1. Introduction
Complete rehabilitations of the edentulous jaws supported by implants have been a treatment option for a decade [
1]. During complete-mouth fixed rehabilitation using dental implants, an interim restoration can be fabricated with digital technology before implant placement [
2]. The careful adjustment of interim implant-supported fixed prostheses is essential to ensure overall success and patient satisfaction with the definitive restoration in terms of occlusion, function and aesthetics.
The interim fixed complete-arch implant-supported restoration provides information on occlusal vertical dimension (OVD), tooth shape and position for the definitive restoration [
3]. The two main approaches have been used to fabricate the interim restoration. The first is the recording of the position of the implants after their surgical placement and the fabrication of the interim fixed prosthesis by the dental technician, which is sometimes unsuccessful because of inaccuracy of the occlusal registration and impression thus requiring adjustments by the clinician [
4,
5]. The second approach is the chairside conversion of an existing removable complete prosthesis. Clinically converted prostheses are often made of not-reinforced acrylic resin and sometimes face difficulty to adapt to the modified alveolar ridge after extraction of the teeth [
6].
Despite the development of digital technologies in dentistry, which has led to greater predictability of clinical and laboratory procedures [
7], full-arch implant supported rehabilitation could present several issues when a fully digital workflow is to be used. In order to transfer information, such as preoperative OVD, between the preoperative situation to the postoperative one through a digital process, stable points of references are required. Due to the surgical treatment both the hard and soft tissue are going to remodel, resulting in dynamical changes through all the healing phases. Due to this process, a stable point of references for the digital process from the presurgical to the postsurgical situations are difficult to find. In fact, to provide a reliable maxilla–mandibular three-dimensional relationship the main problem to overcome is to transfer information between different stages of implant supported rehabilitation due to the lack of stable points of reference in the lower jaw. In fact, in the upper jaw the palatal rugae provide us with a stable anatomical structure over the different surgical and prosthodontic stages. In fact, they are a useful human identification marker for forensic purposes [
8]. Lanteri et al. demonstrated that not even palatal expansion in children could affect their stability [
8].
On the lower jaw no such anatomical structure exists, thus complicating the transfer of information that could be gathered preoperatively, i.e., tooth position, vertical dimension of occlusion and maxilla–mandibular relationship.
In recent years, some authors have addressed these problems [
9,
10], but several issues are still far from being solved. In 2019, Shao et al. [
11] proposed a digital technique to fabricate an interim fixed complete-arch restoration based on the exact occlusion relationship, tooth position and tooth contour of the original dentition. Despite its high quality, this procedure may be considered invasive and at a high biological and economic cost to the patients, due to the insertion of the mini-screw and the virtual surgical planning on cone-beam computed tomography (CBCT) images. In 2020, Espona et al. [
12] proposed a similar method using pins instead of a mini-screw, but without solving the previously cited invasive procedure [
12].
The purpose of the present clinical report is to describe a novel digital workflow based on the use of a digital index that allows a precise superimposition of the mandibular presurgical scan with the postoperative impression aiming at fabricating an interim fixed complete-arch restoration. The protocol entails recording the vertical dimension of the occlusion, occlusal plane and intermaxillary relationship in implant-supported complete rehabilitations before the surgical insertion of the fixtures. Successively, information is transferred to the impressions with the scan abutments to be able to produce accurate immediate provisional prosthetic rehabilitation.
2. Case Report
A 50-year-old man was referred to the Prosthodontic Department of the University of Turin (C.I.R. Dental School, Molinette, Italy) with a complaint of mobile teeth and poor masticatory function. The extraoral examination did not reveal any abnormalities (
Figure 1).
