New Technologies in Orthodontics: A Digital Workflow to Enhance Treatment Plan and Photobiomodulation to Expedite Clinical Outcomes
Abstract
1. Introduction
2. Materials and Methods
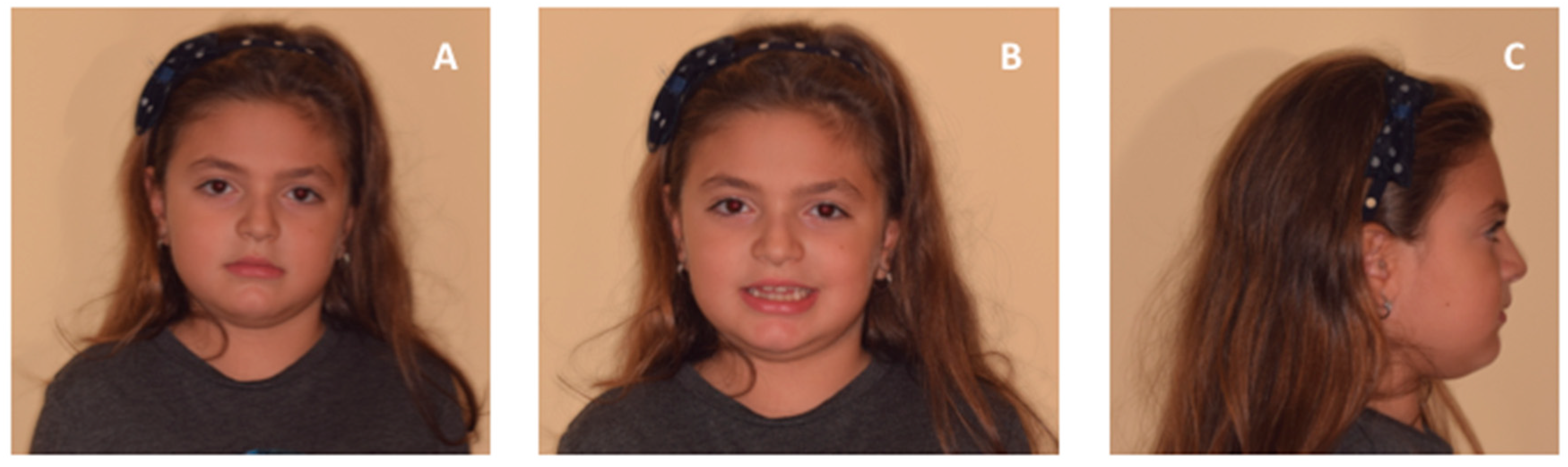
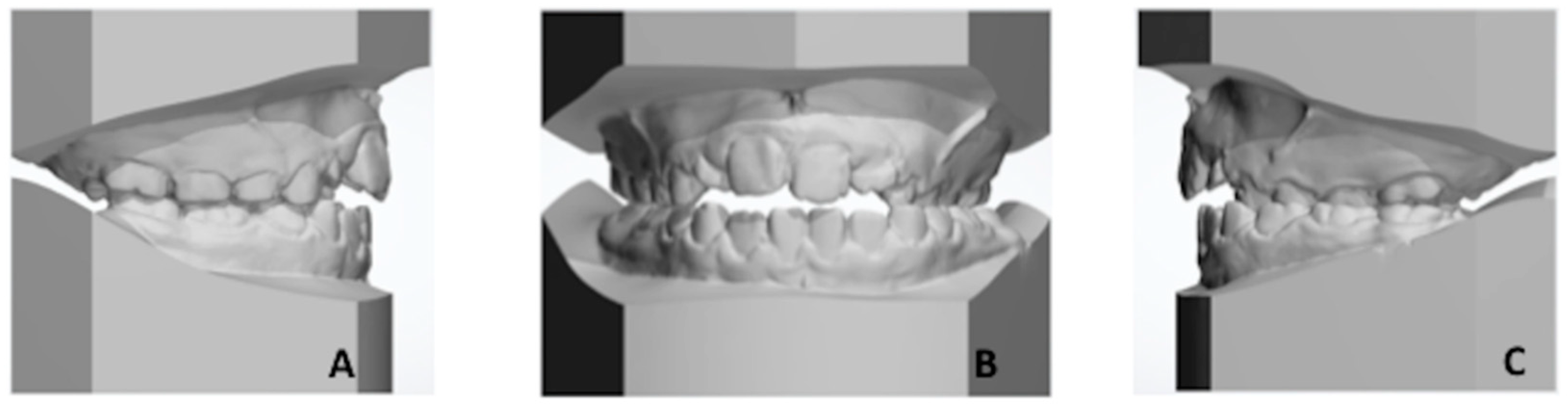
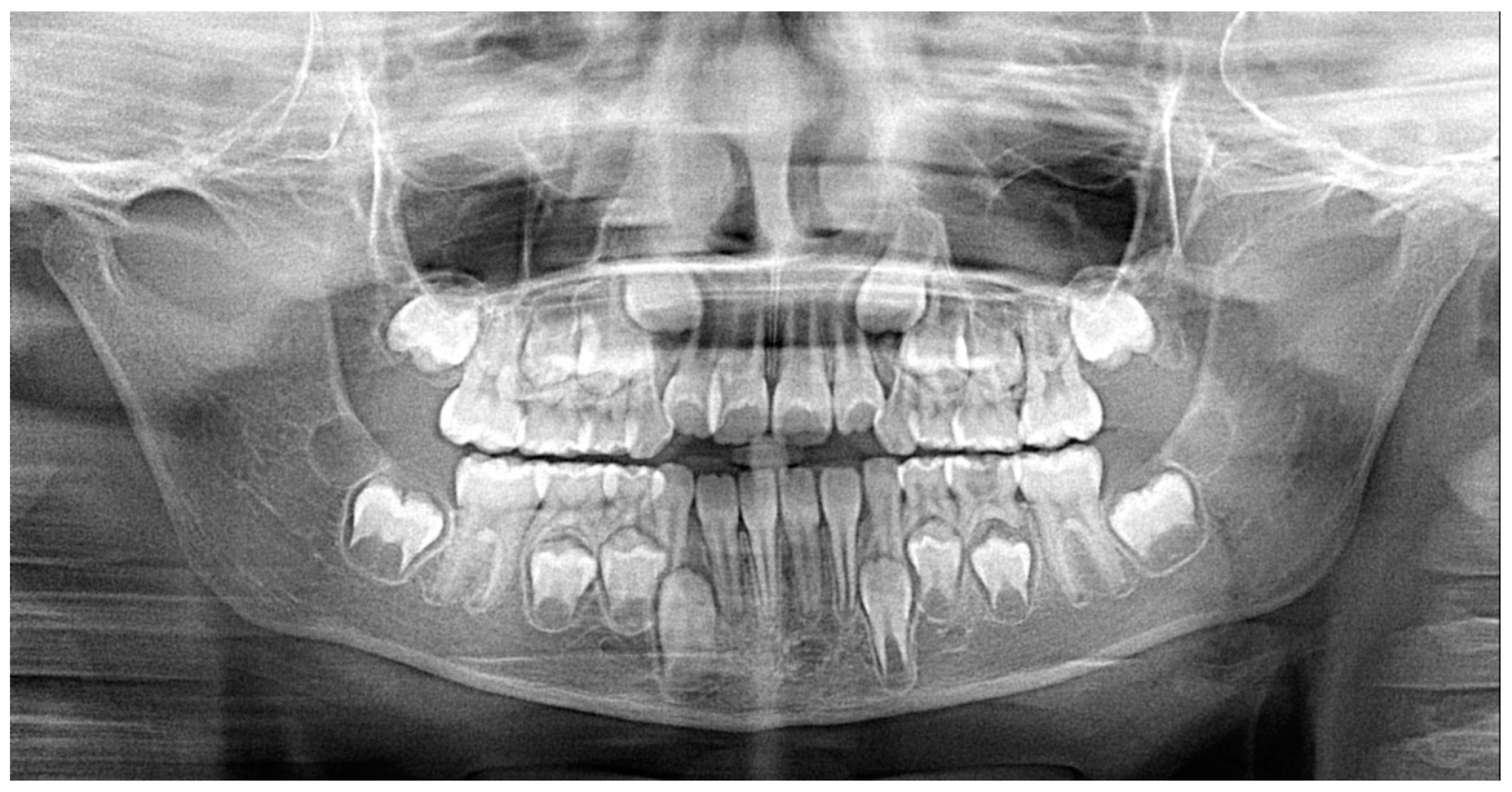
2.1. Patient’s Clinical Characteristics
