Current Imaging Evaluation of Tumor Response to Advanced Medical Treatment in Metastatic Renal-Cell Carcinoma: Clinical Implications
Abstract
:1. Introduction
2. Advanced Medical Treatments in Metastatic RCC: Mechanisms of Action
3. Imaging Evaluation of Therapy Response in Metastatic RCC
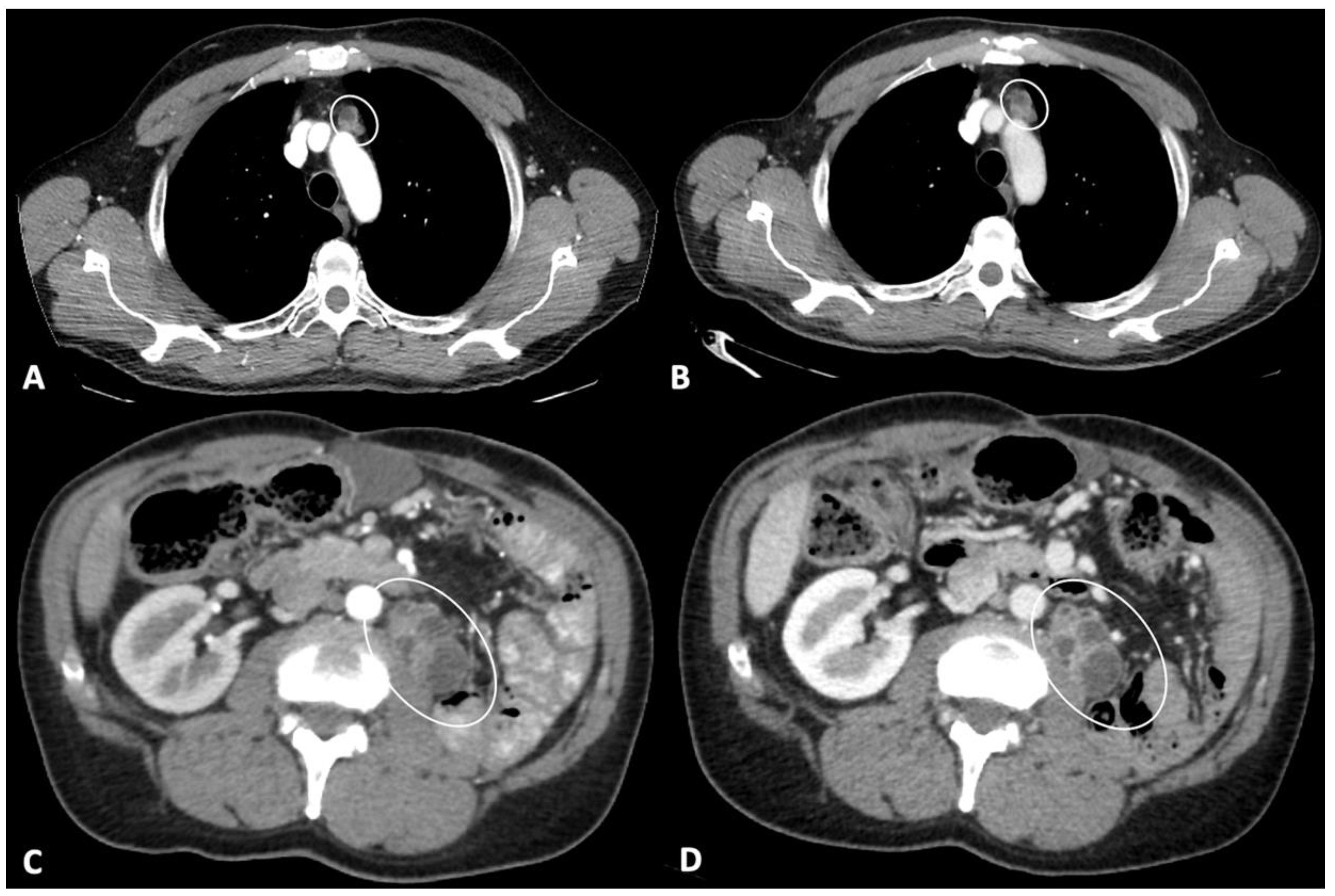
3.1. Antiangiogenic Therapies
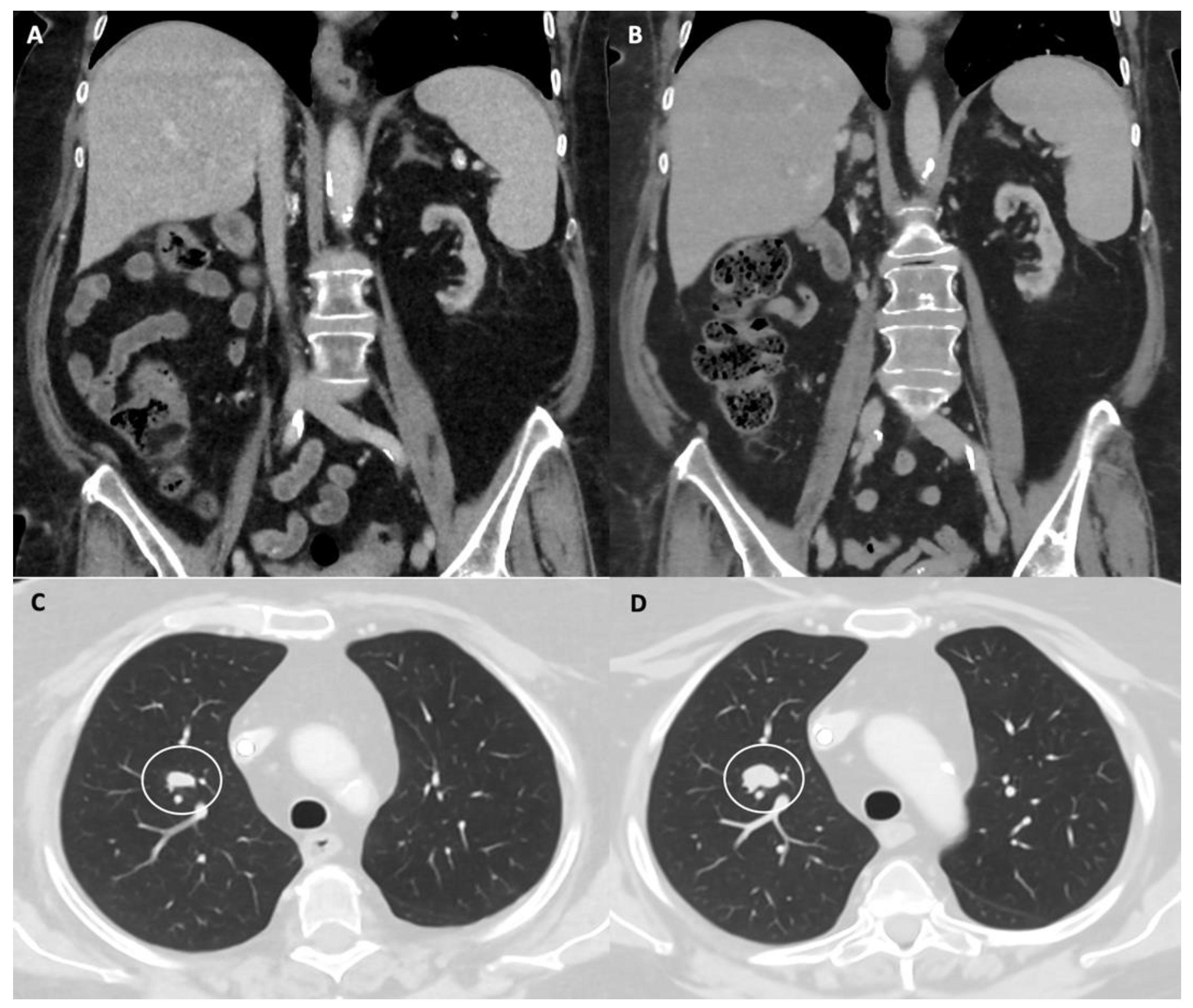
3.2. Immune Checkpoint Inhibitors
3.3. Combined Treatment Using Antiangiogenic and ICIs Drugs
4. Prognostic Evaluation in Metastatic RCC Using Antiangiogenic Therapies
5. Prognostic Evaluation in Metastatic RCC Using Immune Checkpoint Inhibitors
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Padala, S.A.; Barsouk, A.; Thandra, K.C.; Saginala, K.; Mohammed, A.; Vakiti, A.; Rawla, P.; Barsouk, A. Epidemiology of renal cell carcinoma. World J. Oncol. 2020, 11, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Silverman, S.G.; Israel, G.M.; Herts, B.R.; Richie, J.P. Management of the incidental renal mass 1. Radiology 2008, 249, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, J.J.; Purdue, M.P.; Signoretti, S.; Swanton, C.; Albiges, L.; Schmidinger, M.; Heng, D.Y.; Larkin, J.; Ficarra, V. Renal cell carcinoma. Nat. Rev. Dis. Prim. 2017, 3, 17009. [Google Scholar] [CrossRef]
- Janzen, N.K.; Kim, H.L.; Figlin, R.A.; Belldegrun, A.S. Surveillance after radical or partial nephrectomy for localized renal cell carcinoma and management of recurrent disease. Urol. Clin. N. Am. 2003, 30, 843–852. [Google Scholar] [CrossRef]
- Brufau, B.P.; Cerqueda, C.S.; Villalba, L.B.; Izquierdo, R.S.; González, B.M.; Molina, C.N. Metastatic renal cell carcinoma: Radiologic findings and assessment of response to targeted antiangiogenic therapy by using multidetector CT. Radiographics 2013, 33, 1691–1716. [Google Scholar] [CrossRef] [Green Version]
- Lombardi, G.; Zustovich, F.; Donach, M.; Dalla Palma, M.; Nicoletto, O.; Pastorelli, D. An update on targeted therapy in metastatic renal cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2012, 30, 240–246. [Google Scholar] [CrossRef]
- Motzer, R.J.; Hutson, T.E.; Glen, H.; Michaelson, M.D.; Molina, A.; Eisen, T.; Jassem, J.; Zolnierek, J.; Maroto, J.P.; Mellado, B.; et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: A randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015, 16, 1473–1482. [Google Scholar] [CrossRef] [Green Version]
- Cuenod, C.A.; Fournier, L.; Balvay, D.; Guinebretière, J.M. Tumor angiogenesis: Pathophysiology and implications for contrast-enhanced MRI and CT assessment. Abdom. Imaging 2006, 31, 188–193. [Google Scholar] [CrossRef]
- Jonasch, E.; Gao, J.; Rathmell, W.K. Renal cell carcinoma. BMJ 2014, 349. [Google Scholar] [CrossRef]
