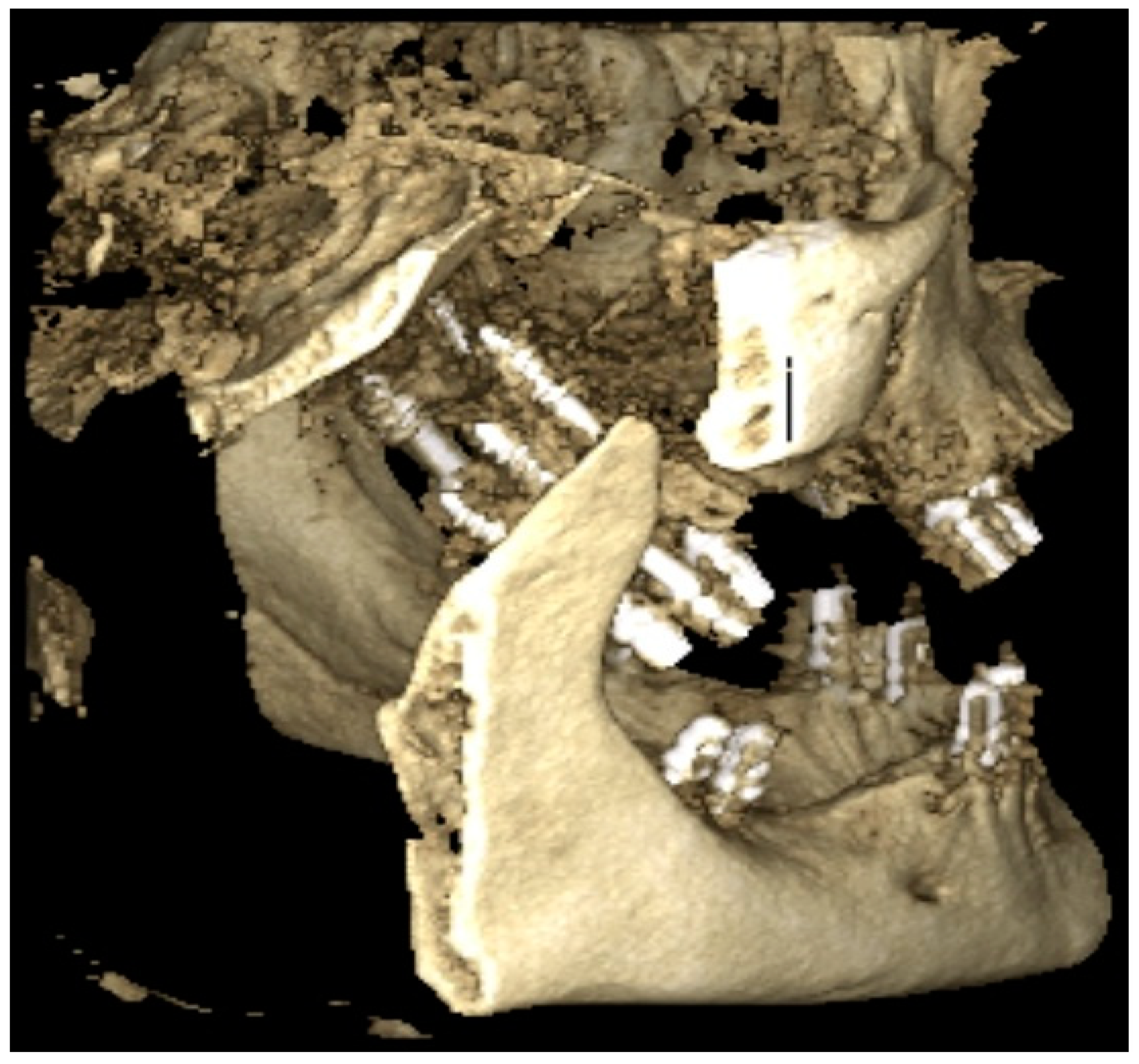
Three-Dimensional Determination of the Fusion Zone between the Distal Maxilla and the Pterygoid Plate of the Sphenoid Bone and Considerations for Implant Treatment Procedure
Abstract
1. Introduction
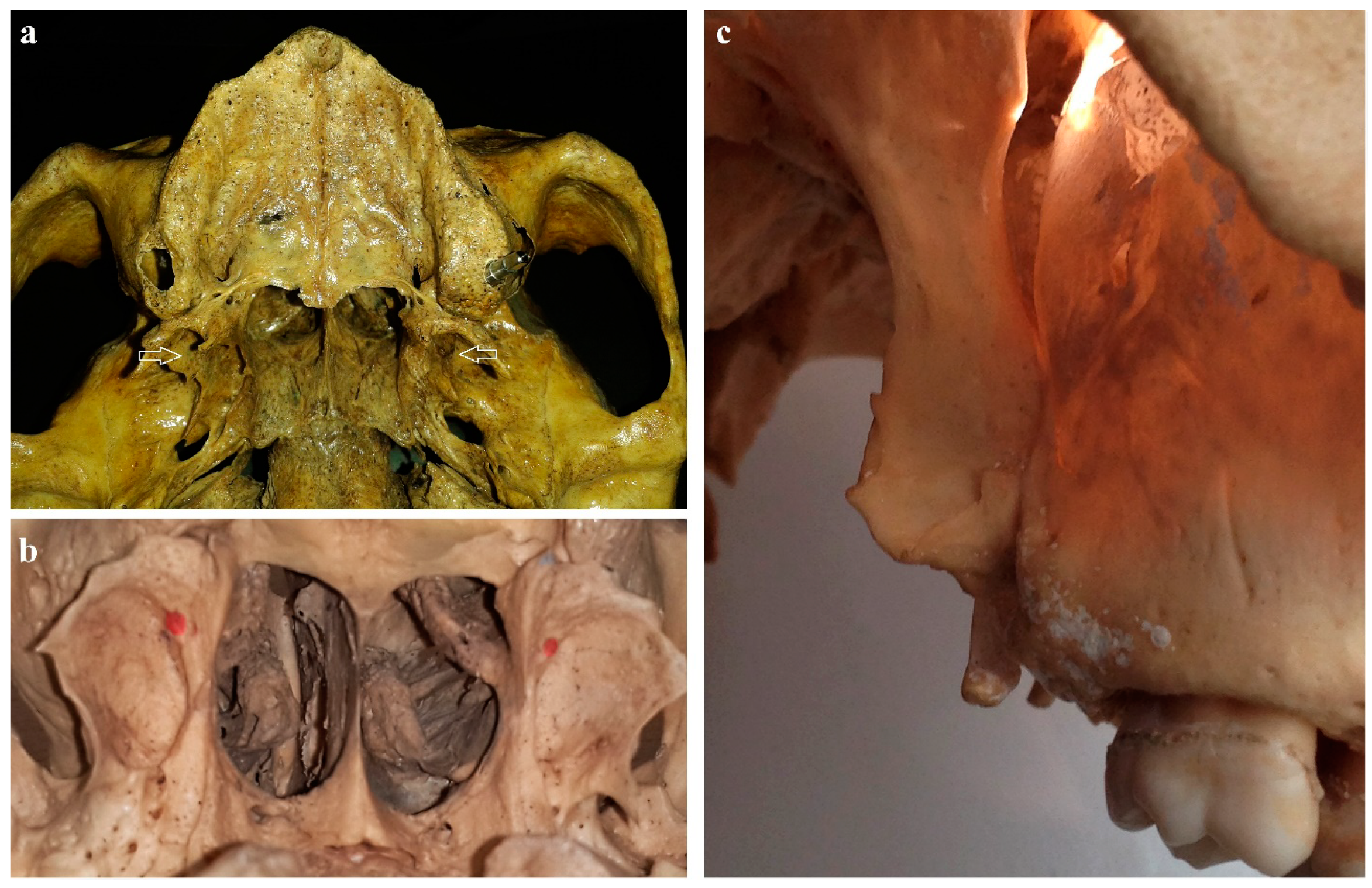
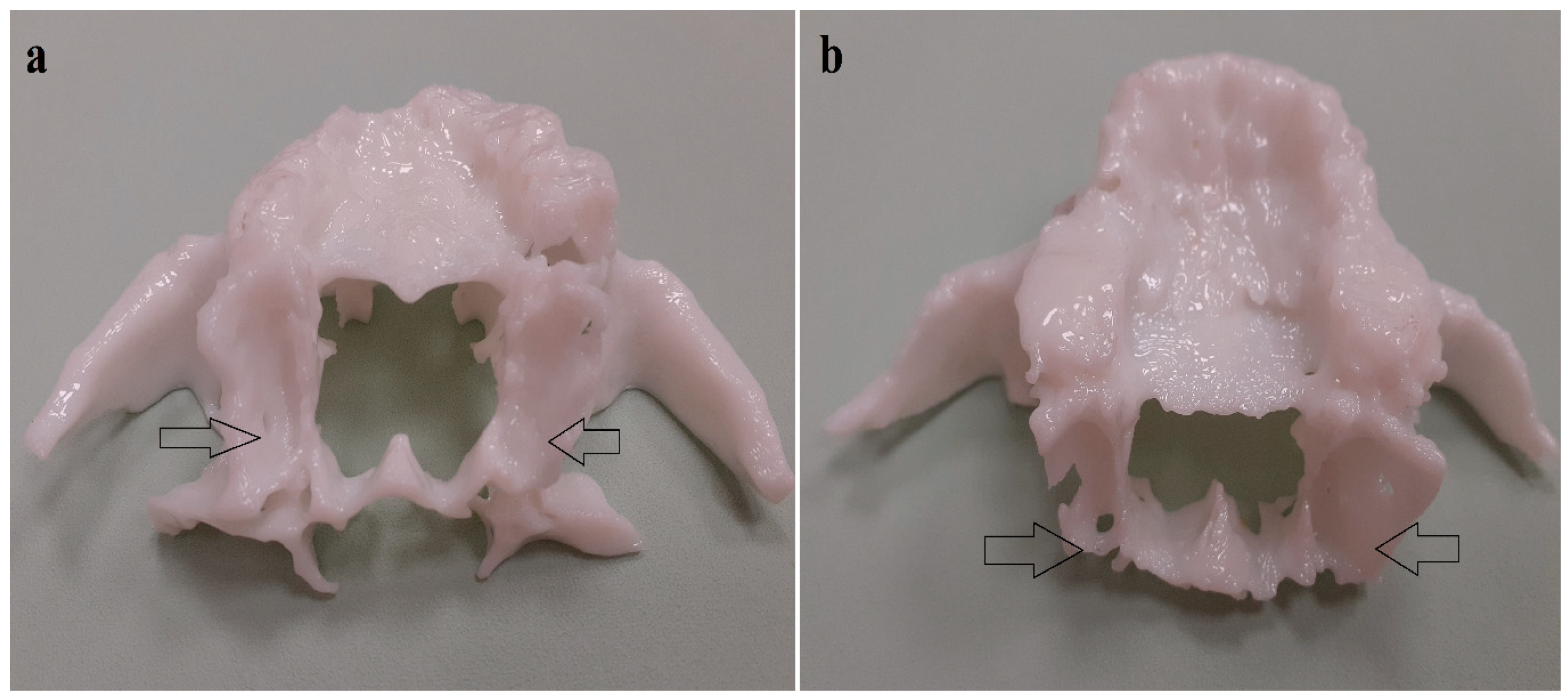
2. Materials and Methods
2.1. Study Group
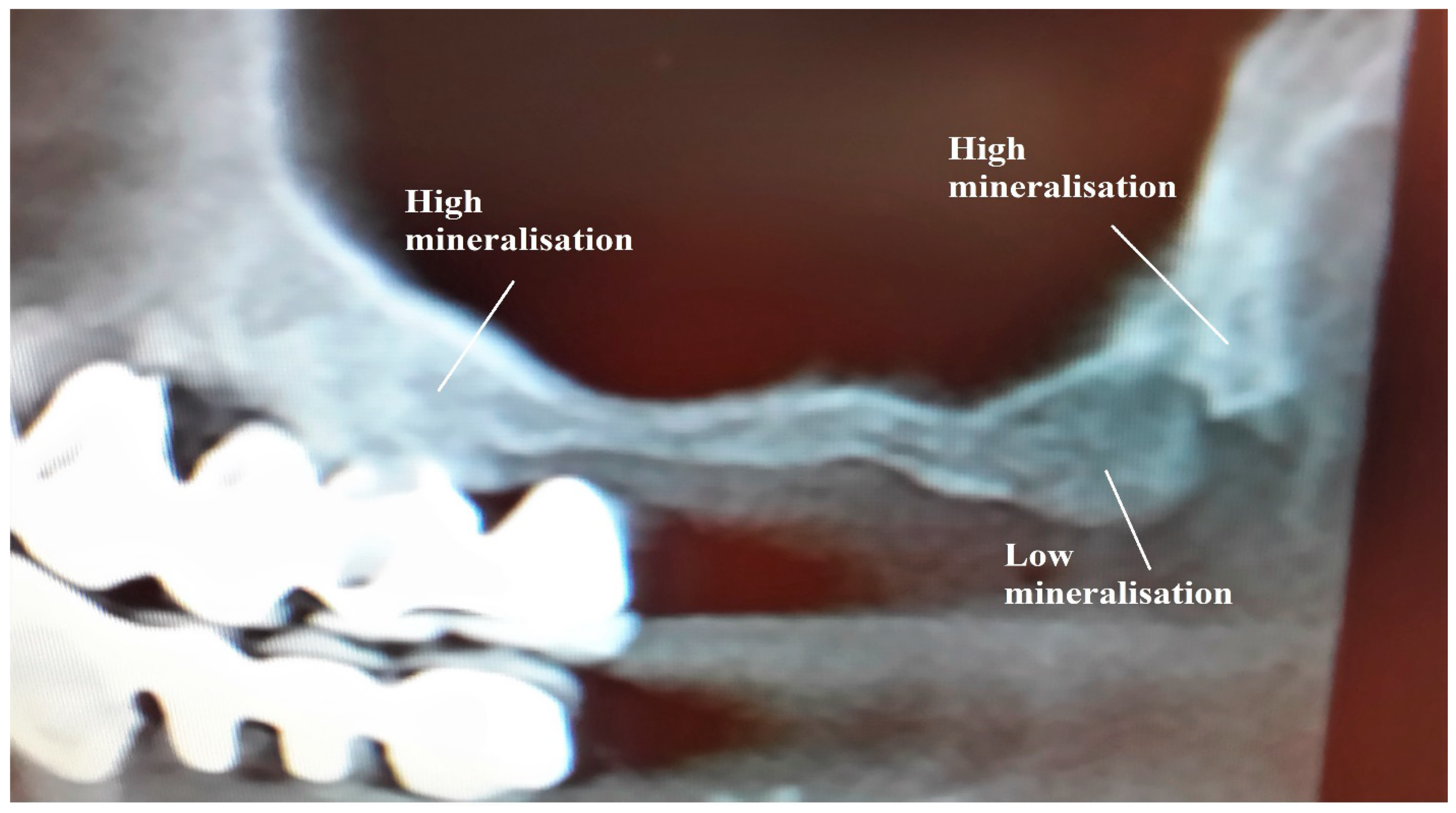
2.2. Measurements
2.3. Comparisons and Statistical Analysis
3. Results
3.1. Anatomical Measurements
3.2. Comparison between Right and Left Side
3.3. Comparison between Female and Male Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lindhe, J.; Bressan, E.; Cecchinato, D.; Corra, E.; Toia, M.; Liljenberg, B. Bone tissue in different parts of the edentulous maxilla and mandible. Clin. Oral Implants Res. 2013, 24, 372. [Google Scholar] [PubMed]
- Rodríguez, X.; Lucas-Taulé, E.; Elnayef, B.; Altuna, P.; Gargallo-Albiol, J.; Peñarrocha Diago, M.; Hernandez-Alfaro, F. Anatomical and radiological approach to pterygoid implants: A cross-sectional study of 202 conebeam computed tomography examinations. Int. J. Oral. Maxillofac. Surg. 2016, 45, 636. [Google Scholar] [CrossRef] [PubMed]
- Hjørting-Hansen, E.; Laney, W.R.; Broggini, N.; Buser, D.; Cochran, D.L.; Garcia, L.T. Glossary of Oral and Maxillofacial Implants; Quintessence Publishing Ltd.: Berlin, Germany, 2007. [Google Scholar]
