Lower-Limb Exosuits for Rehabilitation or Assistance of Human Movement: A Systematic Review
Abstract
Featured Application
Abstract
1. Introduction
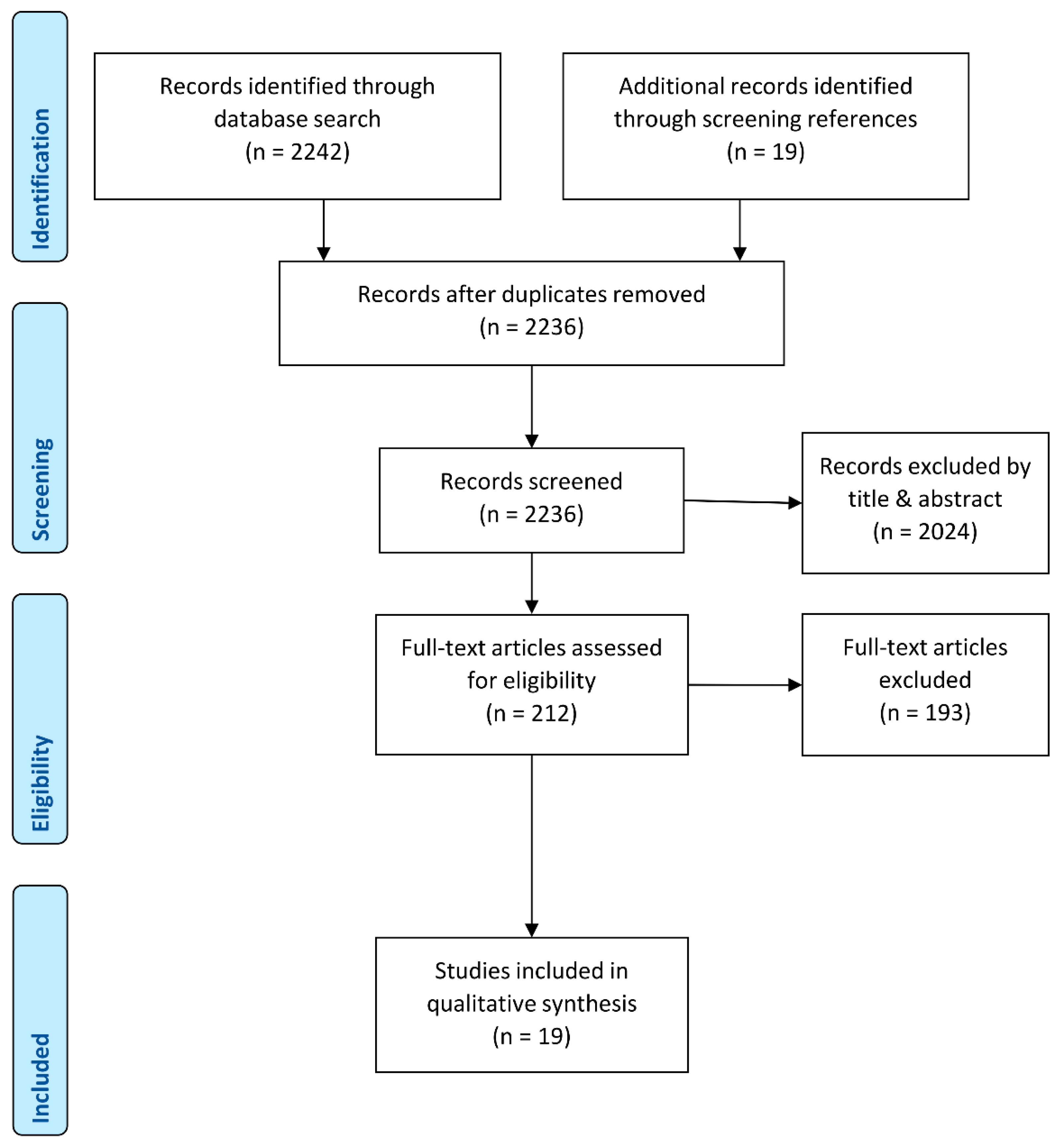
2. Methods
2.1. Search Strategy
(exoskeleton OR exoskeletons OR exosuit OR exosuits OR orthosis OR orthotics OR frame OR suit) AND (soft OR elastic OR semi-rigid OR flexible) AND (rehabilitation OR enhancing OR enhancement OR activity OR stability OR running OR walking OR gait OR assistance OR stroke OR energy)
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
3. Review
3.1. Database Search
3.2. Quality Assessment
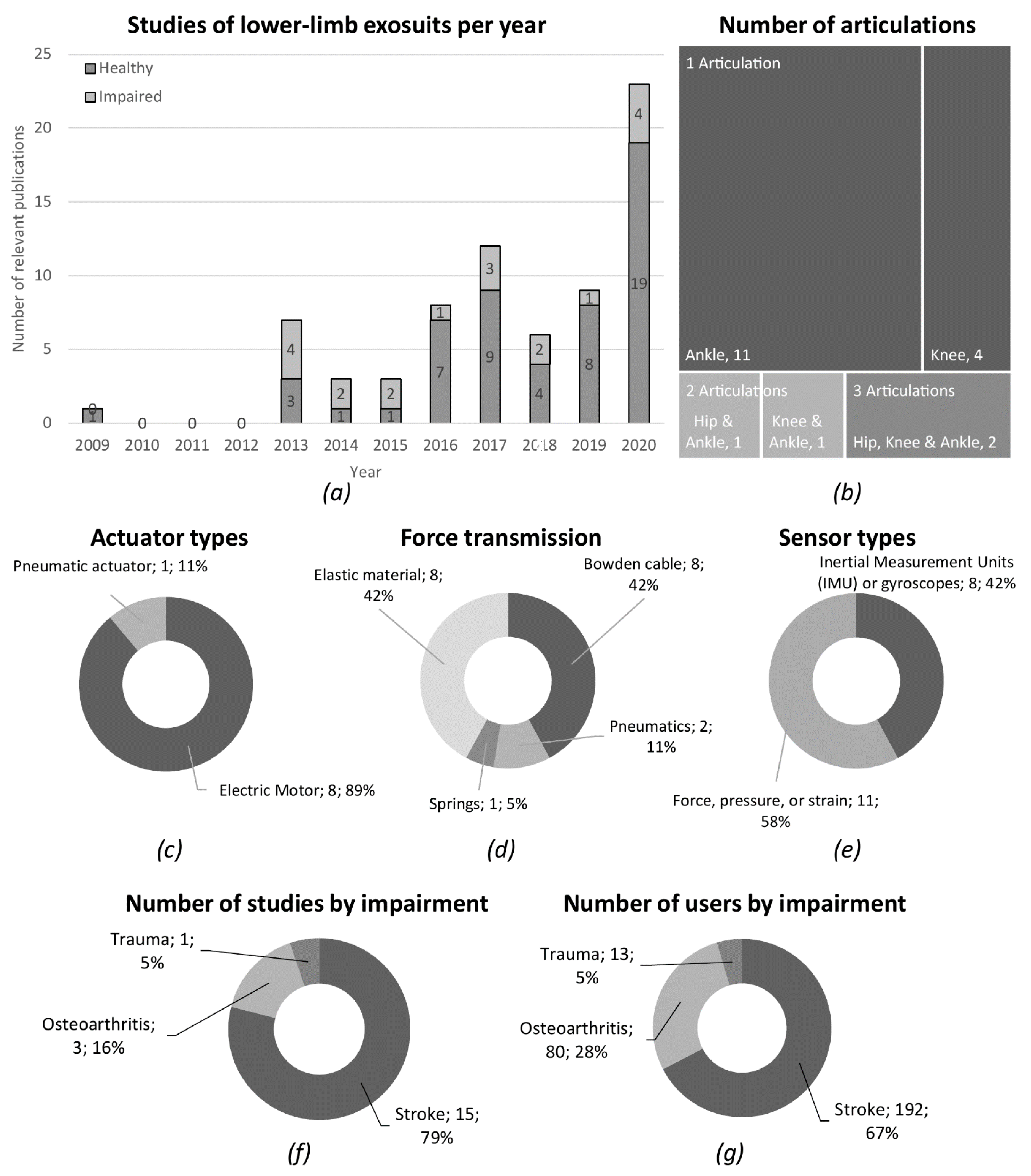
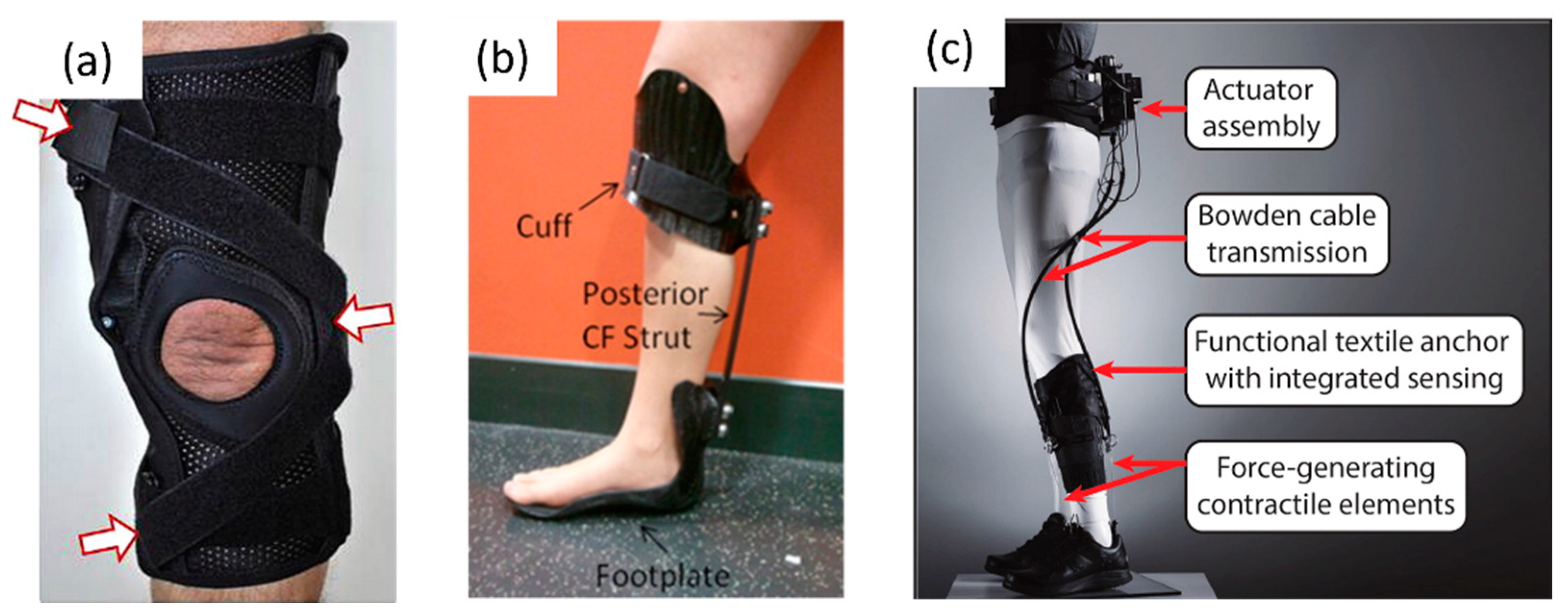
3.3. Exosuit Technology
3.4. Clinical Studies
3.5. Study Limitations
4. Conclusions
4.1. What Technologies Are Used in Lower-Limb Exosuits?
4.2. What Are the Outcomes of Clinical Evaluations of Lower-Limb Exosuits with Users Suffering from Mobility Impairment?