- Shinagare, A.B.; Krajewski, K.M.; Braschi-Amirfarzan, M.; Ramaiya, N.H. Advanced renal cell carcinoma: Role of the radiologist in the era of precision medicine. Radiology 2017, 284, 333–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rini, B.I.; Plimack, E.R.; Stus, V.; Gafanov, R.; Hawkins, R.; Nosov, D.; Pouliot, F.; Alekseev, B.; Soulières, D.; Melichar, B.; et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N. Engl. J. Med. 2019, 380, 1116–1127. [Google Scholar] [CrossRef]
- De Velasco, G.; Bex, A.; Albiges, L.; Powles, T.; Rini, B.I.; Motzer, R.J.; Heng, D.Y.C.; Escudier, B. Sequencing and combination of systemic therapy in metastatic renal cell carcinoma. Eur. Urol. Oncol. 2019, 2, 505–514. [Google Scholar] [CrossRef]
- Dromain, C.; Beigelman, C.; Pozzessere, C.; Duran, R.; Digklia, A. Imaging of tumour response to immunotherapy. Eur. Radiol. Exp. 2020, 4, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Xiang, R.; Lode, H.N.; Gillies, S.D.; Reisfeld, R.A. T cell memory against colon carcinoma is long-lived in the absence of antigen. J. Immunol. 1999, 163, 3676–3683. [Google Scholar]
- Motzer, R.J.; Escudier, B.; McDermott, D.F.; George, S.; Hammers, H.J.; Srinivas, S.; Tykodi, S.S.; Sosman, J.A.; Procopio, G.; Plimack, E.R.; et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 2015, 373, 1803–1813. [Google Scholar] [CrossRef]
- Vig, S.V.L.; Zan, E.; Kang, S.K. Imaging for metastatic renal cell carcinoma. Urol. Clin. N. Am. 2020, 47, 281–291. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Litière, S.; De Vries, E.G.; Sargent, D.; Shankar, L.; Bogaerts, J.; Seymour, L. The role of response evaluation criteria in solid tumour in anticancer treatment evaluation: Results of a survey in the oncology community. Eur. J. Cancer 2014, 50, 260–266. [Google Scholar] [CrossRef]
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images are more than pictures, they are data. Radiology 2016, 278, 563–577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stanzione, A.; Ricciardi, C.; Cuocolo, R.; Romeo, V.; Petrone, J.; Sarnataro, M.; Mainenti, P.P.; Improta, G.; De Rosa, F.; Insabato, L.; et al. MRI radiomics for the prediction of fuhrman grade in clear cell renal cell carcinoma: A machine learning exploratory study. J. Digit. Imaging 2020, 33, 879–887. [Google Scholar] [CrossRef]
- Khene, Z.-E.; Mathieu, R.; Peyronnet, B.; Kokorian, R.; Gasmi, A.; Khene, F.; Rioux-Leclercq, N.; Kammerer-Jacquet, S.F.; Shariat, S.; Laguerre, B.; et al. Radiomics can predict tumour response in patients treated with Nivolumab for a metastatic renal cell carcinoma: An artificial intelligence concept. World J. Urol. 2020, 3–5. [Google Scholar] [CrossRef]
