Abstract
This study aimed to prove the hypothesis that the medial structures of the ankle are interconnected through the flexor retinaculum’s projections. We conducted a retrospective re-evaluation of 132 MRI examinations of the ankle joint from 57 females and 75 males with an age range of 18–65 and a mean age of 35 years. The correlation between the presence of connections between the flexor retinaculum and the deltoid ligament, the spring ligament, the inferior extensor retinaculum, the paratenon, the fibulotalocalcaneal ligament, the fascia covering the abductor hallucis, and the flexor fibrous sheath were studied. The most common connections of the flexor retinaculum were to the deltoid ligament (97%), the fibulotalocalcaneal ligament (84.1%), and the flexor fibrous sheath (83.3%). Interconnection between the flexor retinaculum and the deltoid ligament correlated with the presence of connections between the flexor retinaculum and the inferior extensor retinaculum, the paratenon, and the spring ligament. Side difference was noticed in connections to the flexor fibrous sheath, the deltoid ligament, the fascia on the abductor hallucis, and the paratenon (p < 0.05). The flexor retinaculum formed a more complex anatomical unit with adjacent structures.
1. Introduction
The primary function of the flexor retinaculum (FR) is to maintain the tibialis posterior and the flexor digitorum longus tendons to the underlying medial malleolus during the ankle joint movements [1]. This is supported by clinical observation of patients with injury or insufficiency of the FR after a tear, leading to subluxation of the posterior tibialis tendon over the medial malleolus edge [2]. The FR has a stabilizing and mechanical importance, tethering the tibialis posterior tendon, keeping it in the groove, and preventing dislocation [3]. Furthermore, it is also an essential element of proprioception, described in the literature as a typical fascial feature [1]. The retinaculum proprioception effect was used in the surgical transfer of the inferior extensor retinaculum (IER) to augment the superior peroneal retinaculum [1]. Diversified collagen fiber systems within the fascia, the ligament, or the tendons [4] enable several functional units to be combined into one anatomical structure [5].
The FR is a brad triangular structure, which extends from the medial malleolus to the posterosuperior aspect of the calcaneus [6]. The anterior extension of the FR is not described in detail. The FR limits the tarsal tunnel from the posterior and medial side and attaches to the medial malleolus, forming the anterior limit of the tarsal tunnel [7]. The tarsal tunnel continues inferiorly to the sustentaculum tali, the abductor halluces, and the plantar aponeurosis [6]. Projections of the FR divide the tarsal tunnel into smaller compartments for every tendon. The deltoid ligament (DL) is located laterally and inferiorly to the tarsal tunnel; however, there are no data on connections between these structures. Demarcation between retinaculum and other elements of the crural fascia is based on the relative change in thickness of the fascia as they form retinacula [6]. The literature on the anatomy of FR is exceptionally modest or even non-existent. Clinical observation of concomitant injury of the DL and spring ligament (SL) has no anatomical background. On the other hand, observation of concomitant injuries to the lateral ankle ligaments was supported by anatomical studies, where anatomical connections were noticed.
Concomitant injuries involving several structures are relatively common in the area of the medial malleolus. Injury of the SL has a high association with a tear of the tibialis posterior tendon or sinus tarsi alterations. Likewise, injuries of the posterior tibial tendon associate with plantar fascia tears [8]. A similar phenomenon of concomitant injuries, which are more common than a single structure injury, also occurs in the lateral malleolus area. The anatomical connections that resemble a complex between the anterior talofibular ligament, the calcaneofibular ligament, and the posterior talofibular ligament were described previously [9]. Connections of fascial elements, such as the fibulotalocalcaneal ligament (FTCL) and the paratenon, are visible in Kager’s fat pad [10]. This is an example of how the fascia system and the tendon system connects.
This study aims to test the hypothesis that the structures about the medial malleolus connect through the FR, which is a fascial element, and that these connections can be revealed on routine MRI of the ankle.
2. Materials and Methods
Our study included 57 females and 75 males with an age range of 18–65 and a mean age of 35 years. The right ankle was examined in 74 cases and the left ankle in 58 cases.
2.1. Inclusion and Exclusion Criteria
The ankle MRI examinations were performed in 2019 on 3.0 T scanners. MRI examination protocols could differ between cases, but we only included patients with at least proton density (PD) or T2-weighted images without fat saturation in axial and coronal sections. The exclusion criteria were trauma in the anamnesis (43 cases excluded), edema of the subcutaneous tissue (35 cases excluded), the presence of orthopedic hardware due to possible artifacts (19 cases excluded), a history of previous fracture (17 cases excluded), obvious abnormality about the medial malleolus (8 cases excluded), and obvious abnormality in the medial region of the ankle (2 cases excluded). In total, 132 MRI examinations of the ankle fulfilled inclusion and exclusion criteria. All studies were reviewed twice, and the final results were made by consensus.