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Armour, B.S.; Courtney-Long, E.A.; Fox, M.H.; Fredine, H.; Cahill, A. Prevalence and Causes of Paralysis-United States, 2013. Am. J. Public Health 2016, 106, 1855–1857. [Google Scholar] [CrossRef] [PubMed]
- Fagerström, C.; Borglin, G. Mobility, functional ability and health-related quality of life among people of 60 years or older. Aging Clin. Exp. Res. 2010, 22, 387–394. [Google Scholar] [CrossRef]
- Okoro, C.A.; Hollis, N.D.; Cyrus, A.C.; Griffin-Blake, S. Prevalence of Disabilities and Health Care Access by Disability Status and Type Among Adults—United States, 2016. MMWR Morb. Mortal Wkly. Rep. 2018, 67, 882–887. [Google Scholar] [CrossRef]
- Eurostat. Ageing Europe—Looking at the Lives of Older People in the EU, Statistical Books, 20th ed.; Corselli-Nordblad, L., Strandell, H., Eds.; Publications Office of the European Union: Luxembourg, 2020; ISBN 978-92-76-21520-2. [Google Scholar]
- Esquenazi, A.; Talaty, M. Robotics for Lower Limb Rehabilitation. Phys. Med. Rehabil. Clin. 2019, 30, 385–397. [Google Scholar] [CrossRef]
- Herr, H. Exoskeletons and orthoses: Classification, design challenges and future directions. J. Neuroeng. Rehabil. 2009, 6, 21. [Google Scholar] [CrossRef]
- Nycz, C.; Delph, M.; Fischer, G. Modeling and design of a tendon actuated soft robotic exoskeleton for hemiparetic upper limb rehabilitation. In Proceedings of the 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 3889–3892. [Google Scholar]
- Awad, L.; Bae, J.; O’Donnell, K.; De Rossi, S.M.; Hendron, K.; Sloot, L.H.; Kudzia, P.; Allen, S.; Holt, K.G.; Ellis, T.D.; et al. A soft robotic exosuit improves walking in patients after stroke. Sci. Transl. Med. 2017, 9, eaai9084. [Google Scholar] [CrossRef]
- Body Braid. Available online: https://bodybraid.com (accessed on 13 June 2018).
- SuperFlex Soft Biofidelic Actuated Exosuit. Available online: https://www.sri.com/brochures/superflex-soft-biofidelic-actuated-exosuit (accessed on 13 June 2018).
- The ReStore™ Sof Exo-Suit. ReWalk—More Than Walking. Available online: https://rewalk.com/restore-exo-suit/ (accessed on 1 October 2020).
