Partial Threading of Pedicle Screws in a Standard Construct Increases Fatigue Life: A Biomechanical Analysis
Abstract
1. Introduction
2. Materials and Methods
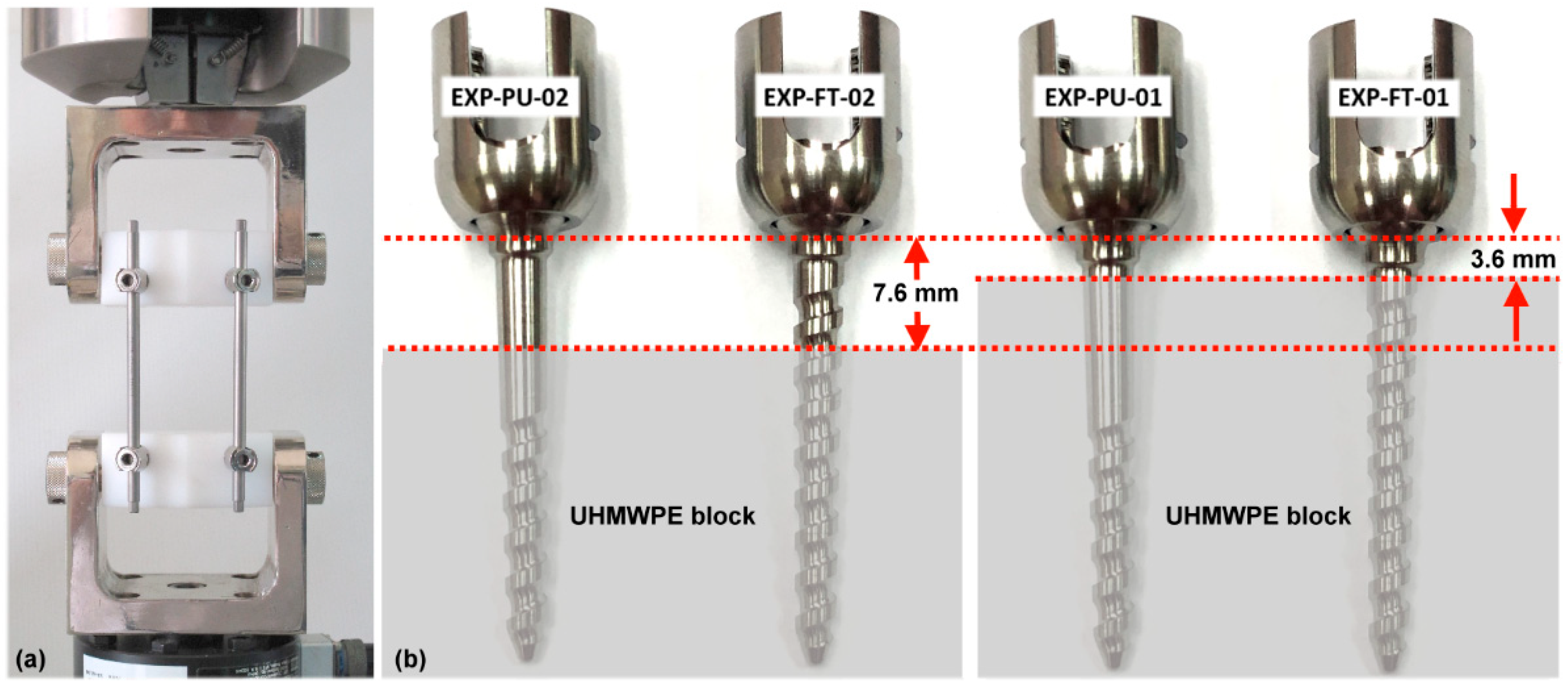
2.1. Mechanical Fatigue Testing
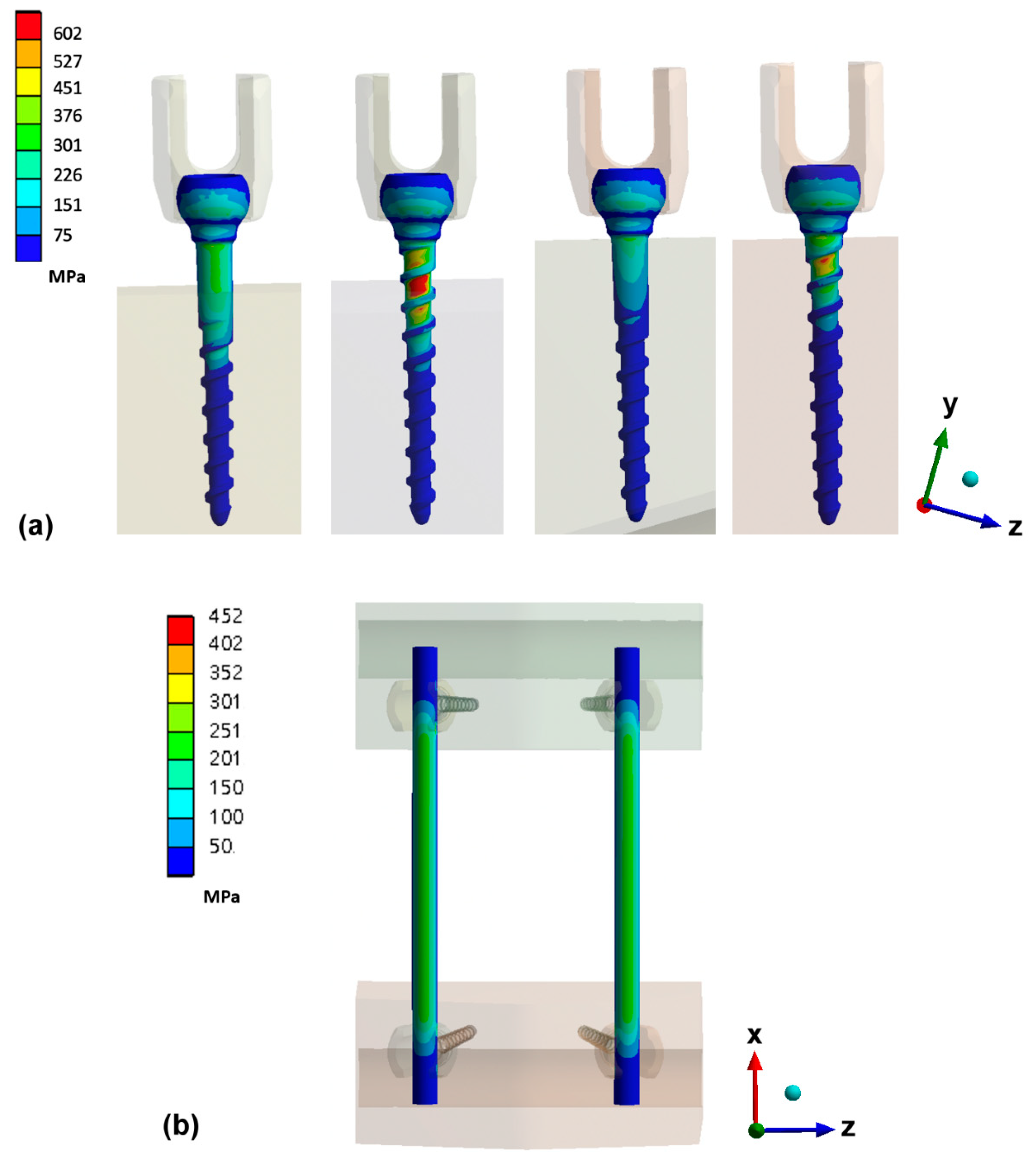
2.2. Finite Element Models
3. Results
3.1. Dynamic Compression Bending Test
3.2. Maximum Von Mises Stress on Pedicle Screw and Rod
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dvorak, M.F.; Pitzen, T.; Zhu, Q.; Gordon, J.D.; Fisher, C.G.; Oxland, T.R. Anterior cervicalplate fixation: A biomechanical study to evaluate the effects of plate design, endplate preparation, and bone mineral density. Spine 2005, 30, 294–301. [Google Scholar] [CrossRef]
- Ramaswamy, R.; Evans, S.; Kosashvili, Y. Holding power of variable pitch screws inosteoporotic, osteopenic and normal bone: Are all screws created equal? Injury 2010, 41, 179–183. [Google Scholar] [CrossRef]
- Halvorson, T.L.; Kelley, L.A.; Thomas, K.A.; Whitecloud, T.S., III; Cook, S.D. Effects of bone mineral density on pedicle screw fixation. Spine 1994, 19, 2415–2420. [Google Scholar] [CrossRef]
- Lattig, F. Bone cement augmentation in the prevention of adjacent segment failure after multilevel adult deformity fusion. J. Spinal Disord. Tech. 2009, 22, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Par’e, P.E.; Chappuis, J.L.; Rampersaud, R.; Agarwala, A.O.; Perra, J.H.; Erkan, S.; Wu, C. Biomechanical evaluation of a novel fenestrated pedicle screw augmented with bone cement in osteoporotic spines. Spine 2011, 36, E1210–E1214. [Google Scholar] [CrossRef]
