In Vitro Accuracy of Static Guided Implant Surgery Measured by Optical Scan: Examining the Impact of Operator Experience
Abstract
:1. Introduction
2. Materials and Methods
2.1. Operator Enrollment
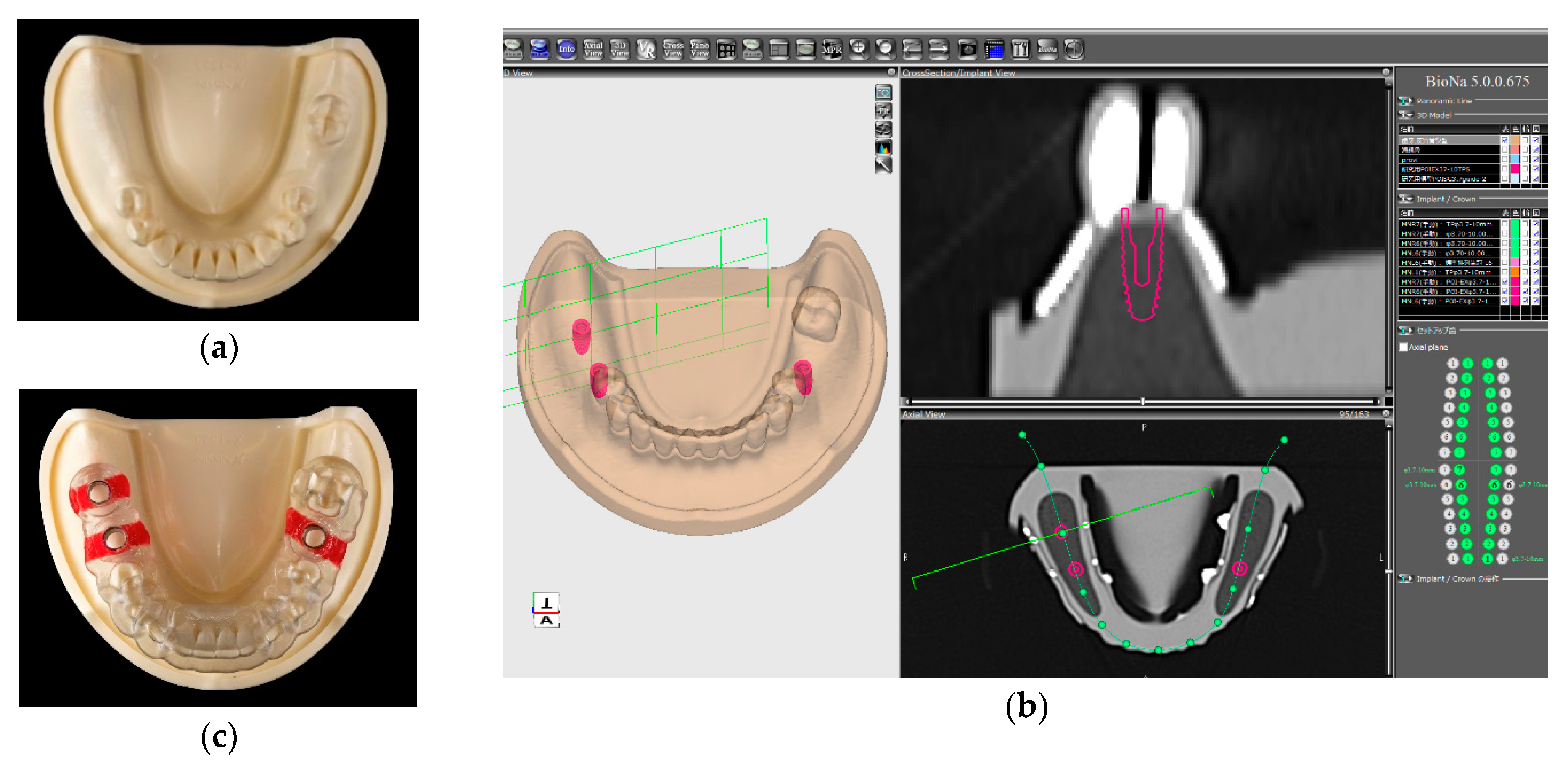
2.2. Implant Planning and Surgical Guide Fabrication
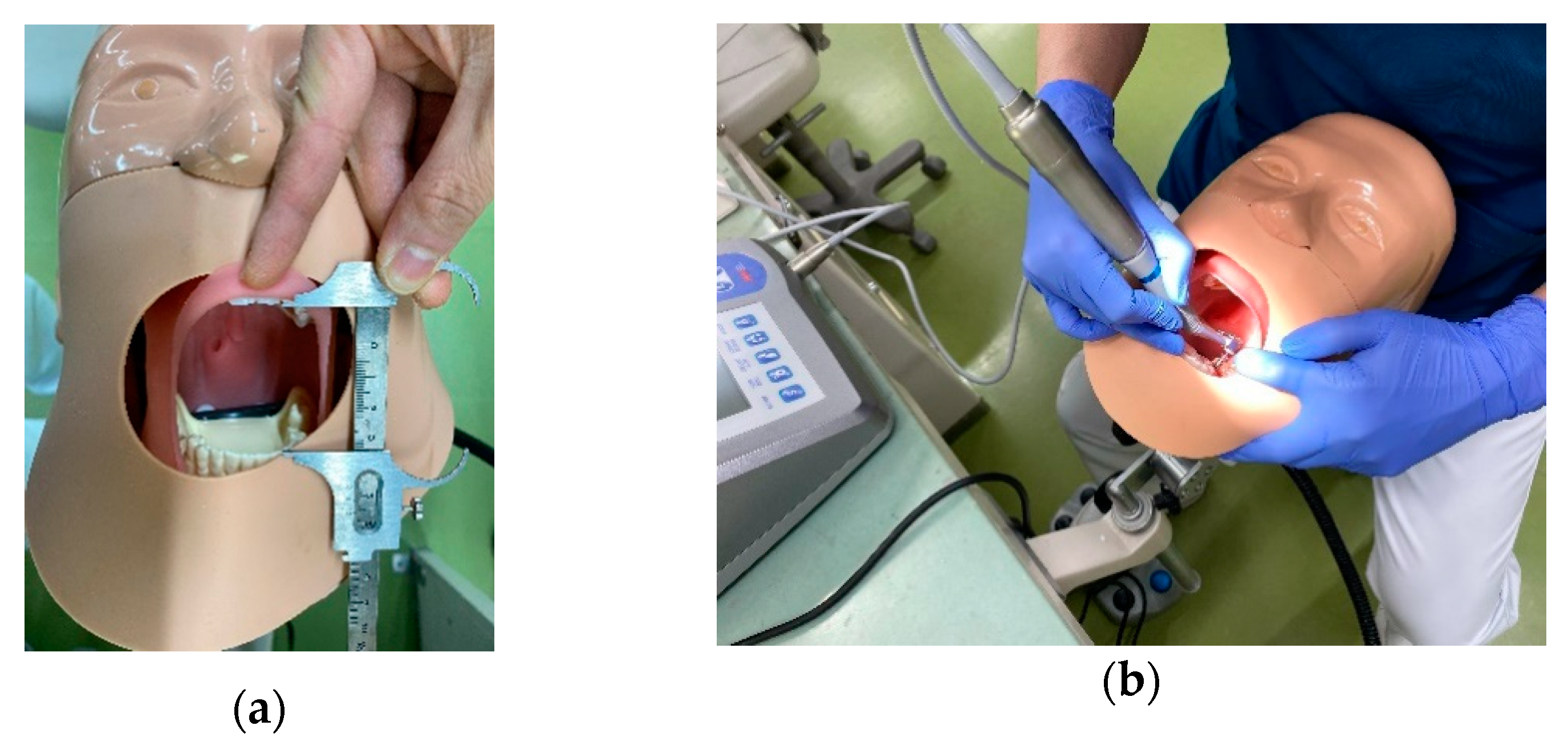
2.3. Simulation Implant Placement
2.4. Deviation Measurement
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Operator experience is not a critical factor for achieving accuracy of static guided implant surgery when using a tooth-supported surgical guide in a well-controlled environment. The SLA surgical guide aids inexperienced dentists in placing dental implants such that accuracy is comparable to that of experienced surgeons.