- Han, K.S.; Jung, D.C.; Choi, H.J.; Jeong, M.S.; Cho, K.S.; Joung, J.Y.; Seo, H.K.; Lee, K.H.; Chung, J. Pretreatment assessment of tumor enhancement on contrast-enhanced computed tomography as a potential predictor of treatment outcome in metastatic renal cell carcinoma patients receiving antiangiogenic therapy. Cancer 2010, 116, 2332–2342. [Google Scholar] [CrossRef] [PubMed]
- Baccala, A.; Hedgepeth, R.; Kaouk, J.; Magi-Galluzzi, C.; Gilligan, T.; Fergany, A. Pathological evidence of necrosis in recurrent renal mass following treatment with sunitinib. Int. J. Urol. 2007, 14, 1095–1097. [Google Scholar] [CrossRef]
- Smith, A.D.; Lieber, M.L.; Shah, S.N. Assessing tumor response and detecting recurrence in metastatic renal cell carcinoma on targeted therapy: Importance of size and attenuation on contrast-enhanced CT. Am. J. Roentgenol. 2010, 194, 157–165. [Google Scholar] [CrossRef] [Green Version]
- Choi, H.; Charnsangavej, C.; Faria, S.C.; Macapinlac, H.A.; Burgess, M.A.; Patel, S.R.; Chen, L.L.; Podoloff, D.A.; Benjamin, R.S. Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: Proposal of new computed tomography response criteria. J. Clin. Oncol. 2007, 25, 1753–1759. [Google Scholar] [CrossRef]
- Thian, Y.; Gutzeit, A.; Koh, D.-M.; Fisher, R.; Lote, H.; Larkin, J.; Sohaib, A. Revised choi imaging criteria correlate with clinical outcomes in patients with metastatic renal cell carcinoma treated with sunitinib. Radiology 2014, 273, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Sabir, A.; Schor-Bardach, R.; Wilcox, C.J.; Rahmanuddin, S.; Atkins, M.B.; Kruskal, J.B.; Signoretti, S.; Raptopoulos, V.D.; Goldberg, S.N. Perfusion MDCT enables early detection of therapeutic response to antiangiogenic therapy. Am. J. Roentgenol. 2008, 191, 133–139. [Google Scholar] [CrossRef]
- Goh, V.; Ng, Q.S.; Miles, K. Computed tomography perfusion imaging for therapeutic assessment: Has it come of age as a biomarker in oncology? Investig. Radiol. 2012, 47, 2–4. [Google Scholar] [CrossRef]
- Wolchok, J.D.; Hoos, A.; O’Day, S.; Weber, J.S.; Hamid, O.; Lebbé, C.; Maio, M.; Binder, M.; Bohnsack, O.; Nichol, G.; et al. Guidelines for the evaluation of immune therapy activity in solid tumors: Immune-related response criteria. Clin. Cancer Res. 2009, 15, 7412–7420. [Google Scholar] [CrossRef] [Green Version]
- Fujimoto, D.; Yoshioka, H.; Kataoka, Y.; Morimoto, T.; Hata, T.; Kim, Y.H.; Tomii, K.; Ishida, T.; Hirabayashi, M.; Hara, S.; et al. Pseudoprogression in previously treated patients with non–small cell lung cancer who received nivolumab monotherapy. J. Thorac. Oncol. 2019, 14, 468–474. [Google Scholar] [CrossRef] [Green Version]
