Choice between Surgery and Conservative Treatment for Patients with Lumbar Spinal Stenosis: Predicting Results through Data Mining Technology
Abstract
1. Introduction
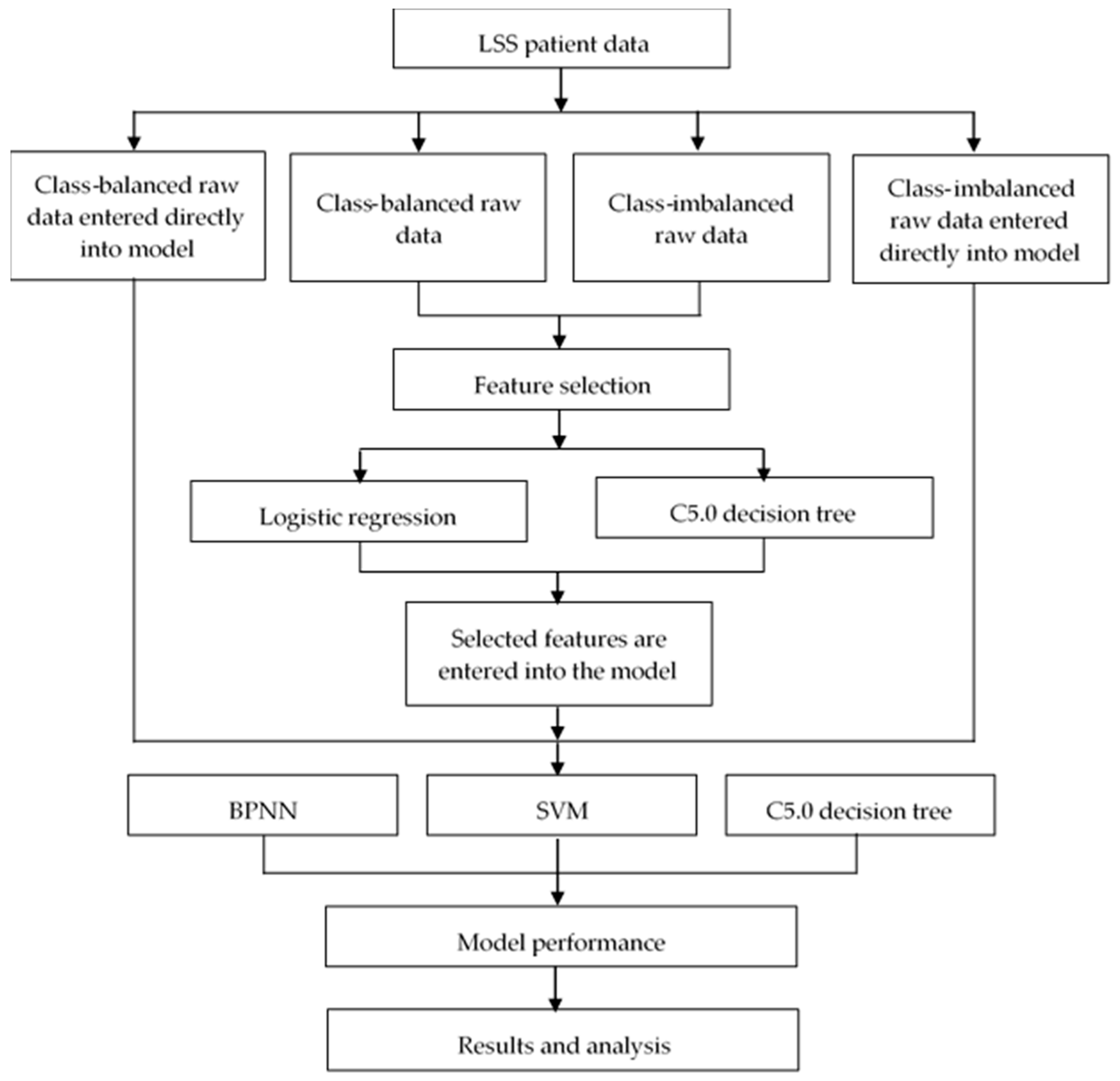
2. Previous Studies on LSS Prediction Models
3. Methods
3.1. Data
3.2. Application of Data Preprocessing Techniques
- , are the minimum and maximum value of A, respectively,
- is the new value of each entry in data,
- is the old value of each entry in data,
- , is the max and min value of the range (i.e., boundary value of range required), respectively.
