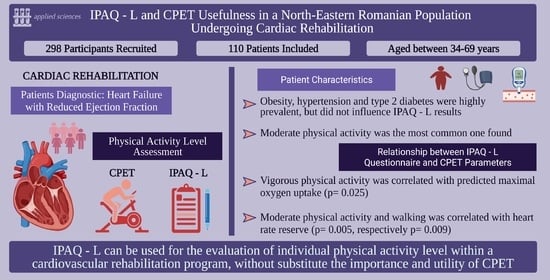
IPAQ-L and CPET Usefulness in a North-Eastern Romanian Population Undergoing Cardiac Rehabilitation
Abstract
1. Introduction
1.1. Background and Rationale
1.2. Study Objectives
2. Materials and Methods
2.1. Study Design and Setting
2.2. Ethics Approval
2.3. Study Population
2.4. Study Procedures and Outcome Assessment
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Outcomes
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Association of Cardiovascular & Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs, 5th ed.; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corra, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Conraads, V.; Corrà, U.; Dickstein, K.; Francis, D.P.; Jaarsma, T.; McMurray, J.; Pieske, B.; Piotrowicz, E.; Schmid, J.-P.; et al. Exercise training in heart failure: From theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur. J. Heart Fail. 2011, 13, 347–357. [Google Scholar] [CrossRef]
- Coats, A.J.; Adamopoulos, S.; Meyer, T.E.; Conway, J.; Sleight, P. Effects of physical training in chronic heart failure. Lancet 1990, 335, 63–66. [Google Scholar] [CrossRef]
- Bjarnason-Wehrens, B.; Nebel, R.; Jensen, K.; Hackbusch, M.; Grilli, M.; Gielen, S.; Schwaab, B.; Rauch, B. Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2020, 27, 929–952. [Google Scholar] [CrossRef] [PubMed]
- Zupo, R.; Castellana, F.; Sardone, R.; Sila, A.; Giagulli, V.A.; Triggiani, V.; Cincione, R.I.; Giannelli, G.; de Pergola, G. Preliminary Trajectories in Dietary Behaviors during the COVID-19 Pandemic: A Public Health Call to Action to Face Obesity. Int. J. Environ. Res. Public Health 2020, 17, 7073. [Google Scholar] [CrossRef]
- Martinez Aguirre-Betolaza, A.; Mujika, I.; Loprinzi, P.; Corres, P.; Gorostegi-Anduaga, I.; Maldonado-Martín, S. Physical Activity, Sedentary Behavior, and Sleep Quality in Adults with Primary Hypertension and Obesity before and after an Aerobic Exercise Program: EXERDIET-HTA Study. Life 2020, 10, 153. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.P.; Mokhtar, N.; Byrne, N.M. Assessment of physical activity and energy expenditure: An overview of objective measures. Front. Nutr. 2014, 1, 5. [Google Scholar] [CrossRef] [PubMed]
- Maiorana, A.; Ntoumanis, N. Physical Activity in Patients with Cardiovascular Disease: Challenges in Measurement and Motivation. Heart Lung Circ. 2017, 26, 1001–1003. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- International Physical Activity Questionnaire. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms. Available online: https://sites.google.com/site/theipaq/ (accessed on 3 October 2017).