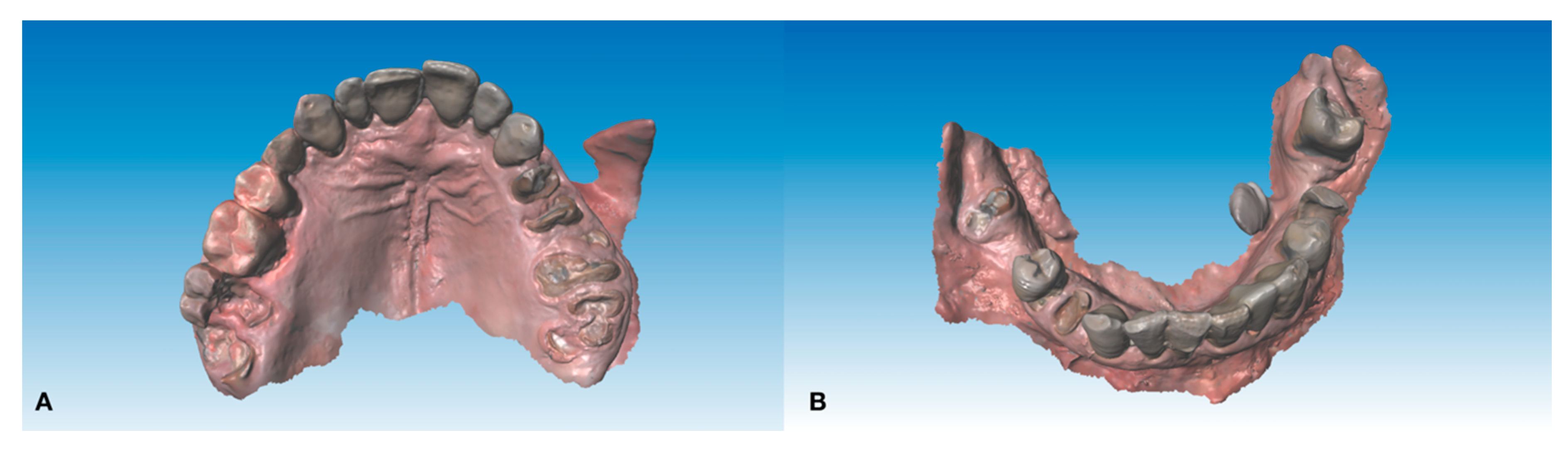
During the intraoral examination, multiple failing teeth were noted in both the maxillary and mandibular arches (
Figure 2).
The patient’s requests were the following: (1) to be rehabilitated, if possible, with fixed prostheses; (2) not to remain for a long time without the teeth and (3) to rehabilitate the upper and the lower arches at the same times due to his little time available for work reasons. After realizing plaster models and taking panoramic radiographs and a Tc cone beam, all the teeth, with the exception of the third lower molar left, were considered with an unfavorable prognoses. After discussing treatment options, the patient was found eligible for an implant-supported fixed restoration with immediate fixed restorations for function and aesthetics. The treatment plan was the following: extraction of all the hopeless teeth, implant insertion, post extractive implant insertion and immediate loading with milling poly methyl methacrylate (PMMA, VIPI BLOCK TRILUX®, VIPI Industria, Pirassununga, SP, Brazil) provisional screw-retained full-arch prosthesis in both the lower and upper jaw.
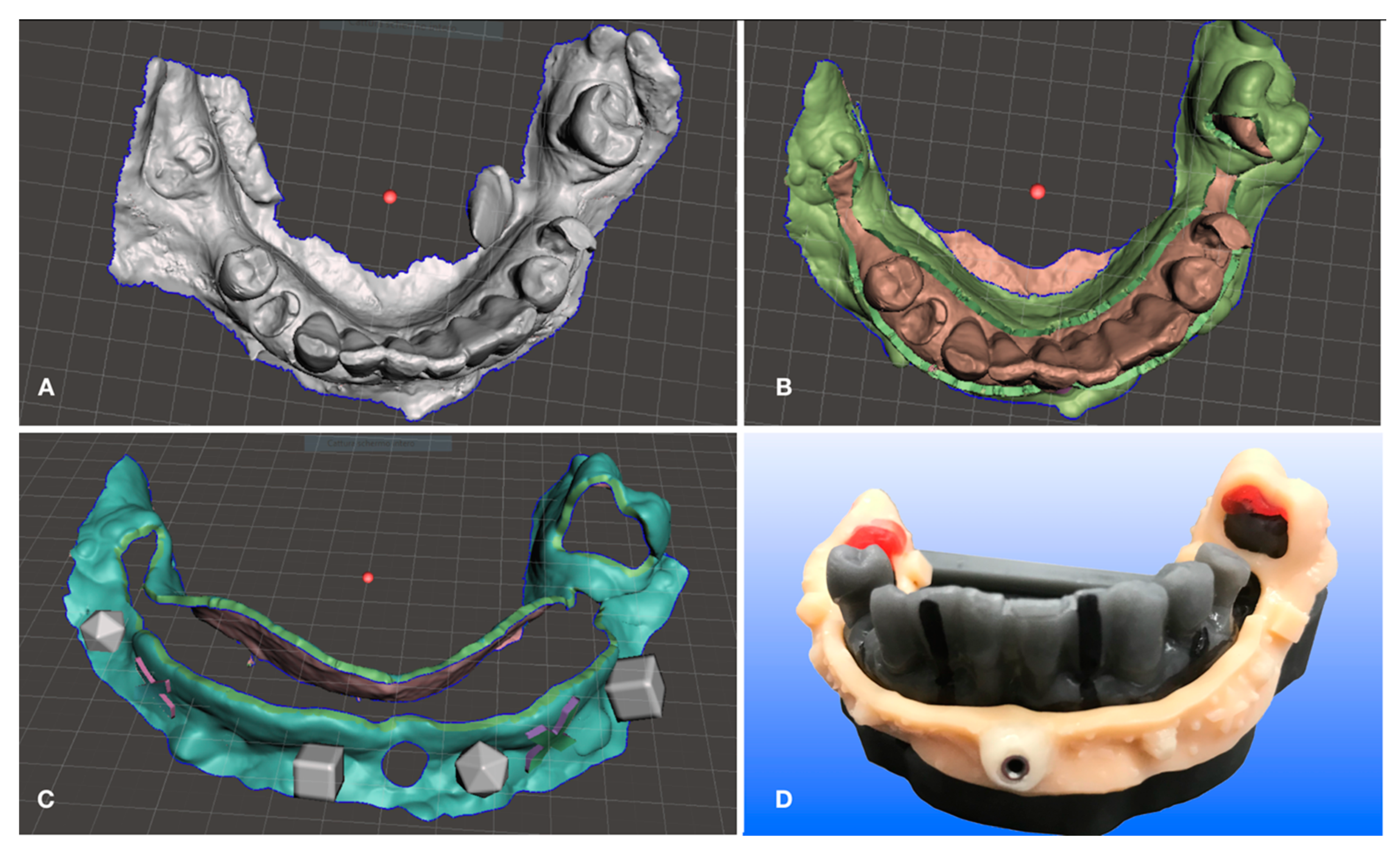
Digital lower preliminary impressions were taken (
Figure 3) during the first visit using an intraoral scanner (Medit i500, Seoul, South Corea) and imported into CAD software (DWOS, Dental Wings Inc., Montreal, Canada, software version 3.7.0.26).
This technique allows one to change the vertical dimension of occlusion before the actual surgery using for example direct composite restorations on the existing dentition if present to test the desired vertical dimension changes for any clinical purpose (gnathological issues, collapsed vertical dimension and so forth). It is also possible to immediately determine an increase or any other kind of change in the maxilla–mandibular relationship using conventional techniques before digitally recording it. An example is the digital recording of the maxilla–mandibular relationship in the centric relation using an occlusal wax. In the case of a reduced number of occluding teeth proper stabilization of the maxilla–mandibular position into the centric relation is required using conventional methods before digitally recording the determined position by scanning. The described case did not require any change to the existing occlusal determinants. The next step consisted of the design of the lower acrylic resin jig, which is the digital index, on the preliminary lower impression (