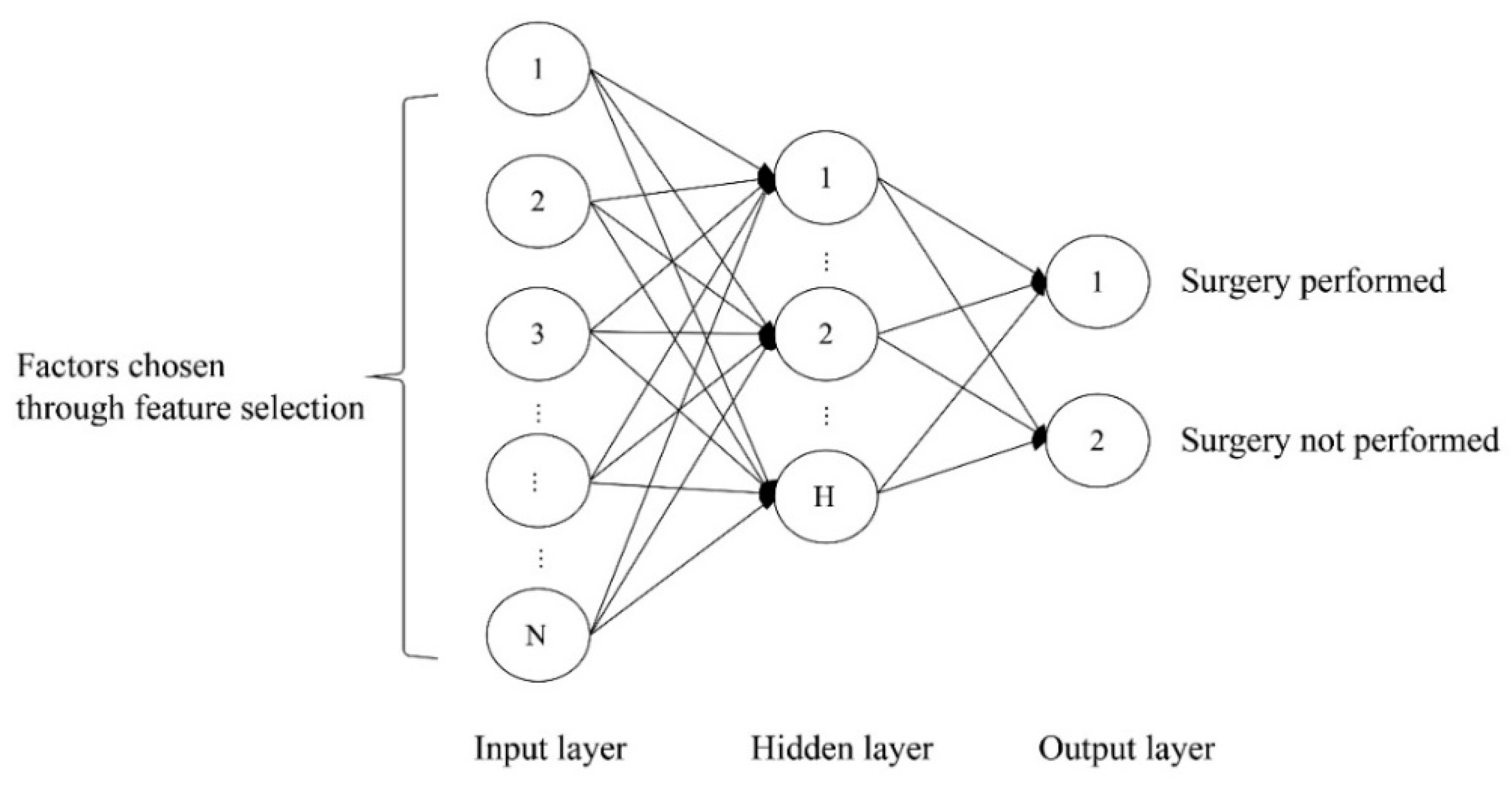
3.3. Supervised Learning Techniques
3.4. Feature Selection
3.5. Experimental Setup and Performance Measure
4. Measurements and Experimental Results
4.1. Feature Selection Results
