“Pull-through” Resection for Total and Subtotal Glossectomy Involving the Posterior Third of Tongue
Abstract
1. Introduction
2. Materials and Methods
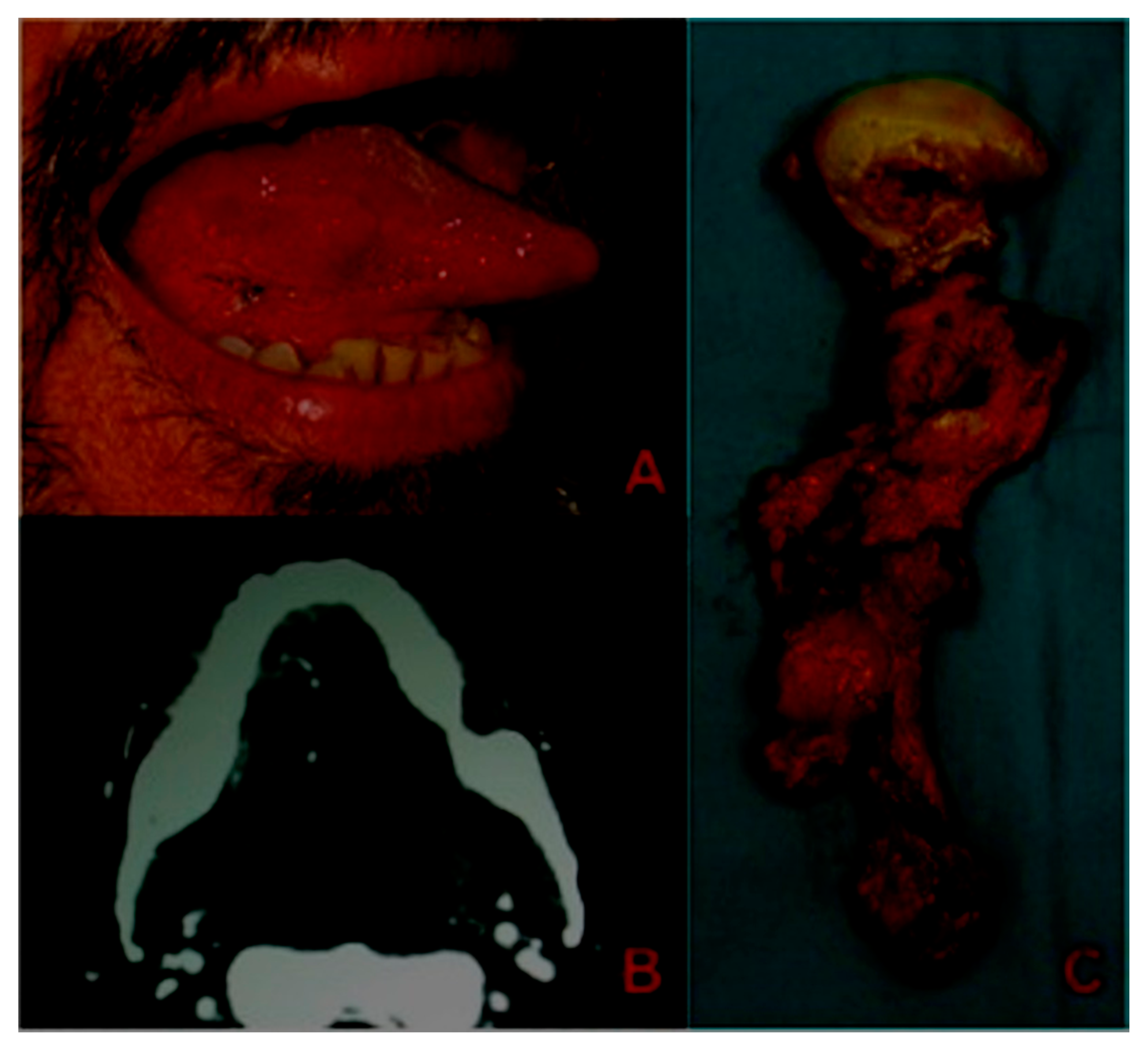
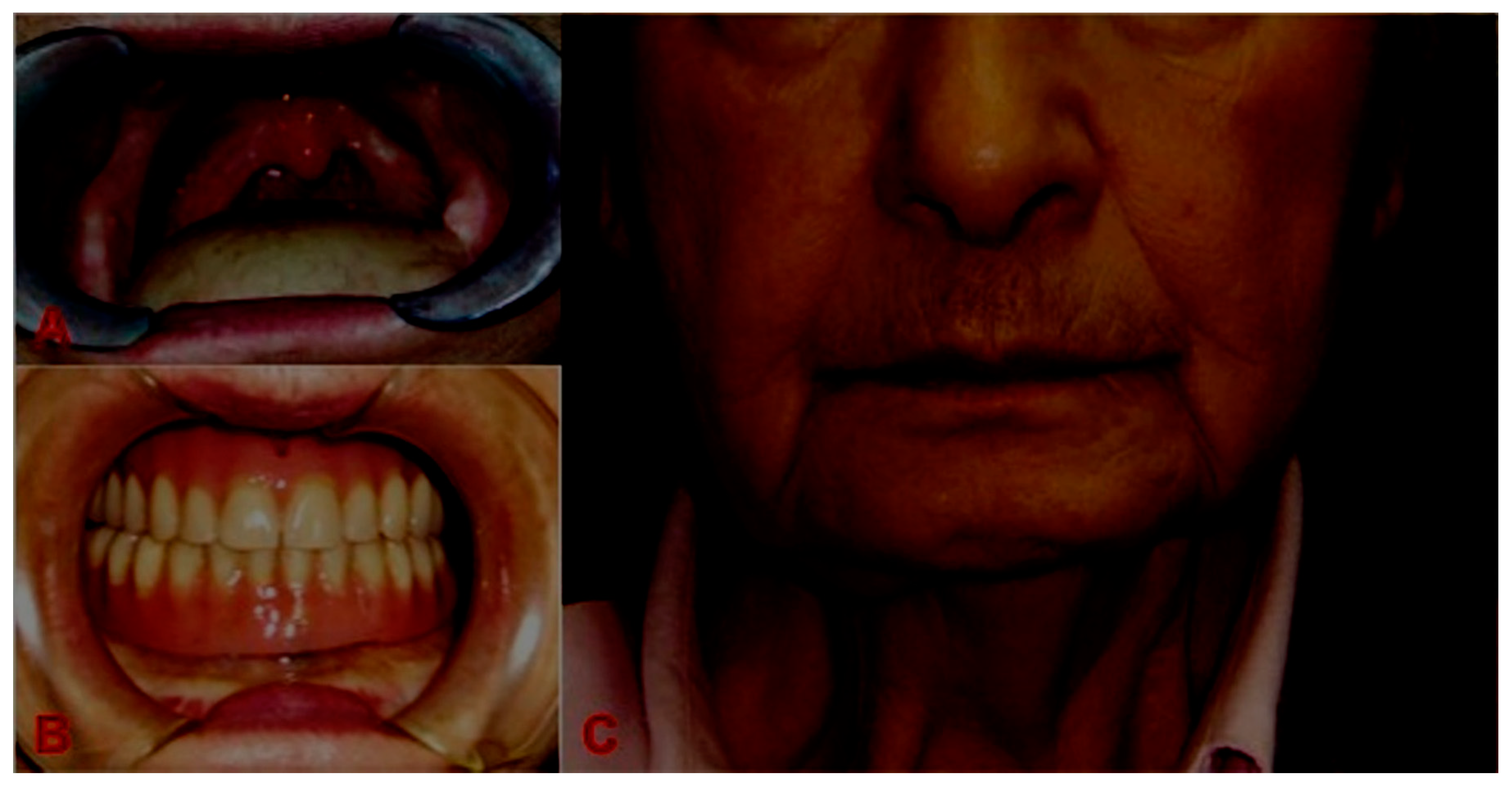
Surgical Technique
3. Results
4. Discussion
5. Conclusions
- a)
- to gain three-dimensional resection of the tumor: Theoretically, the lip-splitting technique in conjunction with a mandibulotomy allows us to obtain a clear visualization of the tumor in order to obtain a wide resection. Nevertheless, it has been found that clear margins can also be achieved in patients treated using the “pull-through” technique [10]. In our study we found a rate of free margin comparable to the one found in the case of the lip-splitting approach.
- b)
- to facilitate flap inset: Obviously, flap inset is easier if the proximal mandible is swung outwards, and theoretically the post-operative complication rate should be lower. According to other authors [12], there is not found a high rate of flap failure, for both the use of free or pedicled flaps. In our practice, we obviously prefer to use free flaps (usually ALT), and we reserve the use of pectoralis pedicled flaps for those cases in which it is not possible due to the patient’s condition. In particular, reconstruction was performed with free flaps in 29 cases, and only a 3.4% partial flap necrosis was observed.