2.2. Structures Included in The Study
We analyzed the presence of connections between the FR and adjacent structures. The following structures were included in this study: DL, SL, IER, paratenon of the Achilles tendon, FTCL, the fascia on the abductor hallucis (AbH), the fibrous sheath of flexors (FFS). We also analyzed whether the plantaris tendon is related to projections of the FR and the accessory navicular bone incidence.
Firstly, the FR was found on the horizontal sections based on the anatomical location. We then assessed where the FR ends by analyzing subsequent cross-sections and whether there is a clear difference between the FR, which was considered as an absent connection. The presence of a connection was recognized when the structures smoothly merged into each other. Observations were confirmed on the frontal images.
2.3. Statistics
To assess if one connection is correlated with other connections, we conducted a statistical analysis using the Pearson correlation coefficient. A p-value < 0.05 was considered statistically significant.
Cohen’s Kappa coefficient was used to determine interobserver agreement. A coefficient was calculated for each connection. The kappa coefficient ranges from −1 to +1, and agreements may be qualified as: excellent (>0.81), good (0.61–0.8), intermediate (0.21–0.60), or poor (<0.21) [11]. The final determination of the subtendons was made by consensus.
2.4. Ethics
Swedish Institutional Review Board approved the current study. The Bioethical Committee at the Medical University of Warsaw gave ethical approval (AKBE/258/2020) for the current retrospective study and waived the need for informed consent. The study was conducted following the Declaration of Helsinki.
3. Results
Connections of the FR with other structures are common and have been found in most cases. In 97% of cases, the FR is connected with the DL (Table 1, Figure 1 and Figure 2), most often with the anterior tibiotalar part (ATTP) (93.2%) (Table 1 and Figure 2). The FR frequently merges in a smooth transition with the FTCL (84.1%) (Figure 3) and the FFS (83.3%) (Figure 4). Inferiorly, the FR joins the AbH (72.7%) (Figure 5); anteriorly, the FR merges with the IER (64.4%) (Figure 3). A direct projection to the paratenon was found in 62.1% of cases (Figure 6); additionally, accessory projection from the FTCL was seen in 39 cases (29.5%). An interconnection between the FR and the SL was noticed in 31.1% of cases (Figure 7) and was directly related to the posterior tibial tendon attachment.

Table 1.
Number of connections of FR with other structures included in the study. p values for the differences in the number of connections in the groups of patients with plantaris tendon type 4 and with accessory navicular bone.
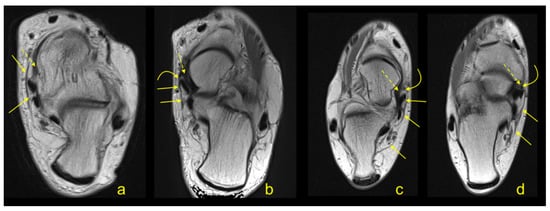
Figure 1.
(a,b)—a 55-year-old patient with clinical suspicion of tenosynovitis. (c,d)—an 18-year-old patient with clinical suspicion of Achilles tendinopathy. (a–d)—proton density (PD) weighted images. Flexor retinaculum (FR) (straight arrow) sends band (curved arrow) to joint with the tibionavicular part (TNP) (dashed arrow).
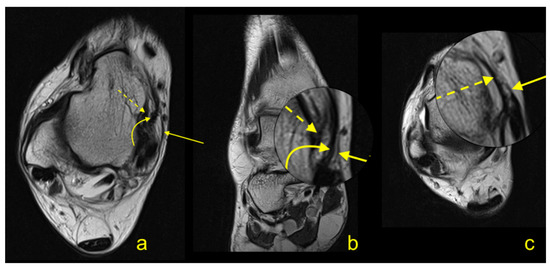
Figure 2.
A 43-year-old patient with clinical suspicion of a ganglion. (a–c)—PD weighted images.