- Reiser, G.M. Implant use in the tuberosity, pterygoid, and palatine region. Anatomic and surgical consideration. Implant Ther. Clin. Approaches Evid. Success. 1998, 2, 197–206. [Google Scholar]
- Ihde, S. Principles of BOI; Springer: Berlin/Heidelberg, Germany, 2004; ISBN 3-540-21665-0. [Google Scholar]
- Ihde, S.; Ihde, A. Immediate Loading, 2nd ed.; International Implant Foundation Publishing: Munich, Germany, 2012; ISBN 978-3-9851468-3-5. [Google Scholar]
- Lee, S.P.; Paik, K.S.; Kim, M.K. Anatomical study of the pyramidal process of the palatine bone in relation to implant placement in the posterior maxilla. J. Oral Rehabil. 2001, 28, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Manzanera, E.; Llorca, P.; Manzanera, D.; García-Sanz, V.; Sada, V.; Paredes-Gallardo, V. Anatomical study of the maxillary tuberosity using cone beam computed tomography. Oral Radiol. 2018, 34, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Linkow, L. The pterygoid extension implant. J. Miss. Dent. Assoc. 1972, V28, 10–19. [Google Scholar]
- Tulasne, J.F. Implant treatment of missing posterior dentition. In The Branemark Osseointegrated Implant; Quintessence: Chicago, IL, USA, 1989; pp. 103–116. [Google Scholar]
- Tulasne, J.F. Osseointegrated fixtures in the pterygoid region. In Advanced Osseointegration Surgery Applications in the Maxillofacial Region; Quintessence: Chicago, IL, USA, 1992; pp. 182–188. [Google Scholar]
