C. Hawk: The blockchain model of cryptography and privacy-preserving smart contracts. In Proceedings of the 2016 IEEE Symposium on Security and Privacy (SP), San Jose, CA, USA, 22–26 May 2016; pp. 839–858. [Google Scholar]
- Biryukov, A.; Khovratovich, D.; Pustogarov, I. Deanonymisation of clients in Bitcoin P2P network. In Proceedings of the 2014 ACM SIGSAC Conference on Computer and Communications Security, Scottsdale, AZ, USA, 3–7 November 2014; pp. 15–29. [Google Scholar]
- Zheng, Z.; Xie, S.; Dai, H.; Chen, X.; Wang, H. An overview of blockchain technology: Architecture, consensus, and future trends. In Proceedings of the 2017 IEEE International Congress on Big Data (BigData Congress), Honolulu, HI, USA, 25–30 June 2017; pp. 557–564. [Google Scholar]
- Mehar, M.I.; Shier, C.L.; Giambattista, A.; Gong, E.; Fletcher, G.; Sanayhie, R.; Kim, H.M.; Laskowski, M. Understanding a revolutionary and flawed grand experiment in blockchain: The DAO attack. J. Cases Inf. Technol. 2019, 21, 19–32. [Google Scholar] [CrossRef]
- Ghaleb, B.; Al-Dubai, A.; Ekonomou, E.; Qasem, M.; Romdhani, I.; Mackenzie, L. Addressing the DAO insider attack in RPL’s Internet of Things networks. IEEE Commun. Lett. 2019, 23, 68–71. [Google Scholar] [CrossRef]
- Wadhaj, I.; Ghaleb, B.; Thomson, C.; Al-Dubai, A.; Buchanan, W.J. Mitigation mechanisms against the DAO attack on the routing protocol for low power and lossy networks (RPL). IEEE Access 2020, 8, 43665–43675. [Google Scholar] [CrossRef]
- Dwork, C.; Naor, M. Pricing via processing or combatting junk mail. In Proceedings of the Annual International Cryptology Conference, Santa Barbara, CA, USA, 16–20 August 1992; pp. 139–147. [Google Scholar]
- Jakobsson, M.; Juels, A. Proofs of work and bread pudding protocols. In Secure Information Networks; Springer: Berlin/Heidelberg, Germany, 1999; pp. 258–272. [Google Scholar]
- Song, R.; Song, Y.; Liu, Z.; Tan, M.; Zhou, K. GaiaWorld: A Novel Blockchain System Based on Competitive PoS Consensus Mechanism. CMC Comput. Mater. Contin. 2019, 60, 973–987. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, S.; Yang, M.; He, P.; Wang, Q. Research on Architecture of Risk Assessment System Based on BlockChain. CMC Comput. Mater. Contin. 2019, 61, 677–686. [Google Scholar]
- Park, Y.; Choi, H.; Cho, S.; Kim, Y.G. Security Analysis of Smart Speaker: Security Attacks and Mitigation. CMC Comput. Mater. Contin. 2019, 61, 1075–1090. [Google Scholar] [CrossRef]
- Albanese, G.; Calbimonte, J.-P.; Schumacher, M.; Calvaresi, D. Dynamic consent management for clinical trials via private blockchain technology. J. Ambient Intell. Humaniz. Comput. 2020, 11, 1–18. [Google Scholar] [CrossRef]
- Benchoufi, M.; Porcher, R.; Ravaud, P. Blockchain protocols in clinical trials: Transparency and traceability of consent. F1000Research 2017, 6, 1–66. [Google Scholar] [CrossRef]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. Medrec: Using blockchain for medical data access and permission management. In Proceedings of the 2016 2nd International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; pp. 25–30. [Google Scholar]
- Fan, K.; Wang, S.; Ren, Y.; Li, H.; Yang, Y. Medblock: Efficient and secure medical data sharing via blockchain. J. Med. Syst. 2018, 42, 136. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Liu, M.; Yang, C.; Liu, Y.; Wang, R. A Blockchain-Based Authentication Protocol for WLAN Mesh Security Access. CMC Comput. Mater. Contin. 2019, 58, 45–59. [Google Scholar] [CrossRef]
- Bordel, B.; Alcarria, R.; Martin, D.; Sanchez-Picot, A. Trust Provision in the Internet of Things Using Transversal Blockchain Networks. Intell. Autom. Soft Comput. 2019, 25, 155–170. [Google Scholar] [CrossRef]
- Singh, S.; Sharma, P.K.; Yoon, B.; Shojafar, M.; Cho, G.H.; Ra, I.H. Convergence of blockchain and artificial intelligence in IoT network for the sustainable smart city. Sustain. Cities Soc. 2020, 63, 102364. [Google Scholar] [CrossRef]
