The Effects of a 10-Week Home-Based Exercise Programme in Individuals with Parkinson’s Disease during the COVID-19 Pandemic: A Pilot Study
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
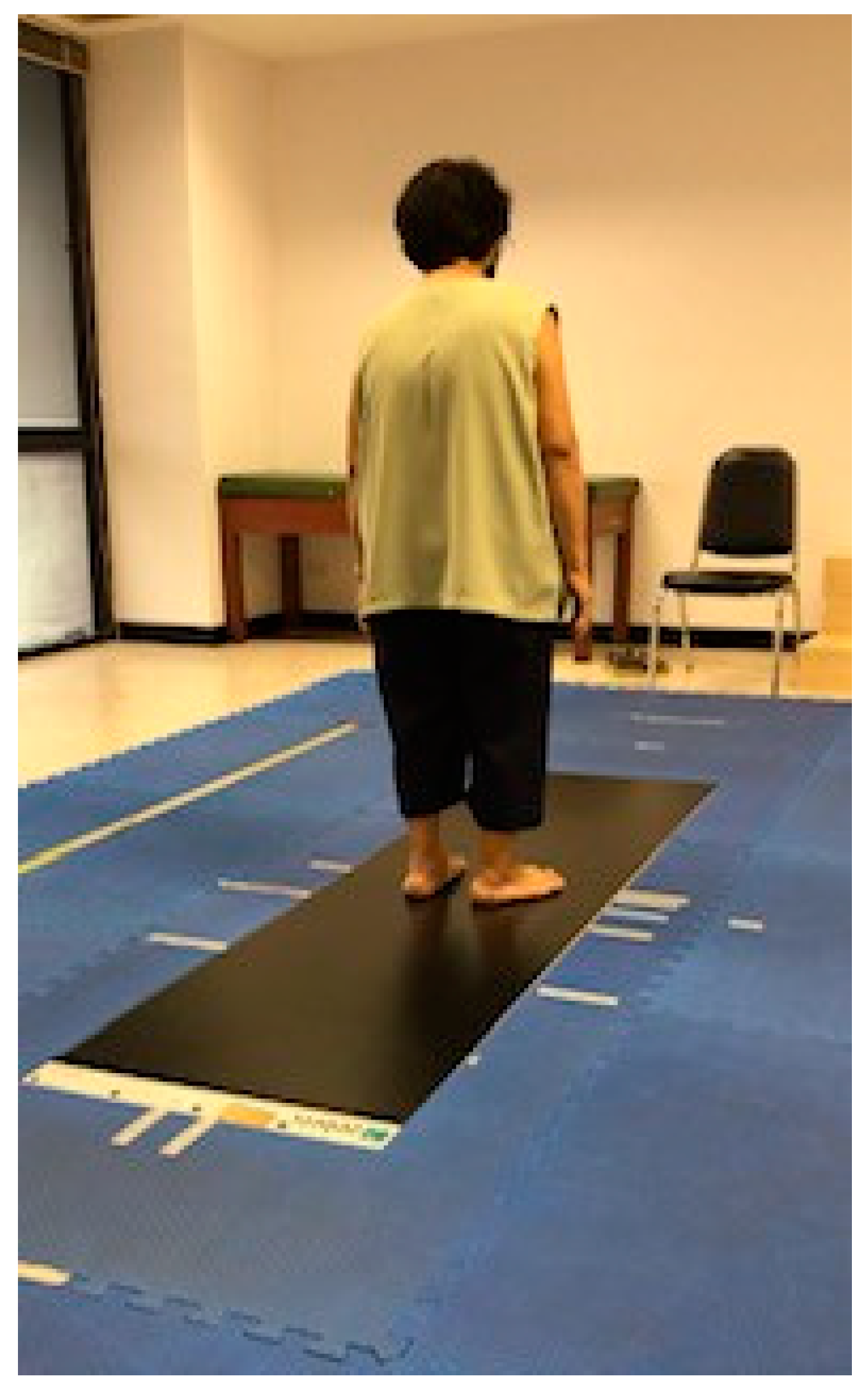
2.2. Exercise Programme
2.3. Procedure
2.3.1. Primary Outcome Measures
2.3.2. Secondary Outcome Measures
2.4. Statistical Analysis
3. Results
Booklet and Telephone Follow up Reporting during the 10 Week Exercise Period
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abbruzzese, G.; Marchese, R.; Avanzino, L.; Pelosin, E. Rehabilitation for Parkinson’s disease: Current outlook and future challenges. Parkinsonism Relat. Disord. 2016, 22, S60–S64. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.; Alcock, L.; Yarnall, A.J.; Lord, S.; Lawson, R.A.; Morris, R.; Taylor, J.P.; Burn, D.J.; Rochester, L.; Galna, B. Gait progression over 6 years in Parkinson’s disease: Effects of age, medication, and pathology. Front. Aging Neurosci. 2020, 12, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Khobkhun, F.; Hollands, K.; Hollands, M.; Ajjimaporn, A. Effectiveness of exercise-based rehabilitation for the treatment of axial rigidity in people with Parkinson’s disease: A Scoping Review. Phys. Ther. Rev. 2020. [Google Scholar] [CrossRef]
- Di Biase, L.; Di Santo, A.; Caminiti, M.L.; De Liso, A.; Shah, S.A.; Ricci, L.; Di Lazzaro, V. Gait analysis in Parkinson’s disease: An overview of the most accurate markers for diagnosis and symptoms monitoring. Sensors 2020, 20, 3529. [Google Scholar] [CrossRef] [PubMed]
- Ni, M.; Hazzard, J.B.; Signorile, J.F.; Luca, C. Exercise guidelines for gait function in Parkinson’s disease: A systematic review and meta-analysis. Neurorehabilit. Neural Repair 2018, 32, 872–886. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Wong-Yu, I.S.K.; Mak, M.K.Y. Effects of exercise on falls, balance, and gait ability in Parkinson’s disease: A meta-analysis. Neurorehabilit. Neural Repair 2016, 30, 512–527. [Google Scholar] [CrossRef] [PubMed]
- Radder, D.L.M.; Lígia Silva de Lima, A.; Domingos, J.; Keus, S.H.J.; van Nimwegen, M.; Bloem, B.R. Physiotherapy in Parkinson’s disease: A meta-analysis of present treatment modalities. Neurorehabilit. Neural Repair 2020, 34, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.Y.; Cho, K.H.; Jin, C.; Lee, J.; Kim, T.H.; Jung, W.S.; Moon, S.K.; Ko, C.N.; Cho, S.Y.; Jeon, C.Y.; et al. Exercise therapies for Parkinson’s disease: A systematic review and meta-analysis. Parkinson’s Dis. 2020, 2020, 2565320. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.; Painter, P. ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities, 4th ed.; Human Kinetics, Inc.: Champaign, IL, USA, 2016. [Google Scholar]