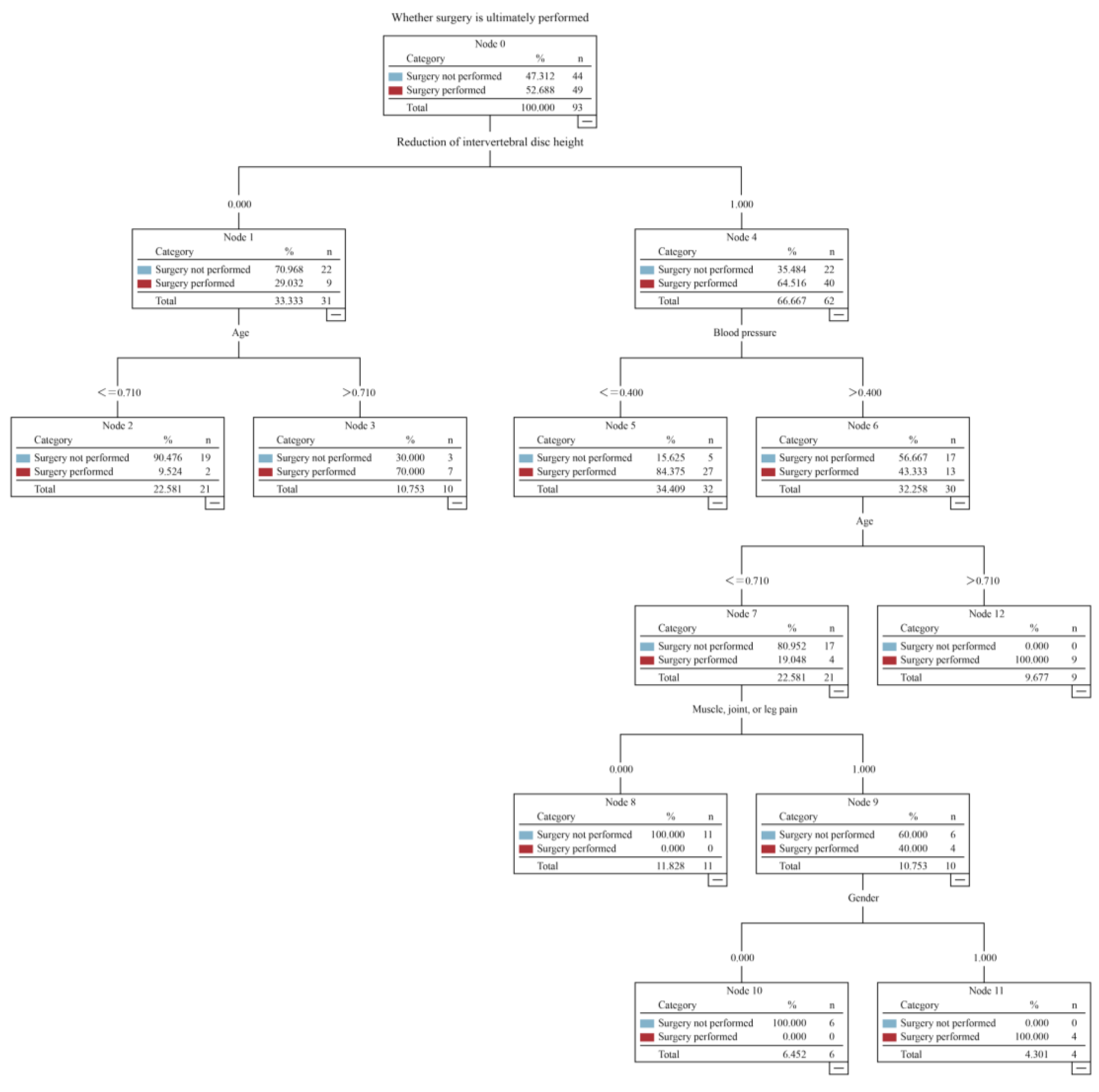
4.2. Evaluation of Model Performance
- ✓
- If no reduction of the intervertebral disc height occurred and the patient was older than 77 years, the patient ultimately underwent the operation.
