Abstract
The predicted mean vote (PMV) is the most widely used model around the world to assess thermal comfort in indoor environments. The year 2020 marks the 50th anniversary of the PMV model and also the year in which the World Health Organization (WHO) declared the COVID-19 outbreak a pandemic. In this context, hospital environments and health professionals are at the center of attention, and a good indoor environment for those professionals to develop their activities is essential. Thus, considering the PMV model and focusing on hospital environments, this study performed a literature review of studies published between 1968 and August 2020. The research identified 153 papers on thermal comfort and its application in hospitals, health centers, and elderly centers. Specific inclusion and exclusion criteria were adopted to determine the most relevant studies for the four research questions proposed in this study. After applying the exclusion criteria, 62 studies were included in order to identify their main characteristics. In the universe of the 62 studies, this review identified 24 studies that applied the PMV model and 12 where there was a comparison of PMV and the thermal sensation votes (TSV) reported by people. The main findings of this research are: (i) A good thermal environment for professionals and patients is important, and more studies are needed; (ii) there are little explored topics, such as productivity related to thermal comfort in hospital environments; (iii) in addition to thermal comfort, other indoor environmental quality (IEQ) parameters have also been evaluated, such as indoor air quality (IAQ); (iv): the COVID-19 pandemic has highlighted how the quality of indoor spaces is important in order to ensure occupant’s health.
1. Introduction
The predicted mean vote (PMV) is an index that shows the average thermal sensation of a large group of people exposed to the same environment [1]. This thermal comfort index was proposed by P.O. Fanger in 1970 and is used to evaluate the thermal sensation in moderate environments [2]. Currently, there is a growing need to evaluate indoor environments, given that in an environment with good thermal comfort, there is a significant improvement in people’s health, wellbeing, and productivity [3,4]. Although thermal comfort is extremely relevant for occupants, buildings must be prepared not only to offer comfort to their users, but also to operate efficiently, since buildings are responsible for approximately one third of the total energy consumption throughout the world [5].
The year 2020 marks the 50th anniversary of the PMV model, which has been applied in different areas in recent decades to assess thermal comfort: the automotive sector [6], naval sector [7], construction [8], schools [9], universities [10], offices [11], and industry [12]. This year is also important in that it is the year in which the World Health Organization (WHO) declared the outbreak of the new coronavirus (SARS-CoV-2), which causes the disease COVID-19, a pandemic [13]. The attention of scientists and researchers from different areas has turned to this theme, putting hospitals and health centers in the spotlight. These facilities have been forced to review their mode of operation to serve a very large number of infected patients in almost all countries around the world.
Although hospital environments are now at the center of attention, the relationship between these environments and studies on thermal comfort is not recent, having started several decades ago, even before Fanger’s studies. One of the first studies that combined thermal comfort and hospital environments is the research performed by Wyon, Lidwell, and Williams [14], carried out in the British Isles. The authors performed measurements of air temperature, relative humidity, air movement, and radiant temperature, as well as applied questionnaires to teams in 30 operating rooms to collect data on their feeling of thermal sensation using the Bedford 7-point scale. The objective was to investigate, by means of sequential multiple regression analysis, the influence of these aspects on comfort. It was observed that all variables collected, with emphasis on air temperature, had some significant effect on the staff.
The first study developed in hospitals that cited Fanger’s research was performed by Smith and Rae [15]. In this study, the authors explain that environmental thermal conditions should maximize the comfort of patients in the “uniforms” that they wear. According to the authors, this relationship could be determined since Fanger established values such as clothes and metabolic activity level for a population, and thus, it is possible to estimate thermal comfort in any situation. However, the authors claimed that due to the peculiarities of the wards’ environment, they chose to conduct the study autonomously to determine the preferred conditions for the hospital tested.
Twenty-three years after the publication of the Fanger’s study and nine years after the publication of the first version of ISO 7730 (1984), Berardi and Leoni [16] conducted a study at the Bologna General Hospital, using the PMV index. It was found that in most of the rooms analyzed, Fanger’s index was not in the range of thermal comfort, especially in the summer. Del Ferraro et al. [17] examined thermal comfort in an Italian hospital considering the differences between gender and age of staff and patients. In order to do this, the authors collected the actual mean vote (AMV) from 30 patients and 19 medical teams for comparison purposes, in order to determine differences between PMV and AMV. Fabbri, Gaspari and Vandi [18], in a recent study performed in a health center in Italy, compared the thermal sensation vote (TSV) in pregnant women with the predicted mean vote (PMV), showing that the PMV underestimates the real thermal sensation.
Not only studies in hospitals have been performed in the past few years. Mui et al. [19], for instance, studied thermal comfort in 19 elderly centers in Hong Kong, with thermal comfort being one of the aspects assessed to determine indoor environmental quality (IEQ) for patients and staff. Tartarini, Cooper, and Fleming [20] explored adaptive behavior to compensate for the lack of thermal comfort in five elderly centers in Australia, as well as to assess the perception and preference of the occupants.
Studies in health centers were also performed over the last few years. Verheyen et al. [21], in Italy, conducted a comparative study between real thermal sensation votes and the sensation calculated by PMV; they concluded that PMV predicted well the real thermal sensation reported by people. Although there is a large number of studies on thermal comfort in the literature, there are only few that focus on the review of thermal comfort literature in hospital environments, which makes it difficult to find studies that directly investigate the effects of thermal comfort on health in this type of environment [22].
Thermal comfort in hospital environments is mandatory, as the nature of patients’ sickness directly changes their thermal sensation, metabolic rate, and regulatory response. A good environment contributes a lot toward patient recovery and wellbeing, the primary focus of any hospital. Additionally, the evaluation of thermal conditions and their requirements plays a critical role in verifying which critical settings may affect medical staff performance. Then, with this motivation, this paper performed a literature review with papers published from 1968 until August 2020, which apply the concepts of thermal comfort in hospitals, health centers, and elderly centers, aiming to answer four research questions (RQs) proposed in this paper, as well as to verify the main characteristics of these studies.