- Goodwin, V.A.; Richards, S.H.; Taylor, R.S.; Taylor, A.H.; Campbell, J.L. The effectiveness of exercise interventions for people with Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2008, 23, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Flynn, A.; Allen, N.E.; Dennis, S.; Canning, C.G.; Preston, E. Home-based prescribed exercise improves balance-related activities in people with Parkinson’s disease and has benefits similar to centre-based exercise: A systematic review. J. Physiother. 2019, 65, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Dereli, E.E.; Yaliman, A. Comparison of the effects of a physiotherapist-supervised exercise programme and a self-supervised exercise programme on quality of life in patients with Parkinson’s disease. Clin. Rehabil. 2010, 24, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Nocera, J.; Horvat, M.; Ray, C.T. Effects of home-based exercise on postural control and sensory organization in individuals with Parkinson disease. Parkinsonism Relat. Disord. 2009, 15, 742–745. [Google Scholar] [CrossRef] [PubMed]
- Khalil, H.; Busse, M.; Quinn, L.; Nazzal, M.; Batyha, W.; Alkhazaleh, S.; Alomari, M.A. A pilot study of a minimally supervised home exercise and walking program for people with Parkinson’s disease in Jordan. Neurodegener. Dis. Manag. 2017, 7, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.E.; Watts, J.J.; Evans, A.; Horne, M.; Kempster, P.; Danoudis, M.; McGinley, J.; Martin, C.; Menz, H.B. A home program of strength training, movement strategy training and education did not prevent falls in people with Parkinson’s disease: A randomised trial. J. Physiother. 2017, 63, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Schenkman, M.; Cutson, T.M.; Kuchibhatla, M.; Chandler, J.; Pieper, C.F.; Ray, L.; Laub, K.C. Exercise to improve spinal flexibility and function for people with Parkinson’s disease: A randomized, controlled trial. J. Am. Geriatr. Soc. 1998, 46, 1207–1216. [Google Scholar] [CrossRef] [PubMed]
- Srivanitchapoom, P.; Pitakpatapee, Y.; Suengtaworn, A. Parkinsonian syndromes: A review. Neurol. India 2018, 66, s15–s25. [Google Scholar] [CrossRef] [PubMed]