- Large positional or angular deviations of implant placement can occur, even with the aid of the SLA surgical guide and under well-controlled conditions. Care must be taken to avoid errors by appropriately executing the static guided implant surgery for both experienced and inexperienced operators.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Vercruyssen, M.; Laleman, I.; Jacobs, R.; Quirynen, M. Computer-supported implant planning and guided surgery: A narrative review. Clin. Oral Implants Res. 2015, 26 (Suppl. 11), 69–76. [Google Scholar] [CrossRef] [PubMed]
- Mediavilla Guzman, A.; Riad Deglow, E.; Zubizarreta-Macho, A.; Agustin-Panadero, R.; Hernandez Montero, S. Accuracy of computer-aided dynamic navigation compared to computer-aided static navigation for dental implant placement: An in vitro study. J. Clin. Med. 2019, 8, 2123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 25–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Haese, J.; Van De Velde, T.; Komiyama, A.; Hultin, M.; De Bruyn, H. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: A review of the literature. Clin. Implant Dent. Relat. Res. 2012, 14, 321–335. [Google Scholar] [CrossRef]
- Zhou, W.; Liu, Z.; Song, L.; Kuo, C.L.; Shafer, D.M. Clinical Factors Affecting the Accuracy of Guided Implant Surgery—A Systematic Review and Meta-analysis. J. Evid. Based Dent. Pract. 2018, 18, 28–40. [Google Scholar] [CrossRef]
- Raico Gallardo, Y.N.; da Silva-Olivio, I.R.T.; Mukai, E.; Morimoto, S.; Sesma, N.; Cordaro, L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: A systematic review and meta-analysis. Clin. Oral Implants Res. 2017, 28, 602–612. [Google Scholar] [CrossRef]
- Pozzi, A.; Polizzi, G.; Moy, P.K. Guided surgery with tooth-supported templates for single missing teeth: A critical review. Eur. J. Oral Implantol. 2016, 9 (Suppl. 1), S135–S153. [Google Scholar]
- Fernandez-Gil, A.; Gil, H.S.; Velasco, M.G.; Moreno Vazquez, J.C. An In Vitro Model to Evaluate the Accuracy of Guided Implant Placement Based on the Surgeon’s Experience. Int. J. Oral Maxillofac. Implants 2017, 32, 151–154. [Google Scholar] [CrossRef] [Green Version]
- Pyo, S.W.; Lim, Y.J.; Koo, K.T.; Lee, J. Methods Used to Assess the 3D Accuracy of Dental Implant Positions in Computer-Guided Implant Placement: A Review. J. Clin. Med. 2019, 8, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brandt, J.; Brenner, M.; Lauer, H.C.; Brandt, S. Accuracy of a Template-Guided Implant Surgery System with a CAD/CAM-Based Measurement Method: An In Vitro Study. Int. J. Oral Maxillofac. Implants 2018, 33, 328–334. [Google Scholar] [CrossRef] [Green Version]
