Physical Ergonomics in Peripheral Nerve Block
Abstract
1. Introduction
2. Conceptual Framework of Physical Ergonomics in PNB
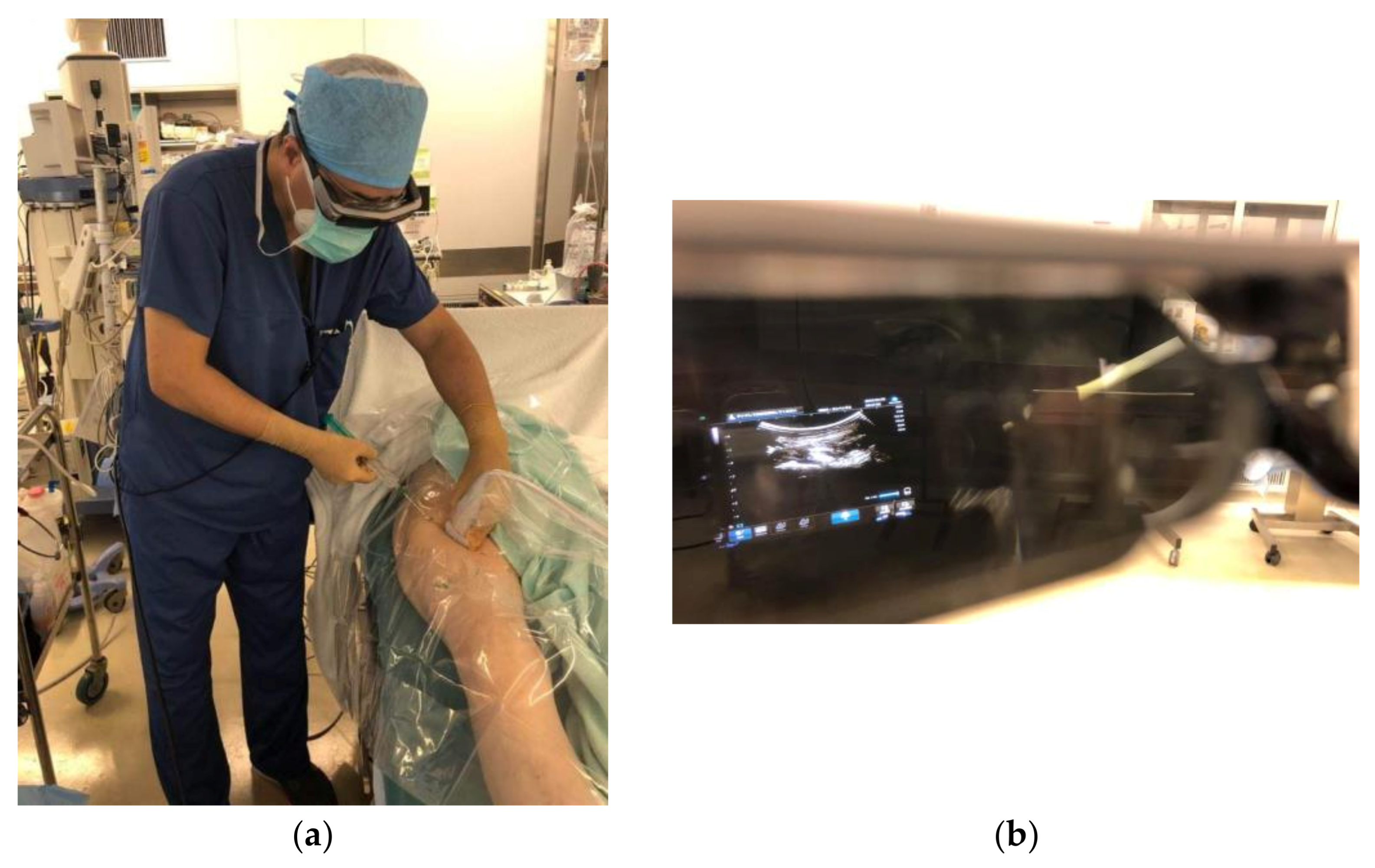
2.1. Brain: Minimising Visuospatial Neuroprocessing Burden Using Equipment Configuration
2.1.1. Importance of Gaze-Down Viewing
2.1.2. Head-Mounted Display
2.1.3. Visuospatial Aptitude
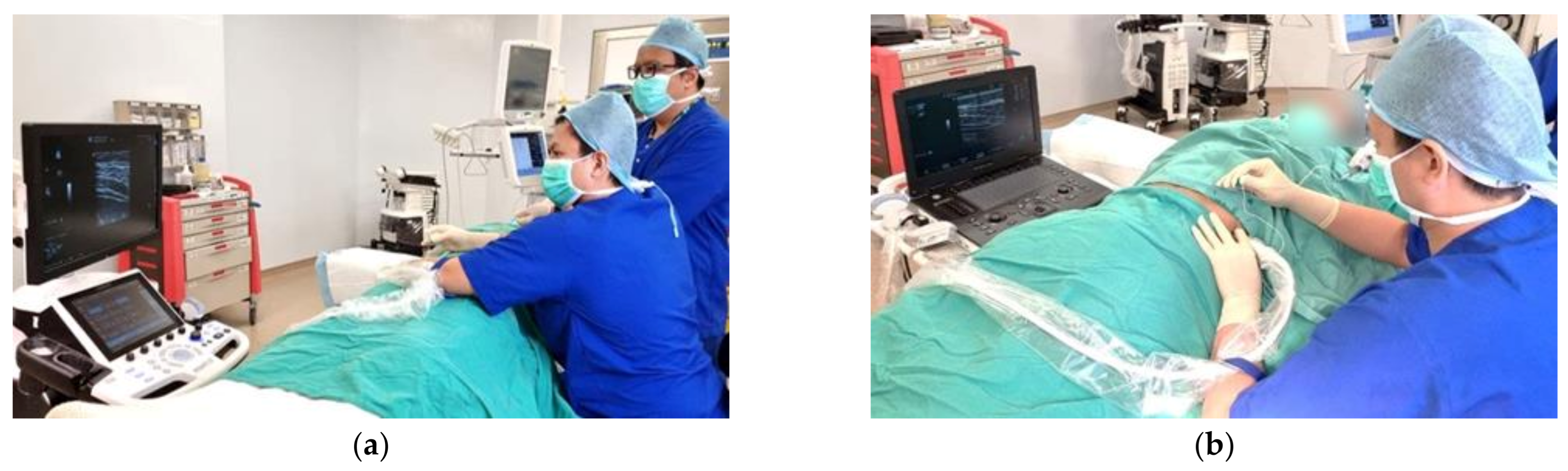
2.2. Environment Principles
2.3. Role of Assistants
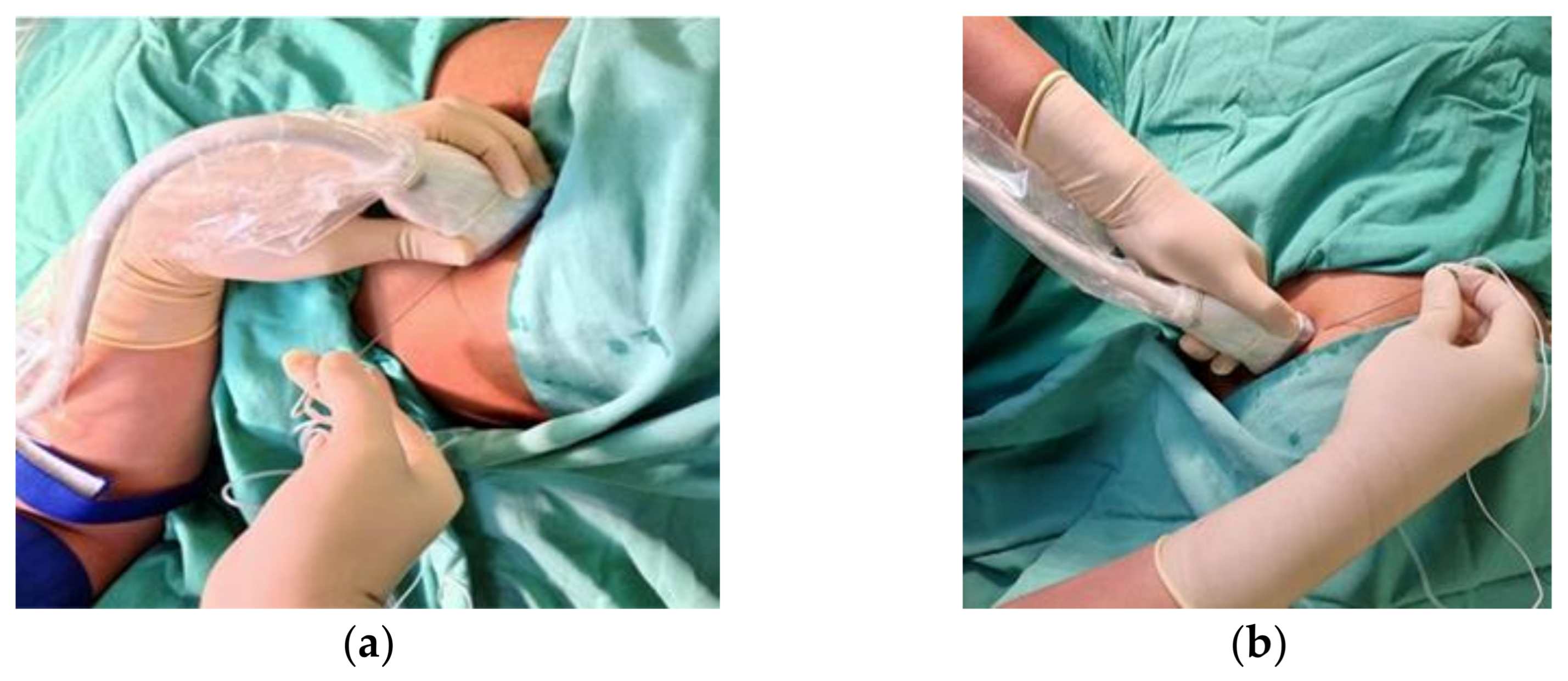
2.4. Musculoskeletal: Neutral Posture and Patient Positioning
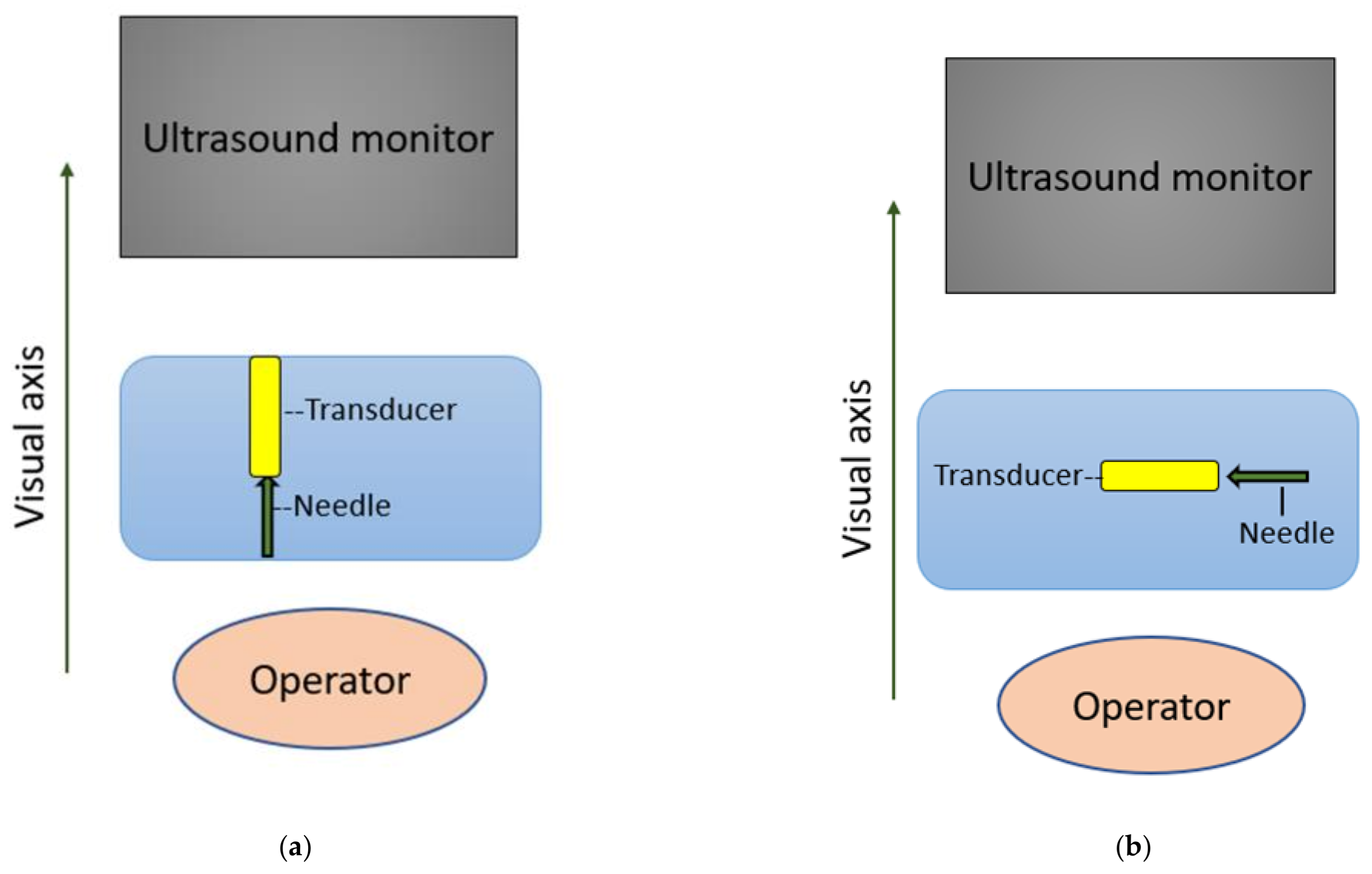
2.5. Ergonomic Needling Strategy
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albrecht, E.; Chin, K.J. Advances in regional anaesthesia and acute pain management: A narrative review. Anaesthesia 2020, 75, e101–e110. [Google Scholar] [CrossRef] [PubMed]
- Alexander, G.; Staggers, N. A Systematic Review on the Designs of Clinical Technology: Findings and Recommendations for Future Research. ANS Adv. Nurs. Sci. 2009, 32, 252–279. [Google Scholar] [CrossRef] [PubMed]