- Balshi, T.J.; Wolfinger, G.J.; Balshi, S.F., 2nd. Analysis of 356 pterygomaxillary implants in edentulous arches for fixed prosthesis anchorage. Int. J. Oral Maxillofac. Implants 1999, 14, 398–406. [Google Scholar] [PubMed]
- Ihde, S. Fixed Prosthodontics in Skeletal Class III Patients with partially edentulous jaws and age related prognathism: The basal osseointegration procedure. Implant Dent. 1999, 8, 241. [Google Scholar] [CrossRef] [PubMed]
- Graves, S.L. The pterygoid plate implant: A solution for restoring the posterior maxilla. Int. J. Periodontics Restor. Dent. 1994, 14, 512–523. [Google Scholar]
- Rodriguez, X.; Lucas-Taule, E.; Elnayef, B. Anatomical and radiological approach to pterygoid implants: A cross-sectional study of 202 cone beam computed tomography examinations. Int. J. Oral Maxillofac. Surg. 2016, 45, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, X.; Mendez, V.; Vela, X.; Segala, M. Modified surgical protocol for placing implants in the pterygomaxillary region: Clinical and radiologic study of 454 implants. Int. J. Oral Maxillofac. Implant 2012, 27, 1547–1553. [Google Scholar]
- Wesemann, C.; Muallah, J.; Mah, J.; Bumann, A. Accuracy and efficiency of full-arch digitalization and 3D printing: A comparison between desktop model scanners, an intraoral scanner, a CBCT model scan, and stereolithographic 3Dprinting. Quintessence Int. 2017, 48, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Radic, J.; Patcas, R.; Stadlinger, B.; Wiedemeier, D.; Rücker, M.; Giacomelli-Hiestand, B. Do we need CBCTs for sufficient diagnostics?-dentist-related factors. Int. J. Implant Dent. 2018, 4, 37. [Google Scholar] [CrossRef] [PubMed]