2. Methods
This literature review was performed considering a three-step methodology: the proposition of research questions (RQs) to guide the literature review, a method to search and select the studies, and a tool to perform content analysis. In the following subsections, this three-step methodology is explained in detail.
2.1. Research Questions (RQs)
The main goal of this study was to verify and summarize the studies that apply thermal comfort in hospital environments. In order to achieve this goal, 4 research questions (RQs) are proposed:
- (a)
- According to Djongyang et al. [23] and de Dear et al. [3], thermal comfort is required in indoor environments because it directly affects people’s perception, in terms of health/wellbeing and productivity. On the other hand, Thapa et al. [24] claim that optimizing the energy used in buildings, whether for heating or for cooling, is a reality today, because there is a need for energy saving. Based on these premises, RQ1 is formulated:RQ1: Considering studies on thermal comfort in hospital environments, what are the main aspects that are taken into account: health/wellbeing, productivity or energy saving?
- (b)
- According to Humphreys and Nicol [25], the PMV model does not consider the adaptive actions that people undertake in indoor environments in order to maintain their comfort, leading PMV to underestimate or overestimate the real thermal sensation felt by people in buildings. Based on this premise, RQ2 is formulated:RQ2: Considering studies on thermal comfort in hospital environments, which relate PMV and real thermal sensation, studies indicate that PMV predicted well, underestimates or overestimates the real thermal sensation?
- (c)
- Different levels of activity require specific environmental conditions for people, in order to achieve thermal comfort. Thus, it is important to define the target group of the research [26]. In addition to this factor, the type of environment in which people are inserted in the hospitals usually has its own standardized environmental requirements, determined by the type of activity to be performed [21]. Based on these premises, RQ3 is formulated:RQ3: Considering studies on thermal comfort in hospital environments, what was the most evaluated group and which area within the hospital was most evaluated?
- (d)
- The hospital environment is complex, since it can change from waiting rooms to operating rooms and intensive care units (ICUs), which demand different requirements for environmental parameters due to the type of activity/care. The concern with planning the environment must go far beyond simply offering thermal comfort to its occupants [27]. Thus, the hospital environment should be prepared to offer a good indoor environmental quality (IEQ). Based on these premises, RQ4 is formulated:RQ4: What other parameters of indoor environmental quality (IEQ) were evaluated, in addition to thermal comfort?
2.2. Method for Bibliographic Search
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [28] guidelines were adapted to apply in this study. This method combines keywords and performs research in scientific information databases. Then, through a specific screening, it is possible to reduce the number of studies found, through specific and defined selection criteria for the research. Over the last few years, literature review studies on thermal comfort have been published using this method [29,30]. It has 4 steps to reduce the number of articles that will be selected: identification (step 1), screening (step 2), eligibility (step 3), and inclusion (step 4) for analysis.
As a search strategy and to identify the articles (step 1), it was decided to combine the following keywords, using Boolean operators, in the SCOPUS database (“thermal comfort” OR “thermal conditions” OR “predicted mean vote” OR “predicted percentage of dissatisfied”) AND (“hospital” OR “health centers” OR “elderly centers”). The search occurred in the titles, abstracts, and keywords of the published studies, considering the time period from 1968 until August 2020. The final search was conducted on 25 August 2020. The SCOPUS database was chosen to perform this research to attend to the objective of this review, since the authors understand that all major journals publishing in thermal comfort are indexed there.
After identification, the screening phase started (step 2), where inclusion and exclusion criteria were applied in order to delimit the studies found and align with the RQs. Table 1 shows the inclusion and exclusion criteria that were adopted:

Table 1.
Inclusion and exclusion criteria.
After this screening, the next step consisted of a preliminary analysis of the selected articles with complete and accessible texts. Eligibility (step 3) consisted of reading the abstracts to verify if the selected articles might answer RQ1, RQ2, RQ3, and RQ4, this being a second refinement. After this second refinement, we were able to obtain the portfolio of articles included to perform the review (step 4).
2.3. Tool for Content Analysis
An open code environment developed to carry out thorough bibliometric analyses, Bibliometrix [31] was used. The Bibliometrix package, written in R language, provides a set of tools for scientific research using bibliometrics, and it was used in this study for data content. Also, provides several routines to import bibliographic data from the SCOPUS database, implementing bibliometric analysis and setting up data matrixes for co-citation, coupling, scientific collaboration analysis, and co-word analysis. Based on the selected articles, their main characteristics were analyzed, such as the number of articles per year of publication; most used keywords; most relevant authors; and most relevant sources/journals.
Additionally, Critical Appraisal Skill Programme(CASP) checklists [32,33] were used in order to focus on studies that are relevant to obtain the answers to the proposed research questions. Each one of the articles was verified in order to verify it would be suitable to be included in the final portfolio for performing the review.
3. Results
3.1. Preliminary Results
The results of the search strategy through the combinations of keywords in SCOPUS can be found in Table 2:

Table 2.
Results of search strategy.
Based on the total of 153 articles found, the method described in Section 2.2 was applied. Figure 1 shows the application of the method:
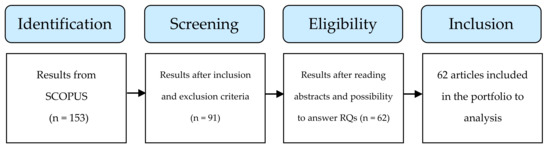
Figure 1.
Obtaining the articles for review.
