Novel Digital Technique to Analyze the Influence of the Operator Experience on the Accuracy of the Orthodontic Micro-Screws Placement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
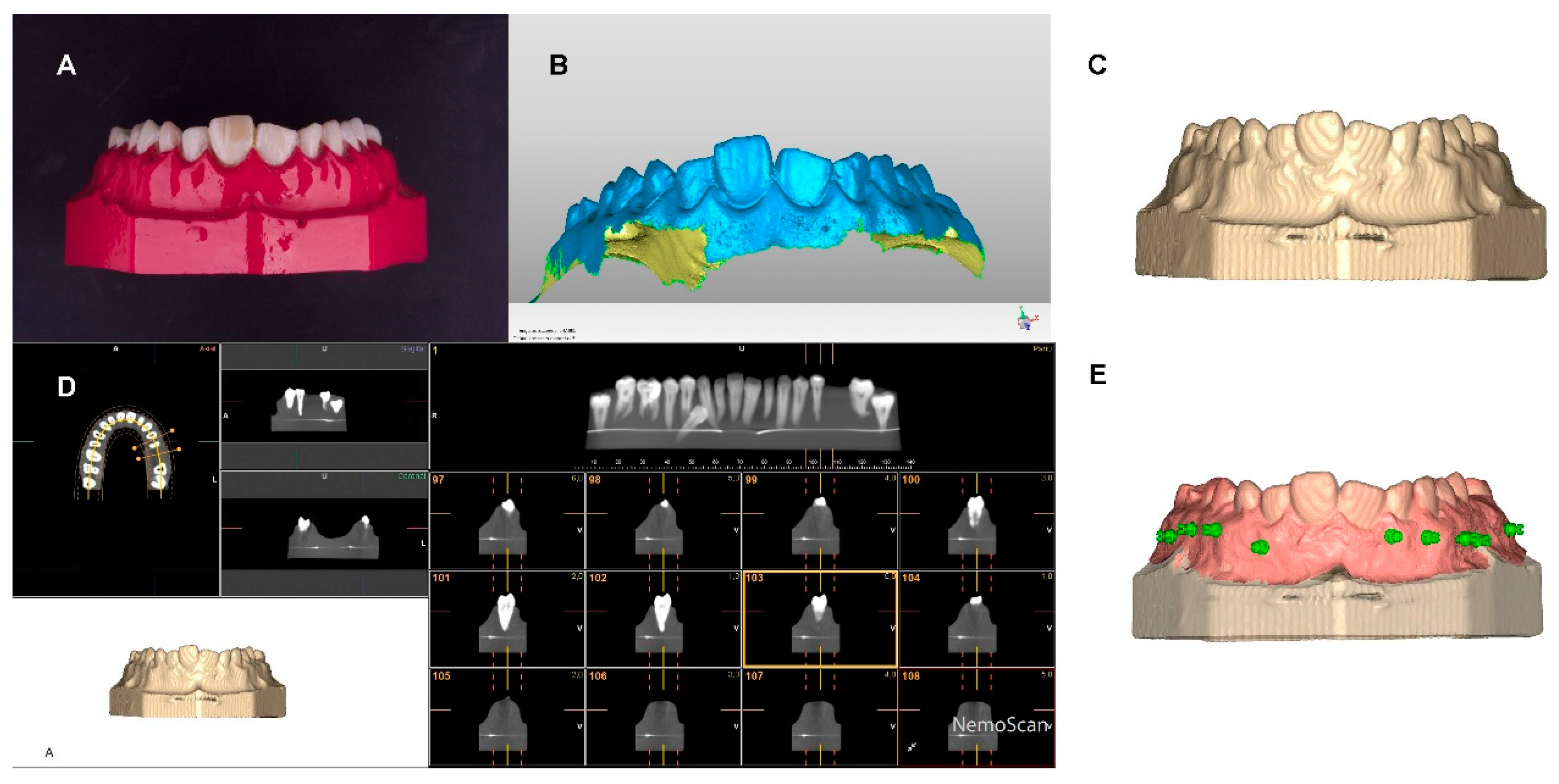
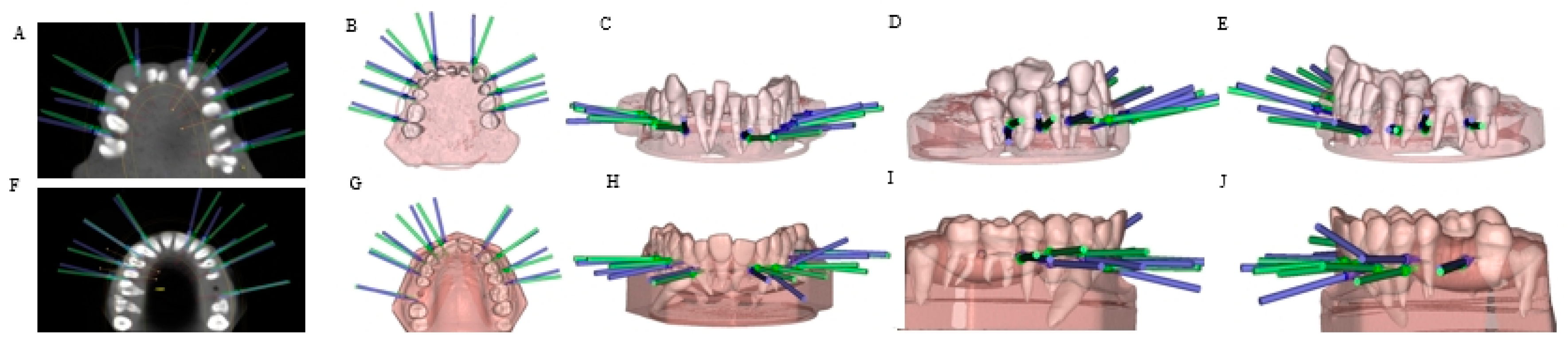
2.2. Experimental Procedure
2.3. Measurement Procedure
2.4. Statistical Tests
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Atalla, A.I.; Aboulfotouh, M.H.; Fahim, F.H.; Foda, M.Y. Effectiveness of orthodontic mini-screw implants in adult deep bite patients during incisor intrusion: A systematic review. Contemp Clin. Dent. 2020, 10, 372–381. [Google Scholar]
- Tseng, Y.-C.; Hsieh, C.-H.; Chen, C.-H.; Shen, Y.-S.; Huang, I.-Y.; Chen, C.-M. The application of mini-implants for orthodontic anchorage. Int. J. Oral Maxillofac. Surg. 2006, 35, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Jasoria, G.; Naik, V.R.; Manchanda, M.; Kalra, A.; Pai, V. Comparison between drill and drill free screws as a source of rigid orthodontic anchorage: A prospective clinical study. Int. J. Orthod. Milwaukee Wis. 2013, 24, 51–57. [Google Scholar]
- Mecenas, P.; Espinosa, D.G.; Cardoso, P.C.; Normando, D. Stainless steel or titanium mini-implants? Angle Orthod. 2020, 90, 587–597. [Google Scholar] [CrossRef] [Green Version]
- Yi, J.; Ge, M.; Li, M.; Li, C.; Li, Y.; Li, X.; Zhao, Z. Comparison of the success rate between self-drilling and self-tapping miniscrews: A systematic review and meta-analysis. Eur. J. Orthod. 2016, 39, 287–293. [Google Scholar] [CrossRef]