- Kayanja, M.; Evans, K.; Milks, R.; Lieberman, I.H. The mechanics of polymethyl-methacrylate augmentation. Clin. Orthop. Relat. Res. 2006, 443, 124–130. [Google Scholar] [CrossRef]
- Chen, L.-H.; Tai, C.-L.; Lai, P.-L.; Lee, D.-M.; Tsai, T.-T.; Fu, T.-S.; Niu, C.-C.; Chen, W.-J. Pullout strength for cannulated pedicle screws with bone cement augmentation in severely osteoporotic bone: Influences of radial hole and pilot hole tapping. Clin. Biomech. 2009, 24, 613–618. [Google Scholar] [CrossRef]
- Klingler, J.-H.; Scholz, C.; Kogias, E.; Sircar, R.; Krüger, M.T.; Volz, F.; Scheiwe, C.; Hubbe, U. Minimally Invasive Technique for PMMA Augmentation of Fenestrated Screws. Sci. World J. 2015, 2015, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.U.; Baldauf, J.; Marx, S.; Kirsch, M.; Schroeder, H.W.; Pillich, D.T. Cement leakage in pedicle screw augmentation: A pro-spective analysis of 98 patients and 474 augmented pedicle screws. J. Neurosurg. Spine 2016, 25, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.S.; Shepherd, D.E.; Hukins, D.W. The effect of screw insertion angle and thread type on the pullout strength of bone screws in normal and osteoporotic cancellous bone models. Med. Eng. Phys. 2010, 32, 822–828. [Google Scholar] [CrossRef] [PubMed]