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.; Schmid, J.-P.; Vigorito, C.; et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2021, 28, 460–495. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Fisher-Hoch, S.P.; Reininger, B.; McCormick, J.B. Recommended Levels of Physical Activity Are Associated with Reduced Risk of the Metabolic Syndrome in Mexican-Americans. PLoS ONE 2016, 11, e0152896. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.; Bull, F.; Chey, T.; Craig, C.L.; Ainsworth, B.E.; Sallis, J.F.; Bowles, H.R.; Hagstromer, M.; Sjostrom, M.; Pratt, M.; et al. The International Prevalence Study on Physical Activity: Results from 20 countries. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- McDonough, J.R.; Bruce, R.A. Maximal exercise testing in assessing cardiovascular function. J. South Carol. Med Assoc. 1969, 65, 25–33. [Google Scholar] [PubMed]
- van der Ploeg, H.P.; Tudor-Locke, C.; Marshall, A.L.; Craig, C.; Hagströmer, M.; Sjöström, M.; Bauman, A. Reliability and validity of the international physical activity questionnaire for assessing walking. Res. Q. Exerc. Sport 2010, 81, 97–101. [Google Scholar] [CrossRef]
- van Dyck, D.; Cardon, G.; Deforche, B.; de Bourdeaudhuij, I. IPAQ interview version: Convergent validity with accelerometers and comparison of physical activity and sedentary time levels with the self-administered version. J. Sports Med. Phys. Fit. 2015, 55, 776–786. [Google Scholar] [PubMed]
- Clemes, S.A.; David, B.M.; Zhao, Y.; Han, X.; Brown, W. Validity of two self-report measures of sitting time. J. Phys. Act. Health 2012, 9, 533–539. [Google Scholar] [CrossRef] [PubMed]
- van Holle, V.; de Bourdeaudhuij, I.; Deforche, B.; van Cauwenberg, J.; van Dyck, D. Assessment of physical activity in older Belgian adults: Validity and reliability of an adapted interview version of the long International Physical Activity Questionnaire (IPAQ-L). BMC Public Health 2015, 15, 433. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Kamarudin, K.S.; Wan Muda, W.A.M. Associations between self-reported and objectively measured physical activity and overweight/obesity among adults in Kota Bharu and Penang, Malaysia. BMC Public Health 2019, 19, 621. [Google Scholar] [CrossRef] [PubMed]
- Tali, M.; Lusmägi, P.; Unt, E. Leisure time physical activity in Estonian population: Adherence to physical activity recommendations and relationships with overweight. Arch. Public Health 2016, 74, 36. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Varo, J.J.; Santos, J.L.; de Irala, J.; Gibney, M.; Kearney, J.; Martínez, J.A. Prevalence of physical activity during leisure time in the European Union. Med. Sci. Sports Exerc. 2001, 33, 1142–1146. [Google Scholar] [CrossRef] [PubMed]
- Nolan, R.C.; Raynor, A.J.; Berry, N.M.; May, E.J. Self-Reported Physical Activity Using the International Physical Activity Questionnaire (IPAQ) in Australian Adults with Type 2 Diabetes, with and Without Peripheral Neuropathy. Can. J. Diabetes 2016, 40, 576–579. [Google Scholar] [CrossRef]
- Mynarski, W.; Psurek, A.; Borek, Z.; Rozpara, M.; Grabara, M.; Strojek, K. Declared and real physical activity in patients with type 2 diabetes mellitus as assessed by the International Physical Activity Questionnaire and Caltrac accelerometer monitor: A potential tool for physical activity assessment in patients with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2012, 98, 46–50. [Google Scholar] [CrossRef]