- ✓
- If a reduction of the intervertebral disc height occurred and the patient’s blood pressure difference was less than 60 mm/Hg, the patient ultimately underwent the operation.
- ✓
- If a reduction of the intervertebral disc height occurred, the patient’s blood pressure difference was greater than 60 mm/Hg, the patient was younger than 77 years, the patient was male, and the patient had leg pain, the patient ultimately underwent the operation.
- ✓
- If a reduction of the intervertebral disc height occurred, the patient’s blood pressure difference was greater than 60 mm/Hg, and the patient was older than 77 years, the patient ultimately underwent the operation.
- ✓
- If no reduction of the intervertebral disc height occurred and the patient was younger than 77 years, the patient ultimately did not undergo the operation.
- ✓
- If a reduction of the intervertebral disc height occurred, the patient’s blood pressure difference was greater than 60 mm/Hg, the patient was younger than 77 years, the patient was female, and the patient had leg pain, the patient ultimately did not undergo the operation.
- ✓
- If a reduction of the intervertebral disc height occurred, the patient’s blood pressure difference was greater than 60 mm/Hg, the patient was younger than 77 years, and patient did not have leg pain, the patient ultimately did not undergo the operation.
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| LSS | lumbar spinal stenosis; |
| LGR | logistic regression; |
| LBP | lower back pain; |
| MRI | magnetic resonance imaging; |
| VAS | visual analog scale; |
| DT | decision tree; |
| CHAID | chi-square automatic interaction detection; |
| BPNN | back-propagation neural network; |
| SVM | support vector machine; |
| CART | classification and regression tree; |
| SMOTE | synthetic minority oversampling technique; |
| AUC | operating characteristic curve. |
References
- Deyo, R.A.; Gray, D.T.; Kreuter, W.; Mirza, S.; Martin, B.I. United States Trends in Lumbar Fusion Surgery for Degenerative Conditions. Spine 2005, 30, 1441–1445. [Google Scholar] [CrossRef] [PubMed]
- Markman, J.D.; Gaud, K.G. Lumbar Spinal Stenosis in Older Adults: Current Understanding and Future Directions. Clin. Geriatr. Med. 2008, 24, 369–388. [Google Scholar] [CrossRef] [PubMed]
- Genevay, S.; Atlas, S.J.; Katz, J.N. Variation in Eligibility Criteria from Studies of Radiculopathy due to a Herniated Disc and of Neurogenic Claudication due to Lumbar Spinal Stenosis. Spine 2010, 35, 803–811. [Google Scholar] [CrossRef]
- Simotas, A.C. Nonoperative Treatment for Lumbar Spinal Stenosis. Clin. Orthop. Relat. Res. 2001, 384, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Gevirtz, C. Update on treatment of lumbar spinal stenosis. Part 1: Defining the problem, diagnosis, and appropriate imaging. Topics Pain Manag. 2010, 25, 1–5. [Google Scholar]
- Verbiest, H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J. Bone Jt. Surg. Br. 1954, 36, 230–237. [Google Scholar] [CrossRef]
- Backstroma, K.M.; Whitman, J.M.; Flynn, T.M. Lumbar spinal stenosis-diagnosis and management of the aging spine. Man. Ther. 2011, 16, 308–317. [Google Scholar] [CrossRef]
- Dejerine, J. Intermittent claudication of the spinal cord. Press Med. 1911, 19, 981–984. (In French) [Google Scholar]
- Malfair, D.; Beall, D.P. Imaging the Degenerative Diseases of the Lumbar Spine. Magn. Reson. Imaging Clin. N. Am. 2007, 15, 221–238. [Google Scholar] [CrossRef]