- International Ergonomics Association (IEA) Council. Definition and Domains of Ergonomics [IEA Council Website]. Available online: https://iea.cc/what-is-ergonomics/ (accessed on 1 May 2021).
- Lin, J.A.; Blanco, R.; Shibata, Y.; Nakamoto, T. Advances of Techniques in Deep Regional Blocks. BioMed Res. Int. 2017, 7268308. [Google Scholar] [CrossRef] [PubMed]
- Chan, V. Ultrasound Imaging for Nerve: A Standard Practice for the Future? ASA Newsl. 2005, 69, 8–9. [Google Scholar]
- Hana, G.; Shimi, S.; Cuschieri, A. Task Performance in Endoscopic Surgery Is Influenced by Location of the Image Display. Ann. Surg. 1998, 277, 481–484. [Google Scholar] [CrossRef]
- Omar, A.; Wade, N.; Brown, S.; Cuschieri, A. Assessing the benefits of “gaze-down” display location in complex tasks. Surg. Endosc. 2005, 19, 105–108. [Google Scholar] [CrossRef]
- Wade, N.J. Frames of reference in vision. Minim. Invasive Ther. Allied Technol. 1996, 5, 435–439. [Google Scholar] [CrossRef]
- Shalabi, K.M. Neuroscience of Motor Learning in Adults with Non-Dominant Hand. J. Crit. Rev. 2020, 7, 27–30. [Google Scholar]