- Besse, B.; Ferrara, R.; Mezquita, L.; Texier, M.; Lahmar, J.; Audigier-Valette, C.; Tessonnier, L.; Mazieres, J.; Zalcman, G.; Brosseau, S.; et al. Hyperprogressive disease in patients with advanced non-small cell lung cancer treated with PD-1/PD-L1 inhibitors or with single-agent chemotherapy. JAMA Oncol. 2018, 4, 1543–1552. [Google Scholar] [CrossRef]
- Champiat, S.; Dercle, L.; Ammari, S.; Massard, C.; Hollebecque, A.; Postel-Vinay, S.; Chaput, N.; Eggermont, A.; Marabelle, A.; Soria, J.C.; et al. Hyperprogressive disease is a new pattern of progression in cancer patients treated by anti-PD-1/PD-L1. Clin. Cancer Res. 2017, 23, 1920–1928. [Google Scholar] [CrossRef] [Green Version]
- Nishino, M.; Giobbie-Hurder, A.; Gargano, M.; Suda, M.; Ramaiya, N.H.; Hodi, F.S. Developing a common language for tumor response to immunotherapy: Immune-related response criteria using unidimensional measurements. Clin. Cancer Res. 2013, 19, 3936–3943. [Google Scholar] [CrossRef] [Green Version]
- Seymour, P.L.; Cancer, C.; Group, T.; Bogaerts, J.; Perrone, A.; Medicine, T.; Ford, R.; Trials, C.; Consulting, I.; Mead, B.; et al. iRECIST: Guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017, 18, e143–e152. [Google Scholar] [CrossRef] [Green Version]
- Kataoka, Y.; Hirano, K. Which criteria should we use to evaluate the efficacy of immune-checkpoint inhibitors? Ann. Transl. Med. 2018, 6, 222. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Penkov, K.; Haanen, J.; Rini, B.; Albiges, L.; Campbell, M.T.; Venugopal, B.; Kollmannsberger, C.; Negrier, S.; Uemura, M.; et al. Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N. Engl. J. Med. 2019, 380, 1103–1115. [Google Scholar] [CrossRef]
- Fournier, L.S.; Oudard, S.; Thiam, R.; Trinquart, L.; Banu, E.; Medioni, J.; Balvay, D.; Chatellier, G.; Frija, G.; Cuenod, C.A. Metastatic renal carcinoma: Evaluation of antiangiogenic therapy with dynamic contrast-enhanced CT. Radiology 2010, 256, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, K.T.; Rosen, M.A.; Heitjan, D.F.; Gallagher, M.L.; Schwartz, B.; Schnall, M.D.; O’Dwyer, P.J. Pilot study of DCE-MRI to predict progression-free survival with sorafenib therapy in renal cell carcinoma. Cancer Biol. Ther. 2008, 7, 496–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nathan, P.D.; Vinayan, A.; Stott, D.; Juttla, J.; Goh, V. CT response assessment combining reduction in both size and arterial phase density correlates with time to progression in metastatic renal cancer patients treated with targeted therapies. Cancer Biol. Ther. 2010, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goh, V.; Ganeshan, B.; Nathan, P.; Juttla, J.K.; Vinayan, A.; Miles, K.A. Assessment of response to tyrosine kinase inhibitors in metastatic renal cell cancer: CT texture as a predictive biomarker. Radiology 2011, 261, 165–171. [Google Scholar] [CrossRef]