Thus, there are a total of 62 articles. Two articles are literature reviews on the topic and 60 are research articles. The two literature reviews that were previously published are available in Table 3, being the citations obtained from Google Scholar in August 2020:

Table 3.
Literature reviews.
The first study [22], published in 2012, proposes to fill a gap on thermal comfort, since to date, no literature reviews on thermal comfort in hospitals have been published. With a focus only on hospitals, some health-related buildings fall outside of its scope, such as health centers and elderly centers. At the time, the authors considered the number of original works insufficient to determine the relationship between hospital staff productivity and thermal comfort, and they also considered it important to carry out comparative studies in more than one hospital.
The second and most recent study [34] focuses on the energy-saving aspect and its relationship with comfort in hospitals. The authors aimed to review only technologies to achieve energy efficiency. Research of this nature is important as energy demand for buildings has gained international prominence. The authors found that hospitals alone account for approximately 6% of total energy consumption in the public service sector. This review sought, unlike its predecessors, to evaluate articles related to thermal comfort in all kinds of hospital/healthcare environments, not just hospitals, to perform an updated review on the topic. Therefore, health centers and elderly centers were also included.
The 60 research articles are shown in Table 4, organized in chronological order. The table presents the article’s title and journal, as well as the country where the research was performed. The citations were obtained from Google Scholar:

Table 4.
Research articles.
3.2. General Considerations of Studies
In this section, all 62 articles obtained were considered for analysis. Figure 2 shows the number of publications per year that relate thermal comfort and hospital environments:
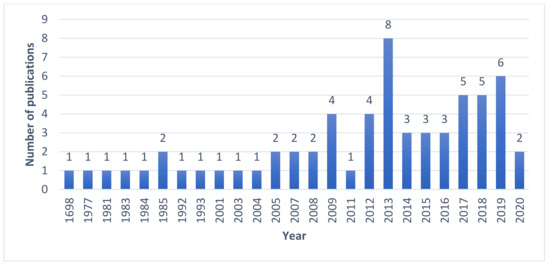
Figure 2.
Number of publications per year.
The publication of the first literature review in 2012 appears to have influenced the production of articles with the theme, with 2013 being the year with a great increase, eight in total. It is noted that in the interstice between 1968 and 2020, there were years when articles with the theme were not published. Figure 3 shows the most used keywords in combination with thermal comfort over the years, with greater emphasis on the size for the words more used:

Figure 3.
Word cloud.
Table 5 shows the most used words in the published papers, with the occurrences of each one:

Table 5.
Most used keywords.
It is visible that the most used keyword, in combination with thermal comfort, is “hospitals”. It can be seen that this information is deducible since most studies are carried out in hospitals. Only four studies differ from this reality, the studies in [19,20] which were carried out in elderly centers, as well as the studies in [21,55] which were carried out in health center facilities.
According to Google Scholar, four articles appear as the most cited: Lomas and Giridharan [53], 124 citations; Hwang et al. [45], 123 citations; Chow and Yang [41], 122 citations and Sodha et al. [38] with 120 citations. Authors with more publications are shown in Figure 4.
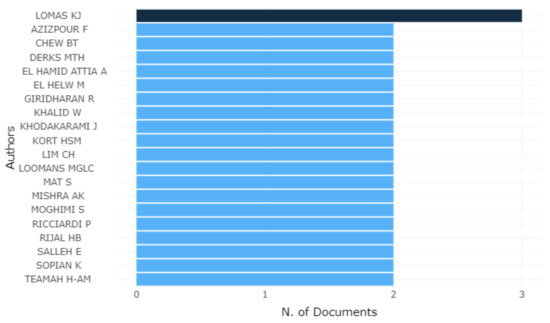
Figure 4.
Authors with more publications.
The author with the greatest number of published papers on the subject is “K.J. Lomas”, with 3 articles. All other authors have 2 publications each. The journals that most published on the topic are shown in Table 6:

Table 6.
Most relevant sources.
Building and Environment is the journal that concentrates the majority of publications in just one source, with 14 publications. The rest of the sources that did not appear in Table 6 have only one published article each and were not presented here to avoid a very large table. For the other sources of publication, please see Table 4.
4. Discussion
4.1. RQ1: Considering Studies in Thermal Comfort in Hospital Environments, What Are the Main Aspects That Are Taken Into Account: Health/Wellbeing, Productivity or Energy Saving?
Table 7 shows, for each study, which main aspect was taken into account by the authors that published the paper:

Table 7.
Division of the main aspects.
Of the 60 research articles, only in [37] was it not possible to determine which aspect the work focuses on, leaving 59 articles. Although the energy-saving aspect is quite relevant and can be considered a research trend in the area, it corresponds to only 17% of the research on the theme that relates thermal comfort and hospital environments. Most works (81%) focus on the health/wellbeing aspect, and this research returned only one work that relates productivity and thermal comfort in hospital environments.
Two possible explanations are raised in order to answer why only one study was performed taking into account the productivity aspect: according to [75,78], temperature control is vital in hospitals, as it can indirectly influence the condition of the patient in addition to contributing to the onset of infections. Thus, research that attempts to ascertain the influence of thermal comfort on employee productivity becomes impracticable as it would be necessary to change these factors. Further, the difficulty in establishing parameters to measure the productivity of a team of doctors or nurses may be another reason.
4.2. RQ2: Considering Studies of Thermal Comfort in Hospital Environments, Which Relate PMV and Real Thermal Sensation, Studies Indicate That PMV Predicted Well, Underestimates or Overestimates the Real Thermal Sensation?
Over the 50 years after the publication of Fanger’s original research, this study found 24 studies that specifically applied PMV in hospital environments: [16,17,18,20,21,45,47,48,50,51,54,56,57,59,61,64,66,67,69,71,75,77,78,84]. Considering these 24 studies, 12 of them compared the real thermal sensation vote (TSV), which is the subjective vote obtained through a specific questionnaire, and the calculated PMV. Table 8 shows the results of these studies that performed a comparison:

Table 8.