- Liu, D.; Jenkins, S.A.; Sanderson, P.M.; Fabian, P.; Russell, W.J. Monitoring with head-mounted displays in general anesthesia: A clinical evaluation in the operating room. Anesth. Analg. 2010, 110, 1032–1038. [Google Scholar] [CrossRef]
- Udani, A.D.; Harrison, T.K.; Howard, S.K.; Kim, T.E.; Brock-Utne, J.G.; Gaba, D.M.; Mariano, E.R. Preliminary study of ergonomic behavior during simulated ultrasound-guided regional anesthesia using a head-mounted display. J. Ultrasound. Med. 2012, 31, 1277–1280. [Google Scholar] [CrossRef]
- Hughey, S.; Cole, J.; Booth, G.; Longwell, J. Letter to the editor: Head-mounted display for regional anesthesia. Reg. Anesth. Pain Med. 2021, 46, 740–741. [Google Scholar] [CrossRef]
- Przkora, R.; McGrady, W.; Vasilopoulos, T.; Gravenstein, N.; Solanki, D. Evaluation of the Head-Mounted Display for Ultrasound-Guided Peripheral Nerve Blocks in Simulated Regional Anesthesia. Pain Med. 2015, 16, 2192–2194. [Google Scholar] [CrossRef]
- Kasuya, Y.; Moriwaki, S.; Inano, C.; Fukada, T.; Komatsu, R.; Ozaki, M. Feasibility of the head-mounted display for ultrasound-guided nerve blocks: A pilot simulator study. J. Anesth. 2017, 31, 782–784. [Google Scholar] [CrossRef]
- Przkora, R.; Mora, J.; Balduyeu, P.; Meroney, M.; Vasilopoulos, T.; Solanki, D. Ultrasound-Guided Regional Anesthesia Using a Head-Mounted Video Display: A Randomised Clinical Study. Pain Physician 2021, 24, 83–87. [Google Scholar]
- Hyunh, K.T.; Chaika, J.; Kim, T.W. Simultaneous display of real-time ultrasound and surface landmark image. Reg. Anesth. Pain Med. 2019, 45, 481. [Google Scholar] [CrossRef]
- Strumia, A.; Costa, F.; Pascarella, G. Felice Agrò, F.E. Eyes-hands alignment during regional anesthesia procedures: The Ultrasound Support. Saudi J. Anesth. 2021, 15, 227–228. [Google Scholar] [CrossRef]
- Smith, H.M.; Kopp, S.L.; Johnson, R.L.; Long, T.R.; Cerhan, J.H.; Hebl, J.R. Looking into learning: Visuospatial and psychomotor predictors of ultrasound-guided procedural performance. Reg. Anesth. Pain Med. 2012, 37, 441–447. [Google Scholar] [CrossRef]