- Lee, S.; Lee, J.; Yeom, J.S.; Kim, K.-J.; Kim, H.-J.; Chung, S.K.; Kang, H.S. A Practical MRI Grading System for Lumbar Foraminal Stenosis. Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef]
- Siebert, E.; Prüss, H.; Klingebiel, R.; Failli, V.; Einhäupl, K.M.; Schwab, J.M. Lumbar spinal stenosis: Syndrome, diagnostics and treatment. Nat. Rev. Neurol. 2009, 5, 392–403. [Google Scholar] [CrossRef]
- Ng, K.K.M.; Cheung, K.M.-C. Is minimally invasive surgery superior to open surgery for treatment of lumbar spinal stenosis? A systematic review. J. Orthop. Surg. 2017, 25. [Google Scholar] [CrossRef]
- Cho, D.-Y.; Lin, H.-L.; Lee, W.-Y.; Lee, H.-C. Split–spinous process laminotomy and discectomy for degenerative lumbar spinal stenosis: A preliminary report. J. Neurosurg. Spine 2007, 6, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.R.; Hurwitz, E.L.; Gregory, A.; Clary, R. A Nonsurgical Approach to the Management of Patients with Cervical Radiculopathy: A Prospective Observational Cohort Study. J. Manip. Physiol. Ther. 2006, 29, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Vo, A.N.; Kamen, L.B.; Shih, V.C.; Bitar, A.A.; Stitik, T.P.; Kaplan, R.J. Rehabilitation of orthopedic and rheumatologic disorders. 5. Lumbar spinal stenosis. Arch. Phys. Med. Rehabil. 2005, 86, 69–76. [Google Scholar] [CrossRef]
- Fitch, K.; Blumen, H.; Engel, T. Utilization and Cost of Surgery for Lumbar Spinal Stenosis in a Commercially Insured Population; Milliman Client Report; Milliman Inc.: Seattle, WA, USA, 2015; pp. 1–18. [Google Scholar]
- Machado, G.C.; Ferreira, M.L. No clinically important benefits of surgery over rehabilitation for lumbar spinal stenosis (PEDro synthesis). Br. J. Sports Med. 2016, 51, 541–542. [Google Scholar] [CrossRef]
- Amundsen, T.; Weber, H.; Nordal, H.J.; Magnaes, B.; Abdelnoor, M.; Lilleås, F. Lumbar spinal stenosis: Conservative or surgical management? A prospective 10-year study. Spine 2000, 25, 1424–1436. [Google Scholar] [CrossRef]
- Azimi, P.; Benzel, E.C.; Shahzadi, S.; Azhari, S.; Mohammadi, H.R. Use of artificial neural networks to predict surgical satisfaction in patients with lumbar spinal canal stenosis. J. Neurosurg. Spine 2014, 20, 300–305. [Google Scholar] [CrossRef]
- Van Dongen, J.M.; Van Hooff, M.L.; Spruit, M.; De Kleuver, M.; Ostelo, R.W.J.G. Which patient-reported factors predict referral to spinal surgery? A cohort study among 4987 chronic low back pain patients. Eur. Spine J. 2017, 26, 2782–2788. [Google Scholar] [CrossRef]
- Spratt, K.F.; Keller, T.S.; Szpalski, M.; Vandeputte, K.; Gunzburg, R. A predictive model for outcome after conservative decompression surgery for lumbar spinal stenosis. Eur. Spine J. 2004, 13, 14–21. [Google Scholar] [CrossRef]
- Wilkens, P.; Scheel, I.B.; Grundnes, O.; Hellum, C.; Storheim, K. Prognostic factors of prolonged disability in patients with chronic low back pain and lumbar degeneration in primary care: A cohort study. Spine 2013, 38, 65–74. [Google Scholar] [CrossRef]
- Chien, C.F.; Hsu, C.Y. Data Mining & Big Data Analytics; Future Career Publishing Corporation: New Taipei City, Taiwan, 2014. (In Chinese) [Google Scholar]
- Rumelhart, D.E.; McClelland, J.L. Parallel Distributed Processing: Explorations in the Microstructure of Cognition; MIT Press: Cambridge, MA, USA, 1986; Volume 1. [Google Scholar]
- Hsu, C.W.; Chang, C.C.; Lin, C.J. A Practical Guide to Support Vector Classification. 2003. Available online: http://www.csie.ntu.edu.tw/~cjlin/papers/guide/guide.pdf (accessed on 19 December 2012).
