Influence of Lateral Sinus Floor Elevation Procedures on the Pulpal and Periapical Status of Adjacent Vital Teeth
Abstract
Featured Application
Abstract
1. Introduction
2. Methods
- Partial edentulism in the posterior maxilla;
- Prosthetic treatment plan that included the insertion of 1–3 implants in the posterior region of the maxilla, requiring lateral sinus floor elevation;
- Sinus augmentation performed by the lateral window approach;
- One sinus elevation procedure per patient;
- At least one vital tooth showing a normal response to thermal pulp testing and normal periapical tissues adjacent to the edentulous area;
- CBCT performed before and 6 months following LSFE and panoramic X-ray examination performed 6 months after implant placement.
- Active periodontal disease;
- Previous history of sinus pathology;
- Negative response to thermal pulp testing or the presence of periapical pathology in adjacent teeth before LSFE;
- Complete loss of the posterior premolars and molars;
- Root canal-treated teeth adjacent to the edentulous area;
3. Description of the Surgical Procedure
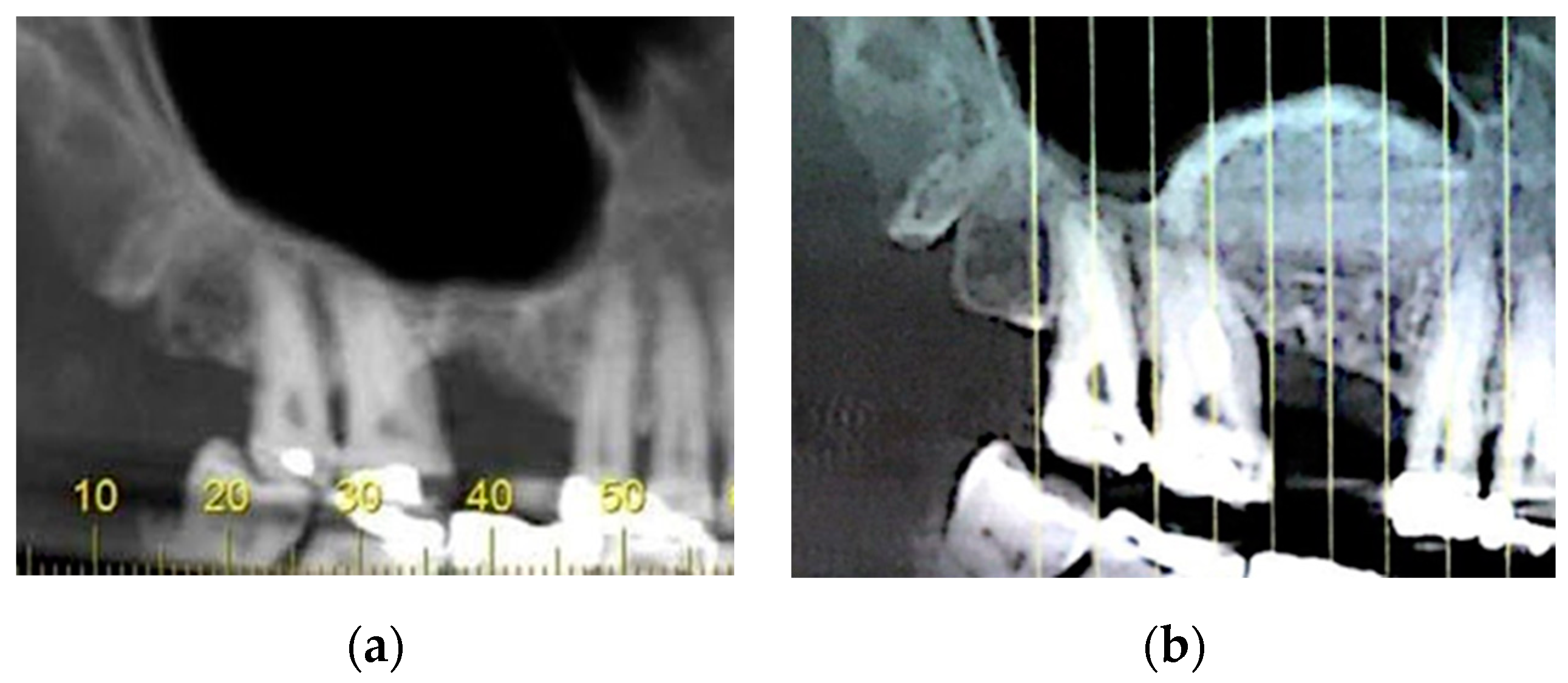
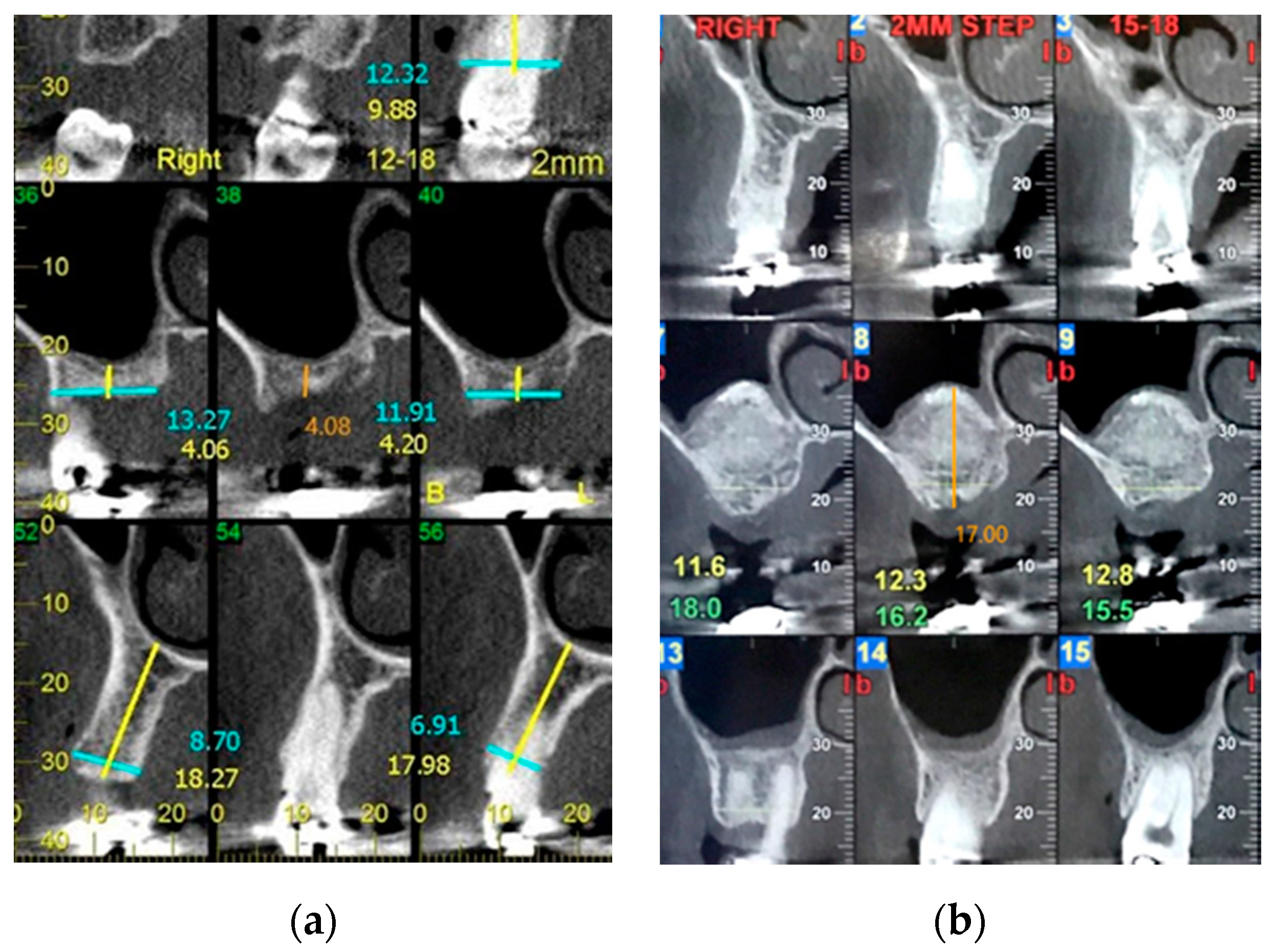
3.1. CBCT Scan Evaluation
3.2. Postoperative Measurements
| 0 | Intact periapical bone structures |
| 1 | Diameter of periapical radiolucency > 0.5–1 mm |
| 2 | Diameter of periapical radiolucency > 1–2 mm |
| 3 | Diameter of periapical radiolucency > 2–4 mm |
| 4 | Diameter of periapical radiolucency > 4–8 mm |
| 5 | Diameter of periapical radiolucency > 8 mm |
| Score (n) + E * | Expansion of periapical cortical bone |
| Score (n) + D * | Destruction of periapical cortical bone |
| * The variables E (expansion of cortical bone) and D (destruction of cortical bone) were added to each score whenever detected in the CBCT analysis. | |
