Radiation Protection Evaluations Following the Installations of Two Cardiovascular Digital X-ray Fluoroscopy Systems
Abstract
:1. Introduction
2. Materials and Methods
2.1. Fluoroscopy X-ray Systems
2.2. Quality Control Tools
2.3. KAP and CAK Accuracy
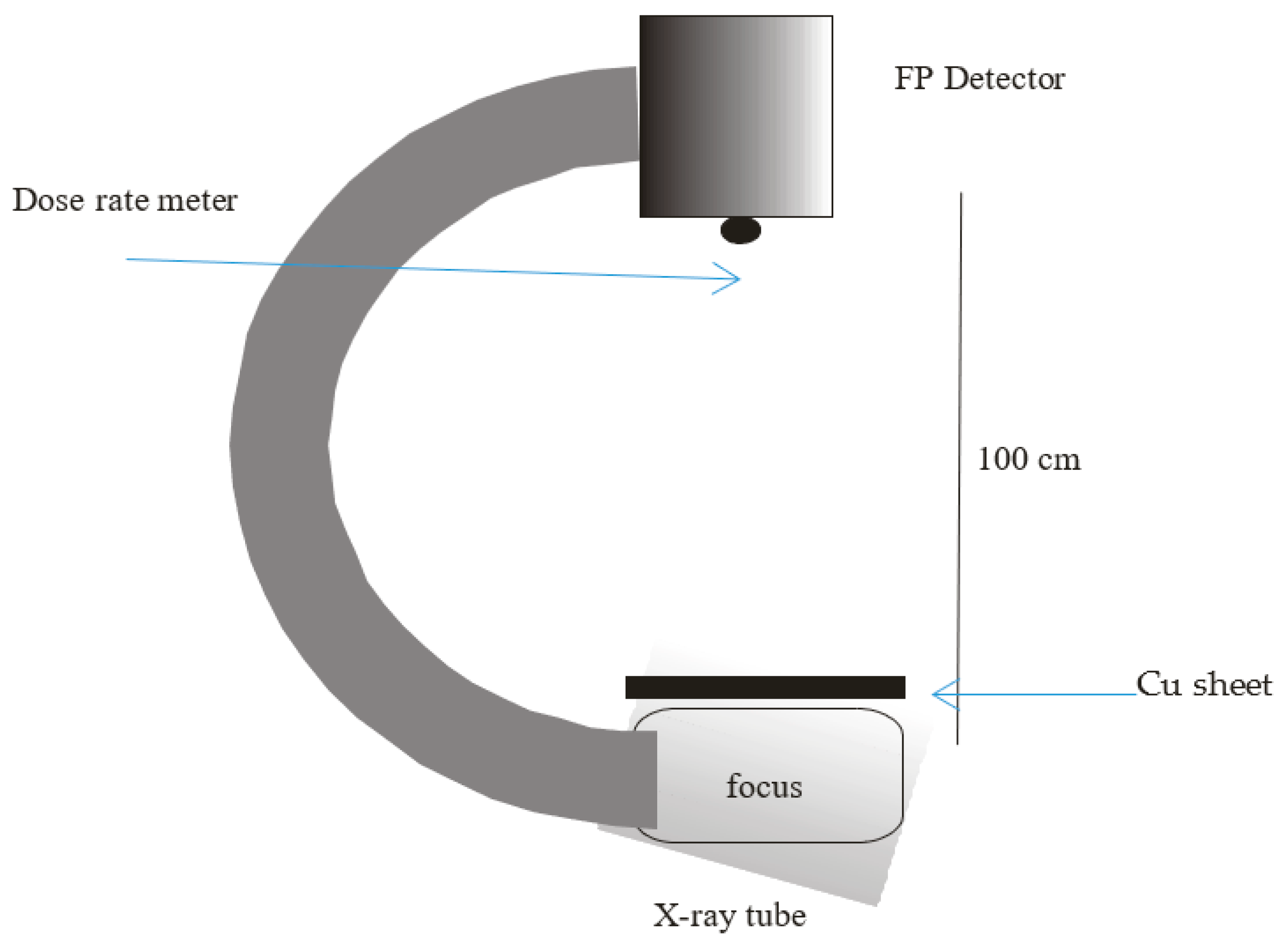
2.4. Dosimetry
2.5. Image Quality
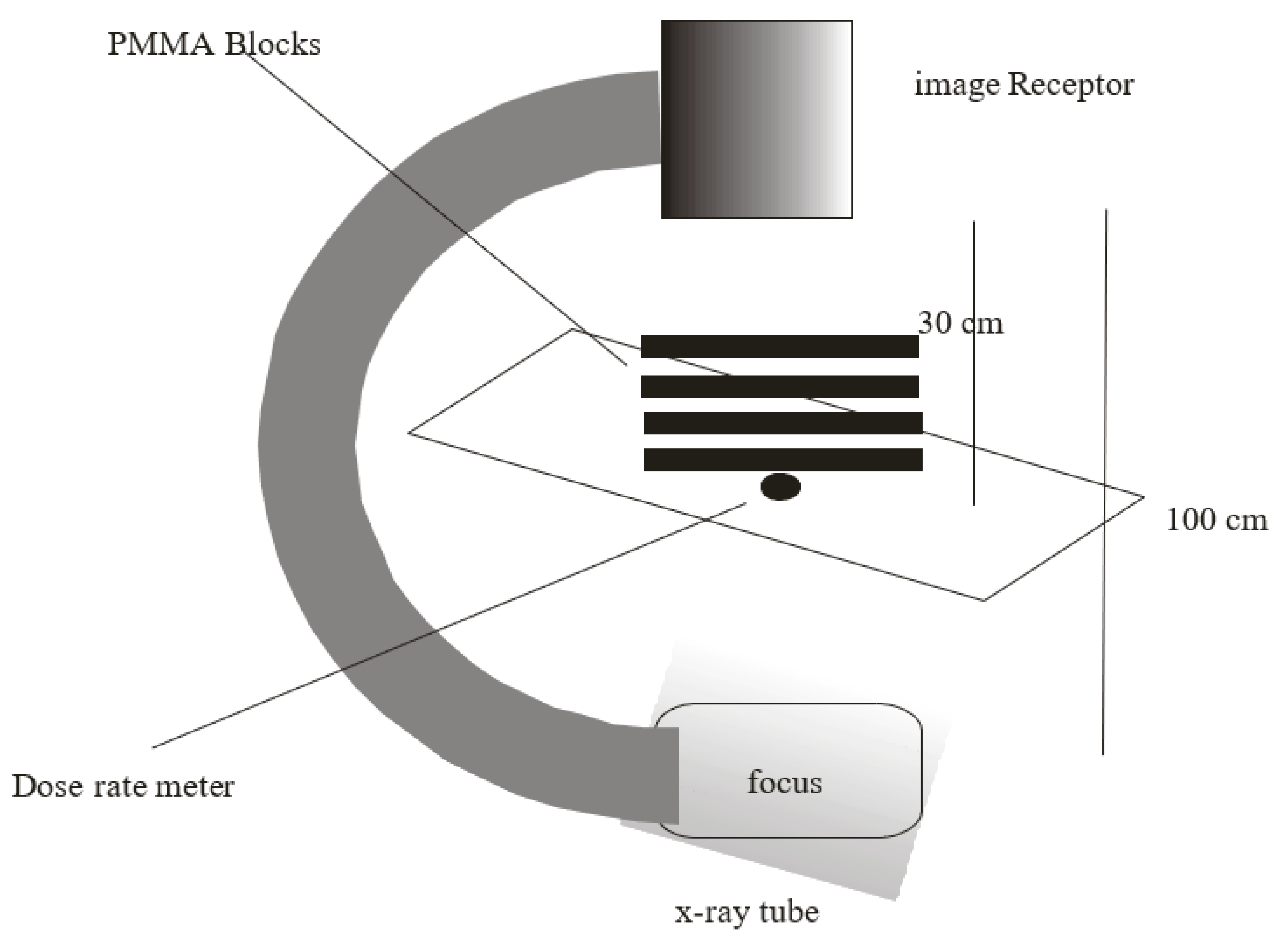
2.5.1. High- and Low-Contrast Resolution
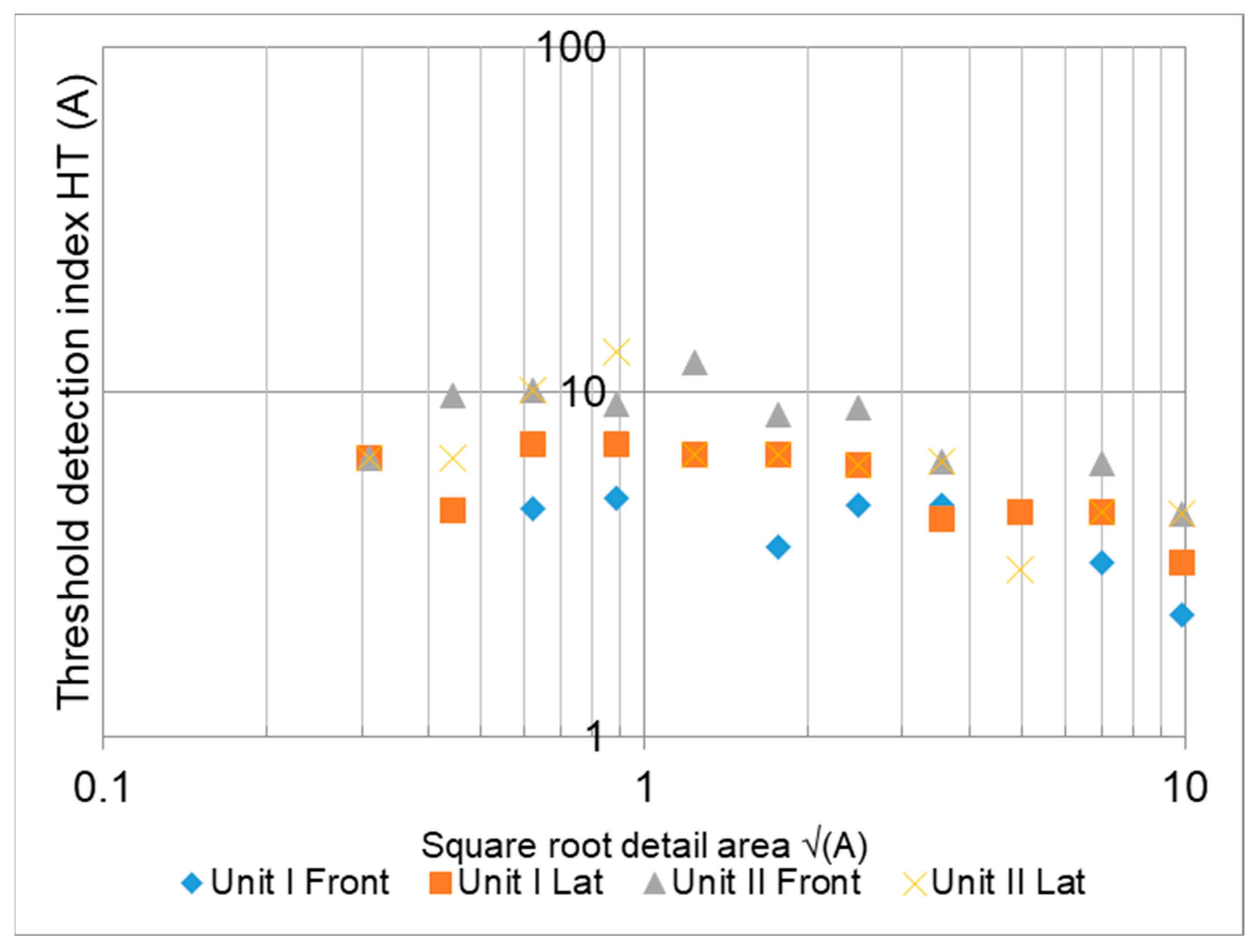
2.5.2. Threshold Contrast Detail Detectability (TCDD)
2.6. Radiation Protection
2.6.1. Light Field Radiation Beam Congruence
2.6.2. Minimum Source-to-Skin Distance (SSD)
2.6.3. Scattered Radiation Levels
3. Results
3.1. X-ray Tube and Generator Parameters
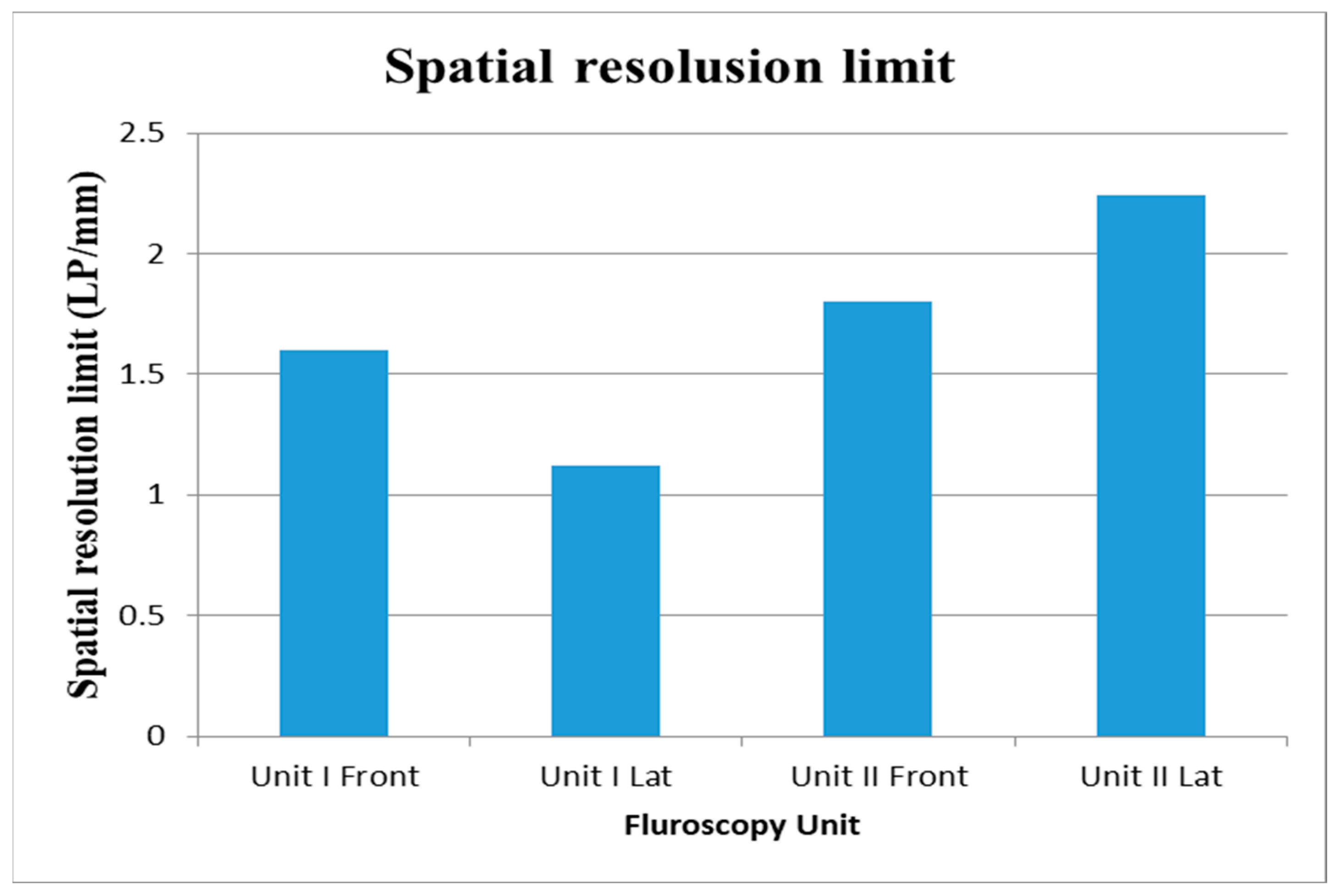
3.2. Image Quality
4. Discussion
4.1. Patient Dose
4.2. Image Quality
4.3. Radiation Protection
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Commission on Radiological Protection (ICRP). Managing patient dose in digital radiology. Ann. ICRP 2004, 34, 1–73. [Google Scholar]