- Shi, D.; Zhang, W.; Zhang, W.; Ding, X. A Review on Lower Limb Rehabilitation Exoskeleton Robots. Chin. J. Mech. Eng. 2019, 32, 74. [Google Scholar] [CrossRef]
- Pamungkas, D.S.; Caesarendra, W.; Soebakti, H.; Analia, R.; Susanto, S. Overview: Types of Lower Limb Exoskeletons. Electronics 2019, 8, 1283. [Google Scholar] [CrossRef]
- Jain, A.; Jain, K. Soft exosuit—A review. Int. Rob. Auto. J. 2020, 6, 99–101. [Google Scholar]
- Crowell, H.P.; Park, J.H.; Haynes, C.A.; Neugebauer, J.M.; Boynton, A.C. Design, Evaluation, and Research Challenges Relevant to Exoskeletons and Exosuits: A 26-Year Perspective From the U.S. Army Research Laboratory. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 199–212. [Google Scholar] [CrossRef]
- Masia, L.; Hussain, I.; Xiloyannis, M.; Pacchierotti, C.; Cappello, L.; Malvezzi, M.; Spagnoletti, G.; Antuvan, C.W.; Binh Khanh, D.; Pozzi, M.; et al. Soft wearable assistive robotics: Exosuits and supernumerary limbs. In Wearable Exoskeleton Systems: Design, Control and Applications; Bai, S., Virk, G.S., Sugar, T.G., Eds.; IET: Stevenage, UK, 2018; pp. 219–254. [Google Scholar]
- Totaro, M.; Natali, C.D.; Bernardeschi, I.; Ortiz, J.; Beccai, L. Mechanical Sensing for Lower Limb Soft Exoskeletons: Recent Progress and Challenges. Adv. Exp. Med. Biol. 2019, 1170, 69–85. [Google Scholar]
- Chen, B.; Ma, H.; Qin, L.; Gao, F.; Chan, K.M.; Law, S.W.; Qin, L.; Liao, W.H. Recent developments and challenges of lower extremity exoskeletons. J. Orthop. Translat. 2016, 5, 26–37. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Study Quality Assessment Tools. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 1 October 2020).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Space Meets Medicine at MEDICA. 2005. Available online: http://www.esa.int/Our_Activities/Human_Spaceflight/Business/Space_meets_medicine_at_MEDICA_20052 (accessed on 19 June 2018).
- Kozlovskaya, I.; Grigoriev, A. Russian system of countermeasures on board of the International Space Station (ISS): The first results. Acta Astronaut. 2004, 55, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Ambrosini, E.; Ferrante, S.; Colombo, R. ‘Regent Suit’ training improves recovery of motor and daily living activities in subjects with subacute stroke: A randomized controlled trial. Clin. Rehabil. 2013, 27, 792–802. [Google Scholar] [CrossRef]
- Noordzij, M.; Dekker, F.W.; Zoccali, C.; Jager, K.J. Sample size calculations. Nephron. Clin. Pract. 2011, 118, c319–c323. [Google Scholar] [CrossRef] [PubMed]
- Gross, C.; Mallory, R.; Heiat, A.; Krumholz, H. Reporting the Recruitment Process in Clinical Trials: Who Are These Patients and How Did They Get There? Ann. Intern. Med. 2002, 137, 10. [Google Scholar] [CrossRef]
- Della Croce, U.; Crapanzano, F.; Li, L.; Kasi, P.K.; Patritti, B.L.; Mancinelli, C.; Hunter, D.J.; Stamenović, D.; Harvey, W.F.; Bonato, P. A Preliminary Assessment of a Novel Pneumatic Unloading Knee Brace on the Gait Mechanics of Patients with Knee Osteoarthritis. PM&R 2013, 5, 816–824. [Google Scholar]
- Harper, N.; Esposito, E.; Wilken, J.; Neptune, R. The influence of ankle-foot orthosis stiffness on walking performance in individuals with lower-limb impairments. Clin. Biomech. 2014, 29, 877–884. [Google Scholar] [CrossRef]
- Awad, L.; Kudzia, P.; Revi, D.; Ellis, T.; Walsh, C. Walking Faster and Farther With a Soft Robotic Exosuit. Implications for Post-Stroke Gait Assistance and Rehabilitation. IEEE Open J. Eng. Med. Biol. 2020, 1, 108–115. [Google Scholar] [CrossRef]
- Awad, L.; Esquenazi, A.; Francisco, G.; Nolan, K.; Jayaraman, A. The ReWalk ReStore™ soft robotic exosuit: A multi-site clinical trial of the safety, reliability, and feasibility of exosuit-augmented post-stroke gait rehabilitation. J. Neuroeng Rehabil. 2020, 17, 80. [Google Scholar] [CrossRef] [PubMed]