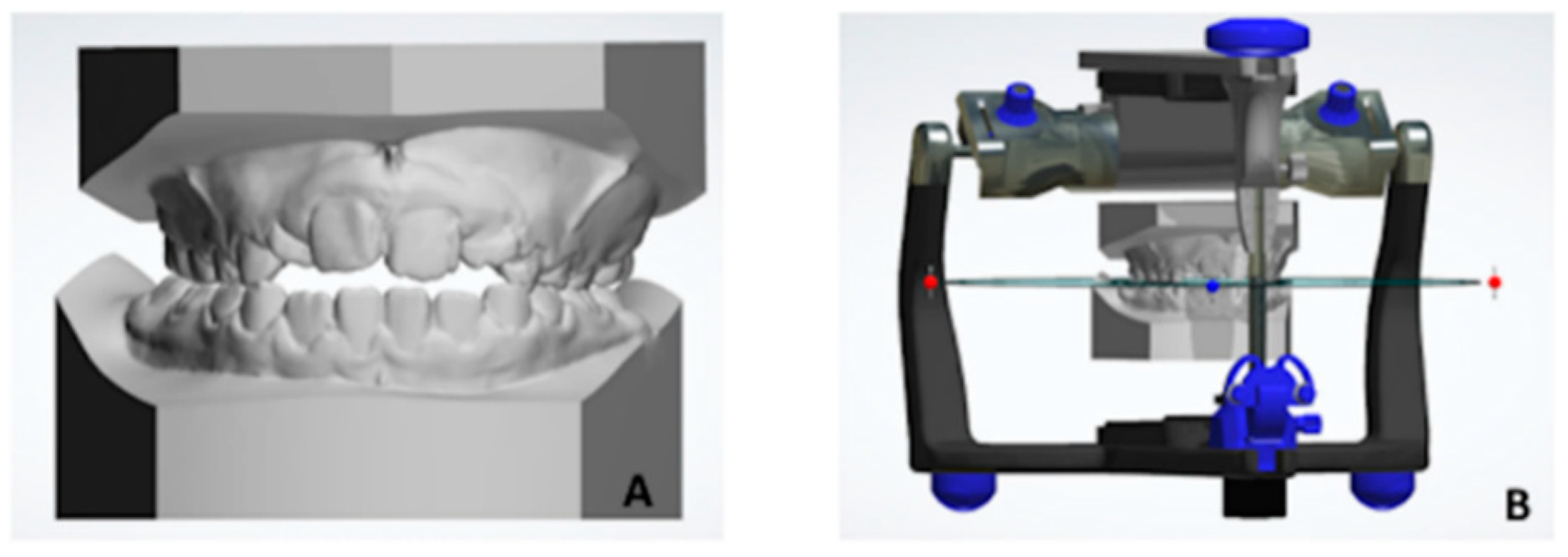
2.2. Creation of 3D Virtual Model of Both Maxillary and Mandibular Arches
2.3. Digitial Workflow for Anatomical Morphological Evaluation of Maxilla
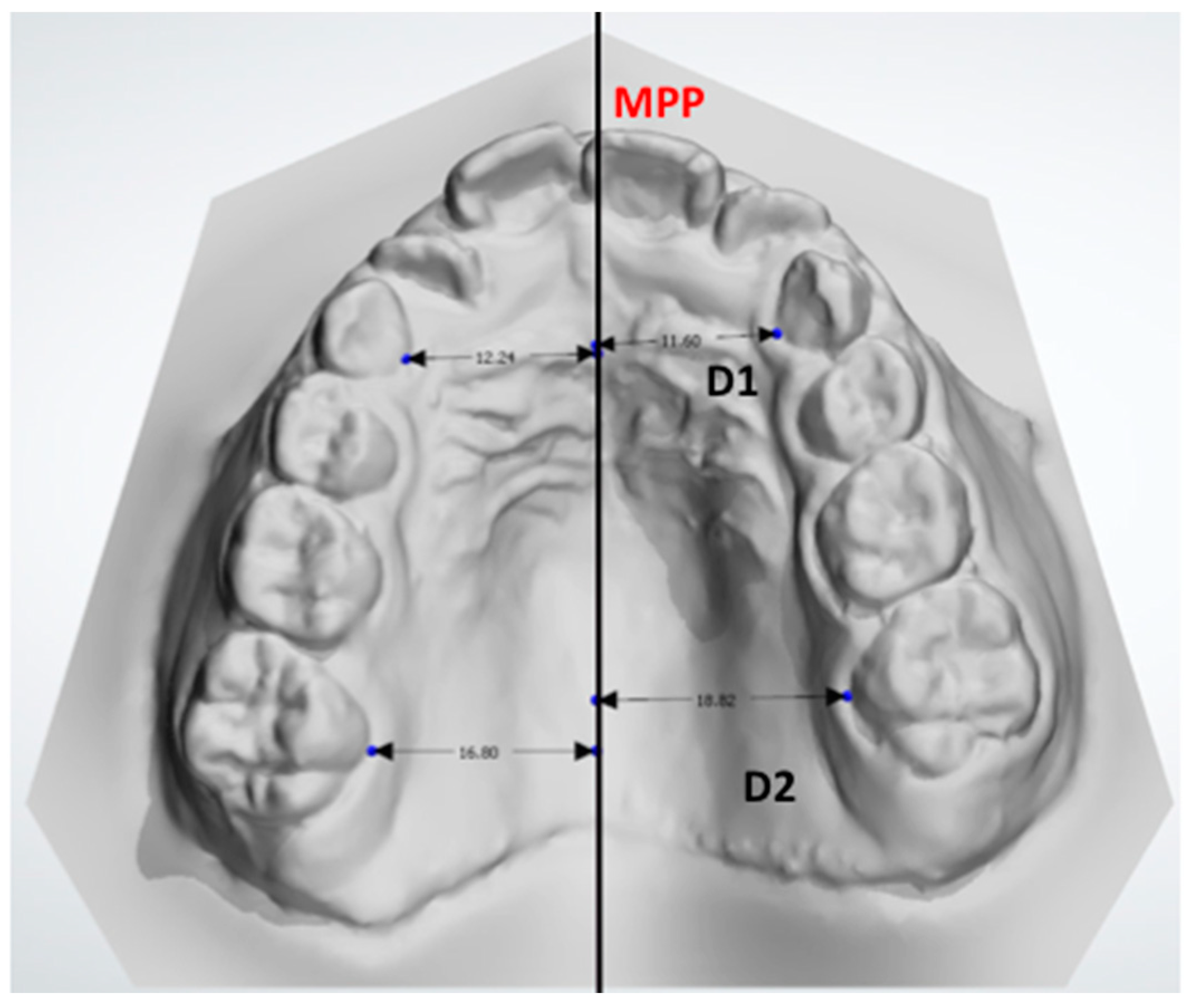
- D1: the distance between the midpoint at the dento-gingival junction of the primary canine from the crossbite and noncrossbite sides compared with the MPP.