Discrepancies between predicted mean vote (PMV) and thermal sensation vote (TSV).
The PMV predicted well the real thermal sensation in [21,69], whereas in the other studies, the PMV was somehow unable to accurately measure the actual mean vote reported by people. Thus, 10 out of the 12 studies concluded that, in some way, PMV was not suitable, either overestimating or underestimating when applied in hospital environments. A possible solution would be the use of adaptive comfort models to assess thermal comfort in hospital environments, in order to obtain better results when comparing real and calculated votes of thermal sensation. However, it is necessary to take into account that the sample is considerably small and more studies are required.
4.3. RQ3: Considering Studies in Thermal Comfort in Hospital Environments, What Was the Most Evaluated Group and Which Area Within Hospital Was Most Evaluated?
In order to answer this question, Table 9 was created. This table contains the specifications of the target group and the site within the hospital environment in which the study was conducted, also presenting the main findings:

Table 9.
Main finding in each group.
Regarding the most explored group in the literature, “staff” and “patients” are tied as the most evaluated, and each one is presented in 30 (71.43%) and 29 (69.05%) articles, respectively out of the 42 studies. Twenty articles bring both together. The “visitants” group is present in eight works. This distribution was already expected, since both staff and patients are the means and the ends of a hospital environment and are the protagonists of the typical activity performed in these environments.
In a more in-depth way, the following distribution for the “staff” group of works that brought some specification in relation to the type of employee includes: the surgical team (8); nurses (5), doctors (2), and nursing assistants (2). For the “patients” group, only two studies specify the type of patient studied. Wheldon and Hull [36] studied full-term babies and premature babies; more recently, Fabbri, Gaspari, and Vandi [18] concentrated efforts to assess the relationship between thermal comfort and pregnant women. This finding shows a gap in thermal comfort studies, since several types of patients and their relationship with the thermal environment have not been explored.
Regarding the site within the hospital environment in which the articles were conducted, most of the articles have specifications. The most explored places in the literature were the wards (17) and the operating rooms (12), corresponding to 40.47% and 28.57%, of the total studies, respectively. The other places, such as the administrative part or waiting rooms, have been little studied, showing that new research can be done in these places.
4.4. RQ4: What Other Parameters of Indoor Environmental Quality (IEQ) Were Evaluated, Aside from Thermal Comfort?
Indoor environmental quality (IEQ) takes into consideration visual comfort (light), sound (noise), thermal comfort (temperature), and indoor air quality (carbon dioxide concentration and volatile organic compounds) [85]. It plays an important role in influencing the comfort and productivity of occupants in buildings, as people remain indoors a significant part of their time [86]. Eleven studies went beyond thermal comfort and analyzed other environmental parameters, as shown in Table 10:

Table 10.
Additional aspects evaluated in parallel to thermal comfort.
In the studies analyzed, it was found that some studies took into account another parameter, in addition to thermal comfort. Azmoon et al. [58] measured the relationship between thermal comfort and light intensity with the quality of sleep and eye strain. Wu et al. [83] studied noise in the environment and how it affects the perception of comfort. Alfa and Öztürk [80] assessed patients’ perceptions of the indoor environment in terms of architectural design, thermal comfort, indoor air quality (IAQ), lighting and acoustic parameters.
However, the parameter that appears most associated with thermal comfort in hospitals is indoor air quality (IAQ). Berardi and Leoni [16], Cheong and Chong [27], Ho, Rosario, and Rahman [48], Lawrence, Jayabal, and Thirumal [76], and Chen, Jiang, and Moser [40] studied IAQ inside hospitals. It is important to note that studies on IAQ are now extremely relevant, due to the pandemic caused by the new coronavirus (COVID-19). Studies on the impacts (IAQ) are necessary given that inadequate ventilation or low air quality in the environment can increase the risk of airborne transmission diseases [87]. According to Correia et al. [88], adequate ventilation reduces the amount of microorganisms suspended in the air, thus reducing the possibility of infection.
The Federation of European Heating, Ventilation, and Air Conditioning Associations (REHVA) [89] updated its guide on the operation and use of services in buildings in areas with a COVID-19 outbreak, in order to prevent the spread of COVID-19, proposing changes in heating, ventilation, and air conditioning systems. The main recommendation is to stop air recirculation and increase intake of external air. The internal environment must be strongly ventilated, exclusively with fresh air, to reduce the concentrations of the virus, in case of eventual contamination by suspended droplets.
According to Zhang [90], in order to reduce the risk of SARS CoV-2 infection, the outdoor ventilation rate must be increased to a level closer to the capacity of the building ventilation system. The required quality level of buildings is increasing, and it is mandatory to acknowledge solutions that facilitate maximized thermal comfort and indoor air quality, while energy consumption is minimized.
5. Final Considerations
It was found in the articles analyzed that there are still some little explored topics, such as productivity in hospital environments. Comfort conditions in specific patients, such as patients with chronic diseases and children, are also little explored. Only two articles were identified, one of which studied pregnant women [18] and another premature babies [36]. Regarding the comfort of specific patients, given the importance of the theme, it is necessary that research of this nature be performed in order to define standards for these types of patients for different types of environments.
The review [22] makes two criticisms addressed here: (a) Studies in the area were conducted in only one hospital and (b) focused on only one group of people. Through the analysis of the current articles, this research adds, relative to criticism (a), that most of the new studies have been carried out in more than one hospital, thus overcoming this judgment; and to criticism (b), that there was no significant improvement since 15 articles focused on more than 1 group while 11 focused on only 1. It should be noted that the universe of thermal comfort in hospital environments is very little explored, especially relative to PMV.