- Riegel, G.R.; Martins, G.B.; Schmidt, A.G.; Rodrigues, M.P.; Nunes, G.S.; Correa, V., Jr.; Fuchs, S.C.; Fuchs, F.D.; Ribeiro, P.A.; Moreira, L.B. Self-reported adherence to physical activity recommendations compared to the IPAQ interview in patients with hypertension. Patient Prefer. Adherence 2019, 13, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Bravo, M.; Romero, T.; Romero Camila, X.; Koch, E.; Sandoval, D.; Gatica, S.; Ahlers, I.; HenrÍquez, O.; Garrido, J. Abstract P274: Predictive Value of the International Physical Activity Questionnaire of the Aerobic Capacity in Sedentary Hypertensive Women. Circulation 2012, 125, AP274. [Google Scholar]
- Caban-Martinez, A.J.; Lee, D.J.; Fleming, L.E.; LeBlanc, W.G.; Arheart, K.L.; Chung-Bridges, K.; Christ, S.L.; McCollister, K.E.; Pitman, T. Leisure-time physical activity levels of the US workforce. Prev. Med. 2007, 44, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Pratt, M.; Macera, C.A.; Blanton, C. Levels of physical activity and inactivity in children and adults in the United States: Current evidence and research issues. Med. Sci. Sports Exerc. 1999, 31, S526–S533. [Google Scholar] [CrossRef]
- Tucker, J.M.; Welk, G.J.; Beyler, N.K. Physical activity in U.S.: Adults compliance with the Physical Activity Guidelines for Americans. Am. J. Prev. Med. 2011, 40, 454–461. [Google Scholar] [CrossRef]
- von Lengerke, T.; Mielck, A. Body weight dissatisfaction by socioeconomic status among obese, preobese and normal weight women and men: Results of the cross-sectional KORA Augsburg S4 population survey. BMC Public Health 2012, 12, 342. [Google Scholar] [CrossRef]
- Lemon, S.C.; Rosal, M.C.; Zapka, J.; Borg, A.; Andersen, V. Contributions of weight perceptions to weight loss attempts: Differences by body mass index and gender. Body Image 2009, 6, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Shediac-Rizkallah, M.C.; Celentano, D.D.; Rohde, C. A population-based study of age and gender differences in patterns of health-related behaviors. Am. J. Prev. Med. 1999, 17, 8–17. [Google Scholar] [CrossRef]
- Fan, M.; Su, M.; Tan, Y.; Liu, Q.; Ren, Y.; Li, L.; Lv, J. Gender, Age, and Education Level Modify the Association between Body Mass Index and Physical Activity: A Cross-Sectional Study in Hangzhou, China. PLoS ONE 2015, 10, e0125534. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.; Tan, L.; Carey-Jones, S.; Riddell, N.; Davies, R.; Brownsdon, A.; Kelson, M.; Williams-Thomas, R.; Busse, M.; Davies, M.M.; et al. Can wearable technology be used to approximate cardiopulmonary exercise testing metrics? Perioper. Med. 2021, 10, 9. [Google Scholar] [CrossRef] [PubMed]
- Dorelli, G.; Braggio, M.; Gabbiani, D.; Busti, F.; Caminati, M.; Senna, G.; Girelli, D.; Laveneziana, P.; Ferrari, M.; Sartori, G.; et al. Importance of Cardiopulmonary Exercise Testing amongst Subjects Recovering from COVID-19. Diagnostics 2021, 11, 507. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, P.D.; Frith, E. Effects of Sedentary Behavior, Physical Activity, Frequency of Protein Consumption, Lower Extremity Strength and Lean Mass on All-Cause Mortality. J. Lifestyle Med. 2018, 8, 8–15. [Google Scholar] [CrossRef]
- Fournier, M.; Radel, R.; Bailly, L.; Pradier, C.; Fabre, R.; Fuch, A.; Mosse, P.; Domerego, J.-J.; Gal, J.; D’arripe-Longueville, F. “As du Coeur” study: A randomized controlled trial on physical activity maintenance in cardiovascular patients. BMC Cardiovasc. Disord. 2018, 18, 77. [Google Scholar] [CrossRef] [PubMed]
- Leuciuc, F. Perception on Physical Education among Students. Rev. Rom. Pentru Educ. Multidimens. 2018, 10, 134–143. [Google Scholar] [CrossRef]