- Yan, Y.; Dai, Y.; Zhou, Z.; Jiang, W.; Guo, S. Edge computing-based tasks offloading and block caching for mobile blockchain. Comput. Mater. Contin. 2020, 62, 905–915. [Google Scholar] [CrossRef]
- Nguyen, B.L.; Lydia, E.L.; Elhoseny, M.; Pustokhina, I.V.; Pustokhin, D.A.; Selim, M.M.; Nguyen, G.N.; Shankar, K. Privacy preserving blockchain technique to achieve secure and reliable sharing of IoT data. Comput. Mater. Contin. 2020, 65, 87–107. [Google Scholar] [CrossRef]
- Wang, Q.; Zhu, F.; Ji, S.; Ren, Y. Secure provenance of electronic records based on blockchain. Comput. Mater. Contin. 2020, 65, 1753–1769. [Google Scholar] [CrossRef]
- Cheng, J.; Li, J.; Xiong, N.; Chen, M.; Guo, H.; Yao, X. Lightweight mobile clients privacy protection using trusted execution environments for blockchain. Comput. Mater. Contin. 2020, 65, 2247–2262. [Google Scholar] [CrossRef]
- Ali, S.; Hafeez, Y.; Jhanjhi, N.Z.; Humayun, M.; Imran, M.; Nayyar, A.; Singh, S.; Ra, I.H. Towards Pattern-Based Change Verification Framework for Cloud-Enabled Healthcare Component-Based. IEEE Access 2020, 8, 148007–148020. [Google Scholar] [CrossRef]
- Singh, S.; Jeong, Y.S.; Park, J.H. A survey on cloud computing security: Issues, threats, and solutions. J. Netw. Comput. Appl. 2016, 75, 200–222. [Google Scholar] [CrossRef]
- Naresh, V.S.; Pericherla, S.S.; Sita, P.; Reddi, S. Internet of things in healthcare: Architecture, applications, challenges, and solutions. Comput. Syst. Sci. Eng. 2020, 35, 411–421. [Google Scholar] [CrossRef]
- Parvathavarthini, S.; Visalakshi, N.; Shanthi, S.; Mohan, J. An Improved Crow Search Based Intuitionistic Fuzzy Clustering Algorithm for Healthcare Applications. Intell. Autom. Soft Comput. 2020, 26, 253–260. [Google Scholar] [CrossRef]
- Bailey, B.W.; LeCheminant, G.; Hope, T.; Bell, M.; Tucker, L.A. A comparison of the agreement, internal consistency, and 2-day test stability of the InBody 720, GE iDXA, and BOD POD (R) gold standard for assessing body composition. Meas. Phys. Educ. Exerc. Sci. 2018, 22, 231–238. [Google Scholar] [CrossRef]
- Androulaki, E.; Barger, A.; Bortnikov, V.; Cachin, C.; Christidis, K.; De Caro, A.; Muralidharan, S. Hyperledger fabric: A distributed operating system for permissioned blockchains. In Proceedings of the Thirteenth EuroSys Conference, Porto, Portugal, 23–26 April 2018; pp. 1–15. [Google Scholar]
- Sharma, G.; Srivastava, G.; Mago, V. A framework for automatic categorization of social data into medical domains. IEEE Trans. Comput. Soc. Syst. 2020, 7, 129–140. [Google Scholar] [CrossRef]
- Manevich, Y.; Barger, A.; Tock, Y. Endorsement in Hyperledger Fabric via service discovery. Ibm J. Res. Dev. 2019, 63, 1–9. [Google Scholar] [CrossRef]
- Lahbib, A.; Toumi, K.; Laouiti, A.; Laube, A.; Martin, S. Blockchain based trust management mechanism for IoT. In Proceedings of the 2019 IEEE Wireless Communications and Networking Conference, Marrakesh, Morocco, 15–18 April 2019; pp. 1–8. [Google Scholar]
- Dubovitskaya, A.; Xu, Z.; Ryu, S.; Schumacher, M.; Wang, F. Secure and trustable electronic medical records sharing using blockchain. Amia Annu. Symp. Proc. 2017, 2017, 650. [Google Scholar] [PubMed]
- Liang, X.; Zhao, J.; Shetty, S.; Liu, J.; Li, D. Integrating blockchain for data sharing and collaboration in mobile healthcare applications. In Proceedings of the 2017 IEEE 28th Annual International Symposium on PIMRC, Montreal, QC, Canada, 8–13 October 2017; pp. 1–5. [Google Scholar]
- Xia, Q.I.; Sifah, E.B.; Asamoah, K.O.; Gao, J.; Du, X.; Guizani, M. MeDShare: Trust-less medical data sharing among cloud service providers via blockchain. IEEE Access 2017, 5, 14757–14767. [Google Scholar] [CrossRef]