- Zindrick, M.R.; Wiltse, L.L.; Widell, E.H.; Thomas, J.C.; Holland, W.R.; Field, B.T.; Spencer, C.W. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin. Orthop. Relat. Res. 1986, 203, 99–112. [Google Scholar] [CrossRef]
- Weinstein, J.N.; Rydevik, B.L.; Rauschning, W. Anatomic and technical considerations of pedicle screw fixation. Clin. Orthop. Relat. Res. 1992, 284, 34–46. [Google Scholar] [CrossRef]
- Krenn, M.H.; Piotrowski, W.P.; Penzkofer, R.; Augat, P. Influence of thread design on pedicle screwfixation: Laboratory investi-gation. J. Neurosurg. Spine 2008, 9, 90–95. [Google Scholar] [CrossRef]
- Varghese, V.; Krishnan, V.; Kumar, G.S. Comparison of pullout strength of pedicle screws following revision using larger di-ameter screws. Med. Eng. Phys. 2019, 74, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Tsuang, F.-Y.; Chen, C.-H.; Wu, L.-C.; Kuo, Y.-J.; Lin, S.-C.; Chiang, C.-J. Biomechanical arrangement of threaded and unthreaded portions providing holding power of transpedicular screw fixation. Clin. Biomech. 2016, 39, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.L.; Chen, C.H.; Tsuang, F.Y.; Chiang, C.J.; Wu, Y.; Kuo, Y.J. Incomplete insertion of pedicle screws in a standard construct re-duces the fatigue life: A biomechanical analysis. PLoS ONE 2019, 14, e0224699. [Google Scholar] [CrossRef] [PubMed]
- ASTM F1717-18. Standard Test Methods for Spinal Implant Constructs in a Vertebrectomy Model. ASTM Int West Con-Shohocken, PA [Internet], 2018; pp. 1–16. Available online: https://www.astm.org/Standards/F1717.htm (accessed on 11 March 2019).