- Heidemann, W.; Gerlach, K.L.; Gröbel, K.-H.; Köllner, H.-G. Drill free screws: A new form of osteosynthesis screw. J. Cranio-Maxillofac. Surg. 1998, 26, 163–168. [Google Scholar] [CrossRef]
- Mohammed, H.; Wafaie, K.; Rizk, M.Z.; Almuzian, M.; Sosly, R.; Bearn, D.R. Role of anatomical sites and correlated risk factors on the survival of orthodontic miniscrew implants: A systematic review and meta-analysis. Prog. Orthod. 2018, 19, 36. [Google Scholar] [CrossRef] [Green Version]
- Lim, H.-J.; Eun, C.-S.; Cho, J.-H.; Lee, K.-H.; Hwang, H.-S. Factors associated with initial stability of miniscrews for orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 236–242. [Google Scholar] [CrossRef]
- Moon, C.-H.; Lee, D.-G.; Lee, H.-S.; Im, J.-S.; Baek, S.-H. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008, 78, 101–106. [Google Scholar] [CrossRef] [Green Version]
- Papageorgiou, S.N.; Zogakis, I.P.; Papadopoulos, M. Failure rates and associated risk factors of orthodontic miniscrew implants: A meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 577–595. [Google Scholar] [CrossRef]
- Park, H.-S.; Jeong, S.-H.; Kwon, O.-W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, A.; Motoyoshi, M.; Uchida, Y.; Shimizu, N. Root proximity and inclination of orthodontic mini-implants after placement: Cone-beam computed tomography evaluation. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Antoszewska, J.; Papadopoulos, M.A.; Park, H.-S.; Ludwig, B. Five-year experience with orthodontic miniscrew implants: A retrospective investigation of factors influencing success rates. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 158–159. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.-M.; Takano-Yamamoto, T. Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Cozzani, M.; Nucci, L.; Lupini, D.; Dolatshahizand, H.; Fazeli, D.; Barzkar, E.; Naeini, E.; Jamilian, A. The ideal insertion angle after immediate loading in Jeil, Storm, and Thunder miniscrews: A 3D-FEM study. Int. Orthod. 2020, 18, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Morea, C.; Hayek, J.E.; Oleskovicz, C.; Dominguez, G.C.; Chilvarquer, I. Precise insertion of orthodontic miniscrews with a stereolithographic surgical guide based on cone beam computed tomography data: A pilot study. Int. J. Oral Maxillofac. Implant. 2011, 26, 860–865. [Google Scholar]
- Asscherickx, K.; Vannet, B.V.; Wehrbein, H.; Sabzevar, M.M. Root repair after injury from mini-screw. Clin. Oral Implant. Res. 2005, 16, 575–578. [Google Scholar] [CrossRef]
- Raji, S.H.; Noorollahian, S.; Niknam, S.M. The effect of insertion angle on orthodontic mini-screw torque. Dent. Res. J. 2014, 11, 448–451. [Google Scholar]
- Wilmes, B.; Drescher, D. Impact of insertion depth and predrilling diameter on primary stability of orthodontic mini-implants. Angle Orthod. 2009, 79, 609–614. [Google Scholar] [CrossRef]
- Noble, J.; Karaiskos, N.E.; Hassard, T.H.; Hechter, F.J.; Wiltshire, W.A. Stress on bone from placement and removal of orthodontic miniscrews at different angulations. J. Clin. Orthod. JCO 2009, 43, 332–334. [Google Scholar]