- Griggs, K.N.; Ossipova, O.; Kohlios, C.P.; Baccarini, A.N.; Howson, E.A.; Hayajneh, T. Healthcare blockchain system using smart contracts for secure automated remote patient monitoring. J. Med. Syst. 2018, 42, 130. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Zhang, J.; Ma, J.; Yang, C.; Yao, X. BMPLS: Blockchain-based multi-level privacy-preserving location sharing scheme for telecare medical information systems. J. Med. Syst. 2018, 42, 147. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Alam, M.A.; Jameel, R.; Mourya, A.K.; Chang, V. A proposed solution and future direction for blockchain-based heterogeneous medicare data in cloud environment. J. Med. Syst. 2018, 42, 156. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhu, L.; Shen, M.; Gao, F.; Tao, X.; Liu, S. Blockchain-based data preservation system for medical data. J. Med. Syst. 2018, 42, 141. [Google Scholar] [CrossRef]
- Uddin, M.A.; Stranieri, A.; Gondal, I.; Balasubramanian, V. A patient agent to manage Blockchains for remote patient monitoring. Stud. Health Technol. Inform. 2018, 254, 105–115. [Google Scholar]
- Zhang, A.; Lin, X. Towards secure and privacy-preserving data sharing in e-health systems via consortium blockchain. J. Med. Syst. 2018, 42, 140. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Wang, L.; Sun, Y. Mistore: A blockchain-based medical insurance storage system. J. Med. Syst. 2018, 42, 149. [Google Scholar] [CrossRef] [PubMed]
- Al Omar, A.; Bhuiyan, M.Z.A.; Basu, A.; Kiyomoto, S.; Rahman, M.S. Privacy-friendly platform for healthcare data in cloud based on blockchain environment. Future Gener. Comp Syst. 2019, 95, 511–521. [Google Scholar] [CrossRef]
- Casado-Vara, R.; Corchado, J. Distributed e-health wide-world accounting ledger via blockchain. J. Intell. Fuzzy Syst. 2019, 36, 2381–2386. [Google Scholar] [CrossRef]
- Dwivedi, A.D.; Srivastava, G.; Dhar, S.; Singh, R. A decentralized privacy-preserving healthcare blockchain for IoT. Sensors 2019, 19, 326. [Google Scholar] [CrossRef]
- Hyla, T.; Peja’s, J. eHealth integrity model based on permissioned blockchain. Future Internet 2019, 11, 76. [Google Scholar] [CrossRef]
- Islam, N.; Faheem, Y.; Din, I.U.; Talha, M.; Guizani, M.; Khalil, M. A blockchain-based fog computing framework for activity recognition as an application toe-Healthcare services. Future Gener. Comput. Syst. 2019, 100, 569–578. [Google Scholar] [CrossRef]
- Kuo, T.T.; Gabriel, R.A.; Ohno-Machado, L. Fair compute loads enabled by blockchain: Sharing models by alternating client and server roles. J. Am. Med. Inform. Assoc. 2019, 26, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Huang, X.; Li, C.; Yu, R.; Shu, L. EdgeCare: Leveraging edge computing for collaborative data management in mobile healthcare systems. IEEE Access 2019, 7, 22011–22025. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Pathirana, P.N.; Ding, M.; Seneviratne, A. Blockchain for secure EHRs sharing of mobile cloud based e-health systems. IEEE Access 2019, 7, 66792–66806. [Google Scholar] [CrossRef]
- Rahmadika, S.; Rhee, K.H. Toward privacy-preserving shared storage in untrusted blockchain P2P networks. Wirel. Commun. Mob. Comput. 2019, 2019, 1–13. [Google Scholar] [CrossRef]
- Shen, B.; Guo, J.; Yang, Y. MedChain: Efficient healthcare data sharing via Blockchain. Appl. Sci. 2019, 9, 1207. [Google Scholar] [CrossRef]
- Silva, C.A.; Aquino, G.S.; Melo, S.R.; Egídio, D.J. A fog computing-based architecture for medical records management. Wirel. Commun. Mob. Comput. 2019, 2019, 1–16. [Google Scholar] [CrossRef]
- Tian, H.; He, J.; Ding, Y. Medical data management on blockchain with privacy. J. Med. Syst. 2019, 43, 26. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.R.; Bhattacharya, S.; Butte, A.J. Prototype of running clinical trials in an untrustworthy environment using blockchain. Nature Commun. 2019, 10, 917. [Google Scholar] [CrossRef]
- Yang, J.; Onik, M.M.H.; Lee, N.Y.; Ahmed, M.; Kim, C.S. Proof-of-familiarity:a privacy-preserved blockchain scheme for collaborative medical decision-making. Appl. Sci. 2019, 9, 1370. [Google Scholar] [CrossRef]
- Tanwar, S.; Parekh, K.; Evans, R. Blockchain-based electronic healthcare record system for healthcare 4.0 applications. J. Inf. Secur. Appl. 2020, 50, 102407. [Google Scholar] [CrossRef]
- Khatoon, A. A blockchain-based smart contract system for healthcare management. Electronics 2020, 9, 94. [Google Scholar] [CrossRef]