This article proposes four research questions. When answering RQ1, it is shown that around 81% of the published studies deal with the health/wellbeing aspect, 17% deal with energy savings, and around 2% address the productivity aspect. The response from RQ2, on the other hand, shows that the PMV model was not effective when applied in hospital environments since 10 of the 12 articles that relate PMV to TSV pointed out that the Fanger index does not represent the real thermal sensation felt by people in hospital environments. RQ3 shows that the groups “staff” and “patients” are the most studied, as can be expected; however, only the staff group has well-defined specifications, and the medical team is the most approached type. In RQ4, results showed that the IEQ parameter in addition to thermal comfort is IAQ, very important today due the pandemic caused by coronavirus.
Finally, it is important to emphasize the importance of the relationship between buildings and the thermal comfort of the occupants, since discomfort can affect not only patients, but the entire staff. It is believed that this relationship has so far been little explored and that there are still questions to be answered through further studies conducted in these environments.
6. Study Limitations
The search for papers was limited to the combination of keywords. Further limitations lay in bias risk assessment factors, which were not considered in the included articles in the literature review performed in this research.
Author Contributions
Conceptualization, E.E.B.; methodology, E.E.B.; formal analysis, P.F.d.C.P., E.E.B. and A.A.d.P.X.; writing—original draft preparation, P.F.d.C.P., and E.E.B.; writing—review and editing, P.F.d.C.P. and E.E.B; supervision, E.E.B. and A.A.d.P.X.; project administration, E.E.B. and A.A.d.P.X.; funding acquisition, P.F.d.C.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by “Coordenação de Aperfeiçoamento de Pessoal de Nível Superior”, Brasil (CAPES), Finance Code 001.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Peeters, L.; De Dear, R.; Hensen, J.; D’Haeseleer, W. Thermal comfort in residential buildings: Comfort values and scales for building energy simulation. Appl. Energy 2009, 86, 772–780. [Google Scholar] [CrossRef]
- Fanger, P.O. Thermal Comfort. Analysis and Applications in Environmental Engineering; McGraw-Hill: New York, NY, USA, 1970. [Google Scholar]
- De Dear, R.J.; Akimoto, T.; Arens, E.A.; Brager, G.; Candido, C.; Cheong, K.W.D.; Li, B.; Nishihara, N.; Sekhar, S.C.; Tanabe, S.; et al. Progress in thermal comfort research over the last twenty years. Indoor Air 2013, 23, 442–461. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.K.; Ooka, R.; Rijal, H.B.; Takasu, M. Adaptive thermal comfort in the offices of North-East India in autumn season. Build. Environ. 2017, 124, 14–30. [Google Scholar] [CrossRef]
- Märzinger, T.; Österreicher, D. Supporting the Smart Readiness Indicator—A Methodology to Integrate A Quantitative Assessment of the Load Shifting Potential of Smart Buildings. Energies 2019, 12, 1955. [Google Scholar] [CrossRef]
- Alahmer, A.; Mayyas, A.T.; Mayyas, A.A.; Omar, M.; Shan, D. Vehicular thermal comfort models; a comprehensive review. Appl. Therm. Eng. 2011, 31, 995–1002. [Google Scholar] [CrossRef]
- Jang, M.; Koh, C.; Moon, I. Review of thermal comfort design based on PMV/PPD in cabins of Korean maritime patrol vessels. Build. Environ. 2007, 42, 55–61. [Google Scholar] [CrossRef]
- Srinavin, K.; Mohamed, S. Thermal environment and construction workers’ productivity: Some evidence from Thailand. Build. Environ. 2003, 38, 339–345. [Google Scholar] [CrossRef]
- Kwok, A.G.; Chun, C. Thermal comfort in Japanese schools. Sol. Energy 2003, 74, 245–252. [Google Scholar] [CrossRef]
- Jing, S.; Lei, Y.; Wang, H.; Song, C.; Yan, X. Thermal comfort and energy-saving potential in university classrooms during the heating season. Energy Build. 2019, 202, 109390. [Google Scholar] [CrossRef]
- Wu, J.; Li, X.; Lin, Y.; Yan, Y.; Tu, J.; Yang, L. A PMV-based HVAC control strategy for office rooms subjected to solar radiation. Build. Environ. 2020, 177, 106863. [Google Scholar] [CrossRef]
- Pinto, N.D.M.; Xavier, A.A.D.P.; Hatakeyama, K. Thermal Comfort in Industrial Environment: Conditions and Parameters. Procedia Manuf. 2015, 3, 4999–5006. [Google Scholar] [CrossRef]
- World Health Organization. WHO Announces COVID-19 Outbreak a Pandemic n.d. Available online: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus covid19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 15 June 2020).
