1. Introduction
Intraoperative patient management is a challenging undertaking. Among a multitude of laboratory tests and technologies available to monitor patients during surgery, clear selection criteria for one or another monitoring technique is necessary.
The human brain is one of the most metabolically active organs consuming in average 20% of all the body oxygen [
1]. The dangers of prolonged brain hypoxia, also intraoperatively, are already well documented in numerous studies. A large randomized study including 265 patients undergoing coronary artery bypass surgery showed significant correlation between prolonged intraoperative hypoxia and early cognitive decline and prolonged hospital stay [
2]. Intraoperative cerebral desaturation has been proven to predict postoperative cognitive dysfunction and other postoperative complications also in patients undergoing non-cardiac surgery like thoracic, major orthopedic and major abdominal surgery [
3].
Still, brain remains one of the least monitored organ during anesthesia and surgery, as the majority of available methods are invasive, like, jugular venous oximetry, requiring cannulation of the jugular bulbus, brain tissue oxygen monitoring using the Clark electrode in the brain parenchyma or cerebral microdialysis [
4]. Near infrared spectroscopy (NIRS) has been increasingly implemented in clinical practice. NIRS devices are non-invasive, easy to use and monitor cerebral oxygen saturation (rScO
2) continuously.
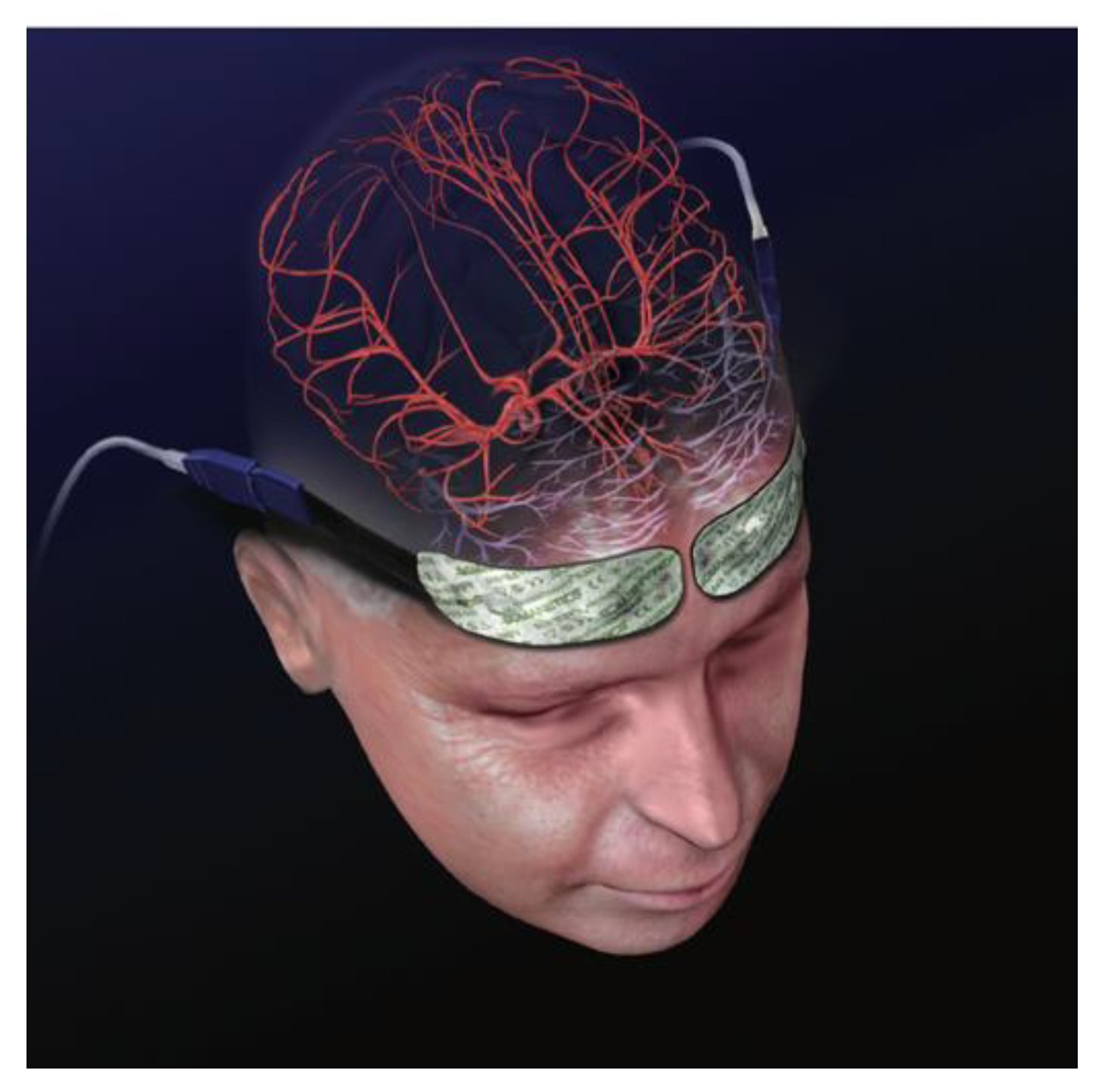
A NIRS device cerebral oximeter consists of a monitor and two adhesive sensors, which are attached to the patients’ forehead: one above the left and one above the right cerebral hemisphere overlying the frontal lobe (
Figure 1). In each sensor there is an incorporated light diode-emitting near infrared light and two light detectors proximal and distal collecting the scattered light returning to the surface, permitting to separate data of shallow and deep optical signals [
5] (
Figure 2).
Near infrared light, used in the cerebral oximetry, is at wave length 730 and 810 nm, which is capable of penetrating the skull [
6]. In the brain tissue, light is either absorbed by hemoglobin (Hb) molecules or scattered back to the brain surface depending on the degree of oxygenation [
5].
Cerebral oxygenation values are calculated using the Beer Lambert law. Beer’s law claims that the light intensity decreases as the concentration of the substance the light passes through increases [