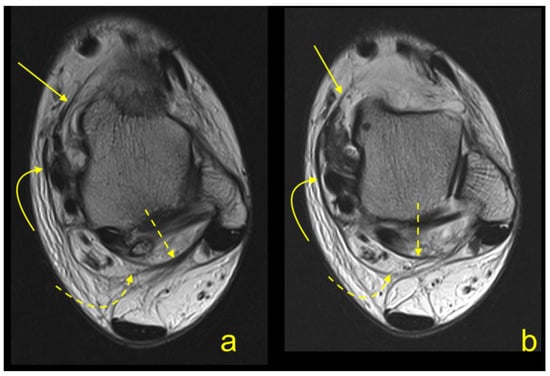
Figure 3.
(a,b)—a 39-year-old patient with clinical suspicion of posterior impingement. (a,b)—PD weighted images. FR (curved arrow) communicates with the inferior extensor retinaculum (IER) (straight arrow). Posterior FR gives projection (curved dashed arrow) to fibulotalocalcaneal ligament (FTCL) (dashed arrow).
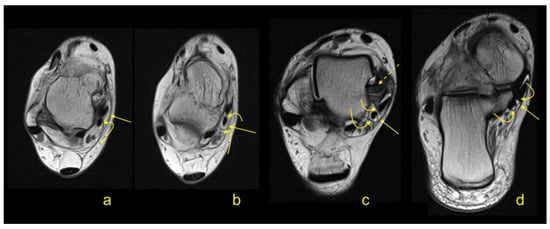
Figure 4.
(a,b)—a 23-year-old patient with clinical suspicion of anterior impingement. (c,d)—a 39-year-old patient with clinical suspicion of rheumatoid arthritis. (a–d)—PD weighted images. FR (straight arrow) communicates with the fibrous sheath of flexors (FFS) (curved arrow) and with the anterior tibiotalar part (ATTP) (dashed arrow).
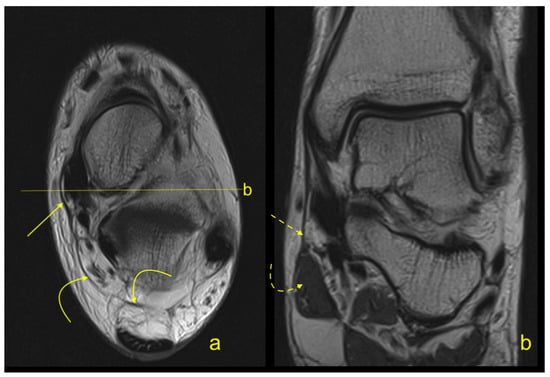
Figure 5.
A 32-year-old patient with clinical suspicion of a lipomatous tumor in the lateral side of the ankle. (a,b)—PD weighted sequences. FR (straight arrow) communicates with the FTCL (curved arrow) in the Kager’s fat pad. The projection (dashed arrow) from FR to abductor hallucis (AbH) (curved arrow) can be identified inferior from the medial malleolus.
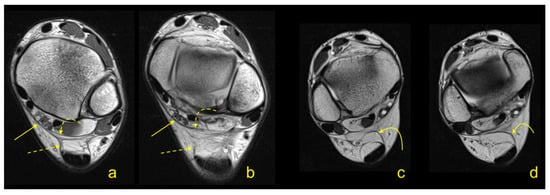
Figure 6.
(a,b)—a 38-year-old patient with clinical suspicion of chondropathy. (c,d)—a 31-year-old patient with clinical suspicion of a ganglion. (a–d)—PD weighted images. FR (straight arrow) communicates with FTCL (curved dashed arrow). Communication between FR and the paratenon (dashed arrow) is visible on (a,b), but on (c,d), the paratenon receives projection only from FTCL (curved arrow).
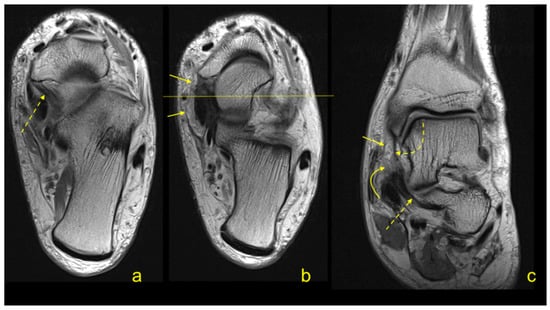
Figure 7.
(a–c)—a 51-year-old patient after kidney transplantation with clinical suspicion of avascular necrosis of the talus. (a,b)—PD weighted images. FR (straight arrow) gives projection (curved arrow) to communicate with SL (dashed arrow). Deeply to FR (straight arrow), TNP (curved dashed arrow) is present.
The plantaris tendon merged with the deep crural fascia in 7.6% of cases (Figure 8), giving projections to the FR, the FTCL, and the paratenon. Statistically significant differences were noticed in connections of the FR to the paratenon, the SL, the IER, the AbH, and the FFS (p < 0.05) (Table 1).