- Romagnoli, G.; Wiedermann, M.; Hübner, F.; Wenners, A.; Mathiak, M.; Röcken, C.; Maass, N.; Klapper, W.; Alkatout, I. Morphological evaluation of tumor-infiltrating lymphocytes (TILs) to investigate invasive breast cancer immunogenicity, reveal lymphocytic networks and help relapse prediction: A retrospective study. Int. J. Mol. Sci. 2017, 18, 1936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, R.; Limkin, E.J.; Vakalopoulou, M.; Dercle, L.; Champiat, S.; Han, S.R.; Verlingue, L.; Brandao, D.; Lancia, A.; Ammari, S.; et al. A radiomics approach to assess tumour-infiltrating CD8 cells and response to anti-PD-1 or anti-PD-L1 immunotherapy: An imaging biomarker, retrospective multicohort study. Lancet Oncol. 2018, 19, 1180–1191. [Google Scholar] [CrossRef]

| Response | RECIST 1.1 [17] | Choi Criteria [25] | Modified Choi Criteria [26] |
|---|---|---|---|
| Complete Response (CR) | No evidence of target and non-target lesions; Short axis of lymph node(s) < 10 mm; No new lesions. | No evidence of target and non-target lesions; Short axis of lymph node(s) < 10 mm; No new lesions. | No evidence of target and non-target lesions; Short axis of lymph node(s) < 10 mm; No new lesions. |
| Partial Response (PR) | Decreased (≥30%) sum of target lesions longest diameters. | Decreased (≥10%) sum of the target lesions longest diameters OR Decreased (≥15%) tumor density (HU). | Decreased (≥10%) sum of the target lesions longest diameters AND Decreased (≥15%) tumor density (HU). Decreased (≥30%) sum of the target lesions longest diameters. |
| Stable Disease (SD) | Not PR/PD. | Not PR/PD. | Not PR/PD. |
| Progressive Disease (PD) | Increased (≥20%) sum of the target lesions longest diameters; Evidence of new lesion(s). | Increased (≥10%) sum of the target lesions longest diameters and not PR by tumor density; Evidence of new lesion(s). New intratumoral nodules or increase in size of the previous intratumoral nodules. | Increased (≥10%) sum of the longest diameters of target lesions; New lesions or intratumoral nodules. |
| Response | RECIST 1.1 [17] | irRC [29] | irRECIST [33] | iRECIST [34] |
|---|---|---|---|---|
| Dimension | One. | Two. | One. | One. |
| New measurable lesions | Designates PD. | New lesion(s) does not define PD; Incorporates into total tumor burden for the assessment of PD. | New lesion(s) does not define PD; Incorporates into total tumor burden for the assessment of PD. | Separately documents; adds into PD. |