- Wyon, D.P.; Lidwell, O.M.; Williams, R.E.O. Thermal comfort during surgical operations. J. Hyg. 1968, 66, 229–248. [Google Scholar] [CrossRef]
- Smith, R.M.; Rae, A. Thermal comfort of patients in hospital ward areas. J. Hyg. 1977, 78, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Berardi, B.M.; Leoni, E. Indoor air climate and microbiological airborne: Contamination in various hospital areas. Zentralblatt Hygiene Umweltmedizin 1993, 194, 405–418. [Google Scholar]
- Del Ferraro, S.; Iavicoli, S.; Russo, S.; Molinaro, V. A field study on thermal comfort in an Italian hospital considering differences in gender and age. Appl. Ergon. 2015, 50, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, K.; Gaspari, J.; Vandi, L. Indoor Thermal Comfort of Pregnant Women in Hospital: A Case Study Evidence. Sustainability 2019, 11, 6664. [Google Scholar] [CrossRef]
- Mui, K.W.; Wong, L.T.; Fong, K.N.K.; Wong, W.W.Y. Evaluation of indoor environment quality of elderly centers of Hong Kong. Int. J. Hous. Sci. Appl. 2008, 32, 121–131. [Google Scholar]
- Tartarini, F.; Cooper, P.; Fleming, R. Thermal perceptions, preferences and adaptive behaviours of occupants of nursing homes. Build. Environ. 2018, 132, 57–69. [Google Scholar] [CrossRef]
- Verheyen, J.; Theys, N.; Allonsius, L.; Descamps, F. Thermal comfort of patients: Objective and subjective measurements in patient rooms of a Belgian healthcare facility. Build. Environ. 2011, 46, 1195–1204. [Google Scholar] [CrossRef]
- Khodakarami, J.; Nasrollahi, N. Thermal comfort in hospitals—A literature review. Renew. Sustain. Energy Rev. 2012, 16, 4071–4077. [Google Scholar] [CrossRef]
- Djongyang, N.; Tchinda, R.; Njomo, D. Thermal comfort: A review paper. Renew. Sustain. Energy Rev. 2010, 14, 2626–2640. [Google Scholar] [CrossRef]
- Thapa, S.; Bansal, A.K.; Panda, G.K. Adaptive thermal comfort in the residential buildings of north east India—An effect of difference in elevation. Build. Simul. 2017, 11, 245–267. [Google Scholar] [CrossRef]
- Humphreys, M.A.; Nicol, J.F. The validity of ISO-PMV for predicting comfort votes in every-day thermal environments. Energy Build. 2002, 34, 667–684. [Google Scholar] [CrossRef]
- Khalid, W.; Salim, S.A.Z.S.; Rijal, H.B.; Yakub, F. Investigation of comfort temperature and thermal adaptation for patients and visitors in Malaysian hospitals. Energy Build. 2019, 183, 484–499. [Google Scholar] [CrossRef]
- Cheong, K.; Chong, K.; Cheong, D.K.W. Development and application of an indoor air quality audit to an air-conditioned building in Singapore. Build. Environ. 2001, 36, 181–188. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Broday, E.E.; Xavier, A.A.P. A systematic literature review on thermal response votes (Tsv) and predicted mean vote (pmv). In Occupational Safety and Hygiene VI; Carneiro, P., Cordeiro, P., Costa, N., Arezes, P.M., Baptista, J.S., Perestrelo, G., Melo, R.B., Barroso, M., et al., Eds.; SHO 2018, UTFPR—Federal University of Technology of Paraná; CRC Press/Balkema: Ponta Grossa, Brazil, 2018; pp. 13–17. [Google Scholar]
- Zlatar, T.; Costa, J.T.; Vaz, M.; Baptista, J.S. Influence of severe cold thermal environment on core and skin temperatures: A systematic review. Work 2019, 62, 337–352. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Inf. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Critical Appraisal Skills Programme. CASP (Systematic Review) Checklist. 2018. Available online: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Systematic-Review-Checklist_2018.pdf (accessed on 18 August 2020).
- Critical Appraisal Skills Programme CASP (Qualitative) Checklist. 2018. Available online: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf (accessed on 18 August 2020).
- Gatea, A.A.; Batcha, M.F.M.; Taweekun, J. Energy efficiency and thermal comfort in hospital buildings: A review. Int. J. Integr. Eng. 2020, 12, 33–41. [Google Scholar]
- Matsui, J. A study of thermal comfort conditions of patients—Thermal sensation of patients for thermal environment in hospital wards. J. Showa Med. Assoc. 1981, 41, 271–284. [Google Scholar]
- Wheldon, A.; Hull, D. The thermal environment in the neonatal nursery. Build. Environ. 1983, 18, 163–169. [Google Scholar] [CrossRef]
- Bovenzi, M.; Fiorito, A. Thermal comfort in a hospital. Med. Del. Lav. 1984, 75, 125–132. [Google Scholar]
- Sodha, M.; Sharma, A.; Singh, S.; Bansal, N.; Kumar, A. Evaluation of an earth—Air tunnel system for cooling/heating of a hospital complex. Build. Environ. 1985, 20, 115–122. [Google Scholar] [CrossRef]
- Terzi, R.; Marcaletti, G.; Catenacci, G. [Evaluation of thermal comfort parameters in the operating rooms of a hospital surgical department]. Boll. Della Soc. Ital. Boil. Sper. 1985, 61, 1009–1014. [Google Scholar]
- Chen, Q.; Jiang, Z.; Moser, A. Control of Airborne Particle Concentration and Draught Risk in an Operating Room. Indoor Air 1992, 2, 154–167. [Google Scholar] [CrossRef]
- Chow, T.-T.; Yang, X.-Y. Performance of ventilation system in a non-standard operating room. Build. Environ. 2003, 38, 1401–1411. [Google Scholar] [CrossRef]