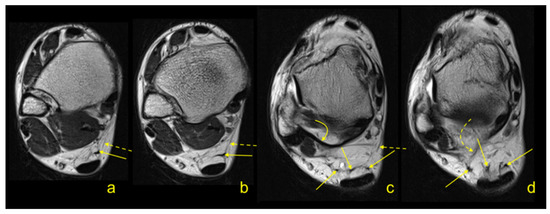
Figure 8.
(a,b)—a 20-year-old patient with clinical suspicion of tenosynovitis. (c,d)—a 19-year-old patient with clinical suspicion of Achilles tendinopathy. (a–d)—PD weighted images. The plantaris tendon branches (straight arrow) anteriorly to the Achilles tendon. Communication between the plantaris tendon and the FR can be seen (dashed arrow). A thick FTCL (curved arrow) with communication with one of the terminal branches (curved dashed arrow) from the plantaris tendon can be noticed.
Significant differences in the relationship between the examined side and the presence of connections were visible in the DL, the AbH, and the FFS (p < 0.05) (Table 1).
The interconnections between the FR and the DL were statistically significantly correlated with the connection of the FR to the IER, the paratenon, and the SL (p < 0.05) (Table 2). Connection to the ATTP was associated with a linking band with the FTCL, the FFS, and the AbH (Table 2). A negative correlation between the coexistence of FR–ATTP and FR–SL connections was noticed (Table 2). The connection between the FR and the posterior tibiotalar part (PTTP) was correlated with connections of the FR with the SL, the FFS, or the FTCL (Table 2).

Table 2.
Coexistence of connections between FR and PTTP, TNP, ATTP and its correlation with the interconnection between FR with SL, AbH, FFS, FTCL, IER, and paratenon.
An accessory navicular bone was found in 10.6% of cases; however, no statistically significant differences (p > 0.05) were noticed in the presence of the connections between groups of patients with and without the accessory navicular bone (Table 1).
Perfect or almost perfect agreement between reviewers was noted for connections of the FR with the IER, the paratenon, the FTCL, the AbH, and the FFS, while moderate agreement was noted for FR connections to the SL, and substantial agreement was seen for FR connections to the DL (Table 1).
4. Discussion
The first contribution of the present study is that we proved the presence of connections between the FR and the DL, the SL, the FFS, the paratenon of the Achilles tendon, the AbH, and the IER in routine MRI ankle examinations. PD and T2-weighted images without fat tissue saturation make it possible to correctly distinguish even narrow bands of collagen-like retinaculum from adjacent adipose tissue [12,13,14]. The FR is a crural fascia-strengthening structure, having bone attachment onto the medial malleolus, together with the DL. It is a thin structure composed of layers; the most inner one is a smooth layer to enable gliding, the thick mid layer is supporting, and the outer layer of loose connective tissue covers the other two layers [6]. The FR is a broad, narrow collagen structure that reinforces the fascia posteriorly and inferiorly from the medial malleolus. It transforms the groove present on the medial malleolus into a fibrous-bone canal called the tarsal tunnel, whose function is to pass the posterior tibial tendon, the flexor digitorum longus, the posterior tibial vessels, and the tibial nerve in three separate compartments.
The FR contributes distally to the tibialis posterior tendon sheath and blends with the superficial part of the DL. In its inferior extension, the FR splits to enclose the AbH and then reunites and blends with the plantar fascia [3,6]. Literature regarding the FR is very limited, and only connections to the superficial part of the DL and the AbH were mentioned in previous studies. We revealed that the FR connects with many more medial malleolus structures.
The FR is a thicker part of the crural fascia, which spans different compartments, creating space that envelopes different groups of muscles and tendons [15]. The arrangement of the crural fascia fibers is multidirectional, reflecting the various loads applied. Likewise, in our study, the FR shows connections with different structures located anteriorly, posteriorly, inferiorly, and medially to the medial malleolus, reinforcing the medial part of the ankle. As the crural fascia integrates structures located in different compartments, the FR integrates the medial ankle ligaments and the non-ligamentous structures, utilizing connections revealed in our study [15,16].