- Shafqat, A.; Ferguson, E.; Thanawala, V.; Bedforth, N.M.; Hardman, J.G.; McCahon, R.A. Visuospatial Ability as a Predictor of Novice Performance in Ultrasound-guided Regional Anesthesia. Anesthesiology 2015, 123, 1188–1197. [Google Scholar] [CrossRef]
- Ajmal, M.; Power, S.; Smith, T.; Shorten, G.D. Ergonomic task analysis of ultrasound-guided femoral nerve block: A pilot study. J. Clin. Anesth. 2011, 23, 35–41. [Google Scholar] [CrossRef]
- Katz, J.D. Control of the Environment in the Operating Room. Anesth. Analg. 2017, 125, 1214–1218. [Google Scholar] [CrossRef]
- Katz, J.D. Noise in the operating room. Anesthesiology 2014, 121, 894–898. [Google Scholar] [CrossRef]
- The 2018 FGI Guidelines—Facility Guidelines. Available online: https://www.fgiguidelines.org/wp-content/uploads/2017/08/SLS17_FGI_ExamProcedureOperatingImaging_170721.pdf (accessed on 1 August 2021).
- CKAPS-ICL-Operation Theatre (Ver. Oct 2016). 1/11. Standard for Operation Theatre. Available online: http://medicalprac.moh.gov.my/v2/uploads/Pelan%20Lantai%20dan%20Lawatan/07OT_Oct%202016.pdf (accessed on 1 August 2021).
- Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations during Severe Shortages. Available online: https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages (accessed on 27 September 2021).
- Bailey, C.R.; Radhakrishna, S.; Asanati, K.; Dill, N.; Hodgson, K.; McKeown, C.; Pawa, A.; Plaat, F.; Wilkes, A. Ergonomics in the anaesthetic workplace. Anaesthesia 2021. [Google Scholar] [CrossRef]
- Tolu, S.; Basaran, B. Work-related musculoskeletal disorders in anesthesiologists: A cross-sectional study on prevalence and risk factors. Ann. Med. Res. 2019, 26, 1406–1414. [Google Scholar] [CrossRef]
- Leifer, S.; Choi, S.W.; Asanati, K.; Yentis, S.M. Upper limb disorders in anaesthetists—A survey of Association of Anaesthetists members. Anaesthesia 2019, 74, 285–291. [Google Scholar] [CrossRef]
- Baker, J.P.; Coffin, C.T. The Importance of an Ergonomic Workstation to Practicing Sonographers. Ultrasound Med. 2013, 32, 1363–1375. [Google Scholar] [CrossRef]
- Murphey, S.; Evans, K.; Merton, D. Industry Standards for the Prevention of Work-Related Musculoskeletal Disorders in Sonography. J. Diagn. Med. Sonogr. 2017, 33, 371–391. [Google Scholar] [CrossRef]
- Ajmal, M.; Power, S.; Smith, T.; Shorten, G.D. An ergonomic task analysis of spinal anaesthesia. Eur. J. Anaesthesiol. 2009, 26, 1037–1042. [Google Scholar] [CrossRef]
- Marhofer, P.; Harrop-Griffiths, W.; Willschke, H.; Kirchmair, L. Fifteen years of ultrasound guidance in regional anaesthesia: Part 2—Recent developments in block techniques. Br. J. Anaesth. 2010, 104, 673–683. [Google Scholar] [CrossRef]
- Sites, B.D.; Spence, B.C.; Gallagher, J.D.; Wiley, C.W.; Bertrand, M.L.; Blike, G.T. Characterizing Novice Behavior Associated with Learning Ultrasound-Guided Peripheral Regional Anesthesia. Reg. Anesth. Pain Med. 2007, 32, 107–115. [Google Scholar] [CrossRef]
- Speer, M.; McLennan, N.; Nixon, C. Novice Learner In-Plane Ultrasound Imaging Which Visualisation Technique? Reg. Anesth. Pain Med. 2013, 38, 350–352. [Google Scholar] [CrossRef]
- Wilson, J.M.B.; Germain, G.; Vaghadia, H.; Tang, R.; Sawka, A. In-plane ultrasound-guided needle insertion ALONG or ACROSS the visual axis hand positions. Br. J. Anaesth. 2014, 113, 717–722. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chin, K.J.; Perlas, A.; Chan, V.M.S.; Brull, R. Needle Visualization in Ultrasound-Guided Regional Anesthesia: Challenges and Solutions. Reg. Anesth. Pain Med. 2008, 33, 532–544. [Google Scholar] [CrossRef] [PubMed]
- Ueshima, H.; Kitamura, A. The use of a needle guide kit improves the stability of ultrasound-guided techniques. J. Anesth. 2015, 29, 803–804. [Google Scholar] [CrossRef] [PubMed]
- Hebard, S.; Hocking, G. Echogenic technology can improve needle visibility during ultrasound-guided regional anesthesia. Reg. Anesth. Pain Med. 2011, 36, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Abbal, B.; Choquet, O.; Gourari, A.; Bouic, N.; Massone, A.; Biboulet, P.; Bringuier, S.; Capdevila, X. Enhanced visual acuity with echogenic needles in ultrasound-guided axillary brachial plexus block: A randomized, comparative, observer-blinded study. Minerva Anestesiol. 2015, 81, 369–378. [Google Scholar] [PubMed]
- Uppal, V.; Sondekoppam, R.V.; Ganapathy, S. Effect of beam steering on the visibility of echogenic and non-echogenic needles: A laboratory study. Can. J. Anaesth. 2014, 61, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Prabhakar, C.; Uppal, V.; Sondekoppam, R.V. Effect of Beam Steering on Echogenic and Nonechogenic Needle Visibility at 40°, 50°, and 60° Needle Insertion Angles. Anesth. Analg. 2018, 126, 1926–1929. [Google Scholar] [CrossRef]