- Bell, C.K.; Sahl, E.F.; Kim, Y.J.; Rice, D.D. Accuracy of Implants Placed with Surgical Guides: Thermoplastic Versus 3D Printed. Int. J. Periodontics Restor. Dent. 2018, 38, 113–119. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Aver | SD | Range | Norm | |||
|---|---|---|---|---|---|---|---|
| Min | Max | Aver − 1.96 × SD | Aver + 1.96 × SD | ||||
| no division | lateral (mm) | 18.74 | 3.2 | 6.68 | 25.44 | 12.46 | 25.01 |
| medial (mm) | 18.73 | 3.02 | 8.64 | 24.39 | 12.82 | 24.65 | |
| rostral (mm) | 5.99 | 0.9 | 3.57 | 8.24 | 4.22 | 7.75 | |
| caudal (mm) | 8.92 | 1.37 | 5.77 | 11.75 | 6.23 | 11.61 | |
| area (mm2) | 157.77 | 39.07 | 45.36 | 328.8 | 81.18 | 234.36 | |
| line-1 longitudinal (mm) | 20.36 | 3.03 | 7.79 | 26.54 | 14.41 | 26.31 | |
| line-2 transverse (mm) | 7.79 | 0.92 | 5.42 | 9.79 | 5.99 | 9.59 | |
| right body side | R lateral (mm) | 18.88 | 3.51 | 6.68 | 25.44 | 12.01 | 25.76 |
| R medial (mm) | 18.67 | 3.26 | 8.64 | 23.59 | 12.29 | 25.06 | |
| R rostral (mm) | 5.99 | 0.99 | 3.57 | 7.99 | 4.06 | 7.93 | |
| R caudal (mm) | 8.86 | 1.30 | 5.83 | 11.19 | 6.31 | 11.41 | |
| R area (mm2) | 160.06 | 44.68 | 45.36 | 328.8 | 72.48 | 247.63 | |
| R line-1 longitudinal (mm) | 20.51 | 3.38 | 7.79 | 26.21 | 13.89 | 27.12 | |
| R line-2 transverse (mm) | 7.82 | 0.93 | 5.87 | 9.42 | 6.00 | 9.63 | |