- Abou-Nassar, E.M.; Iliyasu, A.M.; El-Kafrawy, P.M.; Song, O.Y.; Bashir, A.K.; Abd El-Latif, A.A. DITrust chain: Towards blockchain-based trust models for sustainable healthcare IoT systems. IEEE Access 2020, 8, 111223–111238. [Google Scholar] [CrossRef]
- Sharma, A.; Tomar, R.; Chilamkurti, N.; Kim, B.G. Blockchain based smart contracts for internet of medical things in e-healthcare. Electronics 2020, 9, 1609. [Google Scholar] [CrossRef]
- Kim, S.K.; Huh, J.H. Artificial Neural Network Blockchain Techniques for Healthcare System: Focusing on the Personal Health Records. Electronics 2020, 9, 763. [Google Scholar] [CrossRef]
- Dor-Haim, H.; Katzburg, S.; Leibowitz, D. A novel digital platform for a monitored home-based cardiac rehabilitation program. Jove J. Vis. Exp. 2019, 146, e59019. [Google Scholar] [CrossRef]
- Subramaniyaswamy, V.; Manogaran, G.; Logesh, R.; Vijayakumar, V.; Chilamkurti, N.; Malathi, D.; Senthilselvan, N. An ontology-driven personalized food recommendation in IoT-based healthcare system. J. Supercomput. 2019, 75, 3184–3216. [Google Scholar] [CrossRef]
- Holder, C.J.; Ricketts, S.; Obara, B. Convolutional networks for appearance-based recommendation and visualisation of mascara products. Mach. Vis. Appl. 2020, 31, 1–13. [Google Scholar] [CrossRef]
- Narayanasamy, S.; Markina, V.; Thorogood, A.; Blazkova, A.; Shabani, M.; Knoppers, B.M.; Prainsack, B.; Koesters, R. Genomic sequencing capacity, data retention, and personal access to raw data in Europe. Front. Genet. 2020, 11, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Bild, R.; Bialke, M.; Buckow, K.; Ganslandt, T.; Ihrig, K.; Jahns, R.; Merzweiler, A.; Roschka, S.; Schreiweis, B.; Stäubert, S.; et al. Towards a comprehensive and interoperable representation of consent-based data usage permissions in the German medical informatics initiative. BMC Med. Inform. Decis. Mak. 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Park, D.W.; Jeong, H.H.; Jeong, M.J.; Ryoo, H.S. Improving legislation on the use of healthcare data for research purposes. Korean Soc. Law Med. 2016, 17, 315–346. [Google Scholar]




| Function Classification | Function Contents |
|---|---|
| Data Provider’s App | Basic account functions (log in, create account, etc.) My examination history ledger My examination data (raw data and statistical data) Dynamic consent rule settings |
| Data Utilizer’s App | Basic account functions Input health examination results data function Data provider list management Data providers’ examination history management ledger Data providers’ examination data sharing usage history management ledger Request for data provider data function Data provider data request management function (applicable and non-applicable) |
| Blockchain System | Health examination data hash storage function Sync smart contract with real-time dynamic consent function settings Smart contract and blockchain ledger |
| Blockchain Admin Web | Channel management Peer node management User account management Blockchain data sharing history ledger management |
| Classification | Contents |
|---|---|
| Basic | Serial number, Sex, Age, Smoking Status, Drinking Status, Height, Weight, Waist |
| Out-of-hospital-level tests | Body Water, Protein, Minerals, Body Fat Amount, Weight, Bones and Muscle Amount, BMI, Body Fat Ratio, InBody Score, Abdomen Fat Ratio, Internal Organ Fat Level, Fat-free Mass, Basal Metabolism, Obesity Index, Recommended Calorie Amount, Body Parts’ Muscle Analysis (Right Arm, Left Arm, Body, Right Leg, Left Leg), Body Parts’ Fat Analysis (Right Arm, Left Arm, Body, Right Leg, Left Leg), Body Parts’ Body Water Analysis (Right Arm, Left Arm, Body, Right Leg, Left Leg), Body Parts’ Cell Water Analysis (Right Arm, Left Arm, Body, Right Leg, Left Leg), Body Parts’ Cell-free Water Analysis (Right Arm, Left Arm, Body, Right Leg, Left Leg), Cell-free Water Ratio, Phase Angle |