- Perillo, L.; Jamilian, A.; Shafieyoon, A.; Karimi, H.; Cozzani, M. Finite element analysis of miniscrew placement in mandibular alveolar bone with varied angulations. Eur. J. Orthod. 2014, 37, 56–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poggio, P.M.; Incorvati, C.; Velo, S.; Carano, A. “Safe zones”: A guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006, 76, 191–197. [Google Scholar] [PubMed]
- Pickard, M.B.; Dechow, P.; Rossouw, P.E.; Buschang, P.H. Effects of miniscrew orientation on implant stability and resistance to failure. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Schnelle, M.A.; Beck, F.M.; Jaynes, R.M.; Huja, S.S. A radiographic evaluation of the availability of bone for placement of miniscrews. Angle Orthod. 2004, 74, 832–837. [Google Scholar] [PubMed]
- Tepedino, M.; Cornelis, M.; Chimenti, C.; Cattaneo, P. Correlation between tooth size-arch length discrepancy and interradicular distances measured on CBCT and panoramic radiograph: An evaluation for miniscrew insertion. Dent. Press J. Orthod. 2018, 23, 39.e1–39.e13. [Google Scholar] [CrossRef]
- Landin, M.; Jadhav, A.; Yadav, S.; Tadinada, A. A comparative study between currently used methods and small volume-cone beam tomography for surgical placement of mini implants. Angle Orthod. 2014, 85, 446–453. [Google Scholar] [CrossRef] [Green Version]
- Alsamak, S.; Gkantidis, N.; Bitsanis, E.; Christou, P. Assessment of potential orthodontic mini-implant insertion sites based on anatomical hard tissue parameters: A systematic review. Int. J. Oral Maxillofac. Implant. 2012, 27, 875–887. [Google Scholar]