Figure 4) to superimpose the lower presurgical scan with the postsurgical impression.
This digital index (
Figure 5) was to be stabilized by three support points to ensure a reliable position in relation to the lower jaw. It is important to achieve stability of the index and to avoid undercuts that are retentive areas. After the 3D printing process was finished and supports were removed from the index, it was placed over the 3D-printed lower model (
Figure 4D) and the sleeve for the anterior median pin was placed in a position that could not impair the placement of the implants during surgery. This step did not require much programming and was performed by hand on the model since in this particular case and in any full arch mandibular restorative treatment it is preferable in accordance with plenty of scientific evidence [
13] to reduce the number of implants supporting full-arch rehabilitations, thus leaving plenty of space in the anterior mandibular alveolar bone to place our median pin in an area without damaging anatomical structures nor impairing potential implant sites. There is no issue regarding where to place the sleeve for the pin because the presurgical scan is taken immediately prior to surgery and the postoperative scan is taken just after surgery thus allowing one to place the pin in the exact same hole performed during the presurgical scan. There is no need to place in a particular place in the preoperative scan since the latter represents the reference for the second one, the only issue is to have the pin positioned in the same spot in both scans as explained above. Regarding the distal support points as one may notice in
Figure 4D it is possible to improve precision by relying the occlusal rests of the resin index with some Duralay (Reliance Dental, Worth, IL) to improve the fitting between the digital index and the occlusal rest seats of supporting posterior teeth.