The biomechanical unity of the fascia and the muscles is expressed by a similarity in the structure of the muscle aponeurosis and deep fascia [3,6]. The connection between muscle and fascia can be expressed as communicating the fascial element with the tendon’s compartment. However, far from a complete definition, the myofascial diseases assume that connections between the fascia and the muscle exist [15]. In our study, we demonstrated a connection between FR and FFS, paratenon, and AbH [3,6]. The FR unites with the paratenon of the Achilles tendon in two ways. The first one is direct, and the second is indirect by branching from the FTCL. This type of connection is an example of a fascia–muscle connection, possibly for proprioception [1,16]. The role of the FTCL is to integrate the ligaments and the fibrous bands in Kager’s fat pad [10]; therefore, FTCL has a similar role to the FR in the medial ankle region. Both FR and FTCL are parts of the crural fascia.
About 4% of the plantaris tendon connects with the deep crural fascia [17,18], being an example of a fascial–tendon connection. In our study, the plantaris tendon frequency was nearly twice as high as reported previously [17,19], which may be due to population variability. As in type 4, according to Olewnik et al. [17], the tendon branched in the fat tissue of the Kager’s triangle [18], connecting with the fascial elements, as previously described [10]. Some very narrow terminal projections of the plantaris tendon joined the anterior outline of the paratenon or the FTCL.
It is a known phenomenon that lateral ankle structures communicate [9]. The interconnections between ligaments of Kager’s fat pads and surrounding structures are also described in the posterior region [10]. We could not find any research regarding connections between the FR and other ligamentous and non-ligamentous structures in the medial ankle area. Given the presence of connections in the lateral malleolus area and Kager’s fat pad, there is no reason to assume that similar interconnections are not present on the medial side of the ankle joint. This study aimed to prove this hypothesis based on the clinical observation that a DL tear may be combined with the SL and a posterior tibial tendon injury [20]. Naturally, a similar injury mechanism may be the underlying cause; however, considering previous studies, the presence of connections may also contribute to more concomitant injury [9,10]. A tear or dysfunction of one structure may influence the other structures, leading to medial or multidirectional ankle instability [13,20,21]. One of the essential functions of the medial ankle structure is to restrain against valgus sloping and anterior and lateral translation of the talus [13]. Joining smaller ligament structures into larger anatomical-functional units provides better stability of the ankle joint by causing greater diversification of the direction of the collagen fibers.
The DL is a broad and robust ligament that connects the medial malleolus with the navicular bone, the talus, and the calcaneus [13]. The superficial part of the DL blends with the FR at the common attachment medial malleolus [3,6,22]. The presence of the DL’s anatomical and functional components results in the striated MRI appearance of the DL, which should not be confused with a tear [12]. Anatomical literature distinguishes the superficial and the deep layers of the DL [12], separated by a narrow band of fatty tissue [13], which is an anatomical background of the MRI image of the DL. Individual parts comprising the DL layers are anatomically continuous, indicating a tendency to merge into larger anatomical and functional structures. Disruption of the DL occurs in supination external rotation and pronation external rotation [21], which is a similar pattern to FR injury [2]. There are no reliable epidemiological data on the frequency of injury to the medial ankle structures. About one-third of acute superficial DL injuries are concomitant with an FR tear [23]. The tear may progress deeply to the fibro-osseous tunnel causing injury to the FFS [2], the connection between which was shown in our study.
Only case reports regarding SL or FR injury can be found in the literature, because injuries to the medial ankle ligaments are less common than to the lateral ligaments [24,25,26,27]. SL tears are often associated with tibialis posterior tendon injuries [28], which may confirm the connections between them. Injuries to the medial structures of the ankle joint more often occur due to high energy traumas. This is probably because the medial ligaments are more robust and more resistant to minor injuries than the lateral ankle ligaments [29].
The presence of connections is also relevant in non-traumatic cases. Valgus hindfoot causes overloading of the posterior tibial tendon and the medial structures [30], causing dysfunction and aggravation of deformation, resulting in a flat foot [31,32]. Malfunction of one structure causes the worse function of the other, resembling a domino effect. It can also be partly explained by the presence of the connections shown by us. Since the ankle joint is a functional unit, changes in the hindfoot are also manifested on the joint’s lateral side, e.g., by the more horizontally running calcaneofibular ligament. This could be a reliable MRI symptom of the presence of hindfoot [33].
The accessory navicular bone prevalence is estimated to be between 4 to 25% [34,35]. The incidence of the accessory navicular bone in the current study fits into the mentioned range. An overrepresentation of accessory navicular bone in patients with tibialis posterior tendon insufficiency can be noticed [34]. We observed no statistically significant differences regarding connections in patients with and without the accessory navicular bone, indicating a separate developmental origin [36].