- Shafaee, H.; Ghanbarzadeh, M.; Heravi, F.; Abrishamchi, R.; Ghazi, N.; Heravi, P.; Ghanbarzadeh, H. Cementum and dentin repair following root damage caused by the insertion of self-tapping and self-drilling miniscrews. J. Orthod. Sci. 2017, 6, 91–96. [Google Scholar] [CrossRef]
- Szalma, J.; Gurdán, Z. Evaluation of the success and complication rates of self-drilling orthodontic mini-implants. Niger. J. Clin. Pr. 2018, 21, 546–552. [Google Scholar] [CrossRef]
- Chen, Y.; Shin, H.-I.; Kyung, H.-M. Biomechanical and histological comparison of self-drilling and self-tapping orthodontic microimplants in dogs. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 44–50. [Google Scholar] [CrossRef]
- Kim, J.-W.; Ahn, S.-J.; Chang, Y.-I. Histomorphometric and mechanical analyses of the drill-free screw as orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Deng, F.; Wang, Z.; Zhao, Z.; Wang, J. Biomechanical and histomorphometric analyses of the osseointegration of microscrews with different surgical techniques in beagle dogs. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2008, 106, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Simurda, T.; Dobrotova, M.; Skornova, I.; Sokol, J.; Kubisz, P.; Stasko, J. Successful use of a highly purified plasma von Willebrand factor concentrate containing little FVIII for the long-term prophylaxis of severe (type 3) von Willebrand’s disease. Semin. Thromb. Hemost. 2017, 43, 639–641. [Google Scholar] [PubMed] [Green Version]