- O’Connor, U.; Dowling, A.; Gallagher, A.; Gorman, D.; Walsh, C.; Larkin, A.; Gray, L.; Devine, M.; Malone, J. Acceptance testing of fluoroscopy systems used for interventional purposes. Radiat. Prot. Dosim. 2008, 129, 56–58. [Google Scholar] [CrossRef] [PubMed]
- Tsapaki, V.; Kottou, S.; Kollaros, N.; Dafnomili, P.; Kyriakidis, Z.; Neofotistou, V. Dose performance evaluation of a charge coupled device and a flat-panel digital fluoroscopy system recently installed in an interventional cardiology laboratory. Radiat. Prot. Dosim. 2004, 111, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Suliman, I.I. Estimates of patient radiation doses in digital radiography using DICOM information at a large teaching hospital in Oman. J. Digit. Imaging 2020, 33, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Al-Jabri, A.J.; Alzimami, K.; Alsafi, K.; Alaamer, A.S.; Al-Rajhi, M.A.; Suliman, I.I. Retrospective analysis of patient radiation doses in digital coronary angiography and interventions. Radiat. Prot. Dosim. 2019, 183, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, K. Dose displays and record keeping. Radiat. Prot. Dosim. 2001, 94, 143–145. [Google Scholar] [CrossRef] [PubMed]
- Valentin, J.; Boice, J.D., Jr.; Clarke, R.H.; Cousins, C.; Gonzalez, A.J.; Lee, J.; Lindell, B.; Meinhold, C.B.; Mettler, F.A., Jr.; Pan, Z.; et al. The 2007 Recommendations of the International Commission on Radiological Protection; Ann. ICRP 37; ICRP Publication 103; Pergamon Press: Oxford, UK, 2007; pp. 1–232. [Google Scholar]
- International Basic Safety Standards. General Safety Requirements Part 3; No. GSR Part 3; IAEA: Vienna, Austria, 2014. [Google Scholar]
- European Commission. Basic Safety Standards for Protection Against the Dangers Arising from Exposure to Ionising Radiation; Council Directive 2013/59/Euratom Directive; Official Journal of the European Communities: Luxembourg, 2013.
