Abstract
Temporary anchorage devices (TADs) allow molar intrusion as an additional treatment option to conventional treatment for open bite cases. We investigated the treatment option criteria for open bite treatment. A total of 33 patients with skeletal Class I to Class II open bite who had stable occlusion one year after treatment were enrolled in the study, including 15 patients who had undergone surgical orthodontic treatment, 8 patients who had undergone treatment with molar intrusion, and 10 patients who had undergone treatment with anterior teeth extrusion. Pre-treatment cephalometric analysis of these patients was used for comparison. Furthermore, receiver operating characteristic (ROC) curve analysis was employed to examine the measurement parameters that would be valid as treatment criteria. In the results, FMA showed that patients treated with molar intrusion had a moderately high angle, while those treated with surgical orthodontic treatment had a severe high angle. The area under the curve (AUC) of the ROC curve indicated that FMA is the most appropriate parameter for treatment option criteria. In addition, the cutoff value indicated that the borderline between molar intrusion and surgical orthodontic treatment was 37.5° for FMA. In this study, we suggested criteria for the treatment of open bite with molar intrusion.
1. Introduction
Open bite is considered to be one of the most difficult malocclusions in orthodontic treatment; therefore, in open bite cases, decision of treatment method, mechanics, and maintenance have been the topic of focus [1,2,3,4,5]. This is due to the fact that open bite can be associated with many complex problems such as TMD and tongue habits, which make treatment and maintenance difficult. In addition, the approach to open bite varies depending on skeletal type and dental type [6].
Conventionally, skeletal open bite has been corrected by surgically repositioning the maxilla or mandible [7] (Figure 1), and dental open bite by extruding the anterior teeth [8,9] (Figure 2). In recent years, however, the use of temporary anchorage devices (TADs) in orthodontics has changed the treatment of open bite cases—specifically, intruding the molars using TADs to rotate the mandible counterclockwise and improving open bite [10,11,12] (Figure 3). This treatment method has been reported in many cases and has shown good results and long-term stability [1,13,14]. Therefore, molar intrusion has been established as one of the treatment methods for open bite cases.
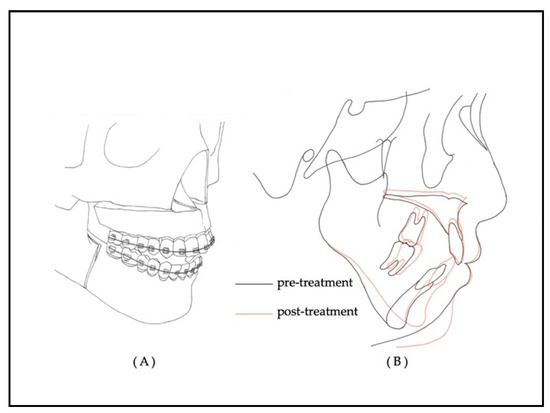
Figure 1.
A schema of surgical orthodontic treatment. (A) Orthognathic surgery; Le Fort 1 osteotomy and sagittal split ramus osteotomy. (B) Superimposition of cephalometric trace changes pre- and post-treatment.
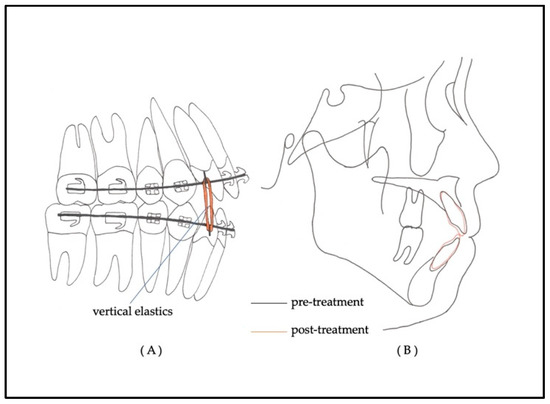
Figure 2.
(A) A schema of orthodontic treatment of open bite with extruding anterior teeth using a multi-bracket appliance system and vertical elastics. (B) Superimposition of cephalometric trace pre- and post-treatment.
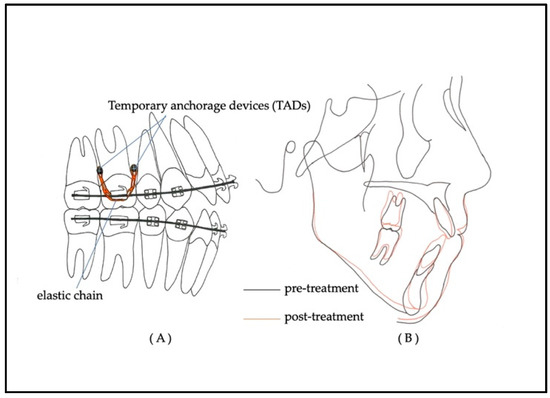
Figure 3.