The tendency to conglomerate smaller structures into larger ones can also be seen in the example of the DL or the SL, where smaller parts unite to form a more significant functional complex [14]. Usually, the SL comprises the superomedial band, the medioplantar oblique band, and the infero-plantar longitudinal band, running in different directions. With the posterior tibial tendon and the long plantar ligament, the SL stabilizes the longitudinal arch of the foot [14]. The connection between the superomedial band and the tendinous sheath of the PTTP has been described previously. Chronic degeneration with tibialis posterior tendon insufficiency is the usual background to an SL tear [32]. Besides the common injury mechanism, the presence of connections demonstrated in our study may explain the described clinical relationship. More acute SL tears may be caused by trauma, with dislocation in the talonavicular joint, inferior migration of the talar head, and a posterior tibial injury [37].
Disorders of the posterior tibial tendon usually result from tendon degeneration and begin around the age of 40. Functional disorders of the posterior tibial tendon are caused by chronic overload of the ligament’s insufficiency. Traumatic dislocation of the posterior tibial tendon is rare and occurs mainly as a consequence of hyperinvertion and either dorsiflextion or plantarflextion, accompanied by a contraction of the posterior tibial tendon [2]. The surgical findings showed diverse injuries of the FR [2]. The end-stage of FR insufficiency or FR injury is the dislocation of the posterior tibialis tendon, which is uncommon but is the second most common ankle tendon dislocation [38]. Dislocation of the posterior tibial tendon due to a tear to the FR may require reinsertion on the medial malleolus [20,39].
The FR connections described in our study integrate individual ligamentous and extra-ligamentous structures to larger anatomical and functional units. The presence of one connection is statistically significantly correlated with the presence of others. The presence of larger anatomical-functional units helps to stabilize the medial side of the ankle joint because the fibers of that structure run in different directions; however, the full significance of the presence of connections remains unknown. A similar pattern of connections occurs in other areas, such as the rotator cuff or the glenohumeral ligament reinforcements of the shoulder joint capsule, providing better joint stability. Furthermore, the importance of proprioception and stabilization in this mechanism is also possible [1,5].
We acknowledge several limitations in the present study. We used routine ankle MRI performed as part of clinical routines. We believe that a full assessment of fibrotic interconnections using thinner slices or 3D sequences would be more accurate. The retrospective character and lack of surgical correlation may also be a limitation of this study.
5. Conclusions
The interconnections between the FR and surrounding ligamentous and non-ligamentous structures can be revealed on routine MRI. The connections shown in our study provide an anatomical basis for the observation that injuries to the medial part of the ankle joint have concomitant character.
Author Contributions
Conceptualization, P.S.; Data curation, P.S. and K.G.G.; Formal analysis, M.P.; Investigation, P.S.; Methodology, K.G.G. and B.C.; Project administration, P.S.; Supervision, B.C.; Visualization, P.S.; Writing—original draft, P.S. and M.P.; Writing—review & editing, K.G.G., M.P. and B.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Stecco, C.; Macchi, V.; Porzionato, A.; Morra, A.; Parenti, A.; Stecco, A.; Delmas, V.; De Caro, R. The Ankle Retinacula: Morphological Evidence of the Proprioceptive Role of the Fascial System. Cells Tissues Organs 2010, 192, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Goucher, N.R.; Coughlin, M.J.; Kristensen, R.M. Dislocation of the posterior tibial tendon: A literature review and presentation of two cases. Iowa Orthop. J. 2006, 26, 122–126. [Google Scholar] [PubMed]