- D2: the distance between the midpoint of the dento-gingival junction of the first molar from the crossbite and noncrossbite sides compared with the MPP.
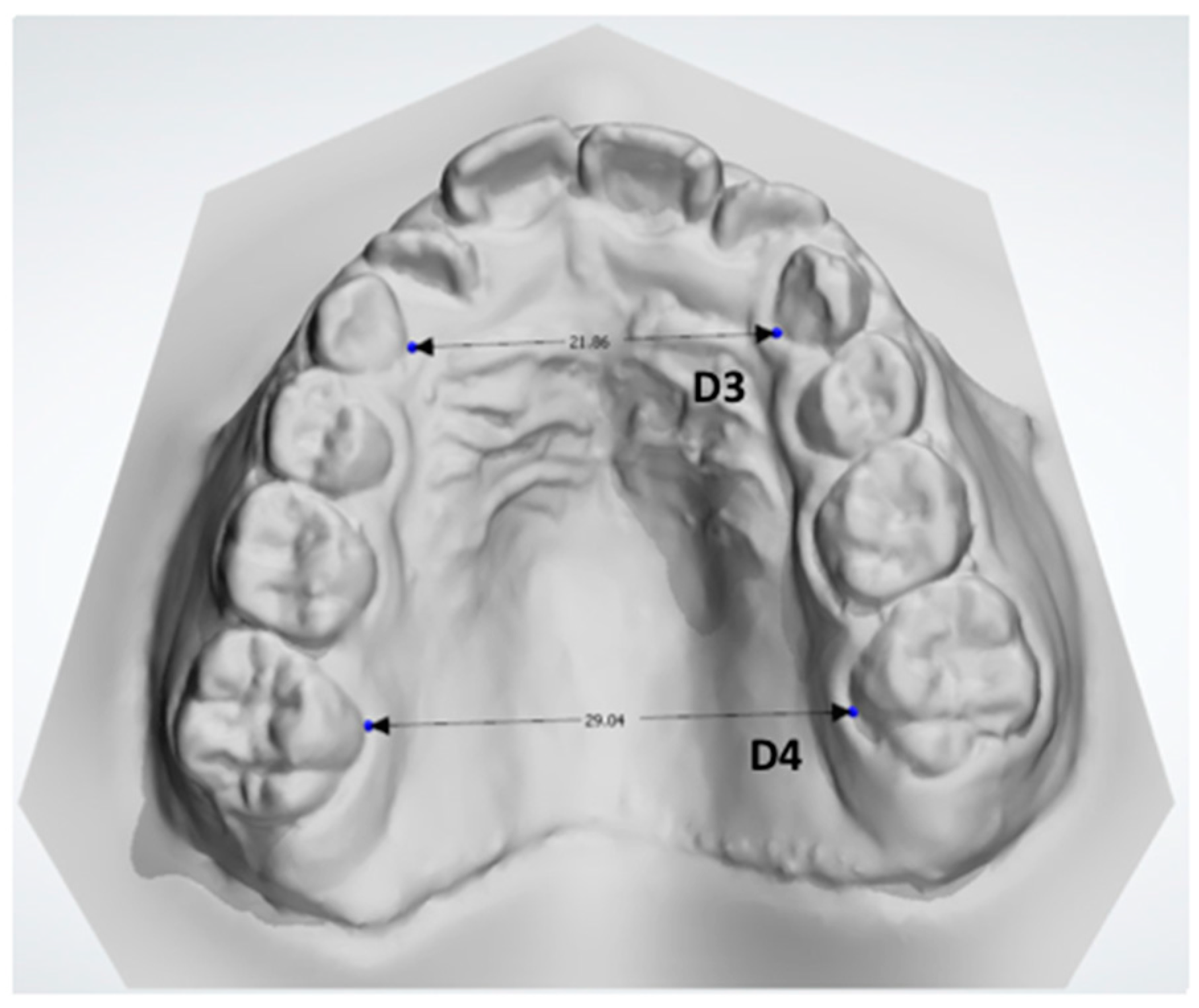
- D3: the distance between the midpoint at the dento-gingival junction of the two primary canines (Figure 7).