(A) A schema of orthodontic treatment of open bite with intruding molars using a multi-bracket appliance system and TADs. (B) Superimposition of cephalometric trace changes pre- and post-treatment.
In orthognathic surgery for skeletal open bite, only the mandible is positioned anteriorly and upward to the occlusal plane of the maxillary dentition, or the mandible is positioned anteriorly and upward with counterclockwise rotation by impacting the posterior region of the maxilla [15]. In other words, surgical orthodontic treatment reduces the lower facial height and surgically improves the vertical skeletal discrepancy. Therefore, this new treatment approach involving molar intrusion has been reported as a treatment method for skeletal open bite cases, mainly because it improves open bite by the same mechanism as surgical orthodontic treatment [16].
However, not all cases of skeletal open bite have been treated with molar intrusion, and there have been no reports on the criteria for the use of TADs in molar intrusion. Kamiyama et al. classified the structure of open bite into low position of anterior teeth, high position of molars, and vertical skeletal disharmony [17]. However, the main cephalometric assess points that determine the treatment strategy are unclear, and a comprehensive assessment is required to diagnose and make a decision on the treatment plan. In this study, we will report the treatment strategy for open bite cases by mainly examining the criteria for the indication of molar intrusion treatment as a retrospective study.
2. Materials and Methods
The subjects were 33 patients with open bite who visited the Tokyo Dental College Chiba Dental Center between 2012 and 2018. Criteria were defined to include cases that ended active treatment 1 year before, at which point the patients had overbite change within 1 mm and a positive overbite. The patients used a circumferential-type retainer after treatment. In addition, prior to treatment, ANB was more than 3.0°, overbite was less than −2 mm, and deviation of menton from the mid-facial line was less than 2 mm as measured by the frontal cephalogram. Exclusion criteria were patients with severe tongue thrust, TMJ symptoms, especially progressive condylar resorption, and congenital abnormality such as craniofacial syndrome, cleft lip palate, and so on. Surgical orthodontic treatment was applied to 15 patients (Group S), and orthodontic treatment was applied to 18 patients, of which 8 cases underwent extrusion of anterior teeth (Group E) and 10 cases underwent intrusion of molars (Group I; Table 1). All cases were diagnosed, treated, and selected by six orthodontic specialists with more than 10 years of experience.

Table 1.
Patients’ characteristics.
Measurements were made using a cephalometric radiograph and dental models of these subjects. Vertical and anterior–posterior measurements of skeletal and denture pattern in the cephalometric analysis were conducted, and overjet and overbite in the dental model analysis were measured. ANB and Wits appraisal were used for cephalometric anterior–posterior evaluation, while FMA, lower facial height, and palatal plane were used for vertical evaluation, which indicates the skeletal type (Figure 4 and Figure 5).
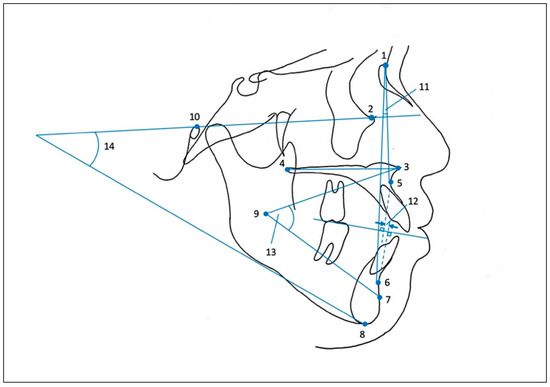
Figure 4.
Cephalometric measurements (skeletal pattern). 1: nasion; 2: orbitale; 3: anterior nasal spine (ANS); 4: posterior nasal spine (PNS); 5: point A; 6: point B; 7: PM; 8: menton; 9: xi; 10: porion; 11: ANB angle; 12: Wits appraisal; 13: lower facial height; 14: mandibular plane angle (FMA). Palatal plane angle: the angle between the palatal plane connecting ANS and PNS and the Frankfort plane.