- Commission for European Communities. Criteria for Acceptability of Radiological, Nuclear Medicine and Radiotherapy Equipment; EC Radiation Protection Report No. 162; European Communities: Luxembourg, 2012.
- Zurcher, K.S.; Naidu, S.G.; Money, S.R.; Stone, W.M.; Fowl, R.J.; Knuttinen, G.; Oklu, R.; Coltvet, L.A.; Crawford, D.; Buras, M.R.; et al. Dose reduction using digital fluoroscopy versus digital subtraction angiography in endovascular aneurysm repair: A prospective randomized trial. J. Vasc. Surg. 2020, 72, 1938–1945. [Google Scholar] [CrossRef] [PubMed]
- Bjørkås, L.W.; Blø, S.; Rekdal, M.K.; Rusandu, A. Quality of radiation protection aprons and quality control routines at different diagnostic imaging modalities. Radiogr. Open 2020, 6, 64–74. [Google Scholar] [CrossRef]
- Zoetelief, J.; Van Soldt, R.T.; Suliman, I.I.; Jansen, J.T.; Bosmans, H. Quality control of equipment used in digital and interventional radiology. Radiat. Prot. Dosim. 2005, 117, 277–282. [Google Scholar] [CrossRef] [PubMed]
- American Association of Physicists in Medicine (AAPM); Diagnostic X-Ray Imaging Committee; Nickoloff, E.L. Cardiac Catheterization Equipment Performance; AAPM: Alexandria, Egypt, 2001. [Google Scholar]
- IEC. Report 60601 Medical electrical equipment. Part 2–43. In Particular Requirements for the Safety of X-ray Equipment for Interventional Procedures, 2nd ed.; International Electrotechnical Commission: Geneva, Switzerland, 2010. [Google Scholar]
- Food and Drug Administration (FDA). Public Health Advisory: Avoidance of Serious X-ray-Induced Skin Injuries to Patients during Fluoroscopically Guided Procedures; Center for Devices and Radiological Health: Rockville, MD, USA. Available online: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm063084.htm (accessed on 12 January 2021).