5]. Lambert’s law incorporates that the intensity of the light decreases as the distance, which the light is traveling, increases [
5]. Based on both laws, oxygen can be measured by how much of the emitted light the substance absorbs and by the amount of light, which is travelling through it. Light absorption will be proportional to the oxygenation status of the tissue [
5,
7]. Values, at which cerebral oxygen saturation is considered to be normal, differ amongst studies published. Normal baseline cerebral oximetry values range between 60% and 80% [
5]. Abnormal rScO
2 values are defined as rScO
2 drop from ones’ individual baseline values for 20% or an absolute drop under a rScO
2 of 50% [
7], marking those as a trigger values for an intervention [
6] (
Figure 3).
The NIRS interventional protocol is used to guide patient management in order to mitigate cerebral desaturation and avoid hypoxic brain injury. The most commonly applied protocol has been published by Deschamps and colleagues [
8]. The protocol includes steps that should be considered when cerebral desaturation occurs. The protocol also proposes a plan of actions.
Interventions aimed at preserving normal cerebral oxygenation within baseline values, can help to avoid postoperative cognitive disturbances, reduce the days spent in the intensive care unit [
9] and avoid complications, like, kidney failure or wound infections [
3].
Monitoring of rScO
2 using NIRS devices, cerebral oximeters, have been widely used during cardiac surgery, especially during cardiac bypass operations, as cardiac surgery patients often suffer from perioperative neurological complications [
5]. Numerous studies regarding NIRS in cardiac surgery show positive correlation between intraoperative cerebral desaturation and postoperative cognitive disturbances, stroke, prolonged hospital stay [
6].
Lately, monitoring of cerebral oxygen saturation has gained increasing popularity also in non- cardiac surgeries. During thoracic surgery—thoracotomy or thoracoscopy where at least one measurement lower than 80% from baseline value has been reported [
3]. During shoulder surgery in the beach chair position, where cerebral desaturation episodes can be 1 minute up to 1 hour long [
3]. In gynecological procedures, where the Trendelenburg position is used, as well as urological operations with hemodilution [
3]. Furthermore, vascular surgery, carotid endarterectomy, where rScO
2 decreases during clamping of internal carotid artery or with the blood loss during abdominal aortic aneurysm repair [
3].