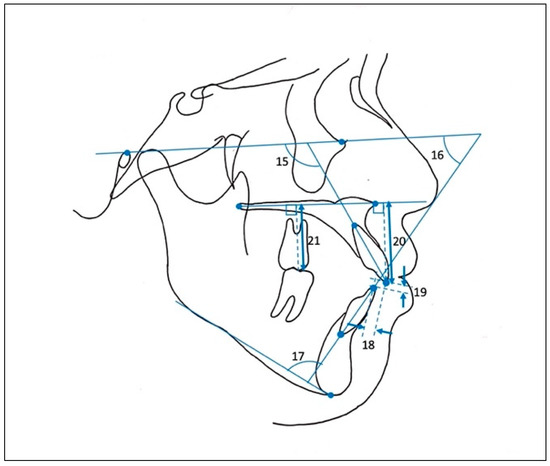
Figure 5.
Cephalometric measurements (denture pattern). 15: U1 to FH plane angle (U1 to FH); 16: Frankfort mandibular incisor angle (FMIA); 17: incisor mandibular plane angle (IMPA); 18: overjet; 19: overbite; 20: upper incisor height; 21: upper molar height.
All measurements were taken manually by the same single researcher. Any measurement errors were re-measured by the researcher after a one-week interval. These measurements were compared between the three groups by one-way ANOVA and Tukey’s analysis.
The measured items that showed significant difference (p < 0.05) among the three groups were selected to perform receiver operating characteristic (ROC) analysis, and the area under the curve (AUC) of the ROC curve was used to determine appropriate cephalometric parameters for the decision of treatment—specifically, deciding between extruding anterior teeth or intruding molars, or between intruding molars or adopting surgical orthodontic treatment. The treatment option criteria were also examined based on the cutoff point, which is the best combination of specificity and sensitivity.
The sample size was calculated using the mean and standard deviation of the pre-treatment mandibular plane angle for each group from our preliminary study, which consisted of 20 subjects, with an alpha error of 80% and a beta error of 20%, requiring 7 patients in each group.
All statistical analysis was performed using the statistical software SPSS (ver. 25.0; IBM, Armonk, NY, USA).
3. Results and Discussion
3.1. Comparison of the Mean Value of Pre-Treatment Measurements in the Three Groups
There was a significant difference in FMA between Group S and Group I and between Group S and Group E. Lower facial height also showed a significant difference between Group S and Group E (Table 2). Since the Japanese standard value for FMA is approximately 25° and that for lower facial height is roughly 49° [18], all of these items show extremely large values in Group E and Group I and values slightly larger than the standard in Group E. The larger the values, the longer the skeletal vertical length is, indicating a high-angle case. Furthermore, there were significant differences in upper molar height (UM height) and upper incisor height (UI height) between the groups.

Table 2.
Comparison of pre-treatment mean values among the three groups.
It has been reported that skeletal open bites are characterized by a downward growth of the mandible with a steep mandibular plane angle and a dentoalveolar development of the maxilla [19,20]. The results of this study agree with this finding and show that those with skeletal vertical problems have a particularly high upper molar height [21]. The results suggest that in cases with severe vertical skeletal problems, surgery is used to reduce posterior elongation, as is molar intrusion. However, it has been reported that the amount of molar intrusion in cases with stable post-treatment is limited to about 2–3 mm [22,23]. Therefore, the treatment of molar intrusion would be applied to moderate skeletal problems.
ANB tended to be larger in Group S and Group I. This suggests that these cases displayed not only anterior–posterior problems but also vertical problems involving mandibular retrusion, i.e., clockwise rotation of the mandible with a steep mandibular plane [24,25]. In such cases, orthognathic surgery can be used to impact the posterior dentition, and molar intrusion can achieve counterclockwise rotation of the mandible [2]. This advances the mandible and improves the aesthetics of the lateral profile.
The overbite, which measures the vertical relationship of the anterior teeth, did not show significant difference among the three groups. This showed that it was not an indicator of whether the case was skeletal or dental and is not very relevant in treatment planning.
3.2. Discrimination of the Optimal Cephalometric Analysis Items to Be Used as Selection Criteria for the Three Treatment Plans
ROC analysis is known to be a useful analysis for comparing diagnostic capabilities. The diagnostic ability is mainly evaluated by the area under the ROC curve, and the further upward and left value on this curve is taken as the cutoff point and used as the diagnostic reference value. It has been widely used in the medical and dental fields and also in orthodontics [26,27].