- Stubinger, S.; Buitrago-Tellez, C.; Cantelmi, G. Deviations between placed and planned implant positions: An accuracy pilot study of skeletally supported stereolithographic surgical templates. Clin. Implant Dent. Relat. Res. 2014, 16, 540–551. [Google Scholar] [CrossRef]
- Vermeulen, J. The Accuracy of Implant Placement by Experienced Surgeons: Guided vs Freehand Approach in a Simulated Plastic Model. Int. J. Oral Maxillofac. Implants 2017, 32, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Van Assche, N.; Vercruyssen, M.; Coucke, W.; Teughels, W.; Jacobs, R.; Quirynen, M. Accuracy of computer-aided implant placement. Clin. Oral Implants Res. 2012, 23 (Suppl. 6), 112–123. [Google Scholar] [CrossRef] [PubMed]
- Vercruyssen, M.; Hultin, M.; Van Assche, N.; Svensson, K.; Naert, I.; Quirynen, M. Guided surgery: Accuracy and efficacy. Periodontology 2000 2014, 66, 228–246. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Ishikawa, M.; Maida, T.; Cheng, H.C.; Ou, K.L.; Nezu, T.; Endo, K. Stereolithographic surgical guide with a combination of tooth and bone support: Accuracy of guided implant surgery in distal extension situation. J. Clin. Med. 2020, 9, 709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, K.T.; Lin, C.C.; Hung, C.H. Maximum mouth opening of ethnic Chinese in Taiwan. J. Dent. Sci. 2009, 4, 40–44. [Google Scholar] [CrossRef] [Green Version]
- Cushen, S.E.; Turkyilmaz, I. Impact of operator experience on the accuracy of implant placement with stereolithographic surgical templates: An in vitro study. J. Prosthet. Dent. 2013, 109, 248–254. [Google Scholar] [CrossRef]
- Hinckfuss, S.; Conrad, H.J.; Lin, L.; Lunos, S.; Seong, W.J. Effect of surgical guide design and surgeon’s experience on the accuracy of implant placement. J. Oral Implantol. 2012, 38, 311–323. [Google Scholar] [CrossRef] [Green Version]
- Rungcharassaeng, K.; Caruso, J.M.; Kan, J.Y.; Schutyser, F.; Boumans, T. Accuracy of computer-guided surgery: A comparison of operator experience. J. Prosthet. Dent. 2015, 114, 407–413. [Google Scholar] [CrossRef] [Green Version]
- Park, S.J.; Leesungbok, R.; Cui, T.; Lee, S.W.; Ahn, S.J. Reliability of a CAD/CAM Surgical Guide for Implant Placement: An In Vitro Comparison of Surgeons’ Experience Levels and Implant Sites. Int. J. Prosthodont. 2017, 30, 367–369. [Google Scholar] [CrossRef] [Green Version]