| Hospital-level tests | Cholesterol, Triglycerides, HDL Cholesterol, LDL Cholesterol, Diastatic Hemoglobin, Diastatic Hemoglobin Before Meal, Protein in Urine, Serum Creatinine, AST, ALT, Gamma GTP, Serial Number, Examination Date, Examined Institution, Sight (Left, Right), Blood Pressure (Systolic, Diastolic) |
| Reference | Main Idea | Target Data | Target Participant | BlockchainPlatform | Consensus Mechanism | System Architecture | Not Addressed |
|---|---|---|---|---|---|---|---|
| DynamiChain | Maximize the autonomy via dynamic consent and Maximize the flexibility to expand participants | Health examination data | Patients, Hospitals, Service providers | Hyperledger | Chaincode based on dynamic consent | Proposed, Implemented | - |
| Azaria, A. et al. (2016) [21] | Innovative approach for handling EMR data | EMR data | Patients, Hospitals, Service providers | Ethereum | Smart contract, PoW | Proposed | Detailed data description, Healthy participants, Dynamic consent, Dapp |
| Dubovitskaya, A. et al. (2017) [39] | Present a framework on managing and sharing EMR data for cancer patient care | Radiation oncology EMR data | Cancer patients Hospitals | Hyperledger | Consensus | Proposed, implemented | Detailed data description, Healthy participants, Dynamic consent, Dapp |
| Liang, X. et al. (2017) [40] | Design a mobile healthcare system for personal health data collection, sharing | Personal health data | Patients, Hospitals, Service providers, Insurance company | Hyperledger | Not specified | Proposed, implemented, Evaluated | Service providers, Dynamic consent |
| Xia, Q. et al. (2017) [41] | Provide trustworthy data sharing model between cloud service providers in a trust-less environment | EMR data | Cloud service providers | Permissioned blockchain | Smart contract | Proposed, implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, Dapp |
| Fan, K. et al. (2018) [22] | Resolve the problem of large-scale EMR data management and sharing in an EMR system and allows the efficient EMRs access and retrieval | EMR data | Patients, Hospitals | Consortium | consensus | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, Dapp |
| Griggs, K.N. et al. (2018) [42] | Resolve many security vulnerabilities associated with remote patient monitoring and automate the delivery of notifications to all involved parties | Protected health data | Remote patients, Hospital | Ethereum, Private | Smart contract, Consensus | Proposed | Service providers, Dynamic consent |
| Ji, Y. et al. (2018) [43] | Investigates the location sharing based on blockchains for telecare medical information systems | Medical data | Patients, Hospitals | Not specified | Consensus | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, Dapp |
| Kaur, H. et al. (2018) [44] | Store and manage huge healthcare data in cloud environment | Heterogeneous medical data | Patients, Hospitals, Drug manufacturer, Insurance company | Not specified | Not specified | proposed | Detailed data description, Healthy participants, Dynamic consent, Dapp |
| Li, H. et al. (2018) [45] | Present a novel data preservation system that provides a reliable storage solution of stored data while preserving users’ privacy | Medical data | Not specified | Ethereum | Not specified | Proposed, Implemented, Evaluated | Detailed data description, Participants, Service providers, Dynamic consent, Dapp |
| Uddin, M.A. et al. (2018) [46] | Presents an architecture that involves a patient agent coordinating the insertion of continuous data streams into blockchain to form an EHREHR data | EHR data | Patients, Hospitals | Bitcoin, Ethereum | Miner | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, DApp |
| Zhang, A. et al. (2018) [47] | Proposes a blockchain-based secure and privacy-preserving personal health data sharing scheme for diagnosis improvements in e-Health systems | Personal health data | Patients, Hospitals | Consortium, Private | Consensus, PoC | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, DApp |