| left body side | L lateral (mm) | 18.59 | 2.88 | 6.83 | 25.05 | 12.95 | 24.24 |
| L medial (mm) | 18.79 | 2.78 | 10.0 | 24.39 | 13.35 | 24.24 | |
| L rostral (mm) | 5.98 | 0.81 | 4.52 | 8.24 | 4.39 | 7.57 | |
| L caudal (mm) | 8.98 | 1.45 | 5.77 | 11.75 | 6.14 | 11.82 | |
| L area (mm2) | 155.48 | 32.69 | 48.74 | 234.96 | 91.41 | 219.55 | |
| L line-1 longitudinal (mm) | 20.21 | 2.66 | 9.11 | 26.54 | 14.99 | 25.44 | |
| L line-2 transverse (mm) | 7.77 | 0.92 | 5.42 | 9.97 | 5.97 | 9.57 | |
| female | F lateral (mm) | 18.86 | 2.75 | 12.05 | 22.67 | 13.48 | 24.24 |
| F medial (mm) | 18.92 | 2.60 | 9.92 | 23.4 | 13.83 | 24.01 | |
| F rostral (mm) | 5.85 | 0.77 | 4.0 | 7.5 | 4.34 | 7.36 | |
| F caudal (mm) | 9.04 | 1.46 | 5.77 | 11.75 | 6.18 | 11.89 | |
| F area (mm2) | 164.14 | 43.78 | 78.18 | 328.8 | 78.34 | 249.94 | |
| F line-1 longitudinal (mm) | 20.62 | 2.47 | 13.21 | 25.24 | 15.77 | 25.47 | |
| F line-2 transverse (mm) | 7.83 | 0.94 | 5.96 | 9.97 | 5.99 | 9.67 | |
| male | M lateral (mm) | 19.47 | 2.95 | 15.31 | 25.44 | 13.69 | 25.25 |
| M medial (mm) | 18.78 | 3.26 | 12.63 | 24.39 | 12.39 | 25.17 | |
| M rostral (mm) | 6.01 | 1.03 | 3.57 | 8.24 | 4.00 | 8.02 | |
| M caudal (mm) | 9.37 | 1.17 | 7.57 | 11.19 | 7.08 | 11.67 | |
| M area (mm2) | 166.15 | 27.86 | 103.2 | 234.96 | 111.55 | 220.74 | |
| M line-1 longitudinal (mm) | 21.05 | 2.74 | 16.4 | 26.54 | 15.68 | 26.43 | |