There is a very limited amount of studies available regarding rScO
2 intraoperative monitoring during spinal operations, although special attention should be paid due to prone position and possible blood loss. Prone position during spinal surgery might be associated with several physiological challenges, which influences cerebral blood flow and oxygen supply creating conditions for cerebral desaturation. Increased abdominal pressure due to various etiologies might decrease vena cava inferior transvascular pressure and reduce venous return to the heart. Moreover, increased external pressure on the chest, resulting from prone positioning, also reduces cardiac index, in addition to increasing the peak airway pressure, thereby decreasing lung compliance causing a further decrease in cardiac output [
10].
The aim of study was to evaluate the usefulness of monitoring intraoperative cerebral oxygenation during spinal surgery in order to discover cerebral desaturation.
2. Materials and Methods
Patients scheduled for spinal surgery were recruited to a prospective study including patients over 18 years of age scheduled for elective spinal surgery. Exclusion criteria were patients undergoing urgent spinal surgery, patients with a history of cerebral disease, like previous stroke, cerebral hematoma or transient ischemic stroke.
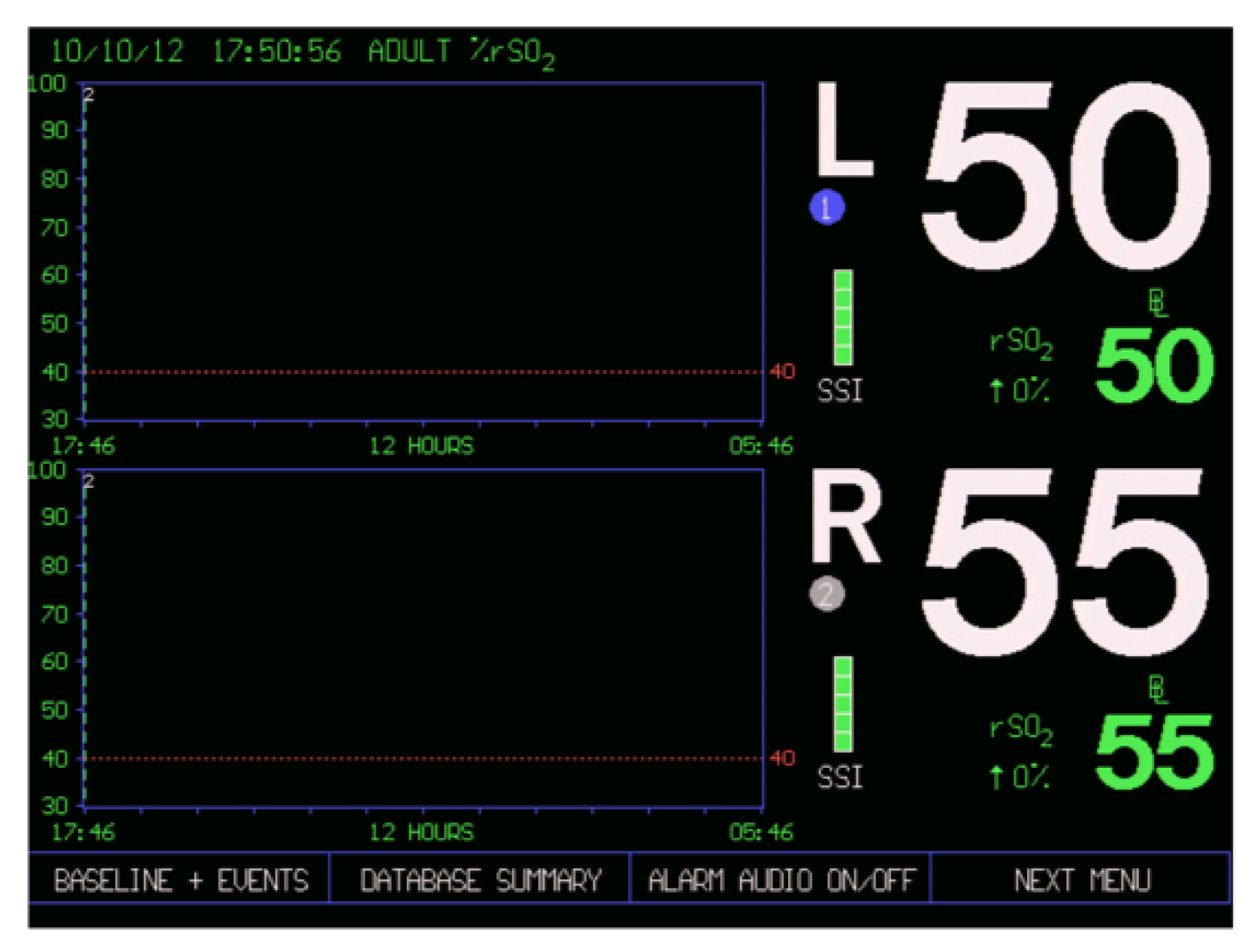
In our study INVOS (in vivo optical spectroscopy) 4100 (Covidien, Minneapolis, USA) two channel cerebral oximeter was used. In the operating room two INVOS sensors were attached to the patients’ forehead, one above the left (L) and one above the right (R) eyebrow, before induction of anesthesia, while breathing room air. Individual baseline values were obtained. Meanwhile other presurgical measures were assessed, such as percutaneous oxygen saturation (SpO2) and mean arterial pressure (MAP) by measuring non-invasive blood pressure. Anesthesia was induced using