- Awad, L.; Bae, J.; Kudzia, P.; Long, A.; Hendron, K.; Holt, K.G.; O’Donnell, K.; Ellis, T.D.; Walsh, C.J. Reducing Circumduction and Hip Hiking During Hemiparetic Walking Through Targeted Assistance of the Paretic Limb Using a Soft Robotic Exosuit. Am. J. Phys. Med. Rehabil. 2017, 96, S157–S164. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.; Awad, L.; Long, A.; O’Donnell, K.; Hendron, K.; Holt, K.G.; Ellis, T.D.; Walsh, C.J. Biomechanical mechanisms underlying exosuit-induced improvements in walking economy after stroke. J. Exp. Biol. 2018, 221, jeb168815. [Google Scholar] [CrossRef] [PubMed]
- Boudarham, J.; Pradon, D.; Roche, N.; Bensmail, D.; Zory, R. Effects of a dynamic-ankle-foot orthosis (Liberté®) on kinematics and electromyographic activity during gait in hemiplegic patients with spastic foot equinus. NeuroRehabilitation 2014, 35, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Cudejko, T.; van der Esch, M.; van der Leeden, M.; van den Noort, J.C.; Roorda, L.D.; Lems, W.; Twisk, J.; Steultjerns, M.; Woodburn, J.; Harlaar, J.; et al. The immediate effect of a soft knee brace on pain, activity limitations, self-reported knee instability, and self-reported knee confidence in patients with knee osteoarthritis. Arthritis Res. Ther. 2017, 19, 260. [Google Scholar] [CrossRef] [PubMed]
- Daher, N.; Lee, S.; Yang, Y. Effects of elastic band orthosis (aider) on balance and gait in chronic stroke patients. Phys. Ther. Rehabil. Sci. 2013, 2, 81–86. [Google Scholar] [CrossRef][Green Version]
- Hwang, Y.; Yoo, W.; An, D. Effects of the Elastic Walking Band on gait in stroke patients. NeuroRehabilitation 2013, 32, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Sim, W.S.; Won, B.H. Effectiveness of elastic band-type ankle-foot orthoses on postural control in poststroke elderly patients as determined using combined measurement of the stability index and body weight-bearing ratio. Clin. Interv. Aging 2015, 10, 1839–1847. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kwon, J.; Park, J.; Ku, S.; Jeong, Y.; Paik, N.; Park, Y. A Soft Wearable Robotic Ankle-Foot-Orthosis for Post-Stroke Patients. IEEE Robot Autom. Lett. 2019, 4, 2547–2552. [Google Scholar] [CrossRef]
- Lee, S.; Cynn, H.; Yi, C.; Yoon, T.; Lee, J. Wearable tubing assistive walking device immediately enhances gait parameters in subjects with stroke: A randomized controlled study. NeuroRehabilitation 2017, 40, 99–107. [Google Scholar] [CrossRef]
- Schween, R.; Gehring, D.; Gollhofer, A. Immediate Effects of an Elastic Knee Sleeve on Frontal Plane Gait Biomechanics in Knee Osteoarthritis. PLoS ONE 2015, 10, e0115782. [Google Scholar] [CrossRef] [PubMed]
- Siviy, C.; Bae, J.; Baker, L.; Porciuncula, F.; Baker, T.; Ellis, T.D.; Awad, L.N.; Walsh, C.J. Offline Assistance Optimization of a Soft Exosuit for Augmenting Ankle Power of Stroke Survivors During Walking. IEEE Robot Autom. Lett. 2020, 5, 828–835. [Google Scholar] [CrossRef]
- Sloot, L.; Bae, J.; Baker, L.; O’Donnell, K.; Menard, N.; Porciuncula, F.; Choe, D.; Ellis, T.; Awad, L.; Walsh, C. O 089—A soft robotic exosuit assisting the paretic ankle in patients post-stroke: Effect on muscle activation during overground walking. Gait Posture 2018, 18, 30881–30886. [Google Scholar] [CrossRef] [PubMed]
- Sridar, S.; Qiao, Z.; Rascon, A.; Biemond, A.; Beltran, A.; Maruyama, T.; Kwasnica, C.; Polygerinos, P.; Zhang, W. Evaluating Immediate Benefits of Assisting Knee Extension With a Soft Inflatable Exosuit. IEEE Trans. Med. Robot Bionics. 2020, 2, 216–225. [Google Scholar] [CrossRef]
- Jin, X.; Prado, A.; Agrawal, S. Retraining of Human Gait—Are Lightweight Cable-Driven Leg Exoskeleton Designs Effective? IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Park, C.H. Suit-type Wearable Robot Powered by Shape-memory-alloy-based Fabric Muscle. Sci. Rep. 2019, 9, 9157. [Google Scholar] [CrossRef]
- Copaci, D.; Flores, A.; Rueda, F.; Alguacil, I.; Blanco, D.; Moreno, L. Wearable elbow exoskeleton actuated with shape memory alloy. In Converging Clinical and Engineering Research on Neurorehabilitation II; Ibáñez, J., González-Vargas, J., Azorín, J.M., Akay, M., Pons, J.L., Eds.; Springer: Berlin, Germany, 2017; pp. 477–481. [Google Scholar]