- Külpmann, R.; Meierhans, R. New air conditioning concepts for better reduction of air pollution. Anasthesiol. Intensivmed. 2004, 45, 526–528. [Google Scholar]
- Hashiguchi, N.; Hirakawa, M.; Tochihara, Y.; Kaji, Y.; Karaki, C. Thermal Environment and Subjective Responses of Patients and Staff in a Hospital during Winter. J. Physiol. Anthr. Appl. Hum. Sci. 2005, 24, 111–115. [Google Scholar] [CrossRef]
- Skoog, J.; Fransson, N.; Jagemar, L. Thermal environment in Swedish hospitals. Energy Build. 2005, 37, 872–877. [Google Scholar] [CrossRef]
- Hwang, R.-L.; Lin, T.-P.; Cheng, M.-J.; Chien, J.-H. Patient thermal comfort requirement for hospital environments in Taiwan. Build. Environ. 2007, 42, 2980–2987. [Google Scholar] [CrossRef]
- Mazzacane, S.; Giaconia, C.; Costanzo, S.; Cusumano, A. A Survey on the Thermal Conditions Experienced by a Surgical Team. Indoor Built Environ. 2007, 16, 99–109. [Google Scholar] [CrossRef]
- Khodakarami, J.; Knight, I. Required and Current Thermal Conditions for Occupants in Iranian Hospitals. HVAC&R Res. 2008, 14, 175–193. [Google Scholar]
- Ho, S.H.; Rosario, L.; Rahman, M.M. Three-dimensional analysis for hospital operating room thermal comfort and contaminant removal. Appl. Therm. Eng. 2009, 29, 2080–2092. [Google Scholar] [CrossRef]
- Lomas, K.J.; Ji, Y. Resilience of naturally ventilated buildings to climate change: Advanced natural ventilation and hospital wards. Energy Build. 2009, 41, 629–653. [Google Scholar] [CrossRef]
- Masia, M.D.; Dettori, M.; Liperi, G.; Deriu, G.M.; Posadino, S.; Maida, G.; Mura, I. Thermal comfort in perioperatory risk’s evaluation. Ann. Ig. 2009, 21, 251–258. [Google Scholar] [PubMed]
- Thermal comfort study of hospital workers in MalaysiaYau YH, Chew BT. Thermal comfort study of hospital workers in Malaysia. Indoor Air 2009, 19, 500–510. [Google Scholar] [CrossRef]
- Adamu, Z.; Price, A.D.F.; Cook, M. Performance evaluation of natural ventilation strategies for hospital wards—A case study of Great Ormond Street Hospital. Build. Environ. 2012, 56, 211–222. [Google Scholar] [CrossRef]
- Lomas, K.J.; Giridharan, R. Thermal comfort standards, measured internal temperatures and thermal resilience to climate change of free-running buildings: A case-study of hospital wards. Build. Environ. 2012, 55, 57–72. [Google Scholar] [CrossRef]
- Pourshaghaghy, A.; Omidvari, M. Examination of thermal comfort in a hospital using PMV–PPD model. Appl. Ergon. 2012, 43, 1089–1095. [Google Scholar] [CrossRef]
- Ascione, F.; Bianco, N.; De Masi, R.F.; Vanoli, G.P. Rehabilitation of the building envelope of hospitals: Achievable energy savings and microclimatic control on varying the HVAC systems in Mediterranean climates. Energy Build. 2013, 60, 125–138. [Google Scholar] [CrossRef]
- Azizpour, F.; Moghimi, S.; Lim, C.H.; Mat, S.; Salleh, E.; Sopian, K. A Thermal Comfort Investigation of a Facility Department of a Hospital in Hot-Humid Climate: Correlation between Objective and Subjective Measurements. Indoor Built Environ. 2012, 22, 836–845. [Google Scholar] [CrossRef]
- Azizpour, F.; Moghimi, S.; Salleh, E.; Mat, S.; Lim, C.; Sopian, K. Thermal comfort assessment of large-scale hospitals in tropical climates: A case study of University Kebangsaan Malaysia Medical Centre (UKMMC). Energy Build. 2013, 64, 317–322. [Google Scholar] [CrossRef]
- Azmoon, H.; Dehghan, H.; Akbari, J.; Soury, S. The Relationship between Thermal Comfort and Light Intensity with Sleep Quality and Eye Tiredness in Shift Work Nurses. J. Environ. Public Heal. 2013, 2013, 1–5. [Google Scholar] [CrossRef] [PubMed]
- De Giuli, V.; Zecchin, R.; Salmaso, L.; Corain, L.; De Carli, M. Measured and perceived indoor environmental quality: Padua Hospital case study. Build. Environ. 2013, 59, 211–226. [Google Scholar] [CrossRef]
- Giridharan, R.; Lomas, K.J.; Short, C.A.; Fair, A.J. Performance of hospital spaces in summer: A case study of a ’Nucleus’-type hospital in the UK Midlands. Energy Build. 2013, 66, 315–328. [Google Scholar] [CrossRef]
- El Hamid, A.A.; El Helw, M.; Teamah, H.-A.M. Three-dimensional thermal comfort analysis for hospital operating room with the effect of door gradually opened: Part (II) effect on mean age of the air and predicted mean vote distribution. CFD Lett. 2013, 5, 20–31. [Google Scholar]
- El Hamid, A.A.; El Helw, M.; Teamah, H.-A.M. Three-dimensional thermal comfort analysis for hospital operating room with the effect of door gradually opened part (I) effect on velocity and temperature distributions. CFD Lett. 2013, 5, 6–19. [Google Scholar]
- Dovjak, M.; Shukuya, M.; Krainer, A. Individualisation of personal space in hospital environment. Int. J. Exergy 2014, 14, 125–155. [Google Scholar] [CrossRef]
- Van Gaever, R.; Jacobs, V.; Diltoer, M.; Peeters, L.; Vanlanduit, S. Thermal comfort of the surgical staff in the operating room. Build. Environ. 2014, 81, 37–41. [Google Scholar] [CrossRef]
- Yau, Y.H.; Chew, B. Adaptive thermal comfort model for air-conditioned hospitals in Malaysia. Build. Serv. Eng. Res. Technol. 2013, 35, 117–138. [Google Scholar] [CrossRef]