| Complete Response (CR) | No evidence of target and non-target lesions; Short axis of lymph node(s) < 10 mm; No new lesions. | No evidence of target and non-target lesions in two consecutive exams (at least 4 weeks apart); Short axis of lymph node(s) < 10 mm; No new lesions. | No evidence of target and non-target lesions; Short axis of lymph node < 10 mm; Short axis of lymph node(s) < 10 mm; No new lesions. | No evidence of target and non-target lesions; Short axis of lymph node < 10 mm; Short axis of lymph node(s) < 10 mm; No new lesions. |
| Partial Response (PR)a | Decreased (≥30%) sum of target lesions longest diameters. | Decreased (≥50%) total tumor burden; Unclear non-target lesions progression. | Decrease (≥30%) in the sum of target lesions longest diameter; Unclear non-target lesions progression. | Decrease (≥30%) in the sum of target lesions longest diameter; Unclear non-target lesions progression. |
| Stable Disease (SD) | Not PR/PD. | Not PR/PD. | Not PR/PD. | Not PR/PD. |
| Progressive Disease (PD)b | Increased (≥20%) sum of the target lesions longest diameters; New lesion(s). | Increased (≥25%) total tumor burden. | Increased (≥20%) sum of the target lesions longest diameters; Increased non-target lesions. | iUPD: increased (≥20%; at least ≥5 mm) sum of the target lesions longest diameters; Increased non-target lesions. |
| Confirmation of PD (at least 4 weeks apart from the previous exam) | NA. | Increased (≥25%) in total tumor burden. | New clear progression or continued progression from the first PD; Evidence of new lesions. | iCPD: increased new target lesions (≥5 mm); Progression of target, non-target lesions and new non-target lesions; Evidence of new lesions. Presence of other new lesions. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caruso, M.; Romeo, V.; Stanzione, A.; Buonerba, C.; Di Lorenzo, G.; Maurea, S. Current Imaging Evaluation of Tumor Response to Advanced Medical Treatment in Metastatic Renal-Cell Carcinoma: Clinical Implications. Appl. Sci. 2021, 11, 6930. https://doi.org/10.3390/app11156930
Caruso M, Romeo V, Stanzione A, Buonerba C, Di Lorenzo G, Maurea S. Current Imaging Evaluation of Tumor Response to Advanced Medical Treatment in Metastatic Renal-Cell Carcinoma: Clinical Implications. Applied Sciences. 2021; 11(15):6930. https://doi.org/10.3390/app11156930
Chicago/Turabian StyleCaruso, Martina, Valeria Romeo, Arnaldo Stanzione, Carlo Buonerba, Giuseppe Di Lorenzo, and Simone Maurea. 2021. "Current Imaging Evaluation of Tumor Response to Advanced Medical Treatment in Metastatic Renal-Cell Carcinoma: Clinical Implications" Applied Sciences 11, no. 15: 6930. https://doi.org/10.3390/app11156930
APA StyleCaruso, M., Romeo, V., Stanzione, A., Buonerba, C., Di Lorenzo, G., & Maurea, S. (2021). Current Imaging Evaluation of Tumor Response to Advanced Medical Treatment in Metastatic Renal-Cell Carcinoma: Clinical Implications. Applied Sciences, 11(15), 6930. https://doi.org/10.3390/app11156930