- Scholten, H.J.; Pourtaherian, A.; Mihajlovic, N.; Korsten, H.H.M.; Bouwman, R.A. Improving needle tip identification during ultrasound-guided procedures in anaesthetic practice. Anaesthesia 2017, 72, 889–904. [Google Scholar] [CrossRef]








| 1. | Optimise the Balance between Visual Input and the Cognitive Capacity to Orientate and Respond to the Combination of Visual and Physical Feedback | |
|---|---|---|
| (a) | The monitor is located in front of the operator, at the level of the hands, allowing gaze-down viewing and alignment of the visual and motor axes. | |
| (b) | The image of the needle on the ultrasound monitor is placed on the same side as the needle entry. | |
| (c) | The block needle is best held in the dominant hand for better fine motor control. | |
| (d) | The head-mounted display has been shown to improve ergonomics by abolishing the need to view the ultrasound monitor directly. | |
| 2. | Careful Planning of Posture and Position to Reduce Physical Fatigue | |
| (a) | Neutral posture is a seated or standing posture balanced around the operator’s centre of gravity. | |
| (b) | Avoid non-neutral postures: sustained reach; bending and twisting of the trunk; excess neck flexion, extension or protraction and rotation; uneven seated or standing weight distribution; wrist flexion or extension; and/or deviation pinch grip. | |
| (c) | Avoid improper postures: Arm abduction, defined as an angle greater than 30° between the torso and the upper extremity, and overreaching, requires the operator to use the shoulder muscles. | |
| (d) | Place the ultrasound monitor straight ahead for the operator to have a slight 15° to 20° neck flexion while viewing the monitor (vertically adjustable articulating monitors). | |
| (e) | Adjust the patient bed/trolley or operating table. | |
| (f) | Adopt neutral wrist position while holding the probe or the block needle and resting on the patient’s body or using the patient’s skin for support. | |
| (g) | Utilise palmar grip; it is firmer and there is less strain. | |
| (h) | Regional anaesthesia trolley or tray should also be placed on the dominant side of the operator’s handedness to avoid reaching across and overreaching. | |
| 3. | Choosing an Effective Approach Strategy for Insertion of the Block Needle to Achieve Needle Beam Alignment for Optimal Needle Visualisation | |
| (a) | Probe and needle should be aligned along the visual axis with an in-plane approach. | |
| (b) | The needle is best inserted at a needle beam angle greater than 55° for the best needle visibility in the in-plane approach. | |
| (c) | Use of needle guidance, echogenic needle and ultrasound beam steering improve needle visualisation. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fathil, S.M.; Ghani, M.R.A.; Chen, K.-Y.; Lee, P.; Hou, J.-D.; Lin, J.-A. Physical Ergonomics in Peripheral Nerve Block. Appl. Sci. 2021, 11, 9736. https://doi.org/10.3390/app11209736
Fathil SM, Ghani MRA, Chen K-Y, Lee P, Hou J-D, Lin J-A. Physical Ergonomics in Peripheral Nerve Block. Applied Sciences. 2021; 11(20):9736. https://doi.org/10.3390/app11209736
Chicago/Turabian StyleFathil, Shahridan Mohd, Muhamad Rasydan Abdul Ghani, Kung-Yen Chen, Pinhsin Lee, Jin-De Hou, and Jui-An Lin. 2021. "Physical Ergonomics in Peripheral Nerve Block" Applied Sciences 11, no. 20: 9736. https://doi.org/10.3390/app11209736
APA StyleFathil, S. M., Ghani, M. R. A., Chen, K.-Y., Lee, P., Hou, J.-D., & Lin, J.-A. (2021). Physical Ergonomics in Peripheral Nerve Block. Applied Sciences, 11(20), 9736. https://doi.org/10.3390/app11209736