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fugazzotto, P.; Melnick, P.R.; Al-Sabbagh, M. Complications when augmenting the posterior maxilla. Dent. Clin. N. Am. 2015, 59, 97–130. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Rees, J.; Karasoulos, D.; Felice, P.; Alissa, R.; Worthington, H.; Coulthard, P. Effectiveness of sinus lift procedures for dental implant rehabilitation: A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 7–26. [Google Scholar] [PubMed]
- Moreno Vazquez, J.C.; Gonzalez de Rivera, A.S.; Gil, H.S.; Mifsut, R.S. Complication rate in 200 consecutive sinus lift procedures: Guidelines for prevention and treatment. J. Oral Maxillofac. Surg. 2014, 72, 892–901. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, L.; Schiebel, V.; Hof, M.; Ulm, C.; Watzek, G.; Pommer, B. Risk Factors of Membrane Perforation and Postoperative Complications in Sinus Floor Elevation Surgery: Review of 407 Augmentation Procedures. J. Oral Maxillofac. Surg. 2015, 73, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Zijderveld, S.A.; van den Bergh, J.P.; Schulten, E.A.; ten Bruggenkate, C.M. Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J. Oral Maxillofac. Surg. 2008, 66, 1426–1438. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.M.; Park, J.W.; Suh, J.Y.; Sohn, D.S.; Lee, J.M. Bone-added osteotome technique versus lateral approach for sinus floor elevation: A comparative radiographic study. Implant Dent. 2011, 20, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Nolan, P.J.; Freeman, K.; Kraut, R.A. Correlation between Schneiderian membrane perforation and sinus lift graft outcome: A retrospective evaluation of 359 augmented sinus. J. Oral Maxillofac. Surg. 2014, 72, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E.; Papadimitriou, D.E.; Hoyo, M.J.; Caton, J.G. Loss of pulp vitality after maxillary sinus augmentation: A surgical and endodontic approach. J. Periodontol. 2014, 85, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Beck, F.; Lauterbrunner, N.; Lettner, S.; Stavropoulos, A.; Ulm, C.; Bertl, K. Devitalization of adjacent teeth following maxillary sinus floor augmentation: A retrospective radiographic study. Clin. Implant Dent. Relat. Res. 2018, 20, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar] [PubMed]