If the existing dentition lacks one or more distal teeth that can be maintained even after surgery (second and third lower molars) to be used as support points, one or more anchor pins should be used instead to provide sufficient stability for the digital index. A median anterior anchor pin is always needed to provide anterior stability. Geometrical patterns are to be included in the digital index in order to provide sufficient reference points to superimpose preoperative and postoperative impressions. In this patient only the anterior pin was needed.
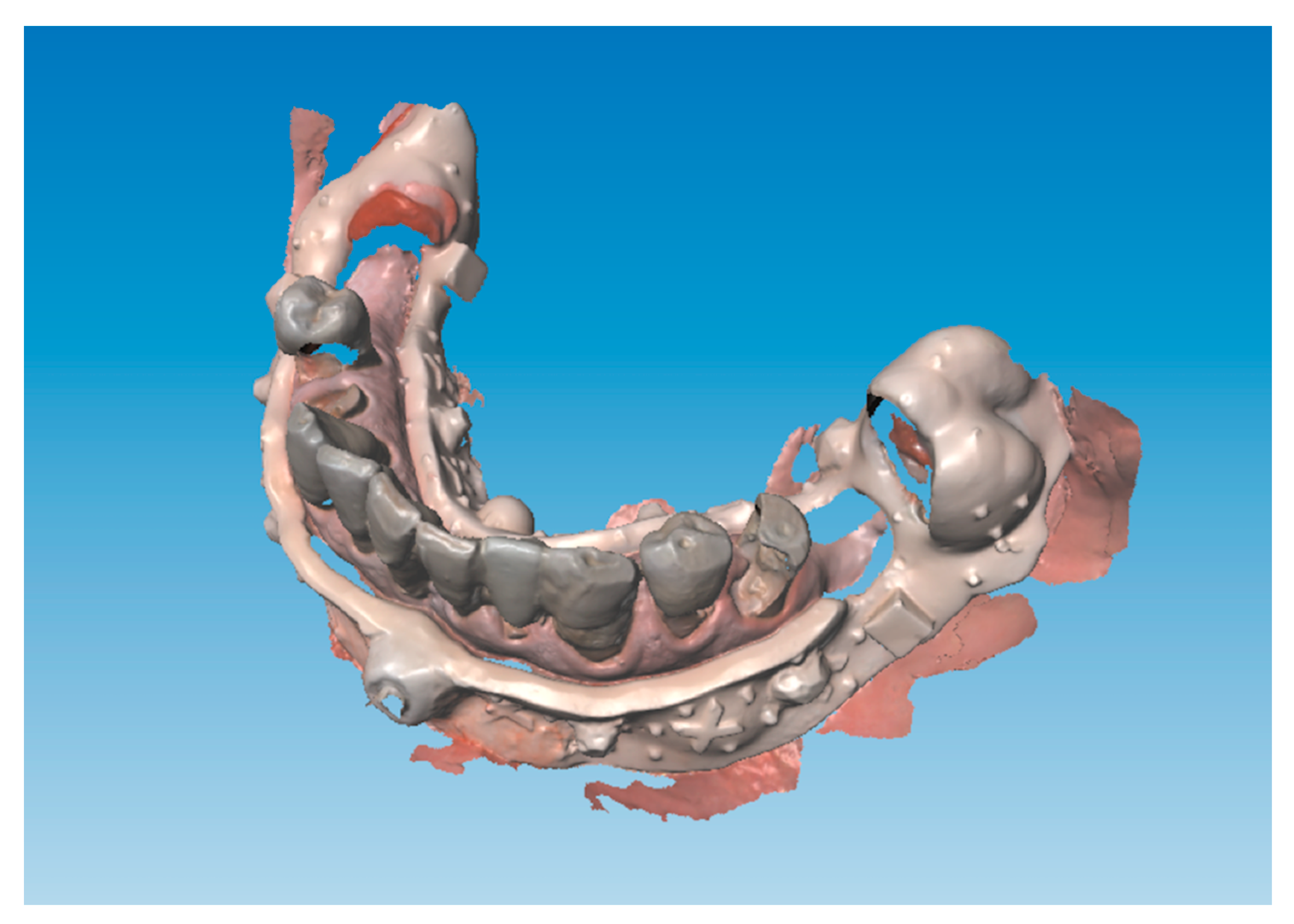
In the second appointment, immediately prior to surgical intervention and right after the local anesthesia, the digital index was placed in the lower jaw. Lower impression was taken (
Figure 5) and it was superimposed over the prior lower scan to keep the information regarding vertical dimension of occlusion in centric occlusion recorded on the existing dentition during the first appointment using an occlusal wax (Miltex beauty pink xhard, York, USA) to stabilize the maxilla–mandibular relationship (
Figure 6).