Based on the results of Table 2, FMA, UM height, and UI height, which have p-values less than 0.05 and are appropriate as vertical indicators, were selected using ROC analysis. Table 3 shows that the AUC values of the ROC curves for Group S and Group I are the highest in FMA (Figure 6a). This indicates that FMA has better diagnostic accuracy in determining whether orthognathic surgery or molar intrusion is required. On the other hand, UM height and UI height have low AUC and are less reliable as criteria for open bite treatment (Figure 6b,c). The measurement of tooth height was considered to be biased because of the measurement errors that may occur on the cephalometric film where the left and right sides overlap and also because of individual differences in tooth size and length. In other words, these measurements are not suitable enough as a criterion for the diagnosis of open bite.

Table 3.
Results of the ROC curve analysis for Group S and Group I.
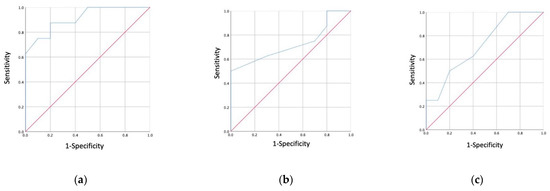
Figure 6.
(a) The ROC curve of FMA measurement (between molar intrusion treatment and surgical orthodontic treatment); (b) the ROC curve of upper molar height measurement (between molar intrusion treatment and surgical orthodontic treatment); (c) the ROC curve of upper incisor height measurement (between molar intrusion treatment and surgical orthodontic treatment).
Table 4 also showed the highest AUC value for FMA (Figure 7a), but the value was lower than that of the results in Table 3. The AUC values for UM height and UI height were low (Figure 7b,c), as shown in Table 3. These results suggest that the borderline between orthognathic surgery and molar intrusion is clearer than the borderline between molar intrusion and anterior tooth extrusion.

Table 4.
Results of the ROC curve analysis for Group I and Group E.
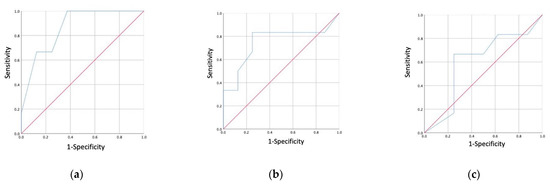
Figure 7.
(a) The ROC curve of FMA measurement (between anterior teeth extrusion and molar intrusion); (b) the ROC curve of upper molar height measurement (between anterior teeth extrusion and molar intrusion); (c) the ROC curve of upper incisor height measurement (between anterior teeth extrusion and molar intrusion).
The cutoff point was determined as the value with the highest sensitivity and specificity. Table 3 shows that the borderline between the indications of orthognathic surgery and molar intrusion in FMA is 37.5°. This value seems to be extremely high, but this is due to the data consisting only of Japanese data. It is reported that the cephalometric norms of Japanese are characterized by mandibular retrusion, labial inclination of mandibular anterior teeth, steep mandibular plane, etc., compared to those of Caucasians, and generally tend to be high-angle facial type [28], explaining why the FMA in this study showed high values. This FMA value is regarded as reliable because it shows high sensitivity and specificity. On the other hand, the FMA showed a cutoff point of 30.0° as the borderline between molar intrusion and anterior tooth extrusion. This value has low sensitivity and specificity and is considered to be less reliable. This is due to molar intrusion being used for skeletal open bite cases as a method to avoid surgery [29], and the borderline between orthognathic surgery and molar intrusion becomes clearer, while the borderline between molar intrusion and anterior teeth extrusion remains unclear.
3.3. Study Limitations
The case selection for this study was from patients with ANB of more than 3°. In other words, we restricted the study to skeletal Class I or II and excluded Class III patients, on the grounds that molar intrusion is unsuitable for skeletal Class III treatment [30]. Patients with normal mandibular body length would present skeletal Class I and II malocclusions, while those with anterior–posterior disharmony display skeletal Class III malocclusion. Thus, the results of this study do not apply to skeletal Class III patients.
In addition, the sample size in this study satisfied the calculation, although it was less than that of similar studies. This may be due to the small sample size of the preliminary study used in the power analysis.
In our treatment, the method of molar intrusion using skeletal anchorage is not standardized—cases vary in having TADs implanted in the buccal alveolar region or palate. In addition, even with molar intrusion, some percentage of the amount of improvement in overbite may also result in anterior tooth extrusion, which is considered a limitation of this study.
This study consisted of cases with stability one year after active treatment. Baek et al. reported a three-year follow-up in open bite molar intrusion cases. According to their study, 80% of the amount of molar relapse occurred in the first year [1]. Therefore, we set the follow-up period to one year, but a longer follow-up period is desirable as a future research prospect.