- Van de Wiele, G.; Teughels, W.; Vercruyssen, M.; Coucke, W.; Temmerman, A.; Quirynen, M. The accuracy of guided surgery via mucosa-supported stereolithographic surgical templates in the hands of surgeons with little experience. Clin. Oral Implants Res. 2015, 26, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Bellardini, M. How much does experience in guided implant surgery play a role in accuracy? A randomized controlled pilot study. Int. J. Oral Maxillofac. Surg. 2017, 46, 922–930. [Google Scholar] [CrossRef]
- Al-Ekrish, A.A.; Ekram, M. A comparative study of the accuracy and reliability of multidetector computed tomography and cone beam computed tomography in the assessment of dental implant site dimensions. Dentomaxillofac. Radiol. 2011, 40, 67–75. [Google Scholar] [CrossRef]
- Marei, H.F.; Abdel-Hady, A.; Al-Khalifa, K.; Al-Mahalawy, H. Influence of surgeon experience on the accuracy of implant placement via a partially computer-guided surgical protocol. Int. J. Oral Maxillofac. Implants 2019, 34, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Bencharit, S.; Staffen, A.; Yeung, M.; Whitley, D., 3rd; Laskin, D.M.; Deeb, G.R. In Vivo Tooth-Supported Implant Surgical Guides Fabricated With Desktop Stereolithographic Printers: Fully Guided Surgery Is More Accurate Than Partially Guided Surgery. J. Oral Maxillofac. Surg. 2018, 76, 1431–1439. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.M.; Lee, H.E.; Lan, T.H. The influence of dental experience on a dental implant navigation system. BMC Oral Health 2019, 19, 222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Golob Deeb, J.; Bencharit, S.; Carrico, C.K.; Lukic, M.; Hawkins, D.; Rener-Sitar, K.; Deeb, G.R. Exploring training dental implant placement using computer-guided implant navigation system for predoctoral students: A pilot study. Eur. J. Dent. Educ. 2019, 23, 415–423. [Google Scholar] [CrossRef]
- Schneider, D.; Marquardt, P.; Zwahlen, M.; Jung, R.E. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin. Oral Implants Res. 2009, 20 (Suppl. 4), 73–86. [Google Scholar] [CrossRef] [Green Version]
- Pettersson, A.; Kero, T.; Soderberg, R.; Nasstrom, K. Accuracy of virtually planned and CAD/CAM-guided implant surgery on plastic models. J. Prosthet. Dent. 2014, 112, 1472–1478. [Google Scholar] [CrossRef]