- Pishvar, M.; Harne, R. Foundations for Soft, Smart Matter by Active Mechanical Metamaterials. Adv. Sci. 2020, 7, 2001384. [Google Scholar] [CrossRef] [PubMed]
- Kos, A.; Umek, A.; Tomazic, S. Biofeedback in sport: Challenges in real-time motion tracking and processing. In Proceedings of the IEEE 15th International Conference on Bioinformatics and Bioengineering (BIBE), Belgrade, Serbia, 2–4 November 2015; pp. 1–4. [Google Scholar]
- Contreras-Vidal, J.L.; Bhagat, N.A.; Brantley, J.; Cruz-Garza, J.G.; He, Y.; Manley, Q.; Nakagome, S.; Nathan, K.; Tan, S.H.; Zhu, F.; et al. Powered exoskeletons for bipedal locomotion after spinal cord injury. J. Neural. Eng. 2016, 13, 31001. [Google Scholar] [CrossRef]
- Ferris, D.; Sawicki, G.; Daley, M. A physiologist’s perspective on robotic exoskeletons for human locomotion. Int. J. Humanoid Robot. 2007, 4, 507–528. [Google Scholar] [CrossRef]
- Di Russo, F.; Berchicci, M.; Perri, R.; Ripani, F.R.; Ripani, M. A Passive Exoskeleton Can Push Your Life Up: Application on Multiple Sclerosis Patients. PLoS ONE 2013, 8, e77348. [Google Scholar]
- Reyes, F.; Niedzwecki, C.; Gaebler-Spira, D. Technological Advancements in Cerebral Palsy Rehabilitation. Phys. Med. Rehabil. Clin. 2020, 31, 117–129. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Eguren, D.; Luu, T.; Contreras-Vidal, J. Risk management and regulations for lower limb medical exoskeletons: A review. Med. Devices 2017, 10, 89–107. [Google Scholar] [CrossRef] [PubMed]
- Gaitrite. Available online: https://www.gaitrite.com/ (accessed on 4 June 2019).
- Microgate OptoGait. Available online: http://www.optogait.com/ (accessed on 17 October 2020).
- Younger, J.; McCue, R.; Mackey, S. Pain outcomes: A brief review of instruments and techniques. Curr. Pain Headache Rep. 2009, 13, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Allen, D. Validity and Reliability of the Movement Ability Measure: A Self-Report Instrument Proposed for Assessing Movement Across Diagnoses and Ability Levels. Phys. Ther. 2007, 87, 899–916. [Google Scholar] [CrossRef] [PubMed]
- Shore, L.; Power, V.; Hartigan, B.; Schülein, S.; Graf, E.; de Eyto, A.; O’Sullivan, L. Exoscore: A Design Tool to Evaluate Factors Associated With Technology Acceptance of Soft Lower Limb Exosuits by Older Adults. Human Factors 2019, 62, 391–410. [Google Scholar] [CrossRef]
- Yandell, M.; Ziemnicki, D.; McDonald, K.; Zelik, K. Characterizing the comfort limits of forces applied to the shoulders, thigh and shank to inform exosuit design. PLoS ONE 2020, 15, e0228536. [Google Scholar] [CrossRef]
- Kermavnar, T.; O’Sullivan, K.; Casey, V.; de Eyto, A.; O’Sullivan, L. Circumferential tissue compression at the lower limb during walking, and its effect on discomfort, pain and tissue oxygenation: Application to soft exoskeleton design. Appl. Ergon. 2020, 86, 103093. [Google Scholar] [CrossRef]
- Haufe, F.; Kober, A.; Schmidt, K.; Sancho-Puchades, A.; Duarte, J.E.; Wolf, P.; Riener, R. User-driven walking assistance: First experimental results using the MyoSuit. In Proceedings of the IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 944–949. [Google Scholar]
- Riemann, B.; Lephart, S. The Sensorimotor System, Part II: The Role of Proprioception in Motor Control and Functional Joint Stability. J. Athl. Train. 2002, 37, 80–84. [Google Scholar]
- Aman, J.; Elangovan, N.; Yeh, I.; Konczak, J. The effectiveness of proprioceptive training for improving motor function: A systematic review. Front. Hum. Neurosci. 2015, 8, 1075. [Google Scholar] [CrossRef]
| Articles Were Scanned for the Following Information: |
|---|
| Year of publication |
| Body part, articulations addressed |
| Power type used for the exosuit (active or passive) |
| Weight of the exosuit |
| Tethered or untethered use |
| Actuator type for moving the exosuit |
| Type of force transmission on body |
| Type of sensors used for control and technological evaluation |
| Control scheme applied |
| Evaluation methods and tasks performed for evaluation |
| Technological results |
| Clinical results |
| Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies: |