- D4: the distance between the midpoint at the dento-gingival junction of the two first molars (Figure 7).
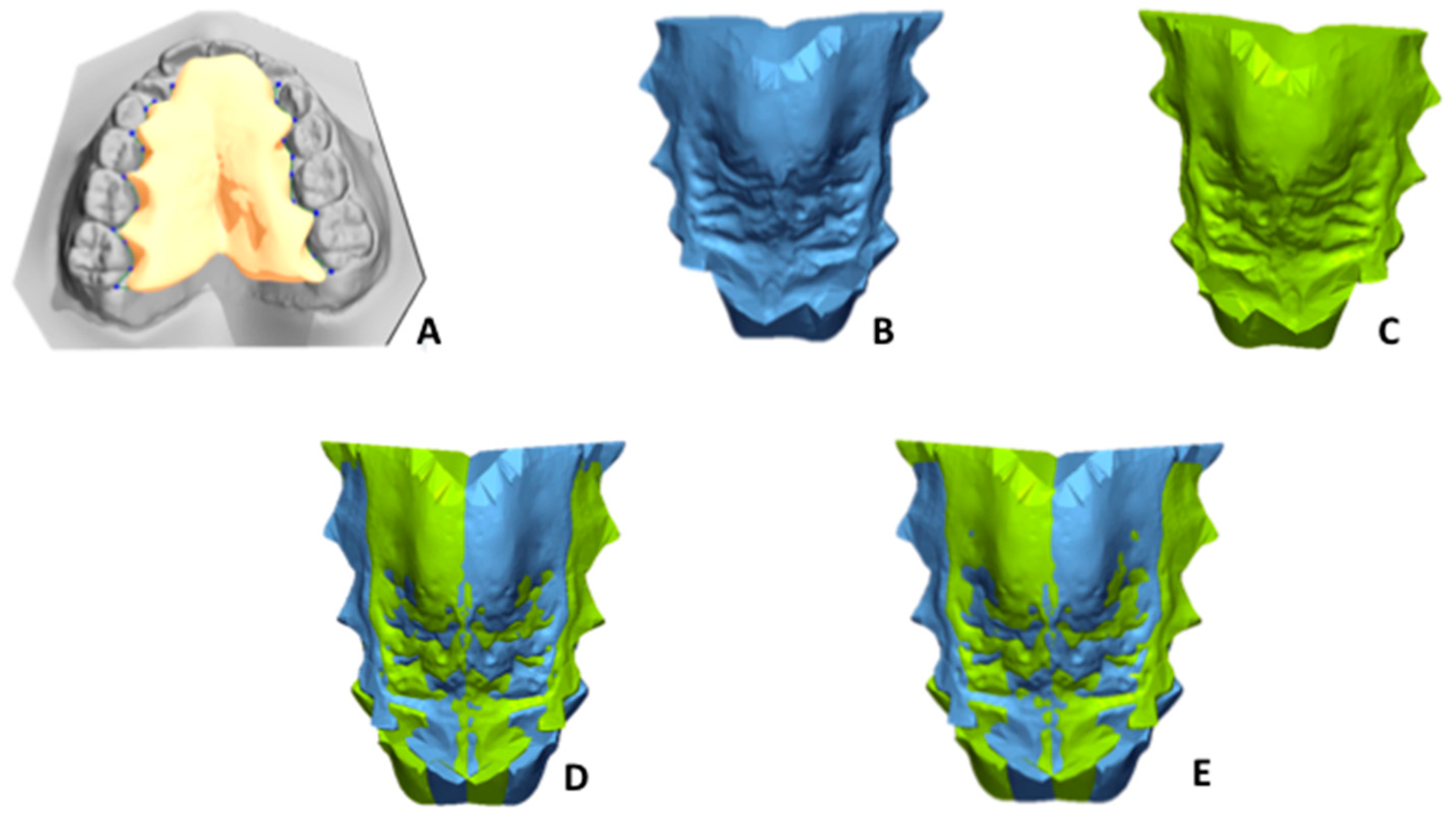
- To define the palate surface of the 3D model to be analysed, a gingival plane had to pass through all the most apical points of the dento-gingival junction of all the teeth (from first right molar to first left molar, Figure 8A).
- Step 1: Mirroring. Mirroring consists of converting the image orientation from right–left, antero–posterior, and infero–superior to left–right, antero–posterior, and infero–superior (Figure 8B,C).
- Step 2: First registration. Initial manual superimposition of the two models. Pairs of models (the original and the mirrored one of the same patient) were oriented and approximately registered by using the MPP and a line drawn perpendicularly through point two of the MPP. (Figure 8D).
- Step 3. Final registration: Final registration was made using the “best-fit alignment” option in the Geomagic Control X software. The precision of the registration was set to at least 0.3 mm (tolerance type: “3D Deviation”) with a maximum of 100,000 polygons for surface representation. The corresponding polygons from selected reference areas were automatically superimposed (Figure 8E).