- Testori, T.; Robiony, M.; Parenti, A.; Luongo, G.; Rosenfeld, A.L.; Ganz, S.D.; Mandelaris, G.A.; Del Fabbro, M. Evaluation of accuracy and precision of a new guided surgery system: A multicenter clinical study. Int. J. Periodontics Restor. Dent. 2014, 34 (Suppl. 3), s59–s69. [Google Scholar] [CrossRef] [Green Version]
- El Kholy, K.; Lazarin, R.; Janner, S.F.M.; Faerber, K.; Buser, R.; Buser, D. Influence of surgical guide support and implant site location on accuracy of static Computer-Assisted Implant Surgery. Clin. Oral Implants Res. 2019, 30, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Vasak, C.; Watzak, G.; Gahleitner, A.; Strbac, G.; Schemper, M.; Zechner, W. Computed tomography-based evaluation of template (NobelGuide)-guided implant positions: A prospective radiological study. Clin. Oral Implants Res. 2011, 22, 1157–1163. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Giansanti, M.; Di Mambro, A.; Calasso, S.; Barbato, E. Accuracy of two stereolithographic surgical templates: A retrospective study. Clin. Implant Dent. Relat. Res. 2013, 15, 448–459. [Google Scholar] [CrossRef] [PubMed]







| Operator Group | Dentist Number | Age | Gender | Years of Practicing | Specialty | |||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Fixed Pros. | OS/Perio. | Others | ||||
| Total | 30 | 42.8 ± 8.8 | 28 | 2 | 16.8 ± 9.3 | 10 | 8 | 12 |
| (Range) | (30–59) | (2–35) | ||||||
| Experienced | 15 | 45.5 ± 9.4 | 15 | - | 20.1 ± 10.3 | 7 | 5 | 3 |
| (Range) | (32–59) | (2–35) | ||||||
| Inexperienced | 15 | 40.1 ± 7.5 | 13 | 2 | 13.4 ± 7.1 | 3 | 3 | 9 |
| (Range) | (30–54) | (5–30) | ||||||
| p Value | 0.1231 | 0.4828 | 0.0774 | 0.0781 | ||||
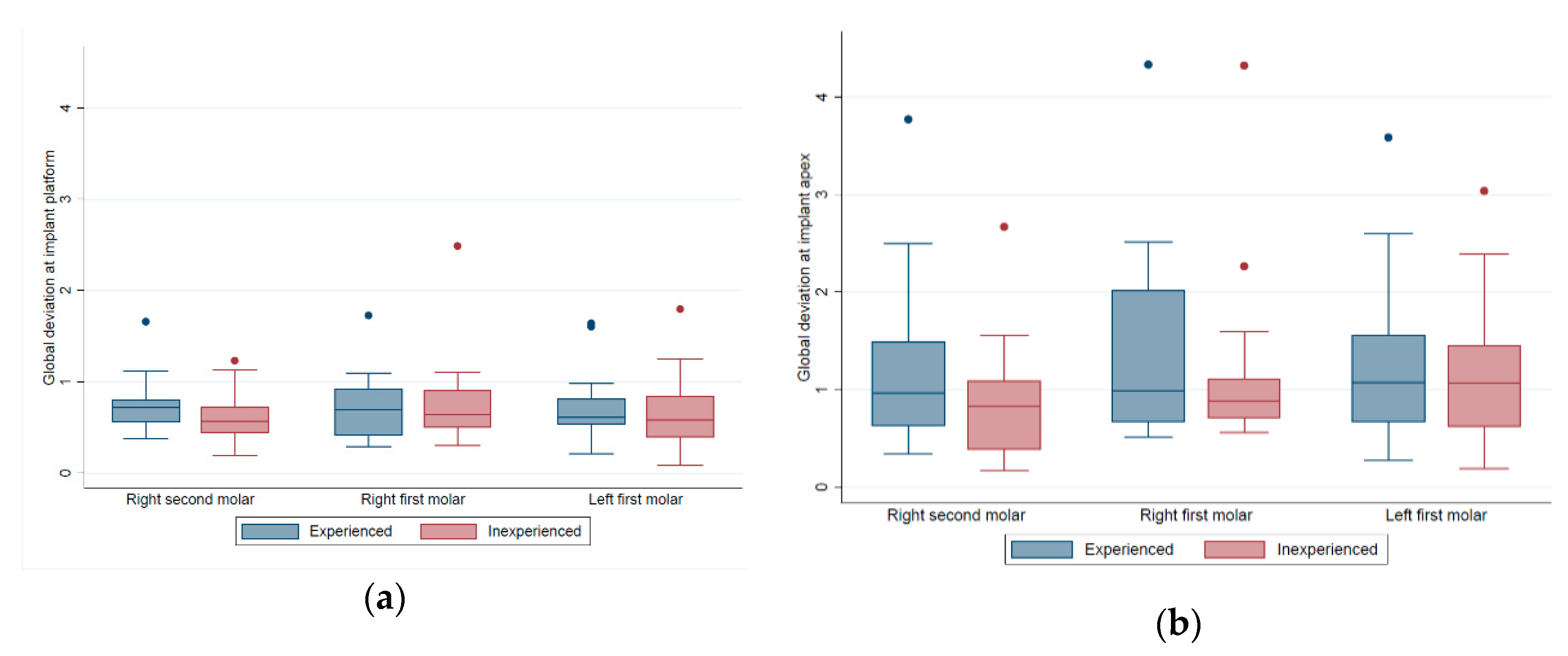
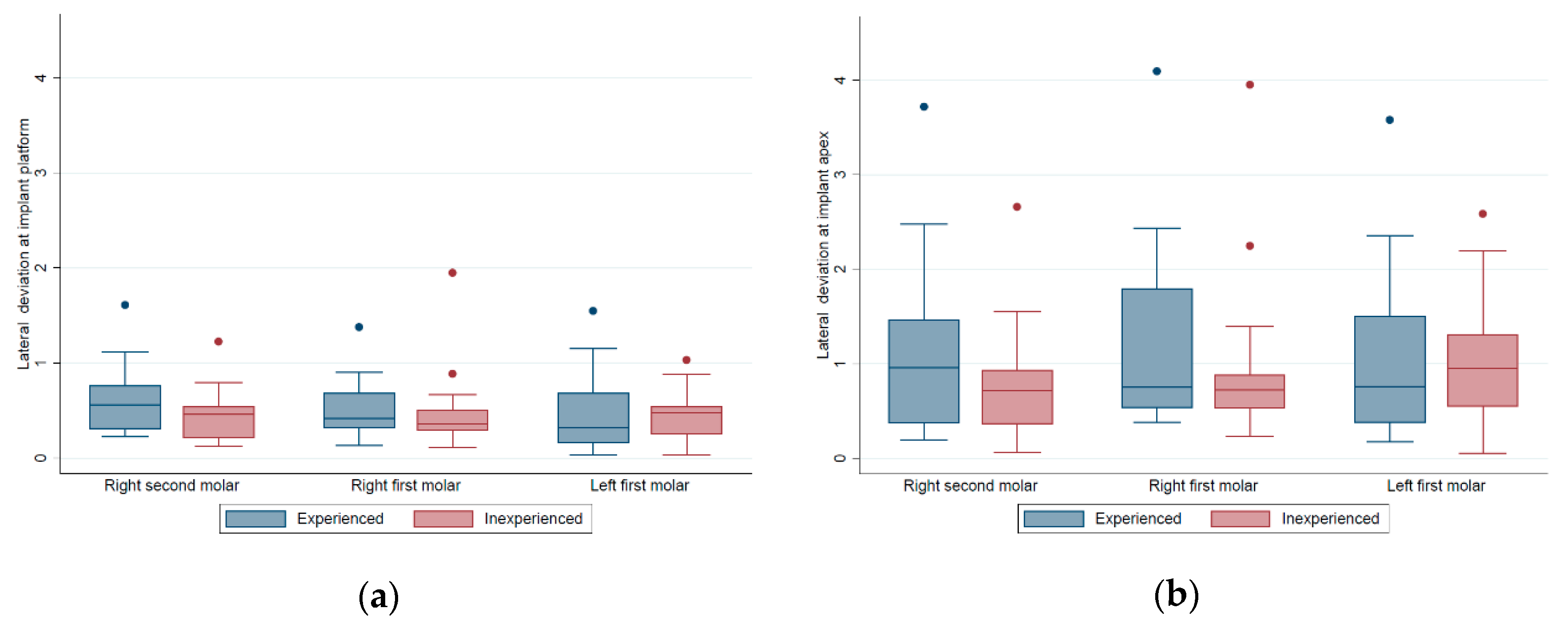
| Operator Experience Group | Implant Number | Implant Platform | Implant Apex | Depth Deviation (mm) | Angular Deviation (Degree) | ||
|---|---|---|---|---|---|---|---|
| Global (mm) | Lateral (mm) | Global (mm) | Lateral (mm) | ||||
| Total | 90 | 0.71 ± 0.39 | 0.50 ± 0.36 | 1.20 ± 0.87 | 1.06 ± 0.87 | 0.41 ± 0.33 | 3.44 ± 3.00 |
| (range) | (0.08–2.49) | (0.03–1.95) | (0.17–4.33) | (0.05–4.09) | (0.01–1.55) | (0.13–15.75) | |
| Experienced | 45 | 0.74 ± 0.36 | 0.54 ± 0.37 | 1.30 ± 0.93 | 1.17 ± 0.96 | 0.40 ± 0.29 | 3.86 ± 3.43 |
| (range) | (0.21–1.73) | (0.03–1.61) | (0.28–4.33) | (0.18–4.09) | (0.01–1.17) | (0.86–15.75) | |