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; John Wiley & Sons, Inc.: New York, NY, USA, 2000. [Google Scholar] [CrossRef]
- Fernández, A.; Del Jesus, M.J.; Herrera, F.; Hilario, A.F. On the influence of an adaptive inference system in fuzzy rule based classification systems for imbalanced data-sets. Expert Syst. Appl. 2009, 36, 9805–9812. [Google Scholar] [CrossRef]
- Padmaja, T.M.; Dhulipalla, N.; Bapi, R.S.; Krishna, P.R. Unbalanced data classification using extreme outlier elimination and sampling techniques for fraud detection. In Proceedings of the 15th International Conference on Advanced Computing and Communications (ADCOM 2007), Guwahati, India, 18–21 December 2007; Institute of Electrical and Electronics Engineers (IEEE): Piscataway, NJ, USA, 2007; pp. 511–516. [Google Scholar]
- Lee, C.-I.; Tsai, C.-J.; Wu, T.-Q.; Yang, W.-P. An approach to mining the multi-relational imbalanced database. Expert Syst. Appl. 2008, 34, 3021–3032. [Google Scholar] [CrossRef]
- Akuthota, V.; Lento, P.; Sowa, G. Pathogenesis of lumbar spinal stenosis pain: Why does an asymptomatic stenotic patient flare? Phys. Med. Rehabil. Clin. 2003, 14, 17–28. [Google Scholar] [CrossRef]
- Bressler, H.B.; Keyes, W.J.; Rochon, P.A.; Badley, E. The Prevalence of Low Back Pain in the Elderly. Spine 1999, 24, 1813–1819. [Google Scholar] [CrossRef] [PubMed]
- Berson, A.; Smith, S.; Thearling, K. Building Data Mining Applications for CRM; McGraw-Hill: New York, NY, USA, 2000. [Google Scholar]
- Linoff, G.S.; Berry, M.J. Data Mining Techniques: For Marketing, Sales, and Customer Relationship Management; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Hastie, T.; Friedman, J.; Tibshirani, R. The Elements of Statistical Learning; Springer Series in Statistics; Springer: Berlin, Germany, 2001; Volume 1. [Google Scholar]
| Input Variables | ||
|---|---|---|
| Medical records | ||
| Demographic data | Age | Continuous variable |
| Gender | Male or female | |
| Education | No education, elementary school, junior high school, senior high school, university or higher | |
| Physiological data | Body mass index (BMI) | Continuous variable |
| Diastolic pressure | Continuous variable | |
| Systolic pressure | Continuous variable | |
| Lifestyle | Smoking history | present or absent |
| Drinking history | present or absent | |
| Physical examination | Presence of other medical conditions | present or absent |
| Walking distance on level ground | Requires complete assistance, requires partial assistance, can walk slowly for approximately 50 m, or can walk independently | |
| Leg pain | present or absent | |
| Joint pain | present or absent | |
| Muscle pain | present or absent | |
| Muscle weakness | present or absent | |
| Mild paralysis/numbness | present or absent | |
| Leg numbness | present or absent | |
| MRI diagnosis | ||
| Reduction of intervertebral disc height | present or absent | |
| Intervertebral disc herniation | present or absent | |
| Output variable | ||
| Surgery | Surgery performed or not performed | |