| Zhou, L. et al. (2018) [48] | Propose a blockchain-based threshold medical insurance storage system | Insurance data | Patients, Hospitals, Insurance company | Ethereum | Consensus, PoW | Proposed, Implemented, Evaluated | Healthy participants, Dynamic consent, DApp |
| Al Omar, A. et al. (2019) [49] | Present privacy-preserving platform in cloud using Elliptic curve cryptography and MediBChain protocol | Healthcare data | Patients, Hospitals | Permissioned blockchain | Smart contract | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers Dynamic consent, DApp |
| Casado-Vera, R. et al. (2019) [50] | Create an e-health system based on wireless sensor networks | Medical data | Patients, Hospitals | Ethereum | Not specified | Proposed | Detailed data description, Healthy participants, Service providers Dynamic consent, DApp Consensus |
| Dwivedi, A.D. et al. (2019) [51] | Provide secure management and analysis of healthcare big data form IoT devices | IoT health data | Patients, Hospitals, Service providers | Bitcoin | Smart contracts | Proposed | Dynamic consent, DApp |
| Hyla, T. et al. (2019) [52] | Use design-science methodology to create an integrity-protection service model based on blockchain technolher | EHR data | Patients, Hospitals | Permissioned blockchain | Consensus | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, DApp |
| Islam, N. et al. (2019) [53] | Propose an activity monitoring and recognition framework to improve the activity classification accuracy in videos supporting cloud computing-based blockchain architecture | IoT video data | Patients, Hospitals, Service providers | Not specified | Not specified | Proposed, Implemented, Evaluated | Healthy participants, Dynamic consent, DApp |
| Kuo, T.T. et al. (2019) [54] | Develop a general model sharing framework to preserve predictive correctness, mitigate the risks of a centralized architecture | Healthcare data, genomic data | Patients, Hospitals | Permissioned blockchain | Consensus | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, DApp |
| Li, X. et al. (2019) [55] | Present a secure and efficient data management system for mobile healthcare system based on edge computing | EMR data, Mobile health data | Patients, Hospitals, Service providers | Permissioned blockchain | Consensus | Proposed, Implemented, Evaluated | Dynamic consent, DApp |
| Nguyen, D.C. et al. (2019) [56] | Propose a novel EHRs sharing framework that combines blockchain and the decentralized interplanetary file system on a mobile cloud platform | EHR data | Patients, Hospitals | Ethereum | Consensus | Proposed, Implemented, Evaluated | Healthy participants, Dynamic consent |
| Rahmadika, S. et al. (2019) [57] | Present a model for shared storage on a blockchain network that allows the authorized parties to access the data on storage without having to reveal their identity | Personal Health Data | Patients, Hospitals, Service providers | Not specified | Not specified | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Dynamic consent, DApp |
| Shen, B. et al. (2019) [58] | Propose an efficient data-sharing scheme which combines blockchain, digest chain, and structured P2P network techniques | EHR | Patients, Hospitals, Insurance company, Service providers | Permissioned blockchain | BFT-SMaRt [57] | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Dynamic consent, DApp |
| Silva, C.A. et al. (2019) [59] | Shows a software architecture based on Fog Computing and designed to facilitate the management of medical records | Medical data | Patients, Hospitals | Ethereum | Not specified | Proposed, Implemented, Evaluated | Healthy participants, Service providers, Dynamic consent |
| Tian, H. et al. (2019) [60] | Establish a shared key that could be reconstructed by the legitimate parties before the process of diagnosis and treatment begins | Medical data | Patients, Hospitals, Pharmacy, Lawyers | Hyperledger | Consensus | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, DApp |