fentanyl 0.1–0.2 mg and propofol 1–2 mg/kg. Tracheal intubation was facilitated with cisatracurium 0.2 mg/kg. Anesthesia was maintained with continuous infusion of fentanyl 0.03–0.06 μg/kg/min, cisatracurium 0.06–0.1 mg/kg/h and sevoflurane at MAC 0.6–0.8. Mechanical lung ventilation was set to 8 mL/kg and fraction of inspired oxygen (FiO2) to 0.4. Ventilation was set to keep end-tidal carbon dioxide (EtCO2) in the range of 35–45 mmHg and SpO2 96–100%.
During the surgery, SpO
2, MAP, EtCO
2 and rScO
2 were documented in the study protocol every 5 min. If the rScO
2 values dropped more than 20% from the patients’ individual baseline value, or if there was an absolute drop of rScO
2 to below 50%, near infrared spectroscopy based interventional protocol was activated to restore rScO
2 values above the threshold. In the current study, we followed the NIRS protocol proposed by Deschamps et al. [
8]. As the protocol was developed for cardiac surgery patients, we adjusted it to spinal surgery patients. Firstly, the head position is verified, in order to exclude head flexion, extension or rotations to the left or right side. Secondly, MAP is raised by injecting boluses of ephedrine. Thirdly, systemic oxygen saturation is tested and arterial blood oxygen partial pressure (PaO
2) is measured, and if low, FiO
2 is raised above 0.4. Fourthly, if EtCO
2 or PaCO
2 are low, hyperventilation is corrected. Fifthly, hemoglobin concentration is assessed and red blood cell transfusion is considered. Sixthly, the cardiac function is optimized by using vasopressor infusion. Seventhly, causes of excessive cerebral O
2 consumption, such as convulsions and hyperthermia, are evaluated and treated [
8].
In the study protocol, we also noted patients’ demographic data (age and sex), comorbidities, daily medication, the type of spinal surgery, preoperative hemoglobin and hematocrit levels, intraoperative blood loss and duration of operation.