- Fagaras, S.-P.; Radu, L.-E.; Vanvu, G. The level of physical activity of university students. Procedia Soc. Behav. Sci. 2015, 197, 1454–1457. [Google Scholar] [CrossRef]
- Badicu, G. Physical Activity and Sleep Quality in Students of the Faculty of Physical Education and Sport of Braşov, Romania. Sustainability 2018, 10, 2410. [Google Scholar] [CrossRef]
- Herghelegiu, A.M.; Moser, A.; Prada, G.I.; Born, S.; Wilhelm, M.; Stuck, A.E. Effects of health risk assessment and counselling on physical activity in older people: A pragmatic randomised trial. PLoS ONE 2017, 12, e0181371. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total | Males | Females | p-Value * |
|---|---|---|---|---|
| Number, n (%) | 110 (100) | 52 (47.27) | 58 (52.72) | |
| Age (years), mean (SD) | 57.20 (6.45) | 57.11 (7.05) | 57.27 (5.92) | 0.897 |
| Weight (kg), mean (SD) | 83.48 (12.40) | 88.15 (12.41) | 79.29 (10.89) | <0.001 |
| BMI (kg/m2), mean (SD) | 30.28 (4.80) | 29.66 (5.22) | 30.84 (4.36) | 0.200 |
| AC (cm), mean (SD) | 97.81 (12.41) | 101.09 (13.18) | 94.87 (10.96) | 0.008 |
| SBP (mmHg), mean (SD) | 134.44 (15.31) | 132.96 (17.57) | 135.77 (12.97) | 0.346 |
| DBP (mmHg), mean (SD) | 83.65 (10.52) | 83.88 (10.20) | 83.44 (10.89) | 0.829 |
| Glycemia (mg/dL), mean (SD) | 114.73 (38.90) | 121.61 (35.79) | 108.45 (32.49) | 0.048 |
| TC (mg/dL), mean (SD) | 200.00 (42.97) | 190.15 (45.68) | 208.82 (38.68) | 0.022 |
| HDL-C (mg/dL), mean (SD) | 48.22 (13.15) | 45.17 (11.87) | 51.05 (13.75) | 0.019 |
| LDL-C (mg/dL), mean (SD) | 121.88 (37.99) | 115.98 (39.76) | 127.45 (35.73) | 0.127 |
| Non-HDL cholesterol (mg/dL), mean (SD) | 151.39 (41.00) | 144.98 (44.14) | 157.35 (37.26) | 0.118 |
| TG (mg/dL), mean (SD) | 158.72 (99.80) | 161.09 (111.53) | 156.60 (88.91) | 0.815 |
| EGFR (mL/min/1.73 m2), mean (SD) | 84.02 (16.58) | 84.02 (17.28) | 81.34 (15.60) | 0.075 |
| LVEDD (mm), mean (SD) | 48.28 (6.29) | 51.63 (5.14) | 45.08 (5.61) | <0.001 |
| LVMI (g/m2), mean (SD) | 120.96 (35.58) | 134.11 (33.44) | 107.19 (32.74) | <0.001 |
| %HR (%), mean (SD) | 75.34 (12.54) | 72.82 (11.89) | 77.60 (12.77) | 0.045 |
| Exercise resistance (W), mean (SD) | 90.02 (30.17) | 105.84 (30.01) | 75.84 (22.38) | <0.001 |
| Workload (METS), mean (SD) | 4.85 (1.33) | 5.21 (1.39) | 4.54 (1.20) | 0.008 |
| Weight status, n (%): Normal weight | 10 (9.09) | 6 (11.54) | 4 (6.9) | 0.512 |
| Overweight | 52 (47.27) | 25 (48.08) | 27 (46.50) | 1.000 |
| First-degree obesity | 30 (27.27) | 15 (28.85) | 15 (25.86) | 0.831 |
| Second-degree obesity | 15 (13.63) | 5 (9.62) | 10 (17.24) | 0.278 |
| Third-degree obesity | 3 (2.72) | 1 (1.92) | 2 (3.45) | 1.000 |
| Hypertension, n (%): Normotensive | 22 (20) | 15 (28.85) | 7 (12.07) | 0.033 |
| First-degree HTN | 10 (9.09) | 2 (3.85) | 8 (13.79) | 0.099 |
| Second-degree HTN | 20 (18.18) | 5 (9.62) | 15 (25.86) | 0.046 |
| Third-degree HTN | 58 (52.72) | 30 (57.69) | 28 (48.28) | 0.345 |
| Type 2 diabetes, n (%) | 31 (28.18) | 21 (40.38) | 10 (17.24) | 0.010 |
| Total | Males | Females | |
|---|---|---|---|
| Low level of PA (%) | 27.07 | 31.79 | 22.40 |
| Moderate level of PA (%) | 65.35 | 62.62 | 68.04 |
| High level of PA (%) | 7.57 | 5.58 | 9.54 |
| Age | MTCF | |||
|---|---|---|---|---|
| R-Value | p-Value * | R-Value | p-Value * | |
| Total MET-minutes/week at work | −0.28 | 0.002 | 0.28 | 0.002 |
| Total MET-minutes/week for transportation | −0.01 | 0.850 | 0.01 | 0.850 |