|---|
| 1. Was the research question or objective in this paper clearly stated? |
| 2. Was the study population clearly specified and defined? |
| 3. Was the participation rate of eligible persons at least 50%? |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
| 5. Were sample size justification, power description, or variance and effect estimates provided? |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as a continuous variable)? |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable and implemented consistently across all study participants? |
| 10. Was the exposure(s) assessed more than once over time? |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable and implemented consistently across all study participants? |
| 12. Were the outcome assessors blinded to the exposure status of participants? |
| 13. Was loss to follow-up after baseline 20% or less? |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
| ID | Year | Articulations | Power Type | Weight | Tethered (T)/ Untethered (U) | Actuators | Type of Force Transmission on Body | Sensor Types/Application | Control Scheme * |
|---|---|---|---|---|---|---|---|---|---|
| Awad et al. [29] | 2020 | Ankle | Active | 5 kg | U | Electric | Bowden cables | Gyroscope, load cells/Identify gait events (foot-mounted gyroscope). Monitor and adjust applied force on Bowden cables (load cells). | A |
| Awad et al. [28] | 2020 | Ankle | Active | <5 kg | U | Electric | Bowden cables | Gyroscope, load cells/Identify gait events (foot-mounted gyroscope). Monitor and adjust applied force on Bowden cables (load cells). | A |
| Awad et al. [30] | 2017 | Ankle | Active | 0.9 kg | T | Electric | Bowden cables | Gyroscope, load cells/Identify gait events (foot-mounted gyroscope). Monitor and adjust applied force on Bowden cables (load cells). | A |
| Awad et al. [8] | 2017 | Ankle | Active | 0.9 kg (Tethered)/ 3.19 kg (Untethered) | U | Electric | Bowden cables | Gyroscope, load cells/Identify gait events (foot-mounted gyroscope). Monitor and adjust applied force on Bowden cables (load cells). | A |
| Bae et al. [31] | 2018 | Hip, Ankle | Active | 0.9 kg | T | Electric | Bowden cables | Gyroscope, load cells/Identify ground contact events (foot-mounted gyroscope). Monitor and adjust applied force on Bowden cables (load cells). | A |
| Boudarhan et al. [32] | 2014 | Ankle | Passive | - | U | - | Elastic material | - | N |
| Cudejko et al. [33] | 2017 | Knee | Passive | - | U | - | Elastic material | - | N |
| Daher et al. [34] | 2013 | Ankle | Passive | - | U | - | Elastic material | - | N |
| Della Croce et al. [26] | 2013 | Knee | Passive | - | U | Pneumatic | Air bladder | - | N |
| Harper et al. [27] | 2014 | Ankle | Passive | - | U | - | Leaf spring | - | N |
| Hwang et al. [35] | 2013 | Hip, Knee Ankle | Passive | - | U | - | Elastic material | - | N |
| Kim et al. [36] | 2015 | Ankle | Passive | - | U | - | Elastic material | - | N |
| Kwon et al. [37] | 2019 | Ankle | Active | 1.54 kg | U | Electric | Bowden cables | Inertial measurement unit (IMU), strain sensors, force sensitive resistors (FSRs)/Detection of gait phase via foot–ground contact events (FSRs). Measurement of knee and ankle angle (strain sensors), and shank angle (IMU). | A |
| Lee et al. [38] | 2016 | Knee, Ankle | Passive | - | U | - | Elastic material | - | N |
| Monticone et al. [23] | 2013 | Hip, Knee Ankle | Passive | - | U | - | Elastic material | - | N |
| Schween et al. [39] | 2015 | Knee | Passive | - | U | - | Elastic material | - | N |
| Siviy et al. [40] | 2020 | Ankle | Active | 4.932 kg | U | Electric | Bowden cables | IMUs, load cells/Identify gait events by foot and shank movement (IMUs). Monitor and adjust applied force on Bowden cables (load cells) to match force profile. | A |
| Sloot et al. [41] | 2018 | Ankle | Active | 2 kg | U | Electric | Bowden cables | Gyroscope, load cells/Identify gait events (foot-mounted gyroscope). Monitor and adjust applied force on Bowden cables (load cells). | A |