| M line-2 transverse (mm) | 8.22 | 0.66 | 6.79 | 9.42 | 6.92 | 9.52 | |
| female; right side | FR lateral (mm) | 18.98 | 3.16 | 12.05 | 22.67 | 12.79 | 25.17 |
| FR medial (mm) | 18.81 | 3.08 | 9.92 | 23.4 | 12.77 | 24.84 | |
| FR rostral (mm) | 5.79 | 0.83 | 4.0 | 7.15 | 4.16 | 7.41 | |
| FR caudal (mm) | 9.00 | 1.33 | 6.86 | 11.0 | 6.39 | 11.62 | |
| FR area (mm2) | 170.55 | 55.72 | 78.18 | 328.8 | 61.35 | 279.76 | |
| FR line-1 longitudinal (mm) | 20.76 | 2.98 | 13.21 | 25.24 | 14.92 | 26.61 | |
| FR line-2 transverse (mm) | 7.81 | 0.88 | 5.96 | 9.05 | 6.08 | 9.54 | |
| female; left side | FL lateral (mm) | 18.75 | 2.31 | 13.14 | 21.07 | 14.22 | 23.28 |
| FL medial (mm) | 19.03 | 2.05 | 15.68 | 22.36 | 15.01 | 23.05 | |
| FL rostral (mm) | 5.91 | 0.72 | 5.07 | 7.5 | 4.50 | 7.32 | |
| FL caudal (mm) | 9.07 | 1.59 | 5.77 | 11.75 | 5.95 | 12.19 | |
| FL area (mm2) | 157.73 | 26.63 | 117.05 | 212.11 | 105.53 | 209.92 | |
| FL line-1 longitudinal (mm) | 20.48 | 1.88 | 16.85 | 22.63 | 16.80 | 24.16 | |
| FL line-2 transverse (mm) | 7.86 | 1.01 | 6.36 | 9.97 | 5.88 | 9.83 | |
| male; right side | MR lateral (mm) | 19.64 | 3.35 | 15.31 | 25.44 | 13.08 | 26.21 |
| MR medial (mm) | 18.53 | 3.33 | 12.8 | 23.59 | 12.01 | 25.04 | |
| MR rostral (mm) | 6.04 | 1.18 | 3.57 | 7.76 | 3.74 | 8.35 | |
| MR caudal (mm) | 9.28 | 1.14 | 7.57 | 11.19 | 7.03 | 11.52 | |
| MR area (mm2) | 163.61 | 26.72 | 103.2 | 210.1 | 111.24 | 215.99 | |