| Total MET-minutes/week in domestic and garden activities | −0.01 | 0.852 | 0.01 | 0.852 |
| Total MET-minutes/week in leisure time | 0.04 | 0.631 | −0.04 | 0.631 |
| Vigorous PA (leisure time) | −0.12 | 0.183 | 0.12 | 0.183 |
| Total physical activity MET-minutes/week | −0.18 | 0.053 | 0.18 | 0.053 |
| BMI (kg/m2) | 0.15 | 0.107 | −0.15 | 0.107 |
| AC (cm) | 0.10 | 0.295 | −0.10 | 0.295 |
| LVEF (%) | 0.10 | 0.338 | −0.10 | 0.338 |
| Total | Males | Females | p Value * | ||||
|---|---|---|---|---|---|---|---|
| Mdn (IQR) | (%) | Mdn (IQR) | (%) | Mdn (IQR) | (%) | ||
| Total MET-minutes/week at work | 6132 (1936–11,370) | 21.1 | 15,210 (6194–25,524) | 22.6 | 2866 (2087–6936) | 19.7 | 0.384 |
| Total MET-minutes/week for transportation | 594 (198–1386) | 18.1 | 988 (181–8752) | 20.3 | 877 (330–4788) | 15.9 | 0.517 |
| Total MET-minutes/week in domestic and garden activities | 2520 (240–5790) | 54.5 | 12,675 (4147–17,085) | 50.8 | 1350 (180–6720) | 58.1 | 0.019 |
| Total MET-minutes/week in leisure time | 198 (33–594) | 6.1 | 123 (49–198) | 6.1 | 579 (99–1482) | 6.1 | 0.983 |
| Total sitting (minutes) | 540 (420–660) | 545 (300–692) | 540 (360–600) | 0.899 | |||
| Total walking (MET-minutes/week) | 1072 (346–2227) | 27.1 | 5131 (1249–10,065) | 31.7 | 2095 (280–5841) | 22.4 | 0.799 |
| Total moderate activity (MET-minutes/week) | 2840 (415–8115) | 65.3 | 13,575 (11,797–17,085) | 62.6 | 5340 (1620–7920) | 68.0 | 0.210 |
| Total vigorous activity (MET-minutes/week) | 2880 (780–7440) | 7.5 | 7440 (4800–19,800) | 5.5 | 2400 (600–4320) | 9.5 | 0.057 |
| Total physical activity (MET-minutes/week) | 4735 (1614–12,515) | 29,382 (23,833–37,727) | 14,061 (3080–20,091) | 0.964 | |||
| CPET Parameters | IPAQ-L and Physical Activity (METS-Minutes/Week) | |||||||
|---|---|---|---|---|---|---|---|---|
| Vigorous Activity | Moderate Activity | Walking | Total Physical Activity | |||||
| R-Value | p-Value | R-Value | p-Value | R-Value | p-Value | R-Value | p-Value | |
| VO2 max% | 0.52 | 0.025 | 0.19 | 0.447 | 0.32 | 0.195 | 0.34 | 0.168 |
| AT | 0.53 | 0.026 | 0.12 | 0.632 | 0.16 | 0.522 | 0.30 | 0.228 |
| RER | 0.02 | 0.923 | 0.18 | 0.468 | 0.16 | 0.502 | 0.07 | 0.781 |
| WR% | 0.52 | 0.027 | 0.45 | 0.061 | 0.48 | 0.040 | 0.48 | 0.040 |
| HRR | 0.61 | 0.007 | 0.63 | 0.005 | 0.59 | 0.009 | 0.65 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manta, A.; Cojocaru, E.; Leon-Constantin, M.M.; Maștaleru, A.; Roca, M.; Rusu, C.; Cojocariu, S.A.; Mitu, F. IPAQ-L and CPET Usefulness in a North-Eastern Romanian Population Undergoing Cardiac Rehabilitation. Appl. Sci. 2021, 11, 5483. https://doi.org/10.3390/app11125483
Manta A, Cojocaru E, Leon-Constantin MM, Maștaleru A, Roca M, Rusu C, Cojocariu SA, Mitu F. IPAQ-L and CPET Usefulness in a North-Eastern Romanian Population Undergoing Cardiac Rehabilitation. Applied Sciences. 2021; 11(12):5483. https://doi.org/10.3390/app11125483
Chicago/Turabian StyleManta, Andrei, Elena Cojocaru, Maria Magdalena Leon-Constantin, Alexandra Maștaleru, Mihai Roca, Cristina Rusu, Sabina Alexandra Cojocariu, and Florin Mitu. 2021. "IPAQ-L and CPET Usefulness in a North-Eastern Romanian Population Undergoing Cardiac Rehabilitation" Applied Sciences 11, no. 12: 5483. https://doi.org/10.3390/app11125483
APA StyleManta, A., Cojocaru, E., Leon-Constantin, M. M., Maștaleru, A., Roca, M., Rusu, C., Cojocariu, S. A., & Mitu, F. (2021). IPAQ-L and CPET Usefulness in a North-Eastern Romanian Population Undergoing Cardiac Rehabilitation. Applied Sciences, 11(12), 5483. https://doi.org/10.3390/app11125483