4. Conclusions
In this study, we suggested criteria for the treatment of open bite with molar intrusion. However, the diagnosis of open bite requires further careful consideration of treatment selection as there are many factors such as TMD and oral habits, and the diagnostic criteria need to be discussed with regard to long-term stability.
Author Contributions
Conceptualization, C.T. and Y.N.; methodology, Y.N.; validation, Y.N., M.Y.; formal analysis, C.T.; investigation, C.T.; data curation, C.T.; writing—original draft preparation, C.T.; writing—review and editing, Y.N., T.T., and M.Y.; visualization, C.T.; supervision, Y.N.; project administration, Y.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study protocol was approved by the Tokyo Dental College Ethics Committee (Approval No. 944).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Baek, M.S.; Choi, Y.J.; Yu, H.S.; Lee, K.J.; Kwak, J.; Park, Y.C. Long-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior Teeth. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 396.e1–396.e9. [Google Scholar] [CrossRef]
- Reichert, I.; Figel, P.; Winchester, L. Orthodontic Treatment of Anterior Open Bite: A Review Article—Is Surgery Always Necessary? Oral Maxillofac. Surg. 2014, 18, 271–277. [Google Scholar] [CrossRef]
- Greenlee, G.M.; Huang, G.J.; Chen, S.S.H.; Chen, J.; Koepsell, T.; Hujoel, P. Stability of Treatment for Anterior Open-Bite Malocclusion: A Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 154–169. [Google Scholar] [CrossRef]
- De Freitas, M.R.; Beltrão, R.T.S.; Janson, G.; Henriques, J.F.C.; Cançado, R.H. Long-Term Stability of Anterior Open Bite Extraction Treatment in the Permanent Dentition. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 78–87. [Google Scholar] [CrossRef]
- Kim, Y.H.; Han, U.K.; Lim, D.D.; Serraon, M.L.P. Stability of Anterior Openbite Correction with Multiloop Edgewise Archwire Therapy: A Cephalometric Follow-up Study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 43–54. [Google Scholar] [CrossRef] [Green Version]
- Jung, S.K.; Kim, T.W. The Relevance Analysis of Hyoid Bone Position to Skeletal or Dental Openbite and Dentofacial Characteristics. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 528–533. [Google Scholar] [CrossRef]
- Proffit, W.R.; Bailey, L.J.; Phillips, C.; Turvey, T.A. Long-Term Stability of Surgical Open-Bite Correction by Le Fort I Osteotomy. Angle Orthod. 2000, 70, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Gavito, G.; Wallen, T.R.; Little, R.M.; Joondeph, D.R. Anterior Open-Bite Malocclusion: A Longitudinal 10-Year Postretention Evaluation of Orthodontically Treated Patients. Am. J. Orthod. 1985, 87, 175–186. [Google Scholar] [CrossRef]
- Küçükkeleş, N.; Acar, A.; Demirkaya, A.A.; Evrenol, B.; Enacar, A. Cephalometric Evaluation of Open Bite Treatment with NiTi Arch Wires and Anterior Elastics. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 555–562. [Google Scholar] [CrossRef]
- Umemori, M.; Sugawara, J. Skeletal Anchorage System for Open-Bite Correction. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 166–174. [Google Scholar]
- Sherwood, K.H.; Burch, J.G.; Thompson, W.J. Closing Anterior Open Bites by Intruding Molars with Titanium Miniplate Anchorage. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 593–600. [Google Scholar] [CrossRef]
- Erverdi, N.; Keles, A.; Nanda, R. The Use of Skeletal Anchorage in Open Bite Treatment: A Cephalometric Evaluation. Angle Orthod. 2004, 74, 381–390. [Google Scholar] [CrossRef] [PubMed]