- Gluck, G.S.; Heckman, D.S.; Parekh, S.G. Tendon Disorders of the Foot and Ankle, Part 3: The posterior tibial tendon. Am. J. Sports Med. 2010, 38, 2133–2144. [Google Scholar] [CrossRef] [PubMed]
- Szaro, P.; Ramirez, W.C.; Borkmann, S.; Bengtsson, A.; Polaczek, M.; Ciszek, B. Distribution of the subtendons in the midportion of the Achilles tendon revealed in vivo on MRI. Sci. Rep. 2020, 10, 16348. [Google Scholar] [CrossRef] [PubMed]
- Stecco, C.; Porzionato, A.; Lancerotto, L.; Stecco, A.; Macchi, V.; Day, J.A.; De Caro, R. Histological study of the deep fasciae of the limbs. J. Bodyw. Mov. Ther. 2008, 12, 225–230. [Google Scholar] [CrossRef]
- Numkarunarunrote, N.; Malik, A.; Aguiar, R.O.; Trudell, D.J.; Resnick, D. Retinacula of the Foot and Ankle: MRI with Anatomic Correlation in Cadavers. Am. J. Roentgenol. 2007, 188, W348–W354. [Google Scholar] [CrossRef]
- Erickson, S.J.; Quinn, S.F.; Kneeland, J.B.; Smith, J.W.; E Johnson, J.; Carrera, G.F.; Shereff, M.J.; Hyde, J.S.; Jesmanowicz, A. MR imaging of the tarsal tunnel and related spaces: Normal and abnormal findings with anatomic correlation. AJR Am. J. Roentgenol. 1990, 155, 323–328. [Google Scholar] [CrossRef]
- Balen, P.F.; Helms, C.A. Association of Posterior Tibial Tendon Injury with Spring Ligament Injury, Sinus Tarsi Abnormality, and Plantar Fasciitis on MR Imaging. Am. J. Roentgenol. 2001, 176, 1137–1143. [Google Scholar] [CrossRef]
- Vega, J.; Malagelada, F.; Céspedes, M.-C.M.; Dalmau-Pastor, M. The lateral fibulotalocalcaneal ligament complex: An ankle stabilizing isometric structure. Knee Surgery, Sports Traumatol. Arthrosc. 2020, 28, 8–17. [Google Scholar] [CrossRef]
- Szaro, P.; Polaczek, M.; Ciszek, B. The Kager’s fat pad radiological anatomy revised. Surg. Radiol. Anat. 2020, 1–8. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef]
- Muhle, C.; Frank, L.R.; Rand, T.; Yeh, L.; Wong, E.C.; Skaf, A.; Dantas, R.W.M.; Haghighi, P.; Trudell, D.; Resnick, N. Collateral Ligaments of the Ankle: High-Resolution MR Imaging with a Local Gradient Coil and Anatomic Correlation in Cadavers. Radiographics 1999, 19, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Savage-Elliott, I.; Murawski, C.D.; Smyth, N.A.; Golanó, P.; Kennedy, J.G. The deltoid ligament: An in-depth review of anatomy, function, and treatment strategies. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1316–1327. [Google Scholar] [CrossRef] [PubMed]
- Omar, H.; Saini, V.; Wadhwa, V.; Liu, G.; Chhabra, A. Spring ligament complex: Illustrated normal anatomy and spectrum of pathologies on 3T MR imaging. Eur. J. Radiol. 2016, 85, 2133–2143. [Google Scholar] [CrossRef] [PubMed]
- Pavan, P.; Pachera, P.; Stecco, C.; Natali, A.N. Biomechanical behavior of human crural fascia in anterior and posterior regions of the lower limb. Med Biol. Eng. Comput. 2015, 53, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Stecco, C.; Pavan, P.G.; Porzionato, A.; Macchi, V.; Lancerotto, L.; Carniel, E.L.; Natali, A.N.; De Caro, R. Mechanics of crural fascia: From anatomy to constitutive modelling. Surg. Radiol. Anat. 2009, 31, 523–529. [Google Scholar] [CrossRef]
- Olewnik, Ł.; Wysiadecki, G.; Polguj, M.; Topol, M. Anatomic study suggests that the morphology of the plantaris tendon may be related to Achilles tendonitis. Surg. Radiol. Anat. 2017, 39, 69–75. [Google Scholar] [CrossRef]
- Kurtys, K.; Gonera, B.; Olewnik, Ł.; Karauda, P.; Polguj, M. A highly complex variant of the plantaris tendon insertion and its potential clinical relevance. Anat. Sci. Int. 2020, 95, 553–558. [Google Scholar] [CrossRef]
- Cummins, E.J.; Anson, B.J. The structure of the calcaneal tendon (of Achilles) in relation to orthopedic surgery, with additional observations on the plantaris muscle. Surg. Gynecol. Obstet. 1946, 83, 107–116. [Google Scholar]
- Ribbans, W.J.; Garde, A. Tibialis Posterior Tendon and Deltoid and Spring Ligament Injuries in the Elite Athlete. Foot Ankle Clin. 2013, 18, 255–291. [Google Scholar] [CrossRef]