| Sridar et al. [42] | 2020 | Knee | Active | 0.26 kg | T | Pneumatic | Inflatable structure | Pressure sensor, shoe insole sensor/Detect gait phase via ground reaction forces (shoe insole sensor). Monitor and control actuator pressure (pressure sensor). | A |
| ID | Impairment | No. of Patients | Age (Years) | Height (m) | Weight (kg) | Task | Evaluation Type |
|---|---|---|---|---|---|---|---|
| Awad et al. [29] | Stroke | 44 | 27–72 | 1.60–1.88 | 51.2–113.3 | Treadmill walk, overground walk | Frequency of adverse events, injuries and device malfunctions, custom questionnaires, walking speed |
| Awad et al. [28] | Stroke | 6 | 52 ± 10 | - | - | 10 MWT, 6-min overground walk | Walking speed, distance, indirect calorimetry |
| Awad et al. [30] | Stroke | 8 | 30–67 | . | - | 10 MWT | Motion capture |
| Awad et al. [8] | Stroke | 9 | 30–67 | . | - | 10 MWT | Motion capture, indirect calorimetry |
| Bae et al. [31] | Stroke | 7 | 30–56 | 1.62–1.86 | 49.4–89.7 | 8-min walk on treadmill | Motion capture, indirect calorimetry, ground reaction force |
| Boudarhan et al. [32] | Stroke | 12 | 51 ± 16 | 1.71 ± 0.1 | 72 ± 14 | 10 MWT | Motion capture, EMG |
| Cudejko et al. [33] | Osteoarthritis | 44 | 65.7 ± 9.3 | - | - | 10 MWT, GUG test, perturbed and level walk on treadmill | Self-report knee pain, number of knee instability episodes, perceived knee confidence |
| Daher et al. [34] | Stroke | 10 | 56.8 ± 13.51 | - | - | Walk, balance test and sit-to-stand test | Timed up and go test, Berg Balance Scale, Optogait System |
| Della Croce et al. [26] | Osteoarthritis | 18 | 68 ± 9 | 1.73 ± 0.07 | 86.1 ± 14.2 | 12-m walk | Motion capture, ground reaction force |
| Harper et al. [27] | Trauma | 13 | 29.4 ± 5.8 | 1.8 ± 0.08 | 88.2 ± 10.8 | Walk at self-selected velocity and Froude velocity | EMG, ground reaction force, audio cues for speed feedback, motion capture |
| Hwang et al. [35] | Stroke | 15 | 36–70 | 1.53–1.75 | 83–46.6 | 10 MWT | GAITrite system |
| Kim et al. [36] | Stroke | 10 | 55.7 ± 8.43 | 1.67 ± 0.0654 | 67.8 ± 11.66 | Balance test under three experimental conditions | Biodex Balance System, plantar foot pressure system |
| Kwon et al. [37] | Stroke | 1 | 48 | - | - | Overground walk | Motion capture, ground reaction force, Fugl-Meyer assessment |
| Lee et al. [38] | Stroke | 23 | 37–66 | 1.48–1.78 | 31–90 | 10 MWT | GAITrite pressure mat |
| Monticone et al. [23] | Stroke | 30 | 60.2 ± 6.1 | - | - | 6-min walk test, balance test, Functional Independence Measure, Barthel Index | Oxygen saturation, heart rate, GAITrite system, Berg Balance Scale |
| Schween et al. [39] | Osteoarthritis | 18 | 50 ± 9 (women) 55 ± 7 (men) | 1.66 ± 0.06 (women) 1.81 ± 0.08 (men) | 62 ± 6 (women) 87 ± 16 (men) | 10 MWT | Ground reaction force, walking speed by light barriers, questionnaire, motion capture |
| Siviy et al. [40] | Stroke | 6 | 33–62 | - | 43.9–101.8 | 3-min walk on treadmill | Ground reaction force, EMG, motion capture |
| Sloot et al. [41] | Stroke | 8 | - | - | - | 5-min walk on treadmill | EMG |
| Sridar et al. [42] | Stroke | 3 | 58–74 | 1.65–1.85 | 59.2–83.6 | Treadmill walk, TUG | Ground reaction force, EMG, motion capture |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koch, M.A.; Font-Llagunes, J.M. Lower-Limb Exosuits for Rehabilitation or Assistance of Human Movement: A Systematic Review. Appl. Sci. 2021, 11, 8743. https://doi.org/10.3390/app11188743
Koch MA, Font-Llagunes JM. Lower-Limb Exosuits for Rehabilitation or Assistance of Human Movement: A Systematic Review. Applied Sciences. 2021; 11(18):8743. https://doi.org/10.3390/app11188743
Chicago/Turabian StyleKoch, Martin Andreas, and Josep M. Font-Llagunes. 2021. "Lower-Limb Exosuits for Rehabilitation or Assistance of Human Movement: A Systematic Review" Applied Sciences 11, no. 18: 8743. https://doi.org/10.3390/app11188743
APA StyleKoch, M. A., & Font-Llagunes, J. M. (2021). Lower-Limb Exosuits for Rehabilitation or Assistance of Human Movement: A Systematic Review. Applied Sciences, 11(18), 8743. https://doi.org/10.3390/app11188743