- King, L.A.; Wilhelm, J.; Chen, Y.; Blehm, R.; Nutt, J.; Chen, Z.; Serdar, A.; Horak, F.B. Effects of group, individual, and home exercise in persons with Parkinson disease: A randomized clinical trial. J. Neurol. Phys. Ther. 2015, 39, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Santos, V.V.; Araújo, M.A.; Nascimento, O.J.; Guimarães, F.S.; Orsini, M.; de Freitas, M.R. Effects of a physical therapy home-based exercise program for Parkinson’s disease. Fisioterapia em Movimento 2012, 25, 709–715. [Google Scholar] [CrossRef]
- Santos, L.; Fernandez-Rio, J.; Winge, K.; Barragan-Perez, B.; Gonzalez-Gomez, L.; Rodriguez-Perez VGonzález-Díez, V.; Lucía, A.; Iglesias-Soler, E.; Dopico-Calvo, X.; Fernández-Del-Olmo, M.; et al. Effects of progressive resistance exercise in akinetic-rigid Parkinson’s disease patients: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2017, 53, 651–663. [Google Scholar] [PubMed]
- Atterbury, E.M.; Welman, K.E. Balance training in individuals with Parkinson’s disease: Therapist-supervised vs. home-based exercise programme. Gait Posture 2017, 55, 138–144. [Google Scholar] [CrossRef] [PubMed]

| Demographic | HOME Group (n = 10) | CON Group (n = 8) |
|---|---|---|
| Age (years (SD)) | 68.60 ± 6.67 | 68.88 ± 6.73 |
| Body mass index (kg/m2 (SD))) | 23.66 ± 3.36 | 23.83 ± 4.23 |
| Men/women n (%) | 6 (60)/4 (40) | 4 (50)/4 (50) |
| Parkinson’s disease duration (years) | 5.08 | 4.80 |
| Modified Hoehn and Yahr scale | 2.6 | 2.58 |
| Medical comorbidities (n, %) Hypertension Diabetes mellitus Dyslipidemia Heart disease | 4 (40%) 3 (30%) 2 (20%) 1 (10%) | 4 (50%) 2 (25%) 1 (12.5%) 1 (12.5%) |
| Mini-Mental State Examination | 29.4 ± 5.02 | 29.25 ± 4.72 |
| Education (n (%)) High School >High school <High school | 6 (80) 1 (10) 3 (30) | 5 (62.5) 2 (25) 1 (12.5) |
| Taking L-DOPA as a single medication (n) | 6 | 5 |
| Taking L-DOPA with other medications (n) | 4 | 3 |
| Outcome Measure | HOME Group (n = 10) | CON Group (n = 8) | p-Value |
|---|---|---|---|
| Primary outcomes | |||
| MDS-UPDRS motor part (score) | 21.83 ± 7.99 | 23.17 ± 9.87 | 0.094 |
| MDS-UPDRS rigidity item (score) | 2.10 ± 0.67 | 2.20 ± 0.55 | 0.109 |
| Functional axial rotation–physical (cm) | 101.02 ± 73.50 | 98.37 ± 47.90 | 0.024 |