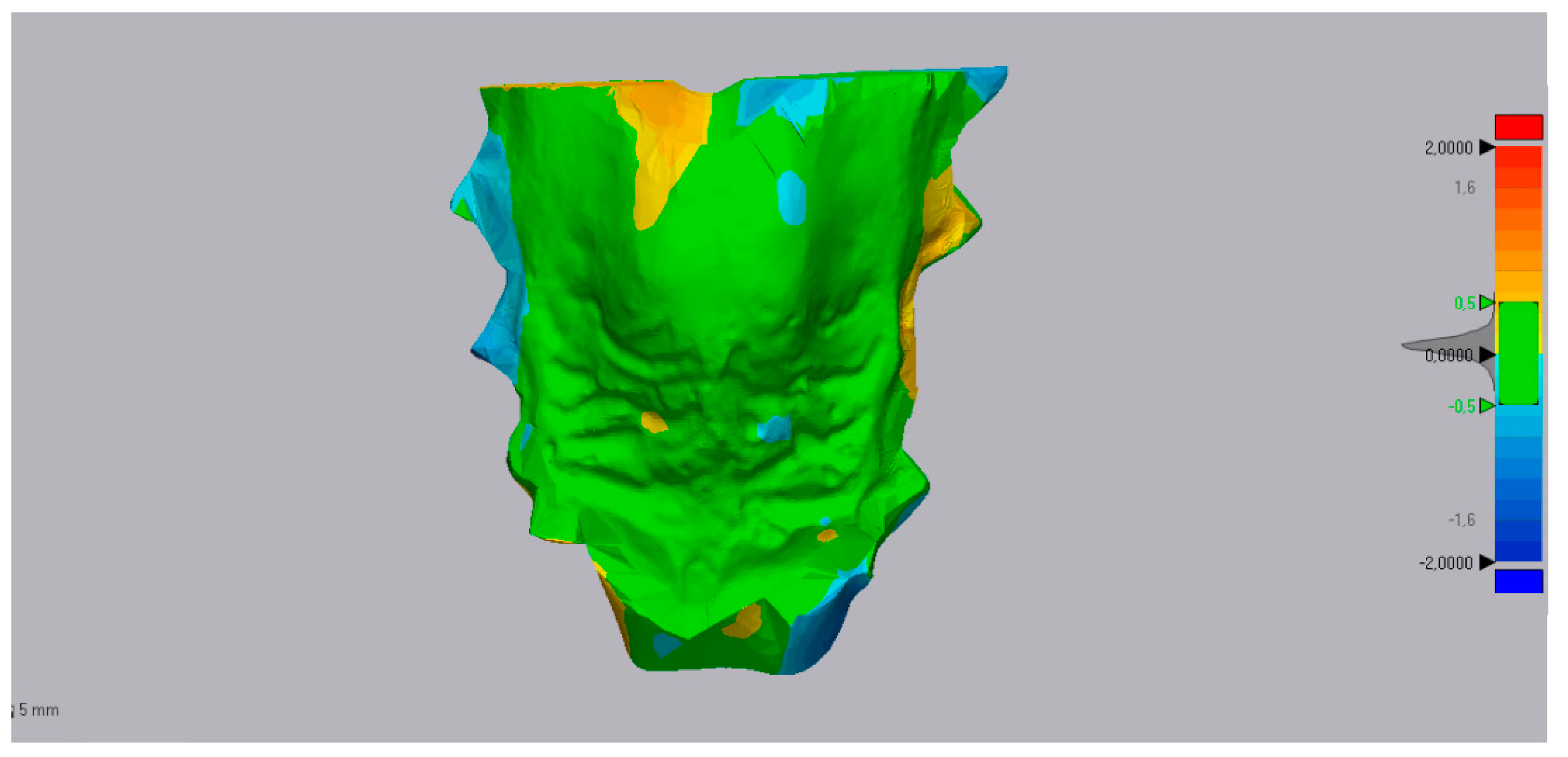
- Step 4. Superimposition and 3D analysis: The distances between corresponding areas of the original maxillary cast and the corresponding mirrored one were compared to obtain color-coded maps (Figure 9). The yellow-to-red fields indicated that the definitive casts were larger than the master model, and the turquoise-to-dark blue fields indicated that the definitive casts were smaller than the master model. The 3D deviation analysis has a tolerance range (green) of ±0.50 mm with a maximum of 2 mm. All the values in this range indicated the matching percentage between the two specular 3D models.
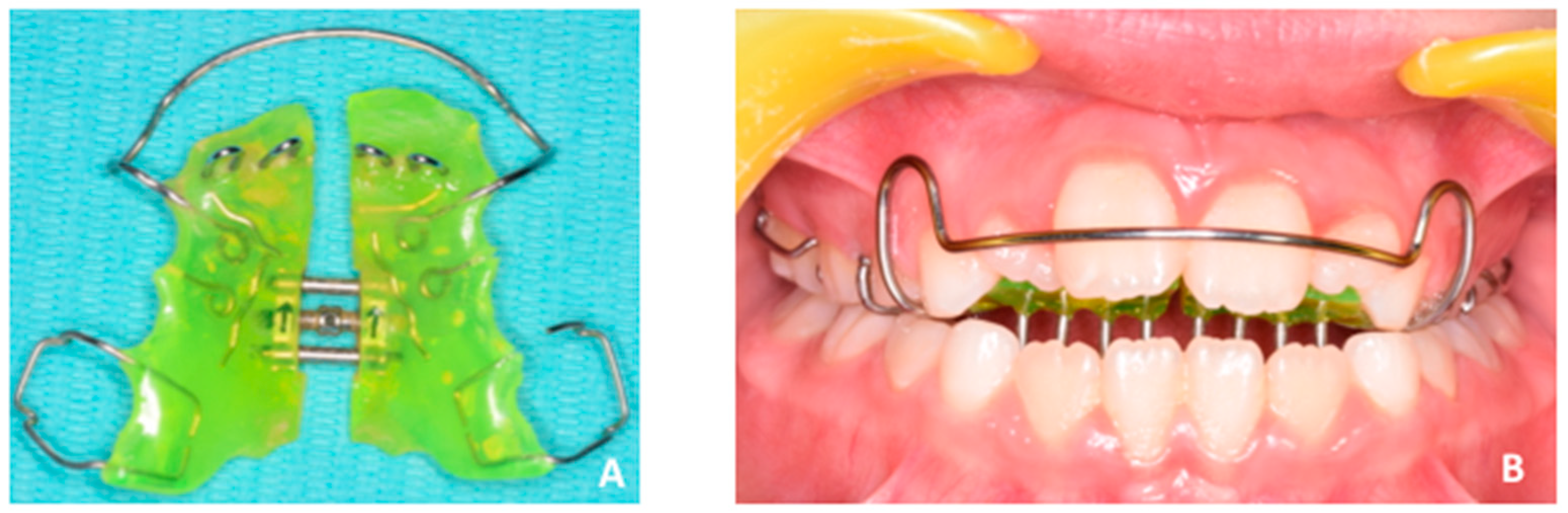
2.4. Diagnosis and Treatment Plan
2.5. PBM Administration
3. Results
4. Discussion
5. Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Silva Filho, O.G.; Santamaria, M.; Jrand Capelozza Filho, L. Epidemiology of posterior crossbite in the primary dentition. J. Clin. Pediatr. Dent. 2007, 32, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Quinzi, V.; Rossi, O.; Paglia, L.; Marzo, G.; Caprioglio, A. Paediatric Orthodontics Part 2: Periodontal effects of maxillary expansion. Eur. J. Paediatr. Dent. 2019, 20, 164–166. [Google Scholar] [PubMed]
- Lo Giudice, A.; Fastuca, R.; Portelli, M.; Militi, A.; Bellocchio, M.; Spinuzza, P.; Briguglio, F.; Caprioglio, A.; Nucera, R. Effects of rapid vs slow maxillary expansion on nasal cavity dimensions in growing subjects: A methodological and reproducibility study. Eur. J. Paediatr. Dent. 2017, 18, 299–304. [Google Scholar] [PubMed]
- McNamara, J.A. Maxillary transverse deficiency. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 567–570. [Google Scholar] [CrossRef]
- Leonardi, R.; Lo Giudice, A.; Rugeri, M.; Muraglie, S.; Cordasco, G.; Barbato, E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018, 40, 556–562. [Google Scholar] [CrossRef]
- Isola, G.; Anastasi, G.; Matarese, G.; Williams, R.C.; Cutroneo, G.; Bracco, P.; Piancino, M.G. Functional and molecular outcomes of the human masticatory muscles. Oral Dis. 2018, 24, 1428–1441. [Google Scholar] [CrossRef]
- Primožic, J.; Baccetti, T.; Franchi, L.; Richmond, S.; Farčnik, F.; Ovsenik, M. Three-dimensional assessment of palatal change in a controlled study of unilateral posterior crossbite correction in the primary dentition. Eur. J. Orthod. 2013, 35, 199–204. [Google Scholar] [CrossRef]
- Ganzer, N.; Feldmann, I.; Liv, P.; Bondemark, L. A novel method for superimposition and measurements on maxillary digital 3D models-studies on validity and reliability. Eur. J. Orthd. 2017, 40, 45–51. [Google Scholar] [CrossRef]
- Kapila, S.D.; Nervina, J.M. CBCT in orthodontics: Assessment of treatment outcomes and indications for its use. Dentomaxillofac. Radiol. 2015, 44, 20140282. [Google Scholar] [CrossRef]
- Leonardi, R.; Muraglie, S.; Lo Giudice, A.; Aboulazm, K.S.; Nucera, R. Evaluation of mandibular symmetry and morphology in adult patients with unilateral posterior crossbite. A CBCT study using a surface-to-surface matching technique. Eur. J. Orthod. 2020. [Epub ahead of print]. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Brewer, I.; Leonardi, R.; Roberts, N.; Bagnato, G. Pain threshold and temporomandibular function in systemic sclerosis: Comparison with psoriatic arthritis. Clin. Rheumatol. 2018, 37, 1861–1867. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Nucera, R.; Leonardi, R.; Paiusco, A.; Baldoni, M.; Caccianiga, G. A comparative assessment of the efficiency of orthodontic treatment with and without photobiomodulation during mandibular de-crowding in young subjects: A single-center, single blind randomized controlled trial. Photobiomodul Photomed. Laser Surg. 2020. [Epub ahead of print]. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Nucera, R.; Perillo, L.; Paiusco, A.; Caccianiga, G. Is Low-Level Laser Therapy an Effective Method to Alleviate Pain Induced by Active Orthodontic Alignment Archwire? A Randomized Clinical Trial. J. Evid. Based Dent. Pract. 2019, 19, 71–78. [Google Scholar] [CrossRef]
- Caccianiga, G.; Crestale, C.; Cozzani, M.; Piras, A.; Mutinelli, S.; Lo Giudice, A.; Cordasco, G. Low-level laser therapy and invisible removal aligners. J. Biol. Regul. Homeost. Agents 2016, 30 (Suppl. 1), 107–113. [Google Scholar]