- Kim, S.-H.; Kook, Y.-A.; Jeong, D.-M.; Lee, W.; Chung, K.-R.; Nelson, G. Clinical application of accelerated osteogenic orthodontics and partially osseointegrated mini-implants for minor tooth movement. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 431–439. [Google Scholar] [CrossRef]
- Ziebura, T.; Flieger, S.; Wiechmann, D. Mini-implants in the palatal slope—A retrospective analysis of implant survival and tissue reaction. Head Face Med. 2012, 8, 32. [Google Scholar] [CrossRef] [Green Version]
- De Padua, V.; Romeo, U.; Santoro, C.; Bosco, R.; Baldacci, E.; Ferretti, A.; Malaspina, F.; Mazzucconi, M.G.; Gaglioti, D. Dental invasive procedures in von Willebrand disease outpatients treated with high purity FVIII/VWF complex concentrate (Fanhdi®): Experience of a single center. Heliyon 2020, 6, e03426. [Google Scholar] [CrossRef]
- Reich, W.; Kriwalsky, M.S.; Wolf, H.H.; Schubert, J. Bleeding complications after oral surgery in outpatients with compromised haemostasis: Incidence and management. Oral Maxillofac. Surg. 2009, 13, 73–77. [Google Scholar] [CrossRef]

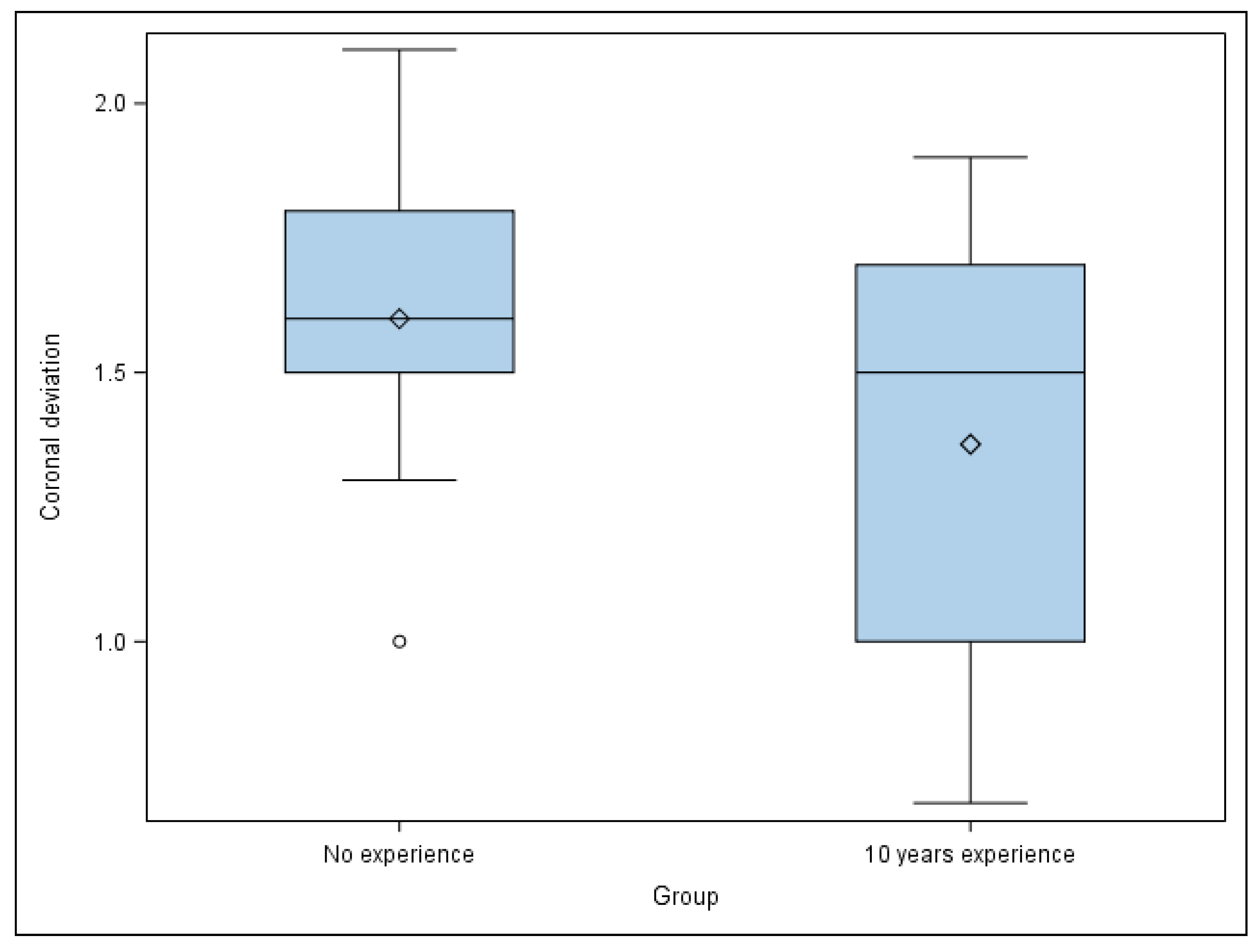
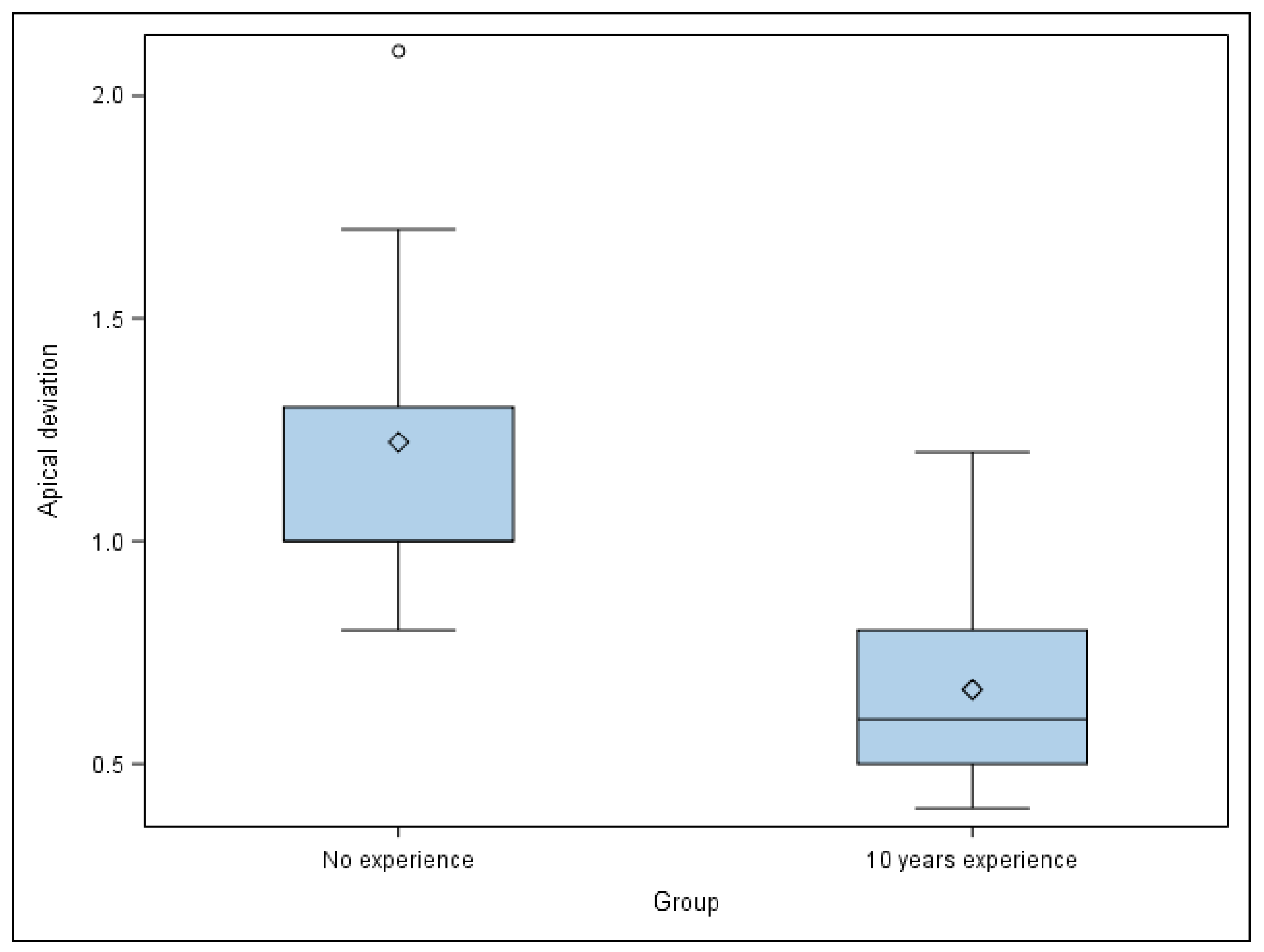
| n | Mean | SD | Minimum | Maximum | ||
|---|---|---|---|---|---|---|
| Coronal | 10 years’ experience | 30 | 1.37 a | 0.43 | 0.70 | 1.90 |
| No experience | 30 | 1.60 a | 0.34 | 1.00 | 2.10 | |
| Apical | 10 years’ experience | 30 | 0.67 a | 0.25 | 0.40 | 1.20 |
| No experience | 30 | 1.22 b | 0.42 | 0.80 | 2.10 | |
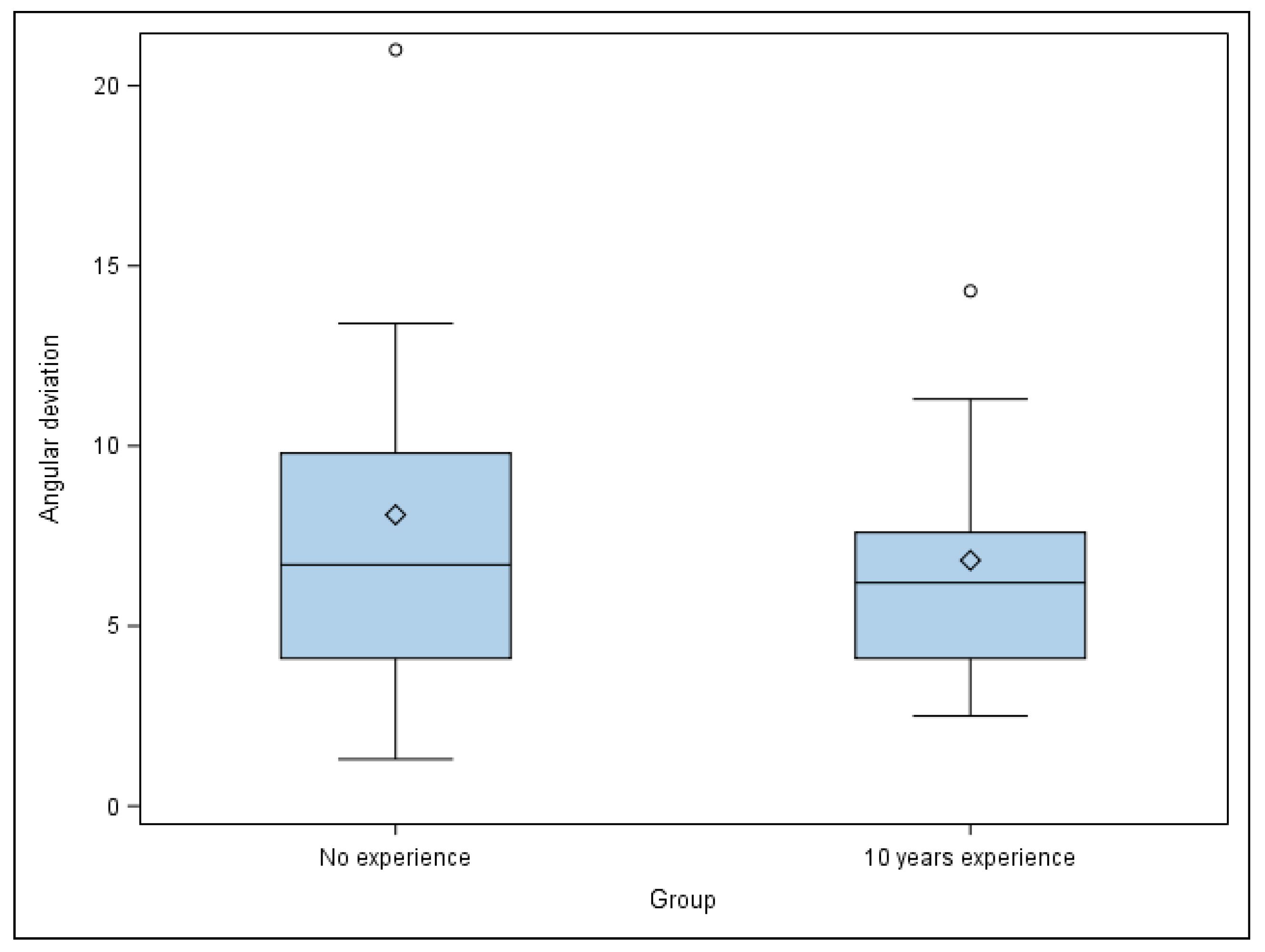
| Angular | 10 years´ experience | 30 | 6.82 a | 3.85 | 2.50 | 14.30 |