| Wong, D.R. et al. (2019) [61] | Propose a blockchain-based system to make data collected in the clinical trial process immutable, traceable, and potentially more trustworthy | Clinical trial data | Patients, Hospitals, | Not specified | Not specified | Proposed, Implemented, Evaluated | Healthy participants, Service providers, Dynamic consent, DApp |
| Yang, J. et al. (2019) [62] | Utilizes the transparency, security, and efficiency of blockchain technology to establish a collaborative medical decision-making scheme | Personal health data | Patients, Hospitals, Insurance company | Consortium | Proof of familiarity | Proposed, Implemented, Evaluated | Detailed data description, Dynamic consent, DApp |
| Zheng, X. et al. (2019) [5] | Integrate IOTA Tangle with IoT to develop a health data sharing system, which could support secure, fee-less, tamper-resist, high-scalable, and granular-controllable health data exchange | IoT health data | Patients, Hospitals, Service providers | IOTA Tangle | Consensus | Proposed, Implemented, Evaluated | Detailed data description, Dynamic consent, DApp |
| Tanwar, S. et al. (2020) [63] | Proposes an Access Control Policy Algorithm for improving data accessibility between healthcare providers, assisting in the simulation of environments to implement the Hyperledger-based EHR sharing system | EHR | Patients, Hospitals | Hyperledger | Consensus | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent, DApp |
| Khatoon, A. (2020) [64] | Proposes multiple workflows involved in the healthcare ecosystem using blockchain technology for better large amount of data management | Medical data | Patients, Hospitals, Pharmacy, Insurance company | Ethereum | Smart contract | Proposed, Implemented, Evaluated | Healthy participants, Dynamic consent, |
| Abou-Nassar, E.M. et al. (2020) [65] | Propose blockchain decentralized interoperable trust framework for IoT zones where a smart contract guarantees authentication of budgets and indirect Trust Inference System Reduces semantic gaps and enhances trustworthy factor (TF) estimation via the network nodes and edges | IoT health data | Patients, Hospitals, Service providers | Ethereum | Smart contract | Proposed | Healthy participants, Dynamic consent, DApp |
| Sharma, A. et al. (2020) [66] | Analyses the dimensions that decentralization and the use of smart contracts will take the IoMT in e-healthcare, proposes a novel architecture, and outlines the advantages, challenges, and future trends related to the integration of all three | IoT health data | Patients, Hospitals, | Not specified | Smart contracts | Proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers Dynamic consent, DApp |
| Kim, S.K. et al. (2020) [67] | Use artificial intelligence blockchain algorithms to ensure safe verification of medical institution PHR data and accurate verification of medical data as existing vulnerabilities | EMR, Personal health data | Patients, Hospitals, | Ethereum | Hyper POR | proposed, Implemented, Evaluated | Detailed data description, Healthy participants, Service providers, Dynamic consent |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, T.M.; Lee, S.-J.; Chang, D.-J.; Koo, J.; Kim, T.; Yoon, K.-H.; Choi, I.-Y. DynamiChain: Development of Medical Blockchain Ecosystem Based on Dynamic Consent System. Appl. Sci. 2021, 11, 1612. https://doi.org/10.3390/app11041612
Kim TM, Lee S-J, Chang D-J, Koo J, Kim T, Yoon K-H, Choi I-Y. DynamiChain: Development of Medical Blockchain Ecosystem Based on Dynamic Consent System. Applied Sciences. 2021; 11(4):1612. https://doi.org/10.3390/app11041612
Chicago/Turabian StyleKim, Tong Min, Seo-Joon Lee, Dong-Jin Chang, Jawook Koo, Taenam Kim, Kun-Ho Yoon, and In-Young Choi. 2021. "DynamiChain: Development of Medical Blockchain Ecosystem Based on Dynamic Consent System" Applied Sciences 11, no. 4: 1612. https://doi.org/10.3390/app11041612
APA StyleKim, T. M., Lee, S.-J., Chang, D.-J., Koo, J., Kim, T., Yoon, K.-H., & Choi, I.-Y. (2021). DynamiChain: Development of Medical Blockchain Ecosystem Based on Dynamic Consent System. Applied Sciences, 11(4), 1612. https://doi.org/10.3390/app11041612