| MR line-1 longitudinal (mm) | 21.21 | 2.95 | 16.4 | 26.21 | 15.42 | 27.00 | |
| MR line-2 transverse (mm) | 8.25 | 0.84 | 6.79 | 9.42 | 6.61 | 9.90 | |
| male; left side | ML lateral (mm) | 19.30 | 2.54 | 15.63 | 25.05 | 14.33 | 24.27 |
| ML medial (mm) | 19.03 | 3.23 | 12.63 | 24.39 | 12.70 | 25.37 | |
| ML rostral (mm) | 5.98 | 0.87 | 5.17 | 8.24 | 4.28 | 7.69 | |
| ML caudal (mm) | 9.47 | 1.21 | 7.76 | 11.01 | 7.09 | 11.85 | |
| ML area (mm2) | 168.68 | 29.23 | 131.88 | 234.96 | 111.39 | 225.97 | |
| ML line-1 longitudinal (mm) | 20.90 | 2.56 | 17.87 | 26.54 | 15.87 | 25.92 | |
| ML line-2 transverse (mm) | 8.18 | 0.43 | 7.55 | 8.74 | 7.33 | 9.02 | |
| No Division | Female | Male | |
|---|---|---|---|
| lateral | 0.59 1 | 0.75 1 | 0.67 1 |
| medial | 0.81 1 | 0.74 1 | 0.57 2 |
| rostral | 0.93 1 | 0.53 1 | 0.82 1 |
| caudal | 0.60 1 | 0.85 2 | 0.54 1 |
| area | 0.48 1 | 0.26 1 | 0.51 1 |
| line-1 longitudinal | 0.57 1 | 0.66 1 | 0.68 1 |
| line-2 transverse | 0.76 1 | 0.85 1 | 0.68 1 |
| No Division | Left Side | Right Side | |
|---|---|---|---|
| lateral | 0.25 1 | 0.39 1 | 0.44 1 |
| medial | 0.80 1 | 0.99 2 | 0.74 1 |
| rostral | 0.33 1 | 0.73 1 | 0.34 2 |
| caudal | 0.18 1 | 0.29 2 | 0.41 2 |
| area | 0.77 1 | 0.14 2 | 0.56 1 |
| line-1 longitudinal | 0.38 1 | 0.48 1 | 0.57 1 |