| No experience | 30 | 8.09 a | 6.00 | 1.30 | 21.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bufalá Pérez, M.; O’Connor Esteban, M.; Zubizarreta-Macho, Á.; Riad Deglow, E.; Hernández Montero, S.; Abella Sans, F.; Albaladejo Martínez, A. Novel Digital Technique to Analyze the Influence of the Operator Experience on the Accuracy of the Orthodontic Micro-Screws Placement. Appl. Sci. 2021, 11, 400. https://doi.org/10.3390/app11010400
Bufalá Pérez M, O’Connor Esteban M, Zubizarreta-Macho Á, Riad Deglow E, Hernández Montero S, Abella Sans F, Albaladejo Martínez A. Novel Digital Technique to Analyze the Influence of the Operator Experience on the Accuracy of the Orthodontic Micro-Screws Placement. Applied Sciences. 2021; 11(1):400. https://doi.org/10.3390/app11010400
Chicago/Turabian StyleBufalá Pérez, María, Miriam O’Connor Esteban, Álvaro Zubizarreta-Macho, Elena Riad Deglow, Sofía Hernández Montero, Francesc Abella Sans, and Alberto Albaladejo Martínez. 2021. "Novel Digital Technique to Analyze the Influence of the Operator Experience on the Accuracy of the Orthodontic Micro-Screws Placement" Applied Sciences 11, no. 1: 400. https://doi.org/10.3390/app11010400
APA StyleBufalá Pérez, M., O’Connor Esteban, M., Zubizarreta-Macho, Á., Riad Deglow, E., Hernández Montero, S., Abella Sans, F., & Albaladejo Martínez, A. (2021). Novel Digital Technique to Analyze the Influence of the Operator Experience on the Accuracy of the Orthodontic Micro-Screws Placement. Applied Sciences, 11(1), 400. https://doi.org/10.3390/app11010400