- International Commission on Radiation Measurements and Units. Patient Dosimetry for X-Rays Used in Medical Imaging; ICRU: Bethesda, MD, USA, 2006. [Google Scholar]
- National Council on Radiation Protection and Measurements. Radiation dose Management for Fuoroscopically Guided Interventional Medical Procedures; Report No.168; National Council on Radiation Protection and Measurements: Bethesda, MD, USA, 2010. [Google Scholar]
- Honey, I.; Rose, A.; Baker, C.; Charnock, P.; Fazakerley, J.; Iball, G.; Koutalonis, M.; Price, M.; Renaud, C.; Shaw, D.; et al. IPEM Topical Report: An evidence and risk assessment based analysis of the efficacy of tube and generator quality assurance tests on general x-ray units. Phys. Med. Biol. 2018, 63, 245011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaw, D.; Worrall, M.; Baker, C.; Charnock, P.; Fazakerley, J.; Honey, I.; Iball, G.; Koutalonis, M.; Price, M.; Renaud, C.; et al. IPEM Topical Report: An evidence and risk assessment based analysis of the efficacy of quality assurance tests on fluoroscopy units—part II; image quality. Phys. Med. Biol. 2020, 65, 225037. [Google Scholar] [CrossRef] [PubMed]
- Worrall, M.; Shaw, D.; Baker, C.; Charnock, P.; Fazakerley, J.; Honey, I.; Iball, G.; Koutalonis, M.; Price, M.; Renaud, C.; et al. IPEM Topical Report: An evidence and risk assessment based analysis of the efficacy of quality assurance tests on fluoroscopy units—part I; dosimetry and safety. Phys. Med. Biol. 2019, 64, 195011. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Inaba, Y.; Saito, H.; Ishibashi, T.; Takahashi, S.; Kohzuki, M.; Zuguchi, M. Radiation dose of interventional radiology system using a flat-panel detector. Am. J. Roentgenol. 2009, 193, 1680–1685. [Google Scholar] [CrossRef] [PubMed]
- Sjöholm, B.; Geijer, H.; Persliden, J. Impact of digital imaging on radiation doses to the patient during X-ray examination of the urinary tract. Acta Radiol. 2005, 46, 657–661. [Google Scholar] [CrossRef] [PubMed]

| Code | Output@ 80 kVp (µGy) | HVL (mm ALeq) | Accuracy (%) a | Field Size b | Contrast Resolution | |||
|---|---|---|---|---|---|---|---|---|
| Fluoro | Radiography | X | Y | |||||
| EC Criteria | 25–90 | 70 kVp | 80 kVp | 10 | 5 | <1% of SID | 3% | |
| Unit I | ||||||||
| Frontal | 68 | 3.0 | 3.5 | 5.4 | 2 | <1 | <1 | 1.3 |
| Lateral | 75 | 3.0 | 3.5 | 4.2 | 1.6 | <1 | <1 | 1.3 |
| Unit II | ||||||||
| Frontal | 56 | 2.9 | 3.3 | 4.5 | 3.0 | <1 | <1 | 1.3 |
| Lateral | 59 | 2.8 | 3.2 | 3.6 | 2.2 | <1 | <1 | 1.3 |
| Unit | Dose Quantity | Measured | Indicated | Error % |
|---|---|---|---|---|
| UNIT I | ||||
| Frontal | KAP (mGy.cm2) | 1114 | 1092 | 2.0 |
| CAK(mGy) | 2.21 | 2.00 | 10.7 | |
| Lateral | KAP (mGy.cm2) | 1037 | 962 | 7.7 |
| CAK (mGy) | 2.98 | 3.00 | −0.8 | |
| UNIT II | ||||
| Frontal | KAP (mGy.cm2) | 135 | 156 | 13.0 |
| CAK (mGy) | 1.02 | 1.2 | 16.0 | |
| Lateral | KAP (mGy.cm2) | 171 | 180 | 6 |
| CAK (mGy) | 2.2 | 2.4 | 8.3 | |
| Phantom | Unit II Frontal | Unit II Lateral | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PMMA cm | AL mm | Kilovoltage | ESAK | Kilovoltage | ESAK (mGy/ min) | ||||