| line-2 transverse | 0.01 1 | 0.13 2 | 0.57 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ihde, S.; Pałka, Ł.; Jarząb, S.; Janeczek, M.; Goździewska-Harłajczuk, K.; Klećkowska-Nawrot, J.; Janus, I.; Dobrzyński, M. Three-Dimensional Determination of the Fusion Zone between the Distal Maxilla and the Pterygoid Plate of the Sphenoid Bone and Considerations for Implant Treatment Procedure. Appl. Sci. 2021, 11, 30. https://doi.org/10.3390/app11010030
Ihde S, Pałka Ł, Jarząb S, Janeczek M, Goździewska-Harłajczuk K, Klećkowska-Nawrot J, Janus I, Dobrzyński M. Three-Dimensional Determination of the Fusion Zone between the Distal Maxilla and the Pterygoid Plate of the Sphenoid Bone and Considerations for Implant Treatment Procedure. Applied Sciences. 2021; 11(1):30. https://doi.org/10.3390/app11010030
Chicago/Turabian StyleIhde, Stefan, Łukasz Pałka, Sławomir Jarząb, Maciej Janeczek, Karolina Goździewska-Harłajczuk, Joanna Klećkowska-Nawrot, Izabela Janus, and Maciej Dobrzyński. 2021. "Three-Dimensional Determination of the Fusion Zone between the Distal Maxilla and the Pterygoid Plate of the Sphenoid Bone and Considerations for Implant Treatment Procedure" Applied Sciences 11, no. 1: 30. https://doi.org/10.3390/app11010030
APA StyleIhde, S., Pałka, Ł., Jarząb, S., Janeczek, M., Goździewska-Harłajczuk, K., Klećkowska-Nawrot, J., Janus, I., & Dobrzyński, M. (2021). Three-Dimensional Determination of the Fusion Zone between the Distal Maxilla and the Pterygoid Plate of the Sphenoid Bone and Considerations for Implant Treatment Procedure. Applied Sciences, 11(1), 30. https://doi.org/10.3390/app11010030