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7. [Google Scholar] [CrossRef] [PubMed]
- Gatta, G.; Botta, L.; Sánchez, M.J.; Anderson, L.A.; Pierannunzio, D.; Licitra, L.; Eurocare Working Group. Prognoses and improvement for head and neck cancers diagnosed in Europe in early 2000s: The EUROCARE-5 population-based study. Eur. J. Cancer 2015, 51, 2130. [Google Scholar] [PubMed]
- Ward, G.; Robben, J.O. The Composite Operation for Radical Neck Dissection and Removal of Cancer of the Mouth. Cancer 1951, 4, 98. [Google Scholar] [CrossRef]
- Slaughter, D.P.; Southwick, H.W. En bloc resection of cancer of the mouth and cervical lymphatics with preservation of the mandible. Ann. Surg. 1952, 136, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Spiro, R.H.; Gerold, F.P.; Strong, E.W. Mandibular “swing” approach for oral and oropharyngeal tumors. Head Neck Surg. 1981, 3, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Gooris, P.J.J.; Worthington, P.; Evans, J.R. Mandibulotomy: A surgical approach to oral and pharyngeal lesions. Int. J. Oral Maxillofac. Surg. 1989, 18, 359–364. [Google Scholar] [CrossRef]
- Baek, C.H.; Lee, S.W.; Jeong, H.S. New modification of the mandibulotomy approach without lip splitting. Head Neck 2006, 28, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Valentini, V.; Cassoni, A.; Marianetti, T.M.; Battisti, A.; Terenzi, V.; Iannetti, G. Anterolateral thigh flap for the reconstruction of head and neck defects: Alternative or replacement of the radial forearm flap? J. Craniofac. Surg. 2008, 19, 1148–1153. [Google Scholar] [CrossRef] [PubMed]
- Martin, H.; DelValle, B.; Ehrlick, H.; Cahan, W.G. Neck Dissection. Cancer 1951, 4, 441–499. [Google Scholar] [CrossRef]
- Ral, L.P.; Shukla, M.; Sharma, V.; Pandey, M. Mandibular conservation in oral cancer. Surg. Oncol. 2012, 21, 109–118. [Google Scholar]
- Myers, L.L.; Sumer, B.D.; Truelson, J.M.; Ahn, C.; Leach, J.L. Resection and free tissue reconstruction of locally advanced oral cancer: Avoidance of lip split. Microsurgery 2011, 31, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Stanley, R.B. Mandibular lingual releasing approach to Oral and Oropharyngeal carcinomas. Laryngoscope 1984, 94, 596–600. [Google Scholar] [CrossRef] [PubMed]
- Devine, J.C.; Rogers, S.N.; McNally, D.; Brown, J.S.; Vaughan, E.D. A comparison of aesthetic, functional and patient subjective outcomes following lip-split mandibulotomy and mandibular lingual releasing access procedures. Int. J. Oral Maxillofac. Surg. 2001, 30, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Gieringer, M.; Gosepath, J.; Naim, R. Radiotherapy and wound healing: Principles, management and prospects. Oncol. Rep. 2011, 26, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, L.; Giugliano, G.; Bruschini, R.; Ansarin, M.; Navach, V.; Grosso, E.; Gibelli, B.; Ostuni, A.; Chiesa, F. Compartmental surgery in tongue tumours: Description of a new surgical technique. Acta Otorhinolaryngol. Ital. 2009, 29, 259–264. [Google Scholar] [PubMed]
- Chang, E.I.; Yu, P.; Skoracki, R.J.; Liu, J.; Hanasono, M.M. Comprehensive analysis of functional outcomes and survival after microvascular reconstruction of glossectomy defects. Ann. Surg. Oncol. 2015, 22, 3061–3069. [Google Scholar] [CrossRef] [PubMed]
- Dziegielewski, P.T.; O’Connell, D.A.; Rieger, A.; Harris, J.R.; Seikaly, H. The lip-splitting mandibulotomy: Aesthetic and functional outcomes. Oral Oncol. 2010, 46, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Cilento, B.W.; Izzard, M.; Weymuller, E.A.; Futran, N. Comparison of approaches for oral cavity cancer resection: Lip-split versus visor flap. Otolaryngol. Head Neck Surg. 2007, 137, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Dziegielewski, P.T.; Mlynarek, A.M.; Dimitry, J.; Harris, J.R.; Seikaly, H. The mandibulotomy: Friend or foe? Safety outcomes and literature review. Laryngoscope 2009, 119, 2369–2375. [Google Scholar] [CrossRef] [PubMed]