| Gait characteristics Foot rotation (deg.) Step width (cm) Step length (cm) Step time (s) Cadence (steps/min) Gait velocity (km/s) | 10.16 ± 8.77 12.10 ± 6.00 22.64 ± 12.39 1.05 ± 0.52 73.80 ± 8.63 1.04 ± 0.79 | 10.65 ± 7.10 11.63 ± 3.96 21.28 ± 13.04 1.30 ± 0.86 72.25 ± 7.76 0.94 ± 0.43 | 0.657 0.720 0.091 0.060 0.083 0.054 |
| Secondary outcomes | |||
| Functional Reach Test (cm) | 31.09 ± 10.99 | 29.45 ± 8.13 | 0.074 |
| Time Up and Go (s) | 17.86 ± 11.07 | 16.27 ± 8.16 | 0.067 |
| Gait speed (m/s) Normal speed Fast speed | 0.80 ± 0.33 1.03 ± 0.29 | 0.78 ± 0.17 1.04 ± 0.33 | 0.723 0.556 |
| Fall Efficacy Scale-International (score) | 20.11 ± 7.18 | 19.83 ± 6.97 | 0.689 |
| Outcome Measure | HOME Group (n = 10) | Change Score from Baseline | CON Group (n = 8) | Change Score from Baseline | p-Value |
|---|---|---|---|---|---|
| Primary outcomes | |||||
| MDS-UPDRS motor part (score) | 20.67 ± 8.25 | 1.16 ± 0.82 | 23.50 ± 10.62 | −0.33 ± 0.23 | 0.237 |
| MDS-UPDRS rigidity item (score) | 1.67 ± 0.71 | 0.43 ± 0.30 | 2.67 ± 0.52 | −0.47 ± 0.33 | 0.017 * |
| Functional axial rotation-physical (cm) | 120.79 ± 71.22 | −19.77 ± 13.98 | 78.84 ± 47.86 | 19.53 ± 13.81 | 0.059 |
| Gait characteristics Foot rotation (deg) Step width (cm) Step length (cm) Step time (s) Cadence (steps/min) Gait velocity (km/s) | 12.86 ± 6.53 13.20 ± 6.11 40.13 ± 17.76 1.46 ± 1.03 87.20 ± 6.96 1.88 ± 0.60 | −2.7 ± 1.91 −1.1 ± 0.78 −17.49 ± 12.37 −0.41 ± 0.29 −13.4 ± 9.48 −0.84 ± 0.59 | 11.53 ± 8.16 13.13 ± 4.29 22.04 ± 12.10 1.29 ± 0.65 83.38 ± 16.15 0.90 ± 0.55 | −0.88 ± 0.62 −1.5 ± 1.06 −0.76 ± 0.54 0.01 ± 0.01 −11.13 ± 7.87 0.04 ± 0.03 | 0.534 0.964 0.033 * 0.059 0.350 0.023 * |
| Secondary outcomes | |||||
| Functional Reach Test (cm) | 33.62 ± 8.78 | −2.53 ± 1.79 | 30.33 ± 9.51 | −0.88 ± 0.62 | 0.723 |
| Time Up and Go (s) | 16.49 ± 6.58 | 1.37 ± 0.97 | 15.27 ± 5.82 | 1 ± 0.71 | 0.960 |
| Gait speed (m/s) Normal speed Fast speed | 0.99 ± 0.35 1.13 ± 0.39 | −0.19 ± 0.13 −0.1 ± 0.07 | 0.79 ± 0.18 0.99 ± 0.17 | −0.01 ± 0.01 0.05 ± 0.04 | 0.239 0.637 |
| Fall Efficacy Scale-International (score) | 18.56 ± 7.57 | 1.55 ± 1.10 | 22.17 ± 7.52 | −2.34 ± 1.65 | 0.047 * |
| The global rating of change (score) | 1 ± 1.58 | 0.5 ± 1.76 | 0.361 |
| Outcome Measure | Baseline | After 10-Week Exercise Regime | p-Value |
|---|---|---|---|
| Primary outcomes | |||
| MDS-UPDRS motor part (score) | 21.83 ± 7.99 | 20.67 ± 8.25 | 0.196 |
| MDS-UPDRS rigidity item (score) | 2.10 ± 0.67 | 1.67 ± 0.71 | 0.057 |