- Caccianiga, G.; Paiusco, A.; Perillo, L.; Nucera, R.; Pinsino, A.; Maddalone, M.; Cordasco, G.; Lo Giudice, A. Does low-level laser therapy enhance the efficiency of orthodontic dental alignment? Results from a randomized pilot study. Photomed. Laser Surg. 2017, 35, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.H.; Liu, S.L.; Chen, C.L.; Shie, M.Y.; Kao, C.T. Low-level laser effects on simulated orthodontic tension side periodontal ligament cells. Photomed. Laser Surg. 2013, 31, 72–77. [Google Scholar] [CrossRef]
- Eells, J.T.; Henry, M.M.; Summerfelt, P.; Wong-Riley, M.T.; Buchmann, E.V.; Kane, M.; Whelan, N.T.; Whelan, H.T. Therapeutic photobiomodulation for methanol-induced retinal toxicity. Proc. Natl. Acad. Sci. USA 2003, 100, 3439–3444. [Google Scholar] [CrossRef]
- Oron, U.; Ilic, S.; De Taboada, L.; Streeter, J. Ga-As (808 nm) laser irradiation enhances ATP production in human neuronal cells in culture. Photomed. Laser Surg. 2007, 25, 180–182. [Google Scholar] [CrossRef]
- Paduano, F.; Marrelli, M.; Alom, N.; Amer, M.; White, L.J.; Shakesheff, K.M.; Tatullo, M. Decellularized bone extracellular matrix and human dental pulp stem cells as a construct for bone regeneration. J. Biomater. Sci. Polym. Ed. 2017, 28, 730–748. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Ramaglia, L.; Cicciù, M.; Matarese, G. Evaluation of the efficacy of celecoxib and ibuprofen on postoperative pain, swelling, and mouth opening after surgical removal of impacted third molars: A randomized, controlled clinical trial. Int. J. Oral Maxillofacial Surg. 2019, 48, 1348–1354. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Caccianiga, G.; Crimi, S.; Cavallini, C.; Leonardi, R. Frequency and type of ponticulus posticus in a longitudinal sample of nonorthodontically treated patients: Relationship with gender, age, skeletal maturity, and skeletal malocclusion. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Lo Giudice, A.; Bellocchio, M.; Spinuzza, P.; Caprioglio, A.; Cordasco, G. Diagnostic concordance between skeletal cephalometrics, radiograph-based soft-tissue cephalometrics, and photograph-based soft-tissue cephalometrics. Eur. J. Orthod. 2017, 39, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Perillo, L.; Migliorati, M.; Matarese, M.; Dalessandri, D.; Grassia, V.; Alibrandi, A.; Matarese, G. The impact of temporomandibular joint arthritis on functional disability and global health in patients with juvenile idiopathic arthritis. Eur. J. Orthod. 2019, 29, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Massaro, C.; Losada, C.; Cevidanes, L.; Yatabe, M.; Garib, D.; Lauris, J.R.P.; Ioshida, M.; Rey, D.; Alvarez, M.A.; Benavides, E.; et al. Comparison of linear and angular changes assessed in digital dental models and cone-beam computed tomography. Orthod. Craniofac. Res. 2019, 23, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Maurice, T.J.; Kula, K. Dental arch asymmetry in the mixed dentition. Angle Orthod. 1998, 68, 37–44. [Google Scholar] [PubMed]
- Leonardi, R. Cone-beam computed tomography and three-dimensional orthodontics. Where we are and future perspectives. J. Orthod. 2019, 46 (Suppl. 1), 45–48. [Google Scholar] [CrossRef]
- Maspero, C.; Abate, A.; Bellincioni, F.; Cavagnetto, D.; Lanteri, V.; Costa, A.; Farronato, M. Comparison of a tridimensional cephalometric analysis performed on 3T-MRI compared with CBCT: A pilot study in adults. Prog. Orthod. 2019, 20, 40. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, G.; Ramaglia, L.; Pedullà, E.; Rapisarda, E.; Iorio-Siciliano, V. Association between periodontitis and glycosylated haemoglobin before diabetes onset: A cross-sectional study. Clin. Oral Investig. 2019. [Google Scholar] [CrossRef]
- Piancino, M.G.; Isola, G.; Cannavale, R.; Cutroneo, G.; Vermiglio, G.; Bracco, P.; Anastasi, G.P. From periodontal mechanoreceptors to chewing motor control: A systematic review. Arch. Oral Biol. 2017, 78, 109–121. [Google Scholar] [CrossRef]
- Piancino, M.G.; Di Benedetto, L.; Matacena, G.; Deregibus, A.; Marzo, G.; Quinzi, V. Paediatric Orthodontics Part 3: Masticatory function during development. Eur. J. Paediatr. Dent. 2019, 20, 247–249. [Google Scholar]