- Rodrigues, N.J.; Oliveira, R.F.; Teixeira, S.; Miguel, A.S.; Teixeira, J.C.; Baptista, J.S. Thermal comfort assessment of a surgical room through computational fluid dynamics using local PMV index. Work 2015, 51, 445–456. [Google Scholar] [CrossRef] [PubMed]
- Uścinowicz, P.; Chludzińska, M.; Bogdan, A. Thermal environment conditions in Polish operating rooms. Build. Environ. 2015, 94, 296–304. [Google Scholar] [CrossRef]
- Cannistraro, G.; Cannistraro, M. Hypothermia Risk, Monitoring and Environment Control in Operating Rooms. Int. J. Heat Technol. 2016, 34, 165–171. [Google Scholar] [CrossRef]
- Carvalhais, C.; Santos, J.; Vieira da Silva, M. Analytical and subjective interpretation of thermal comfort in hospitals: A case study in two sterilization services. J. Toxicol. Environ. Health Part A Curr. Issues 2016, 79, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Jankowski, T.; Młynarczyk, M. An Impact of The Efficient Functioning of the Ventilation and Air-Conditioning System on Thermal Comfort of the Medical Staff in the Operating Room. J. Ecol. Eng. 2016, 17, 114–119. [Google Scholar] [CrossRef]
- Nematchoua, M.K.; Ricciardi, P.; Reiter, S.; Asadi, S.; Demers, C.M. Thermal comfort and comparison of some parameters coming from hospitals and shopping centers under natural ventilation: The case of Madagascar Island. J. Build. Eng. 2017, 13, 196–206. [Google Scholar] [CrossRef]
- Lan, L.; Tushar, W.; Otto, K.; Yuen, C.; Wood, K. Thermal comfort improvement of naturally ventilated patient wards in Singapore. Energy Build. 2017, 154, 499–512. [Google Scholar] [CrossRef]
- Nematchoua, M.K.; Ricciardi, P.; Buratti, C. Statistical analysis of indoor parameters an subjective responses of building occupants in a hot region of Indian ocean; a case of Madagascar island. Appl. Energy 2017, 208, 1562–1575. [Google Scholar] [CrossRef]
- Pirsaheb, M.; Sohrabi, Y.; Yarmohammadi, H. Assessment of Thermal Comfort in Hospital Wards of Kermanshah, Iran, based on the Standards. Indian J. Public Health Res. Dev. 2017, 8, 357. [Google Scholar] [CrossRef]
- Sattayakorn, S.; Ichinose, M.; Sasaki, R. Clarifying thermal comfort of healthcare occupants in tropical region: A case of indoor environment in Thai hospitals. Energy Build. 2017, 149, 45–57. [Google Scholar] [CrossRef]
- Lawrence, I.D.; Jayabal, S.; Thirumal, P. Indoor air quality investigations in hospital patient room. Int. J. Biomed. Eng. Technol. 2018, 27, 124–138. [Google Scholar] [CrossRef]
- Derks, M.; Mishra, A.K.; Loomans, M.; Kort, H. Understanding thermal comfort perception of nurses in a hospital ward work environment. Build. Environ. 2018, 140, 119–127. [Google Scholar] [CrossRef]
- Khalid, W.; Zaki, S.A.; Rijal, H.B.; Yakub, F. Thermal comfort requirements for different occupants in Malaysian hospital in-patient wards. J. Adv. Res. Fluid Mech. Therm. Sci. 2018, 43, 128–140. [Google Scholar]
- Loomans, M.; Mishra, A.K.; Derks, M.; Kraakman, J.; Kort, H. Occupant response to transitions across indoor thermal environments in two different workspaces. Build. Environ. 2018, 144, 402–411. [Google Scholar] [CrossRef]
- Alfa, M.T.; Öztürk, A. Perceived indoor environmental quality of hospital wards and patients’ outcomes: A study of a general hospital, Minna, Nigeria. Appl. Ecol. Environ. Res. 2019, 17, 8235–8259. [Google Scholar] [CrossRef]
- Mora, R.; Meteyer, M. Thermal comfort in health-care settings. ASHRAE J. 2019, 61, 10–19. [Google Scholar]
- Sameh, H.H.; Omar, E.M.; Ezz El-Dein, N.M. Criteria for evaluating the saving and production of energy in hospitals “nursing units”. Int. J. Eng. Res. Technol. 2019, 12, 670–678. [Google Scholar]
- Wu, Y.; Meng, Q.; Li, L.; Mu, J. Interaction between Sound and Thermal Influences on Patient Comfort in the Hospitals of China’s Northern Heating Region. Appl. Sci. 2019, 9, 5551. [Google Scholar] [CrossRef]
- Angelova, R.A.; Velichkova, R. Thermophysiological Comfort of Surgeons and Patient in an Operating Room Based on PMV-PPD and PHS Indexes. Appl. Sci. 2020, 10, 1801. [Google Scholar] [CrossRef]
- Geng, Y.; Ji, W.; Lin, B.; Zhu, Y. The impact of thermal environment on occupant IEQ perception and productivity. Build. Environ. 2017, 121, 158–167. [Google Scholar] [CrossRef]
- Wong, L.; Mui, K.; Tsang, T. An open acceptance model for indoor environmental quality (IEQ). Build. Environ. 2018, 142, 371–378. [Google Scholar] [CrossRef]
- Zakaria Abouleish, M.Y. Indoor Air Quality and Coronavirus Disease (COVID-19) [published online ahead of print, 2020 May 7]. Public Health 2020. [Google Scholar] [CrossRef]
- Correia, G.; Rodrigues, L.; Da Silva, M.G.; Gonçalves, T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med Hypotheses 2020, 141, 109781. [Google Scholar] [CrossRef] [PubMed]
- Adela Cortina. REHVA Covid19 HVAC Guidance. Eur. Univ. Inst. 2012, 2020, 2–5. [Google Scholar]
- Zhang, J. Integrating IAQ control strategies to reduce the risk of asymptomatic SARS CoV-2 infections in classrooms and open plan offices. Sci. Technol. Built Environ. 2020, 2020, 1–6. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).