- Schuberth, J.M.; Collman, D.R.; Rush, S.M.; Ford, L.A. Deltoid ligament integrity in lateral malleolar fractures: A comparative analysis of arthroscopic and radiographic assessments. J. Foot Ankle Surg. 2004, 43, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Crim, J. Medial-sided Ankle Pain: Deltoid Ligament and Beyond. Magn. Reson. Imaging Clin. N. Am. 2017, 25, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.D.; Chew, F.S. Ankle medial flexor retinaculum avulsion fracture. Radiol. Case Rep. 2019, 14, 1144–1147. [Google Scholar] [CrossRef] [PubMed]
- A Bridgman, S.; Clement, D.; Downing, A.; Walley, G.; Phair, I.; Maffulli, N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg. Med. J. 2003, 20, 508–510. [Google Scholar] [CrossRef] [PubMed]
- Debieux, P.; Wajnsztejn, A.; Mansur, N.S.B. Epidemiology of injuries due to ankle sprain diagnosed in an orthopedic emergency room. Einstein (São Paulo) 2020, 18, eAO4739. [Google Scholar] [CrossRef] [PubMed]
- Kolt, G.S.; Kirkby, R.J. Epidemiology of injury in elite and subelite female gymnasts: A comparison of retrospective and prospective findings. Br. J. Sports Med. 1999, 33, 312–318. [Google Scholar] [CrossRef]
- Waterman, C.B.R.; Owens, B.D.; Davey, C.S.; Zacchilli, C.M.A.; Belmont, L.C.P.J. The Epidemiology of Ankle Sprains in the United States. J. Bone Jt. Surg. Am. 2010, 92, 2279–2284. [Google Scholar] [CrossRef]
- Masaragian, H.J.; Ricchetti, H.O.; Testa, C. Acute Isolated Rupture of the Spring Ligament. Foot Ankle Int. 2013, 34, 150–154. [Google Scholar] [CrossRef]
- Crema, M.; Krivokapic, B.; Guermazi, A.; Gravilovic, P.; Popovic, N.; D’Hooghe, P.; Roemer, F.W. MRI of ankle sprain: The association between joint effusion and structural injury severity in a large cohort of athletes. Eur. Radiol. 2019, 29, 6336–6344. [Google Scholar] [CrossRef]
- Rios, A.M.; Rosenberg, Z.S.; Bencardino, J.T.; Rodrigo, S.P.; Theran, S.G. Bone Marrow Edema Patterns in the Ankle and Hindfoot: Distinguishing MRI Features. Am. J. Roentgenol. 2011, 197, W720–W729. [Google Scholar] [CrossRef]
- Ellis, S.J.; Williams, B.R.; Wagshul, A.D.; Pavlov, H.; Deland, J.T. Deltoid Ligament Reconstruction with Peroneus Longus Autograft in Flatfoot Deformity. Foot Ankle Int. 2010, 31, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Hintermann, B.; Valderrabano, V.; Boss, A.; Trouillier, H.H.; Dick, W. Medial Ankle Instability: An exploratory, prospective study of fifty-two cases. Am. J. Sports Med. 2004, 32, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Oliveira, I.; Pressney, I.; Welck, M.; Saifuddin, A. The horizontal calcaneofibular ligament: A sign of hindfoot valgus on ankle MRI. Skelet. Radiol. 2019, 49, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Kalbouneh, H.; Alajoulin, O.; AlSalem, M.; Humoud, N.; Shawaqfeh, J.; Alkhoujah, M.; Mahafza, W.S.; Badran, D.H.; Abu-Hassan, H. Incidence and anatomical variations of accessory navicular bone in patients with foot pain: A retrospective radiographic analysis. Clin. Anat. 2017, 30, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Szaro, P.; Polaczek, M.; Świątkowski, J.; Kocoń, H. How to increase the accuracy of the diagnosis of the accessory bone of the foot? Radiol. Med. 2020, 125, 188–196. [Google Scholar] [CrossRef]
- Uchiyama, E.; Kim, J.H.; Hiroshi, A.; Cho, B.H.; Rodríguez-Vázquez, J.F.; Murakami, G. Fetal development of ligaments around the tarsal bones with special reference to contribution of muscles. Clin. Anat. 2014, 27, 389–398. [Google Scholar] [CrossRef]
- Kavanagh, E.C.; Koulouris, G.; Gopez, A.; Zoga, A.; Raikin, S.; Morrison, W.B. MRI of rupture of the spring ligament complex with talo-cuboid impaction. Skelet. Radiol. 2007, 36, 555–558. [Google Scholar] [CrossRef]
- Schweitzer, M.E.; Karasick, D. MR Imaging of Disorders of the Posterior Tibialis Tendon. AJR Am. J. Roentgenol. 2000, 175, 627–635. [Google Scholar] [CrossRef]
- Ouzounian, T.J.; Myerson, M.S. Dislocation of the Posterior Tibial Tendon. Foot Ankle 1992, 13, 215–219. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).