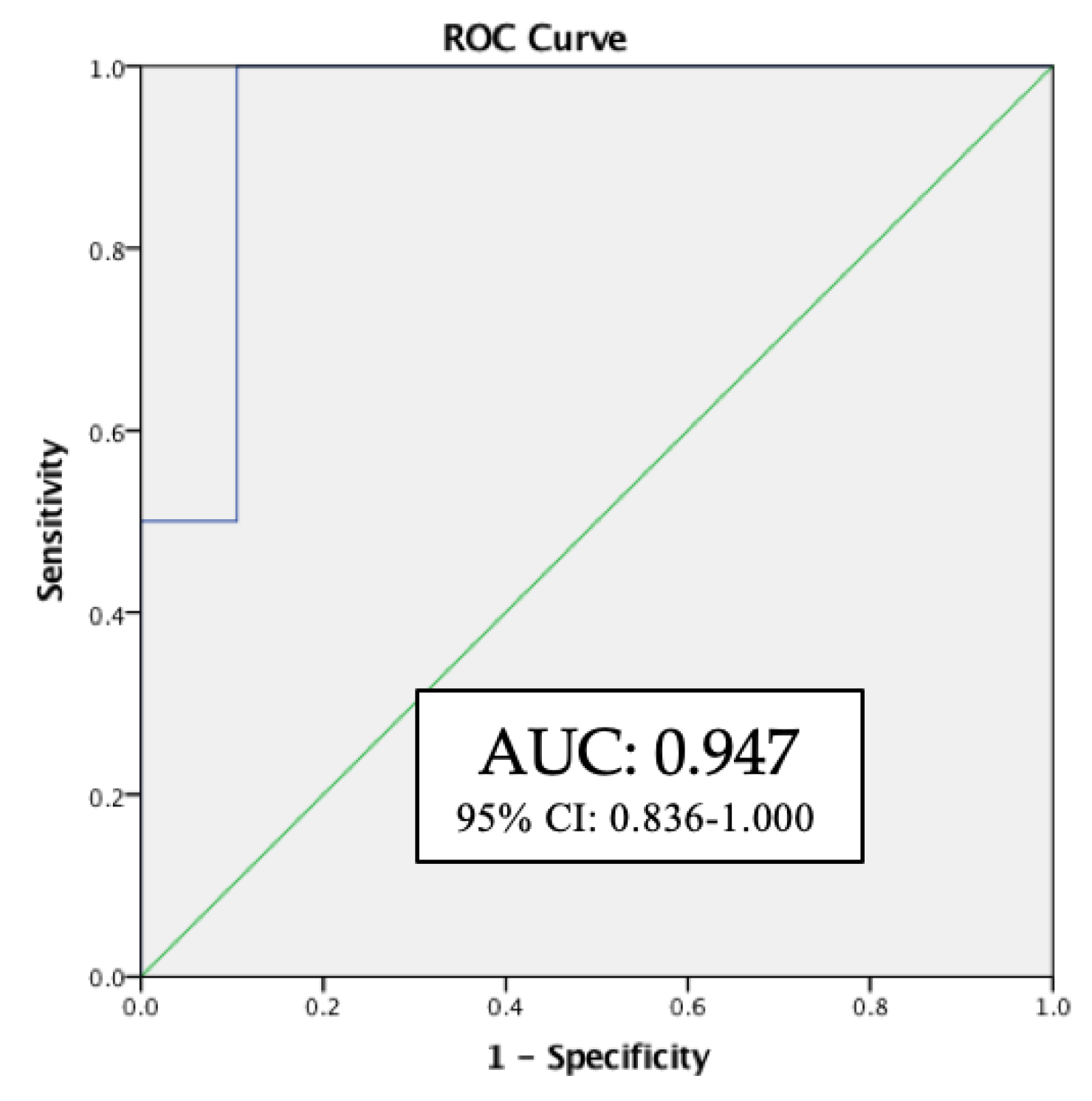
Statistical analysis was performed using SPSS V.23. Values were presented as mean ± standard deviation (SD). Statistical significance was assumed if p < 0.05. The receiver operating characteristic (ROC) curves, their respective 95% confidence intervals, and significance were compared between patients to identify predicting factors for intraoperative cerebral desaturation.
Study protocol and informed consent form was approved by the Medical Research Ethics Committee of Riga Stradins University (Approval No. 85/29.12.2016).
3. Results
In total, 44 patients scheduled for spinal surgery were included. Demographic characteristics and preoperative laboratory findings, duration of operation, intraoperative blood loss, intraoperative MAP, SpO
2 and EtCO
2 are shown in
Table 1. We determined rScO
2 at the following time points: (1) preoperative baseline; (2) after induction of anesthesia; (3) during prone position and (4) at the end of the surgery in supine position, as shown in
Table 2.