- Beitlitum, I.; Habashi, W.; Tsesis, I.; Rosen, E.; Nemcovsky, C.E.; Manor, Y. Extended Maxillary Sinus Augmentation to the Apical Area of the Neighboring Teeth: Advantages and Limitations. Int. J. Periodont. Restor. Dent. 2018, 38, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Lee, K.W.; Oh, T.J.; Misch, C.E.; Shotwell, J.; Wang, H.L. Effect of absorbable membranes on sandwich bone augmentation. Clin. Oral Implant. Res. 2008, 19, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.H.; Rios, H.; Al-Hezaimi, K.; Oh, T.J.; Benavides, E.; Wang, H.L. A randomized clinical trial evaluating the efficacy of the sandwich bone augmentation technique in increasing buccal bone thickness during implant placement. II. Tomographic, histologic, immunohistochemical, and RNA analyses. Clin. Oral Implant. Res. 2015, 26, 1150–1157. [Google Scholar] [CrossRef] [PubMed]
- Urban, I.A.; Lozada, J.L. A prospective study of implants placed in augmented sinuses with minimal and moderate residual crestal bone: Results after 1 to 5 years. Int. J. Oral Maxillofac. Implant. 2010, 25, 1203–1212. [Google Scholar]
- Shahbazian, M.; Vandewoude, C.; Wyatt, J.; Jacobs, R. Comparative assessment of periapical radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Odontology 2015, 103, 97–104. [Google Scholar] [CrossRef]
- Shahbazian, M.; Vandewoude, C.; Wyatt, J.; Jacobs, R. Comparative assessment of panoramic radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Clin. Oral Investig. 2014, 18, 293–300. [Google Scholar] [CrossRef]
- Estrela, C.; Bueno, M.R.; Azevedo, B.C.; Azevedo, J.R.; Pecora, J.D. A new periapical index based on cone beam computed tomography. J. Endod. 2008, 34, 1325–1331. [Google Scholar] [CrossRef] [PubMed]