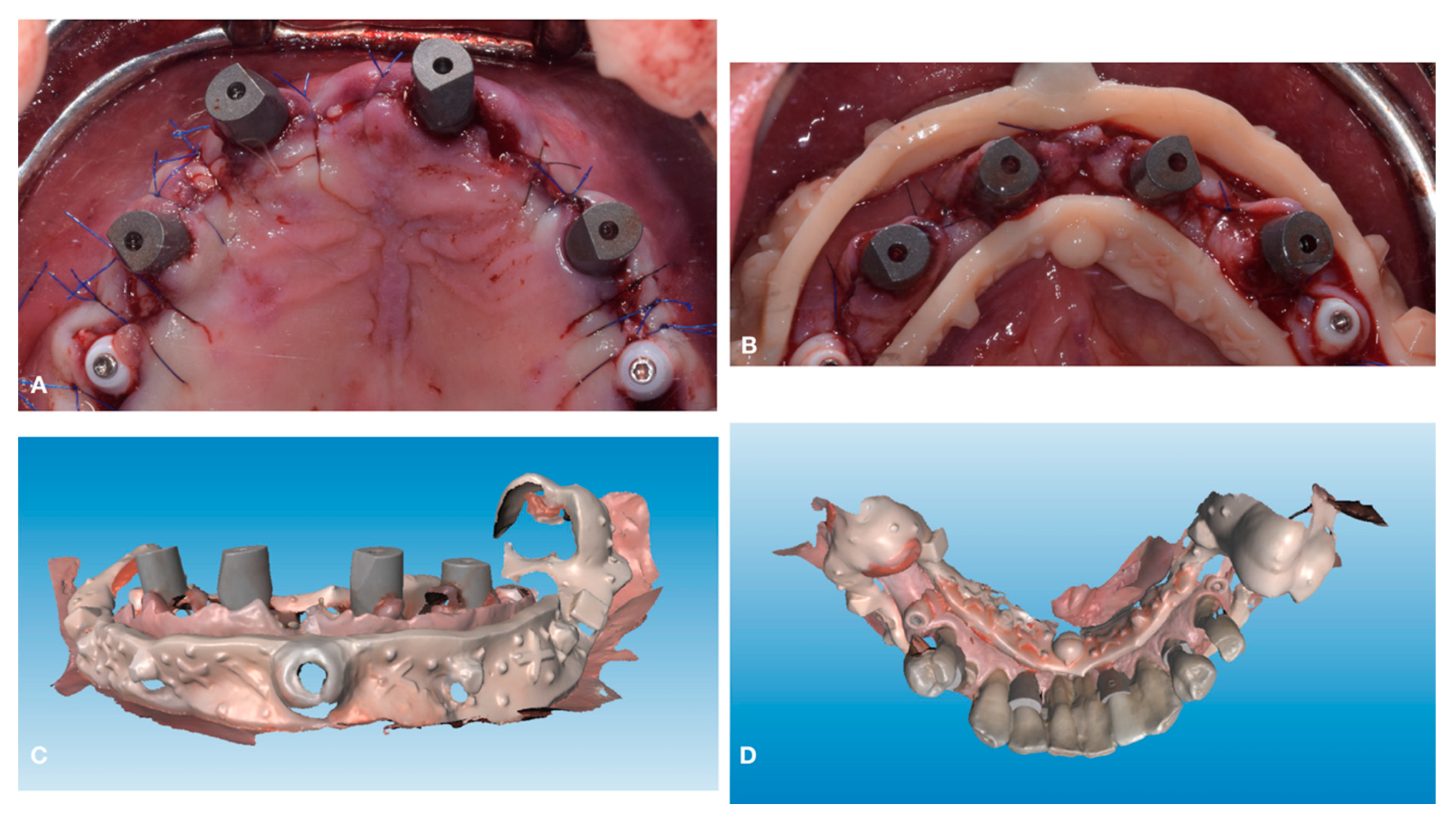
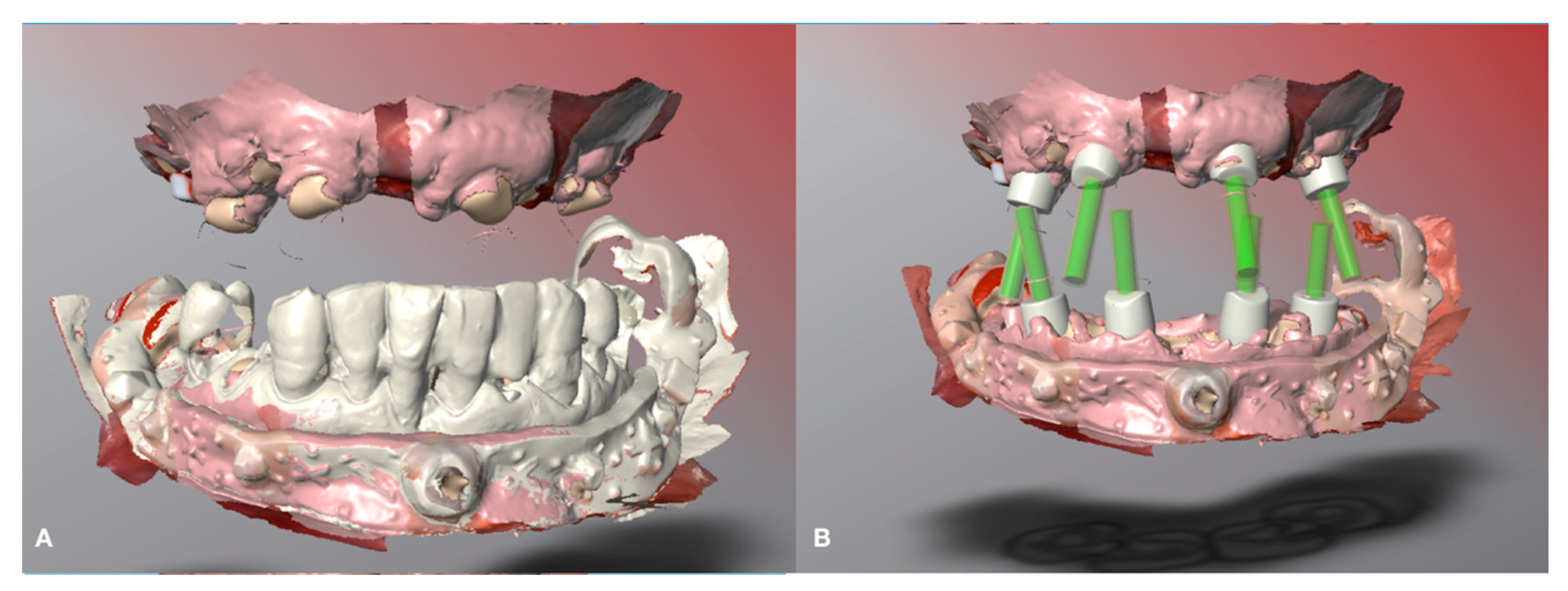
Extraction of all teeth was performed apart from the lower second molars that did not impair implant placement and served as distal support points for the digital index. Implants were inserted and scan abutments and the lower digital index was placed to take the postoperative digital impressions (
Figure 7).
Postoperative impressions have been superimposed over preoperative records thus obtaining implant position and all the information about the three-dimensional relation between the maxilla and the mandible and ultimately the vertical dimension of occlusion (
Figure 8).
Interim superior restoration was computer-aided designed using presurgical occlusal plane as a reference. Interim inferior restoration was designed using the superior virtual interim restoration as a reference (
Figure 9).