| Variables | N° of pts (%) |
|---|---|
| Histology | |
| SCC | 42 (95.5%) |
| ACC | 2 (4.5%) |
| pT classification | |
| T1–T2 | 35 (79.5%) |
| T3–T4a | 9 (20.5%) |
| Reconstruction | |
| RFFF | 2 (4.5%) |
| ALTFF | 26 (59%) |
| Pectoralis major | 15 (34%) |
| Rectus abdominis | 1 (2.5%) |
| Resection margins | |
| R0 | 39 (89%) |
| Close | 1 (2.5%) |
| R1 | 2 (4.5%) |
| Type of ND | |
| RND/MRND | 28 (54%) |
| SND | 24 (46%) |
| Complications | |
| Fistula | 2 (4.5%) |
| Flap necrosis | 1 (partial) (2.5%) |
| Sex | Age | Risk Factors | Resection | Histology | Reconstruction | Complications | Adjiuvant Treatment | Relapse | FU |
|---|---|---|---|---|---|---|---|---|---|
| M | 60 | Smoker, Alcohol abuse | Subtotal glossectomy + RND | SCC pT2pN2b G3 Pn1 DOI: 10 mm R0 | Radial free flap | None | CHT-RT | rT/N (18 months) | DWD |
| M | 48 | Ex smoker | Subtotal glossectomy + left MRND and right SND | SCC pT3pN0 G2 Pn1 DOI: 11 mm R1 | Pectoralis major flap | None | CHT-RT | rT (6 months) | DWD |
| M | 72 | Smoker | Subtotal glossectomy + right MRND and left SND | SCC pT2pN1 G2 Pn1 DOI: 12 mm R0 | ALT | None | CHT-RT | rM (14 months) | DWD |
| F | 53 | None | Subtotal glossectomy + SND | SCC pT2pN0 G2 Pn0 DOI: 6 mm R0 | ALT | None | None | rN (7 months) | DWD |
| F | 63 | Smoker, previous alcohol abuse | Subtotal glossectomy + left MRD + right SND | SCC pT3pN2c G2 Pn1 DOI: 10 mm R0 | Pectoralis major flap | None | CHT-RT | rM (8 months) | DWD |
| F | 33 | Smoker | Subtotal glossectomy + SND | ACC pT2pN0 Pn1 DOI:10 mm R0 | ALT | None | RT | rM (9 months) | AWD |
| M | 52 | Smoker | Subtotal glossectomy + MRND | SCC pT2pN2b G3 pN1 DOI: 11 mm R0 | Pectoralis major flap | None | CHT-RT | rN (7 months) | DWD |
| F | 39 | Ex smoker, Lichen planus | Subtotal glossectomy + SND | SCC pT1pN0 G1 Pn1 DOI: 5 mm R0 | ALT | None | None | rT (4 months) | AWD |
| F | 75 | Smoker, previous alcohol abuse | Subtotal glossectomy + MRND | SCC pT2pN2b G2 Pn1 DOI: 8 mm R0 | Pectoralis major flap | Oro-cervical fistula | RT | rT (4 months) | DWD |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Della Monaca, M.; Terenzi, V.; Raponi, I.; Priore, P.; Battisti, A.; Cassoni, A.; Nocini, R.; Tenore, G.; Brauner, E.; Romeo, U.; et al. “Pull-through” Resection for Total and Subtotal Glossectomy Involving the Posterior Third of Tongue. Appl. Sci. 2020, 10, 8580. https://doi.org/10.3390/app10238580
Della Monaca M, Terenzi V, Raponi I, Priore P, Battisti A, Cassoni A, Nocini R, Tenore G, Brauner E, Romeo U, et al. “Pull-through” Resection for Total and Subtotal Glossectomy Involving the Posterior Third of Tongue. Applied Sciences. 2020; 10(23):8580. https://doi.org/10.3390/app10238580
Chicago/Turabian StyleDella Monaca, Marco, Valentina Terenzi, Ingrid Raponi, Paolo Priore, Andrea Battisti, Andrea Cassoni, Riccardo Nocini, Gianluca Tenore, Edoardo Brauner, Umberto Romeo, and et al. 2020. "“Pull-through” Resection for Total and Subtotal Glossectomy Involving the Posterior Third of Tongue" Applied Sciences 10, no. 23: 8580. https://doi.org/10.3390/app10238580
APA StyleDella Monaca, M., Terenzi, V., Raponi, I., Priore, P., Battisti, A., Cassoni, A., Nocini, R., Tenore, G., Brauner, E., Romeo, U., Polimeni, A., & Valentini, V. (2020). “Pull-through” Resection for Total and Subtotal Glossectomy Involving the Posterior Third of Tongue. Applied Sciences, 10(23), 8580. https://doi.org/10.3390/app10238580