- Lo Giudice, A.; Barbato, E.; Cosentino, L.; Ferraro, C.M.; Leonardi, R. Alveolar bone changes after rapid maxillary expansion with tooth-born appliances: A systematic review. Eur. J. Orthod. 2018, 40, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Rosa, M.; Quinzi, V.; Marzo, G. Paediatric Orthodontics Part 1: Anterior open bite in the mixed dentition. Eur. J. Paediatr. Dent. 2019, 20, 80–82. [Google Scholar] [PubMed]
- Isola, G.; Polizzi, A.; Muraglie, S.; Leonardi, R.; Lo Giudice, A. Assessment of Vitamin C and Antioxidant Profiles in Saliva and Serum in Patients with Periodontitis and Ischemic Heart Disease. Nutrients 2019, 11, 2956. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Ferlito, S. Expression of Salivary and Serum Malondialdehyde and Lipid Profile of Patients with Periodontitis and Coronary Heart Disease. Int. J. Mol. Sci. 2019, 20, 6061. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Alibrandi, A.; Currò, M.; Matarese, M.; Ricca, S.; Matarese, G.; Ientile, R.; Kocher, T. Evaluation of salivary and serum ADMA levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020. [Google Scholar] [CrossRef] [PubMed]
- González Espinosa, D.; Santos, M.; Mendes, S.M.D.A.; Normando, D. Mandibular propulsion appliance for adults with Class II malocclusion: A systematic review and meta-analysis. Eur. J. Orthod. 2019, cjz089. [Google Scholar] [CrossRef]
- Muniz, R.S.C.; Carvalho, C.N.; Aranha, A.C.C.; Dias, F.M.C.S.; Ferreira, M.C. Efficacy of low-level laser therapy associated with fluoride therapy for the desensitisation of molar-incisor hypomineralisation: Randomised clinical trial. Int. J. Paediatr. Dent. 2019. [Epub ahead of print]. [Google Scholar] [CrossRef]
- Kobayashi, F.Y.; Castelo, P.M.; Gonçalves, M.L.L.; Motta, L.J.; Mota, A.C.D.C.; Altavista, O.M.; Pinto, M.M.; Salgueiro, M.C.; Ferreira, K.P.S.; Bussadori, S.K. Evaluation of the effectiveness of infrared light-emitting diode photobiomodulation in children with sleep bruxism: Study protocol for randomized clinical trial. Medicine 2019, 98, e17193. [Google Scholar] [CrossRef]
- Caccianiga, G.; Lo Giudice, A.; Paiusco, A.; Portelli, M.; Militi, A.; Baldoni, M.; Nucera, R. Maxillary Orthodontic Expansion Assisted by Unilateral Alveolar Corticotomy and Low-Level Laser Therapy: A Novel Approach for Correction of a Posterior Unilateral Cross-Bite in Adults. J. Lasers Med. Sci. 2019, 10, 225–229. [Google Scholar] [CrossRef]
- Lo Giudice, G.; Lo Giudice, A.; Isola, G.; Fabiano, F.; Artemisia, A.; Fabiano, V.; Nucera, R.; Matarese, G. Evaluation of bond strength and detachment interface distribution of different bracket base designs. Acta Med. Mediterr 2015, 31, 585. [Google Scholar]
- Nucera, R.; Militi, A.; Lo Giudice, A.; Longo, V.; Fastuca, R.; Caprioglio, A.; Cordasco, G.; Papadopoulos, M.A. Skeletal and Dental Effectiveness of Treatment of Class II Malocclusion With Headgear: A Systematic Review and Meta-analysis. J. Evid. Based Dent. Pract. 2018, 18, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Traini, T.; Danza, M.; Zollino, I.; Altavilla, R.; Lucchese, A.; Sollazzo, V.; Trapella, G.; Brunelli, G.; Carinci, F. Histomorphometric evaluation of an immediately loaded implant retrieved from human mandible after 2 years. Int. J. Immunopathol. Pharmacol. 2011, 24, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Pastorino, R.; Gherlone, E.F.; Perillo, L.; Lupi, S.M.; Lucchese, A. Histomorphometric evaluation of two different bone substitutes in sinus augmentation procedures: A randomized controlled trial in humans. Int. J. Oral Maxillofac. Implants 2017, 32, 188–194. [Google Scholar]
- Isola, G.; Alibrandi, A.; Pedullà, E.; Grassia, V.; Ferlito, S.; Perillo, L.; Rapisarda, E. Analysis of the effectiveness of Lornoxicam and Flurbiprofen on management of pain and sequelae following third molar surgery: A randomized, controlled, clinical trial. J. Clin. Med. 2019, 8, 325. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Matarese, M.; Ramaglia, L.; Iorio-Siciliano, V.; Cordasco, G.; Matarese, G. Efficacy of a drug composed of herbal extracts on postoperative discomfort after surgical removal of impacted mandibular third molar: A randomized, triple-blind, controlled clinical trial. Clin. Oral Investig. 2019, 23, 2443–2453. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of Endothelin-1 concentrations in individuals with periodontitis. Sci. Rep. 2020. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Rapisarda, E.; Matarese, G.; Williams, R.C.; Leonardi, R. Association of vitamin d in patients with periodontal and cardiovascular disease: A cross-sectional study. J. Periodontal Res. 2020, in press. [Google Scholar]