- Galbusera, F.; Schmidt, H.; Wilke, H.-J. Lumbar interbody fusion: A parametric investigation of a novel cage design with and without posterior instrumentation. Eur. Spine J. 2011, 21, 455–462. [Google Scholar] [CrossRef][Green Version]
- Schmidt, H.; Heuer, F.; Wilke, H.-J. Which axial and bending stiffnesses of posterior implants are required to design a flexible lumbar stabilization system? J. Biomech. 2009, 42, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-S.; Chen, W.-J.; Cheng, C.-K.; Jao, S.-H.E.; Chueh, S.-C.; Wang, C.-C. Failure analysis of broken pedicle screws on spinal in-strumentation. Med. Eng. Phys. 2005, 27, 487–496. Available online: http://www.ncbi.nlm.nih.gov/pubmed/15990065 (accessed on 28 March 2019). [CrossRef]
- La Barbera, L.; Galbusera, F.; Wilke, H.-J.; Villa, T. Preclinical evaluation of posterior spine stabilization devices: Can we compare in vitro and in vivo loads on the instrumentation? Eur. Spine J. 2016, 26, 200–209. [Google Scholar] [CrossRef]
- La Barbera, L.; Galbusera, F.; Wilke, H.-J.; Villa, T. Preclinical evaluation of posterior spine stabilization devices: Can the current standards represent basic everyday life activities? Eur. Spine J. 2016, 25, 2909–2918. Available online: http://www.ncbi.nlm.nih.gov/pubmed/27236658 (accessed on 10 April 2019). [CrossRef] [PubMed]
- La Barbera, L.; Galbusera, F.; Villa, T.; Costa, F.; Wilke, H.-J. ASTM F1717 standard for the preclinical evaluation of posterior spi-nal fixators: Can we improve it? Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2014, 228, 1014–1026. Available online: http://www.ncbi.nlm.nih.gov/pubmed/25319550 (accessed on 16 March 2019). [CrossRef] [PubMed]
- Stanford, R.E.; Loefler, A.H.; Stanford, P.M.; Walsh, W.R. Multiaxial Pedicle Screw Designs: Static and Dynamic Mechanical Testing. Spine 2004, 29, 367–375. [Google Scholar] [CrossRef] [PubMed]


| Modulus (MPa) | ν | |
|---|---|---|
| Ultra-high molecular weight polyethylene (UHMWPE) blocks [16] | 1050 | 0.4 |
| Titanium rods [16] | 110,000 | 0.3 |
| Titanium pedicle screws [16] | 110,000 | 0.3 |
| Fully Threaded Polyaxial Screw (Head/Body) | Proximally Unthreaded Polyaxial Screw (Head/Body) | UHMWPE Block of FEM-FT-01 and FEM-PU-01 | UHMWPE Block of FEM-FT-02 and FEM-PU-02 | Rod | |
|---|---|---|---|---|---|
| Type of elements | 4-node tetrahedral | 8-node hexahedron | |||
| Number of elements | 8582/30,059 | 8582/27,855 | 61,059 | 55,832 | 72,471 |