- González Espinosa, D.; de Oliveira Moreira, P.E.; da Sousa, A.S.; Flores-Mir, C.; Normando, D. Stability of Anterior Open Bite Treatment with Molar Intrusion Using Skeletal Anchorage: A Systematic Review and Meta-Analysis. Prog. Orthod. 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, J.; Baik, U.B.; Umemori, M.; Takahashi, I.; Nagasaka, H.; Kawamura, H.; Mitani, H. Treatment and Posttreatment Dentoalveolar Changes Following Intrusion of Mandibular Molars with Application of a Skeletal Anchorage System (SAS) for Open Bite Correction. Int. J. Adult Orthodon. Orthognath. Surg. 2002, 17, 243–253. [Google Scholar]
- Hoppenreijs, T.J.M.; Freihofer, H.P.M.; Stoelinga, P.J.W.; Tuinzing, D.B.; Van’t Hof, M.A.; Van Der Linden, F.P.G.M.; Nottet, S.J.A.M. Skeletal and Dento-Alveolar Stability of Le Fort I Intrusion Osteotomies and Bimaxillary Osteotomies in Anterior Open Bite Deformities: A Retrospective Three-Centre Study. Int. J. Oral Maxillofac. Surg. 1997, 26, 161–175. [Google Scholar] [CrossRef]
- Kuroda, S.; Sakai, Y.; Tamamura, N.; Deguchi, T.; Takano-Yamamoto, T. Treatment of Severe Anterior Open Bite with Skeletal Anchorage in Adults: Comparison with Orthognathic Surgery Outcomes. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Kamiyama, T.; Takiguti, H. Roentgeno-Cephalometric Analysis of Open Bite. J. Jpn. Orthod. Soc. 1958, 17, 31–40. [Google Scholar]
- Alcalde, R.E.; Jinno, T.; Pogrel, M.A.; Matsumura, T. Cephalometric Norms in Japanese Adults. J. Oral Maxillofac. Surg. 1998, 56, 129–134. [Google Scholar] [CrossRef]
- Subtelny, J.D.; Sakuda, M. Open-Bite: Diagnosis and Treatment. Am. J. Orthod. 1964, 50, 337–358. [Google Scholar] [CrossRef]
- Nahoum, H.I. Vertical Proportions and the Palatal Plane in Anterior Open-Bite. Am. J. Orthod. 1971, 59, 273–282. [Google Scholar] [CrossRef]
- Kucera, J.; Marek, I.; Tycova, H.; Baccetti, T. Molar Height and Dentoalveolar Compensation in Adult Subjects with Skeletal Open Bite. Angle Orthod. 2011, 81, 564–569. [Google Scholar] [CrossRef]
- Alsafadi, A.S.; Alabdullah, M.M.; Saltaji, H.; Abdo, A.; Youssef, M. Effect of Molar Intrusion with Temporary Anchorage Devices in Patients with Anterior Open Bite: A Systematic Review. Prog. Orthod. 2016, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheffler, N.R.; Proffit, W.R.; Phillips, C. Outcomes and Stability in Patients with Anterior Open Bite and Long Anterior Face Height Treated with Temporary Anchorage Devices and a Maxillary Intrusion Splint. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 594–602. [Google Scholar] [CrossRef] [Green Version]
- Epker, B.N. Surgical-Orthodontic Collection of Openbite Deformity. Angle Orthod. 1977, 71, 278–299. [Google Scholar] [CrossRef]
- Saltaji, H.; Flores-Mir, C.; Major, P.W.; Youssef, M. The Relationship between Vertical Facial Morphology and Overjet in Untreated Class II Subjects. Angle Orthod. 2012, 82, 432–440. [Google Scholar] [CrossRef] [Green Version]
- Han, U.K.; Kim, Y.H. Determination of Class II and Class III Skeletal Patterns: Receiver Operating Characteristic (ROC) Analysis on Various Cephalometric Measurements. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 538–545. [Google Scholar] [CrossRef]
- Wardlaw, D.W.; Smith, R.J.; Hertweck, D.W.; Hildebolt, C.F. Cephalometrics of Anterior Open Bite: A Receiver Operating Characteristic (ROC) Analysis. Am. J. Orthod. Dentofac. Orthop. 1992, 101, 234–243. [Google Scholar] [CrossRef]
- Ioi, H.; Nakata, S.; Nakasima, A.; Counts, A.L. Comparison of Cephalometric Norms between Japanese and Caucasian Adults in Antero-Posterior and Vertical Dimension. Eur. J. Orthod. 2007, 29, 493–499. [Google Scholar] [CrossRef] [Green Version]
- Kuroda, S.; Katayama, A.; Takano-Yamamoto, T. Severe Anterior Open-Bite Case Treated Using Titanium Screw Anchorage. Angle Orthod. 2004, 74, 558–567. [Google Scholar] [CrossRef]
- Akbaydogan, L.C.; Akin, M. Cephalometric Evaluation of Intrusion of Maxillary Posterior Teeth by Miniscrews in the Treatment of Open Bite. Am. J. Orthod. Dentofac. Orthop. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).