| Inexperienced | 45 | 0.68 ± 0.42 | 0.47 ± 0.34 | 1.09 ± 0.79 | 0.94 ± 0.77 | 0.42 ± 0.37 | 3.02 ± 2.47 |
| (range) | (0.08–2.49) | (0.03–1.95) | (0.17–4.32) | (0.05–3.95) | (0.07–1.55) | (0.13–11.57) | |
| p Value a | 0.4824 | 0.3316 | 0.2520 | 0.2233 | 0.8014 | 0.1870 | |
| p Value b | 0.4808 | 0.3341 | 0.2547 | 0.2258 | 0.7977 | 0.1883 | |
| Operator Experience Group | Implant Number | Implant Platform | Implant Apex | Depth Deviation (mm) | Angular Deviation (Degree) | ||
|---|---|---|---|---|---|---|---|
| Global (mm) | Lateral (mm) | Global (mm) | Lateral (mm) | ||||
| Left first molar | |||||||
| Experienced | 15 | 0.74 ± 0.41 | 0.48 ± 0.42 | 1.24 ± 0.88 | 1.09 ± 0.93 | 0.49 ± 0.26 | 3.57 ± 2.97 |
| Inexperienced | 15 | 0.67 ± 0.43 | 0.44 ± 0.28 | 1.17 ± 0.77 | 1.02 ± 0.72 | 0.45 ± 0.39 | 3.41 ± 2.51 |
| p Value ‡ | 0.6662 | 0.7745 | 0.8063 | 0.8293 | 0.7622 | 0.8685 | |
| p Value ¶ | 0.5338 | 1.0000 | 0.8357 | 1.0000 | 0.3195 | 1.0000 | |
| Right first molar | |||||||
| Experienced | 15 | 0.72 ± 0.38 | 0.51 ± 0.33 | 1.39 ± 1.03 | 1.24 ± 1.03 | 0.43 ± 0.34 | 4.26 ± 4.06 |
| Inexperienced | 15 | 0.77 ± 0.53 | 0.51 ± 0.44 | 1.21 ± 0.96 | 1.01 ± 0.95 | 0.52 ± 0.39 | 2.97 ± 2.97 |
| p Value ‡ | 0.8010 | 0.9872 | 0.6170 | 0.5206 | 0.5366 | 0.3278 | |
| p Value ¶ | 0.9669 | 0.6482 | 0.6187 | 0.5614 | 0.6187 | 0.4553 | |
| Right second molar | |||||||
| Experienced | 15 | 0.75 ± 0.32 | 0.63 ± 0.37 | 1.28 ± 0.94 | 1.17 ± 0.99 | 0.29 ± 0.24 | 3.74 ± 3.38 |
| Inexperienced | 15 | 0.60 ± 0.29 | 0.45 ± 0.28 | 0.90 ± 0.63 | 0.80 ± 0.64 | 0.30 ± 0.29 | 2.69 ± 1.94 |
| p Value ‡ | 0.1833 | 0.1476 | 0.2121 | 0.2285 | 0.9549 | 0.3056 | |
| p Value ¶ | 0.1354 | 0.089 | 0.2455 | 0.2998 | 1.0000 | 0.6783 | |
| ANOVA p Value † | 0.8723 | 0.7509 | 0.7650 | 0.8044 | 0.2442 | 0.7685 | |
| Operator Variables | Implant Number | Implant Platform | Implant Apex | Depth Deviation (mm) | Angular Deviation (Degree) | ||
|---|---|---|---|---|---|---|---|
| Global (mm) | Lateral (mm) | Global (mm) | Lateral (mm) | ||||
| Total | 90 | 0.71 ± 0.39 | 0.50 ± 0.36 | 1.20 ± 0.87 | 1.06 ± 0.87 | 0.41 ± 0.33 | 3.44 ± 3.00 |
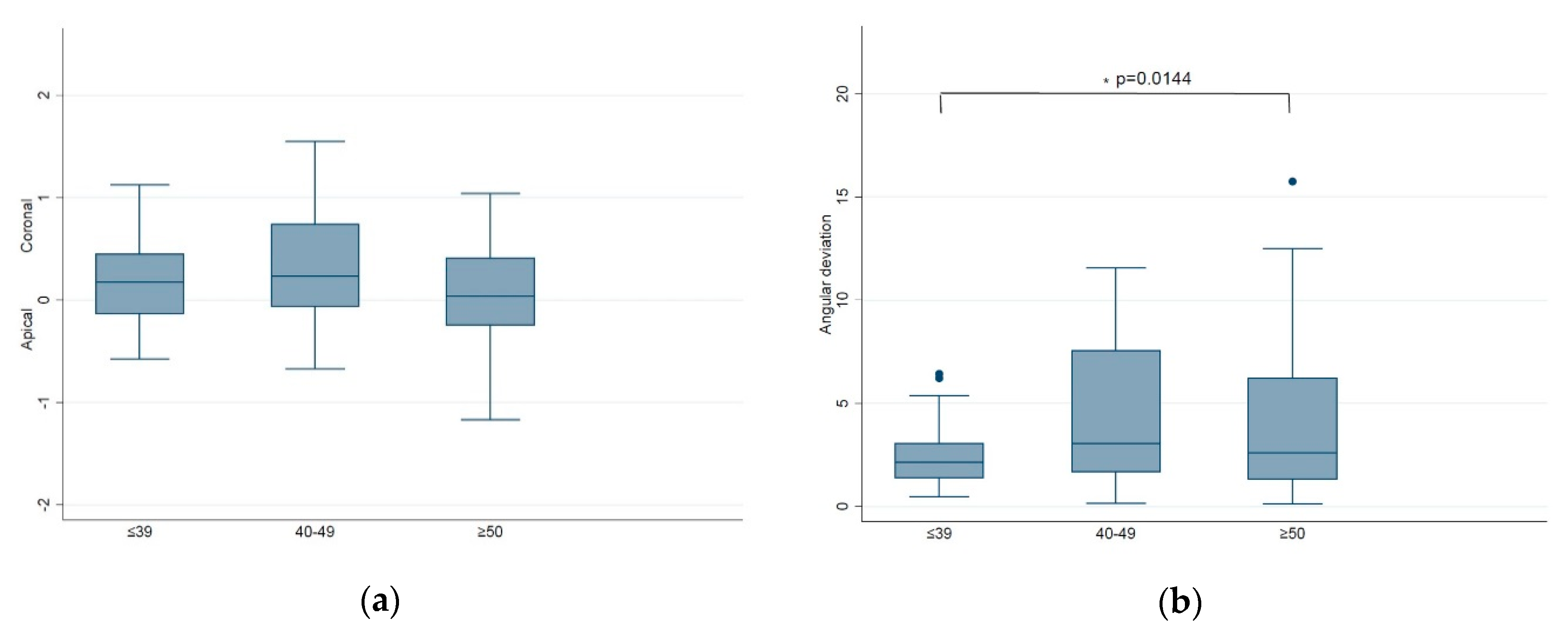
| Age | |||||||
| ≤39 | 39 | 0.57 ± 0.21 | 0.38 ± 0.17 | 0.87 ± 0.39 a | 0.74 ± 0.41 | 0.36 ± 0.25 | 2.40 ± 1.38 |
| 40–49 | 27 | 0.85 ± 0.47 | 0.60 ± 0.40 | 1.46 ± 0.94 b | 1.29 ± 0.92 | 0.50 ± 0.42 | 4.12 ± 3.12 |
| ≥50 | 24 | 0.77 ± 0.46 | 0.59 ± 0.46 | 1.43 ± 1.16 b | 1.30 ± 1.19 | 0.39 ± 0.32 | 4.36 ± 4.19 |