| Number of nodes | 15,448/54,407 | 15,448/49,582 | 109,296 | 99,381 | 289,878 |
| Min. and Max. of Axial Force | 17–170 (N) | 19–190 (N) | 22–220 (N) | |||
|---|---|---|---|---|---|---|
| Group | No. of samples | Cycles | No. of samples | Cycles | No. of samples | cycles |
| EXP-FT-01 | 1 | Run-out | 4 | Run-out | 7 | 719,021 * |
| 2 | Run-out | 5 | Run-out | 8 | 791,733 * | |
| 3 | Run-out | 6 | Run-out | 9 | 736,885 * | |
| EXP-FT-02 | 10 | Run-out | 13 | 1,361,467 * | 16 | 18,209 * |
| 11 | Run-out | 14 | 971,656 * | 17 | 21,779 * | |
| 12 | Run-out | 15 | 1,017,237 * | 18 | 7562 * | |
| EXP-PU-01 | 19 | Run-out | 22 | Run-out | 25 | Run-out |
| 20 | Run-out | 23 | Run-out | 26 | Run-out | |
| 21 | Run-out | 24 | Run-out | 27 | Run-out | |
| EXP-PU-02 | 28 | Run-out | 31 | Run-out | 34 | 4,152,887 ** |
| 29 | Run-out | 32 | Run-out | 35 | 4,001,455 ** | |
| 30 | Run-out | 33 | Run-out | 36 | Run-out | |
| Axial Force (N) | 170 | 220 |
|---|---|---|
| Screw of FEM-FT-01 (MPa) | 677.23 | 875.23 |
| Screw of FEM-FT-02 (MPa) | 1070.91 | 1384.01 |
| Screw of FEM-PU-01 (MPa) | 385.89 | 498.71 |
| Screw of FEM-PU-02 (MPa) | 491.5 | 635.20 |
| Axial Force (N) | 170 | 220 |
|---|---|---|
| Rod of FEM-FT-01 (MPa) | 341.66 | 440.12 |
| Rod of FEM-FT-02 (MPa) | 369.67 | 475.36 |
| Rod of FEM-PU-01 (MPa) | 361.36 | 465.49 |
| Rod of FEM-PU-02 (MPa) | 362.24 | 468.78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsuang, F.-Y.; Chen, C.-H.; Wu, L.-C.; Kuo, Y.-J.; Hsieh, Y.-Y.; Chiang, C.-J. Partial Threading of Pedicle Screws in a Standard Construct Increases Fatigue Life: A Biomechanical Analysis. Appl. Sci. 2021, 11, 1503. https://doi.org/10.3390/app11041503
Tsuang F-Y, Chen C-H, Wu L-C, Kuo Y-J, Hsieh Y-Y, Chiang C-J. Partial Threading of Pedicle Screws in a Standard Construct Increases Fatigue Life: A Biomechanical Analysis. Applied Sciences. 2021; 11(4):1503. https://doi.org/10.3390/app11041503
Chicago/Turabian StyleTsuang, Fon-Yih, Chia-Hsien Chen, Lien-Chen Wu, Yi-Jie Kuo, Yueh-Ying Hsieh, and Chang-Jung Chiang. 2021. "Partial Threading of Pedicle Screws in a Standard Construct Increases Fatigue Life: A Biomechanical Analysis" Applied Sciences 11, no. 4: 1503. https://doi.org/10.3390/app11041503
APA StyleTsuang, F.-Y., Chen, C.-H., Wu, L.-C., Kuo, Y.-J., Hsieh, Y.-Y., & Chiang, C.-J. (2021). Partial Threading of Pedicle Screws in a Standard Construct Increases Fatigue Life: A Biomechanical Analysis. Applied Sciences, 11(4), 1503. https://doi.org/10.3390/app11041503