- Spagnuolo, G.; Ametrano, G.; D’Antò, V.; Rengo, C.; Simeone, M.; Riccitiello, F.; Amato, M. Effect of autoclaving on the surfaces of TiN -coated and conventional nickel-titanium rotary instruments. Int. Endod. J. 2012, 45, 1148–1155. [Google Scholar] [CrossRef]
- Spagnuolo, G.; Ametrano, G.; D’Antò, V.; Formisano, A.; Simeone, M.; Riccitiello, F.; Amato, M.; Rengo, S. Microcomputed tomography analysis of mesiobuccal orifices and major apical foramen in first maxillary molars. Open Dent. J. 2012, 6, 118–125. [Google Scholar] [CrossRef]
- Ametrano, G.; D’Antò, V.; Di Caprio, M.P.; Simeone, M.; Rengo, S.; Spagnuolo, G. Effects of sodium hypochlorite and ethylenediaminetetraacetic acid on rotary nickel-titanium instruments evaluated using atomic force microscopy. Int. Endod. J. 2011, 44, 203–209. [Google Scholar] [CrossRef]
- Cavuoti, S.; Matarese, G.; Isola, G.; Abdolreza, J.; Femiano, F.; Perillo, L. Combined orthodontic-surgical management of a transmigrated mandibular canine: A case report. Angle Orthod. 2016, 86, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Currò, M.; Matarese, G.; Isola, G.; Caccamo, D.; Ventura, V.P.; Cornelius, C.; Lentini, M.; Cordasco, G.; Ientile, R. Differential expression of transglutaminase genes in patients with chronic periodontitis. Oral Dis. 2014, 20, 616–623. [Google Scholar] [CrossRef]
- Matarese, G.; Isola, G.; Alibrandi, A.; Lo Gullo, A.; Bagnato, G.; Cordasco, G.; Perillo, L. Occlusal and MRI characterizations in systemic sclerosis patients: A prospective study from Southern Italian cohort. Jt. Bone Spine 2016, 83, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Matarese, G.; Currò, M.; Isola, G.; Caccamo, D.; Vecchio, M.; Giunta, M.L.; Ramaglia, L.; Cordasco, G.; Williams, R.C.; Ientile, R. Transglutaminase 2 up-regulation is associated with RANKL/OPG pathway in cultured HPDL cells and THP-1-differentiated macrophages. Amino Acids 2015, 47, 2447–2455. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Lo Giudice, A.; Polizzi, A.; Alibrandi, A.; Patini, R.; Ferlito, S. Periodontitis and Tooth Loss Have Negative Systemic Impact on Circulating Progenitor Cell Levels: A Clinical Study. Genes 2019, 7, 1022. [Google Scholar] [CrossRef]
- Varella, A.M.; Revankar, A.V.; Patil, A.K. Low-level laser therapy increases interleukin-1β in gingival crevicular fluid and enhances the rate of orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 535–544. [Google Scholar] [CrossRef]
- Farronato, M.; Maspero, C.; Lanteri, V.; Fama, A.; Ferrati, F.; Pettenuzzo, A.; Farronato, D. Current state of the art in the use of augmented reality in dentistry: A systematic review of the literature. BMC Oral Health 2019, 19, 135. [Google Scholar] [CrossRef]



© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quinzi, V.; Ronsivalle, V.; Campanella, V.; Mancini, L.; Torrisi, S.; Lo Giudice, A. New Technologies in Orthodontics: A Digital Workflow to Enhance Treatment Plan and Photobiomodulation to Expedite Clinical Outcomes. Appl. Sci. 2020, 10, 1495. https://doi.org/10.3390/app10041495
Quinzi V, Ronsivalle V, Campanella V, Mancini L, Torrisi S, Lo Giudice A. New Technologies in Orthodontics: A Digital Workflow to Enhance Treatment Plan and Photobiomodulation to Expedite Clinical Outcomes. Applied Sciences. 2020; 10(4):1495. https://doi.org/10.3390/app10041495
Chicago/Turabian StyleQuinzi, Vincenzo, Vincenzo Ronsivalle, Vincenzo Campanella, Leonardo Mancini, Salvatore Torrisi, and Antonino Lo Giudice. 2020. "New Technologies in Orthodontics: A Digital Workflow to Enhance Treatment Plan and Photobiomodulation to Expedite Clinical Outcomes" Applied Sciences 10, no. 4: 1495. https://doi.org/10.3390/app10041495
APA StyleQuinzi, V., Ronsivalle, V., Campanella, V., Mancini, L., Torrisi, S., & Lo Giudice, A. (2020). New Technologies in Orthodontics: A Digital Workflow to Enhance Treatment Plan and Photobiomodulation to Expedite Clinical Outcomes. Applied Sciences, 10(4), 1495. https://doi.org/10.3390/app10041495