- Solar, P.; Geyerhofer, U.; Traxler, H.; Windisch, A.; Ulm, C.; Watzek, G. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin. Oral Implant. Res. 1999, 10, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Kaur, S. Evaluation of Post-operative Complication Rate of Le Fort I Osteotomy: A Retrospective and Prospective Study. J. Maxillofac. Oral Surg. 2014, 13, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Lang, N.P. Sinus floor elevation utilizing the transalveolar approach. Periodontol. 2000 2014, 66, 59–71. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Type 1 | Type 2 | Type 3 | Type 4 | Total |
|---|---|---|---|---|---|
| PM1 | 1 | 1 | |||
| PM2 | 4 | 2 | 1 | 7 | |
| M1 | 1 | 1 | |||
| M2 | 3 | 6 | 1 | 10 | |
| M3 | 1 | 1 | |||
| Total | 4 | 6 | 9 | 1 | 20 |
| Apex to Sinus Floor Distance | Ridge Height at the Edentulous Area | |||
|---|---|---|---|---|
| Baseline | 6 Months | Baseline | 6 Months | |
| Mean ± SD | 1.05 ± 1.71 | 8.25 ± 3.86 mm | 4.33 ± 2.27 | 17.29 ± 3.02 |
| Range | 0–5.63 | 1.11–18.12 | 0.8–8.81 | 7.82–22.18 |
| Mean difference ± SD | 7.17 ± 3.35 * | 12.95 ± 3.38 * | ||
| N | 20 | 20 | 18 | 18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beitlitum, I.; Slutzkey, G.; Nemcovsky, C.E.; Blazer, T.; Rosen, E.; Tsesis, I. Influence of Lateral Sinus Floor Elevation Procedures on the Pulpal and Periapical Status of Adjacent Vital Teeth. Appl. Sci. 2020, 10, 7185. https://doi.org/10.3390/app10207185
Beitlitum I, Slutzkey G, Nemcovsky CE, Blazer T, Rosen E, Tsesis I. Influence of Lateral Sinus Floor Elevation Procedures on the Pulpal and Periapical Status of Adjacent Vital Teeth. Applied Sciences. 2020; 10(20):7185. https://doi.org/10.3390/app10207185
Chicago/Turabian StyleBeitlitum, Ilan, Gil Slutzkey, Carlos E. Nemcovsky, Tamar Blazer, Eyal Rosen, and Igor Tsesis. 2020. "Influence of Lateral Sinus Floor Elevation Procedures on the Pulpal and Periapical Status of Adjacent Vital Teeth" Applied Sciences 10, no. 20: 7185. https://doi.org/10.3390/app10207185
APA StyleBeitlitum, I., Slutzkey, G., Nemcovsky, C. E., Blazer, T., Rosen, E., & Tsesis, I. (2020). Influence of Lateral Sinus Floor Elevation Procedures on the Pulpal and Periapical Status of Adjacent Vital Teeth. Applied Sciences, 10(20), 7185. https://doi.org/10.3390/app10207185