In 3 out of 44 patients, we observed intraoperative cerebral desaturation. In two patients rScO2 decreased under 20% from individual baseline. One patient was 57 years old undergoing microdiscectomy, the other one was 24 years old undergoing transpedicular fixation due to trauma. In one patient, 54 years old undergoing extirpation of spinal meningioma, rScO2 decreased to below 50%. In all 3 patients the NIRS interventional protocol was initiated. The first step, the verification of correct head position resulted in no changes in rScO2 in two of the patients while rScO2 increased above the threshold value in one patient. In the remaining two patients, MAP was raised using Ephedrin boluses (5-20 mg) and rScO2 raised above threshold and no further interventions were necessary.
Comparing to other spinal surgery patients who experienced only mild cerebral oxygenation fluctuations intraoperatively, which did not reach desaturation threshold, the patients with desaturation episodes had significantly longer operation medium time—114 ± 35 min in patients without cerebral desaturation compared to medium 200 ± 98 min in patients with intraoperative cerebral desaturation (p = 0.01). Pearson’s correlation showed a trend towards a negative correlation between rScO2 and duration of operation, although not statistically significant (r = −0.9, p = 0.2).
Receiver operating characteristic (ROC) curve analysis showed blood loss to be a strong predictor of possible cerebral desaturation (AUC: 0.947, 95% CI: 0.836–1.000,
p = 0.04;
Figure 4).
4. Discussion
In the present study, NIRS was used for monitoring patients undergoing spinal surgery in the prone position. Three out of 44 (6%) patients showed intraoperative cerebral desaturation, indicating that rScO2 monitoring might not be useful in all spinal surgery patients and careful patient selection could be necessary. On the other hand, no correlation between cerebral oxygen saturation and other intraoperatively monitored parameters, like, MAP, SpO2 and EtCO2 were seen. Therefore, without rScO2 monitoring, cerebral desaturation episodes would have remained unnoticed.
In patients experiencing intraoperative cerebral desaturation, longer operation time (not statistically significant) and greater blood loss (statistically significant) were recognized as possible predictors of cerebral oxygen desaturation during spinal surgery. Vertzakis et al. [
11] showed that NIRS might be a valuable tool for guiding the decision regarding the necessity of blood transfusion during cardiac surgery. In his study significantly fewer patients monitored with INVOS received blood transfusion and significantly fewer red blood cell units were transfused in comparison with the control group with no NIRS monitoring [
11].
The patients who experienced intraoperative cerebral desaturation episodes were 24, 54 and 57 years of age. Only one patient had comorbidities. That was adiposities and arterial hypertension, which was treated with one antihypertensive medicine. Therefore, it is not possible to assess whether one or another comorbidity is related to intraoperative cerebral oxygen desaturation. Nevertheless, our study demonstrates that also young people without any known comorbidities can be at risk for cerebral desaturation.
Regarding NIRS interventional protocol, in one patient rScO
2 values raised above the threshold after verifying correct head position. The importance of correct head position during prone position also has been emphasized by Andersen et al., where they strongly recommend a neutral head position, as head rotation, flexion or extension can significantly alter cerebral oxygenation [
12].
The limitation of our study is the lack of analysis of the postoperative period as one or another monitoring device implementation in clinical practice should also improve postoperative period or organ-related outcome [
13]. The majority of studies show clear benefit of rScO
2 intraoperative monitoring. Thus, less renal and respiratory failures and a shorter length of stays in intensive care units have been recognized in patients in whom NIRS guided interventions were used during surgery [
14]. A lower probability of death and major organ dysfunction also have been reported [
15,
16]. A number of studies have been performed focusing on cerebral oxygen saturation intraoperative monitoring and postoperative cognitive outcome as postoperative cognitive decline or dysfunction (POCD) impair patient postoperative recovery and can lead to long-term consequences [
17]. A randomized study has shown that patients suffering from intraoperative cerebral desaturation also have an increased risk of POCD [
2]. What is more important, lower incidence of cognitive deficiencies in patients monitored with NIRS was reported in a study that included spinal surgery patients [
18].
Every monitoring device, that can be used intraoperatively, should work in favor of additional patient safety. NIRS devices can help physicians to guide making decisions during the surgery. However, NIRS is believed to be best used as a trend monitor, without following strict thresholds [
19]. It seems to be better for recognizing patients at risk than guiding interventions [
20].