Interim restorations in PMMA (VIPI BLOCK TRILUX®, VIPI Industria, Pirassununga, SP, Brazil) were immediately produced and implants were immediately loaded (
Figure 10).
Immediate loading of interim fixed prosthesis was performed three hours after surgery (
Figure 11).
3. Discussion
The current clinical report describes a digital workflow in which the preoperative and postoperative scans were superimposed to transfer the occlusal relationship, aesthetics qualities and gingival tissue to build an immediate interim fixed full-arch prosthesis. They were digitally transferred from the original dentition to the virtual arches. The palatal rugae in the upper jaw and geometrical references on the lower digital index stabilized with an anchor pin anteriorly and with occlusal coverage of the second molar posteriorly provided us a stable point of reference to facilitate a high-quality, interim, fixed, full-arch prosthesis. Shao et al. [
11] proposed an alternative method but their approach is not appropriate for patients with a loss of OVD, inadequate occlusal scheme or abnormal occlusal or incisal planes. The presented technique in the presence of one of the previous conditions allows one to modify the patient’s occlusion and maxilla–mandibular relation, while performing at the same time any desired changes before the preoperative scans.
However, after the extraction of the teeth, finding markers to fuse digital scans can be difficult, because of the mobility and swelling of the soft tissue after surgery and local anesthesia. The superimposition of the palatal rugae in the maxilla makes it possible to achieve good-fit matching between scans obtaining reliable and stable landmarks in edentulous patients. In the lower jaw, the use of an acrylic resin digital index anchored to the mandible with occlusal rests over the second lower molar and anterior anchor pin permitted us to avoid the use of multiple miniscrews obtaining a less invasive and more economic procedure. Furthermore, the method proposed by Shao et al. [
11] involved the use of CBCT scans to develop a surgical template for prosthetically-guided implant placement, however this template could not be used in the inferior arch due to interference with the resin markers placed on mandibular mini screws that left no space for seating an implant template and forced them to insert them free-hand.
In recent years, the implant insertion with CAD/CAM surgical guides has become increasingly widespread. Although there have been high hopes regarding computer guided implant placement, only a few reports discovered the risk of errors and complications that dentists may face between the digital planning stage to implant surgery [
14]. Guided surgery is a cutting-edge technique that takes the 3-dimensional (3D) data collected from cone-beam computed tomography (CBCT), optical surface scanning and computer-aided design/computer-aided manufacturing tomography (CAD/CAM) technology for virtual implant planning and fabrication of surgical guides. The various types of surgical guides can be supported by teeth, mucosa or bone and additional support can be achieved using mini-implants, screws or pins [
15]. After the guide is fully seated, the planed drilling protocol can begin. The drilling protocol includes using the guide for a pilot drill nobly, a partially, or even a fully guided drilling protocol. The implant insertion can be performed either without the surgical guide or alternatively with the surgical guide for a fully guided approach. The proper case selection and accurate digital implant planning process throughout the digital workflow allow for accurate placement and execution. Guided implant surgery includes multiple additional steps after the initial prosthetic diagnosis, treatment planning and fabrication of surgical guide phases. Significant errors may occur at each of these various phases of care and can ultimately affect the final accuracy of the process with deviations from proper implant placement [
16]. Guided-implant surgery is believed to be accurate, precise and reliable when compared with free-handed implant surgery. However, there is a chance that deviation may occur between implant virtual planning and the implant real position due to the surgical learning curve and cumulative mistakes that may happen throughout the various steps of the digital workflow. Guided surgery is an advanced implant placement technique and an implant surgeon with a high level of surgical skills, including conventional implant placement, will be in a better position to manage any unforeseen complications [
17].
Despite that guided surgery provides an alternative to simplify and reduce the complexity and the number of appointments required for implant supported rehabilitations, it presents some downsides. It presents greater costs than traditional surgery, it requires volumetric imaging to be planned and it could present shortcomings while finalizing the provisional restoration due to intraoperative modifications to the planned surgery [
18,
19]. Among the advantages of a digital method to record and transfer the maxilla–mandibular relationship and vertical dimension of occlusion one can enumerate: reducing chair time costs compared to not guided implant rehabilitation and reducing costs compared to guided implant rehabilitation, more comfort in the immediate postoperative when an implant supported provisional is required as there is no need to newly record the maxilla–mandibular relation, radiation free alternative to guided implant rehabilitation when immediate loading is required.