| Functional axial rotation-physical (cm) | 101.02 ± 73.50 | 120.79 ± 71.22 | 0.008 * |
| Gait characteristics Foot rotation (deg.) Step width (cm) Step length (cm) Step time (sec) Cadence (steps/min) Gait velocity (km/s) | 10.16 ± 8.77 12.10 ± 6.00 22.64 ± 12.39 1.05 ± 0.52 73.80 ± 8.63 1.04 ± 0.79 | 12.89 ± 6.53 13.20 ± 6.11 40.13 ± 17.76 1.26 ± 1.03 87.20 ± 6.96 1.88 ± 0.60 | 0.053 0.380 0.041 * 0.445 0.446 0.085 |
| Secondary outcomes | |||
| Functional Reach Test (cm) | 31.09 ± 10.99 | 33.62 ± 8.78 | 0.012 * |
| Time Up and Go (s) | 17.86 ± 11.07 | 16.49 ± 6.58 | 0.263 |
| Gait speed (m/s) Normal speed Fast speed | 0.80 ± 0.33 1.03 ± 0.29 | 0.99 ± 0.35 1.13 ± 0.39 | 0.058 0.008 * |
| Fall Efficacy Scale-International (score) | 20.11 ± 7.18 | 18.56 ± 7.57 | 0.012 * |
| The global rating of change (score) | - | 1 ± 1.58 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khobkhun, F.; Suwannarat, J.; Pheungphrarattanatrai, A.; Niemrungruang, K.; Techataweesub, S.; Khacharoen, S.; Ajjimaporn, A.; Srivanitchapoom, P.; Richards, J. The Effects of a 10-Week Home-Based Exercise Programme in Individuals with Parkinson’s Disease during the COVID-19 Pandemic: A Pilot Study. Appl. Sci. 2021, 11, 4518. https://doi.org/10.3390/app11104518
Khobkhun F, Suwannarat J, Pheungphrarattanatrai A, Niemrungruang K, Techataweesub S, Khacharoen S, Ajjimaporn A, Srivanitchapoom P, Richards J. The Effects of a 10-Week Home-Based Exercise Programme in Individuals with Parkinson’s Disease during the COVID-19 Pandemic: A Pilot Study. Applied Sciences. 2021; 11(10):4518. https://doi.org/10.3390/app11104518
Chicago/Turabian StyleKhobkhun, Fuengfa, Jinjuta Suwannarat, Anuchai Pheungphrarattanatrai, Kanjana Niemrungruang, Sakaowrat Techataweesub, Suweena Khacharoen, Amornpan Ajjimaporn, Prachaya Srivanitchapoom, and Jim Richards. 2021. "The Effects of a 10-Week Home-Based Exercise Programme in Individuals with Parkinson’s Disease during the COVID-19 Pandemic: A Pilot Study" Applied Sciences 11, no. 10: 4518. https://doi.org/10.3390/app11104518
APA StyleKhobkhun, F., Suwannarat, J., Pheungphrarattanatrai, A., Niemrungruang, K., Techataweesub, S., Khacharoen, S., Ajjimaporn, A., Srivanitchapoom, P., & Richards, J. (2021). The Effects of a 10-Week Home-Based Exercise Programme in Individuals with Parkinson’s Disease during the COVID-19 Pandemic: A Pilot Study. Applied Sciences, 11(10), 4518. https://doi.org/10.3390/app11104518