| Indicated | Measured | Error % | (mGy/ min) | Indicated | Measured | Error % | |||
| 1.0 | 53.00 | 56.83 | 7.23 | 0.62 | 55.00 | 55.35 | 0.64 | ||
| 3.0 | 58.13 | 55.00 | −5.38 | 0.94 | 59.00 | 60.95 | 3.31 | ||
| 5.5 | 62.17 | 59.00 | −5.10 | 2.01 | 61.00 | 61.91 | 1.49 | 0.88 | |
| 10.5 | 66.13 | 64.00 | −3.22 | 3.96 | 63.00 | 64.94 | 3.08 | 2.81 | |
| 15.0 | 70.00 | 68.00 | −2.86 | 6.45 | 68.00 | 69.80 | 2.65 | 5.77 | |
| 18.0 | 74.30 | 73.00 | −1.75 | 10.15 | 72.00 | 75.80 | 5.28 | 11.69 | |
| 18.0 | 2.5 | 75.90 | 75.00 | −1.19 | 11.99 | 75.00 | 80.20 | 6.93 | 10.30 |
| Fluoroscopy | Mode of Operation | Frontal | Lateral | ||
|---|---|---|---|---|---|
| Vascular | Cardiac | Vascular | Cardiac | ||
| Maximum ESAK (5 mm Al + 5 mm Cu) | |||||
| Unit I | Continuous (mGy/min.) | 8.04 | - | 9.00 | |
| Pulsed (mGy/f) | 0.01 | 0.01 | 0.01 | 0.01 | |
| Unit II | Continuous (mGy/min.) | 20.6 | 40.4 | 19.5 | 39.2 |
| Pulsed (mGy/f) | 0.02 | 0.04 | 0.02 | 0.04 | |
| Maximum FPD input air kerma rates (2 mm Cu) | |||||
| Unit I | Continuous (µGy/s) | 0.29 | 0.18 | 0.39 | - |
| Pulsed (µGy/f) | 0.02 | 0.01 | 0.031 | 0.01 | |
| Unit II | Continuous (µGy/s) | - | 0.72 | 0.10 | 0.94 |
| Pulsed (µGy/f) | 0.074 | 0.047 | - | 0.06 | |
| Phantom | ESAK (mGy/min) | IR Input (µGy/s) | Digital Acquisition (µGy/Frame) | Detector | |
|---|---|---|---|---|---|
| Suliman, et al. * (This Study) | 5 mm Al + 5 mm Cu | 8.0–9.0 | 0.2–0.4 | 0.1 | FP |
| 18 cm PMMA + 2.5 mm Al | 10.3–12.0 | -- | -- | FP | |
| O’Connor, et al. (2008) | 20 cm water | 4.6 | 0.6 | 2.6 | FP |
| Koichi Chida1, et al. (2009) | 20 cm water | 16.6 ± 7.9 | -- | 0.20 ± 0.10 | FP |
| 20 cm water | 17.8 | -- | 0.20 ± 0.10 | II | |
| II |
| Minimum SID | Scatter Radiation at 1 m | Ambient Dose Rates | Warning Signs | ||
|---|---|---|---|---|---|
| Controlled Areas | Supervised Areas | ||||
| Tolerance Ref. [10] | 45 cm | 20 µGymin−1 | 88 (µGy/wk) | 18 (µGy/wk) | Availability |
| Unit I | |||||
| Frontal | 58 | 4.0 | <10 | <10 | Available |
| Lateral | 46 | 4.7 | <10 | <10 | Available |
| Unit II | |||||
| Frontal | 58 | 4.4 | <10 | <10 | Available |
| Lateral | 46 | 4.7 | <10 | <10 | Available |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suliman, I.I.; Sulieman, A.; Mattar, E. Radiation Protection Evaluations Following the Installations of Two Cardiovascular Digital X-ray Fluoroscopy Systems. Appl. Sci. 2021, 11, 9749. https://doi.org/10.3390/app11209749
Suliman II, Sulieman A, Mattar E. Radiation Protection Evaluations Following the Installations of Two Cardiovascular Digital X-ray Fluoroscopy Systems. Applied Sciences. 2021; 11(20):9749. https://doi.org/10.3390/app11209749
Chicago/Turabian StyleSuliman, Ibrahim I., Abdelmoneim Sulieman, and Essam Mattar. 2021. "Radiation Protection Evaluations Following the Installations of Two Cardiovascular Digital X-ray Fluoroscopy Systems" Applied Sciences 11, no. 20: 9749. https://doi.org/10.3390/app11209749
APA StyleSuliman, I. I., Sulieman, A., & Mattar, E. (2021). Radiation Protection Evaluations Following the Installations of Two Cardiovascular Digital X-ray Fluoroscopy Systems. Applied Sciences, 11(20), 9749. https://doi.org/10.3390/app11209749