| Technique | Parameter | Value/Range | Configuration |
|---|---|---|---|
| BPNN | Learning rate | 0.1–1 | 0.9 |
| Number of hidden units | 1–2 | 2 | |
| Number of learning sample | 9–18 | 18 | |
| C5.0 | Minimum number of instances per leaf | 10 | |
| SVM | Kernel | RBF kernel | C:10 Gamma:0.1 |
| Feature Selection Method | ||
|---|---|---|
| LGR | C5.0 DT | LGR and C5.0 DT |
| Gender | Gender | Gender |
| Age | Age | Age |
| Education | - | Education |
| Systolic pressure | - | Systolic pressure |
| Diastolic pressure | Diastolic pressure | Diastolic pressure |
| Reduction of intervertebral disc height | Reduction of intervertebral disc height | Reduction of intervertebral disc height |
| Leg pain | Leg pain | Leg pain |
| Joint pain | - | Joint pain |
| Muscle pain | Muscle pain | Muscle pain |
| - | Muscle weakness | Muscle weakness |
| - | Whether patient has other medical history | Whether patient has other medical history |
| Constructed Model | Sensitivity | Specificity | Accuracy rate | AUC |
|---|---|---|---|---|
| LGR+ C5.0 DT for feature selection using a BPNN | 0.9 | 1 | 94.87 | 0.952 |
| BPNN | 0.95 | 0.947 | 94.87 | 0.949 |
| C5.0 DT for feature selection using a BPNN | 0.9 | 0.947 | 92.30 | 0.924 |
| LGR + C5.0 DT for feature selection using a SVM | 0.9 | 0.947 | 92.30 | 0.924 |
| LGR + C5.0 DT for feature selection using a C5.0 DT | 0.9 | 0.94 | 92.3 | 0.924 |
| LGR for feature selection using a BPNN | 0.8 | 1 | 89.74 | 0.913 |
| SVM | 0.8 | 1 | 89.74 | 0.913 |
| C5.0 DT | 1 | 0.8 | 89.74 | 0.910 |
| C5.0 DT for feature selection using a SVM | 0.8 | 0.947 | 87.17 | 0.880 |
| LGR for feature selection using a SVM | 0.8 | 0.947 | 87.17 | 0.880 |
| C5.0 DT for feature selection using a C5.0 DT | 0.9 | 0.83 | 87.17 | 0.873 |
| LGR for feature selection using a C5.0 DT | 0.8 | 0.88 | 84.6 | 0.840 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tseng, L.-P.; Pei, Y.-C.; Chen, Y.-S.; Hou, T.-H.; Ou, Y.-K. Choice between Surgery and Conservative Treatment for Patients with Lumbar Spinal Stenosis: Predicting Results through Data Mining Technology. Appl. Sci. 2020, 10, 6406. https://doi.org/10.3390/app10186406
Tseng L-P, Pei Y-C, Chen Y-S, Hou T-H, Ou Y-K. Choice between Surgery and Conservative Treatment for Patients with Lumbar Spinal Stenosis: Predicting Results through Data Mining Technology. Applied Sciences. 2020; 10(18):6406. https://doi.org/10.3390/app10186406
Chicago/Turabian StyleTseng, Li-Ping, Yu-Cheng Pei, Yen-Sheng Chen, Tung-Hsu Hou, and Yang-Kun Ou. 2020. "Choice between Surgery and Conservative Treatment for Patients with Lumbar Spinal Stenosis: Predicting Results through Data Mining Technology" Applied Sciences 10, no. 18: 6406. https://doi.org/10.3390/app10186406
APA StyleTseng, L.-P., Pei, Y.-C., Chen, Y.-S., Hou, T.-H., & Ou, Y.-K. (2020). Choice between Surgery and Conservative Treatment for Patients with Lumbar Spinal Stenosis: Predicting Results through Data Mining Technology. Applied Sciences, 10(18), 6406. https://doi.org/10.3390/app10186406