| p Value ‡ | 0.0111 | 0.0175 | 0.0068 * | 0.0101 | 0.2207 | 0.0144 | |
| Gender | |||||||
| Male | 84 | 0.72 ± 0.40 | 0.52 ± 0.36 | 1.22 ± 0.89 | 1.08 ± 0.90 | 0.41 ± 0.33 | 3.52 ± 3.09 |
| Female | 6 | 0.60 ± 0.29 | 0.30 ± 0.18 | 0.88 ± 0.28 | 0.67 ± 0.27 | 0.45 ± 0.37 | 2.38 ± 0.87 |
| p Value ¶ | 0.4716 | 0.091 | 0.452 | 0.3608 | 0.728 | 0.728 | |
| Years of practice | |||||||
| ≤10 | 33 | 0.74 ± 0.43 | 0.50 ± 0.35 | 1.17 ± 0.82 | 1.00 ± 0.80 | 0.47 ± 0.37 | 3.16 ± 2.55 |
| 11–20 | 24 | 0.58 ± 0.30 | 0.42 ± 0.26 | 0.99 ± 0.65 | 0.88 ± 0.66 | 0.33 ± 0.27 | 2.91 ± 2.39 |
| ≥21 | 33 | 0.77 ± 0.41 | 0.57 ± 0.41 | 1.37 ± 1.02 | 1.24 ± 1.05 | 0.41 ± 0.32 | 4.11 ± 3.71 |
| p Value ‡ | 0.1465 | 0.2939 | 0.2562 | 0.2828 | 0.2952 | 0.261 | |
| Specialty | |||||||
| Fixed Pros. | 30 | 0.64 ± 0.30 | 0.42 ± 0.31 | 1.05 ± 0.72 | 0.89 ± 0.77 | 0.41 ± 0.23 | 2.94 ± 2.66 |
| OS/Perio. | 24 | 0.68 ± 0.38 | 0.49 ± 0.37 | 1.19 ± 1.00 | 1.06 ± 1.01 | 0.36 ± 0.32 | 3.62 ± 3.63 |
| Others | 36 | 0.78 ± 0.46 | 0.58 ± 0.37 | 1.33 ± 0.88 | 1.19 ± 0.86 | 0.44 ± 0.40 | 3.74 ± 2.85 |
| p Value ‡ | 0.3278 | 0.2145 | 0.4219 | 0.377 | 0.6598 | 0.5291 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-C.; Ishikawa, M.; Huang, B.-H.; Huang, M.-S.; Cheng, H.-C.; Maida, T.; Nezu, T.; Endo, K. In Vitro Accuracy of Static Guided Implant Surgery Measured by Optical Scan: Examining the Impact of Operator Experience. Appl. Sci. 2020, 10, 2718. https://doi.org/10.3390/app10082718
Lin C-C, Ishikawa M, Huang B-H, Huang M-S, Cheng H-C, Maida T, Nezu T, Endo K. In Vitro Accuracy of Static Guided Implant Surgery Measured by Optical Scan: Examining the Impact of Operator Experience. Applied Sciences. 2020; 10(8):2718. https://doi.org/10.3390/app10082718
Chicago/Turabian StyleLin, Chia-Cheng, Masahiro Ishikawa, Bai-Hung Huang, Mao-Suan Huang, Hsin-Chung Cheng, Takeo Maida, Takashi Nezu, and Kazuhiko Endo. 2020. "In Vitro Accuracy of Static Guided Implant Surgery Measured by Optical Scan: Examining the Impact of Operator Experience" Applied Sciences 10, no. 8: 2718. https://doi.org/10.3390/app10082718
APA StyleLin, C.-C., Ishikawa, M., Huang, B.-H., Huang, M.-S., Cheng, H.-C., Maida, T., Nezu, T., & Endo, K. (2020). In Vitro Accuracy of Static Guided Implant Surgery Measured by Optical Scan: Examining the Impact of Operator Experience. Applied Sciences, 10(8), 2718. https://doi.org/10.3390/app10082718




