PMMA Intraocular Lenses Changes after Treatment with Nd:Yag Laser: A Scanning Electron Microscopy and X-ray Spectrometry Study
Abstract
Featured Application
Abstract
1. Introduction
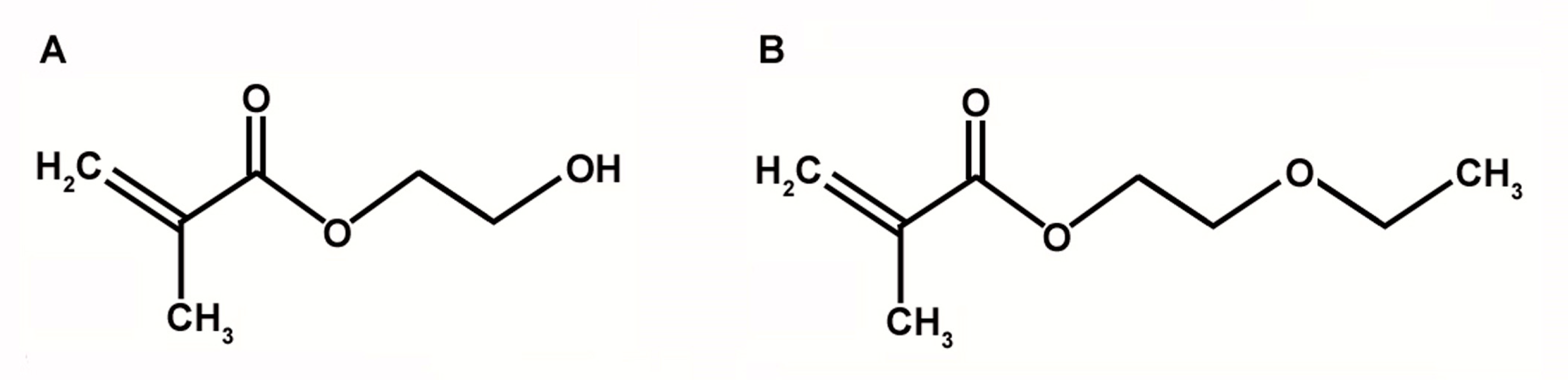
2. Materials and Methods
2.1. IOLs Characteristics and Treatment
2.2. Scanning Electron Microscopy
2.3. SEM and EDX Analyses
2.4. Statistical Analysis
3. Results
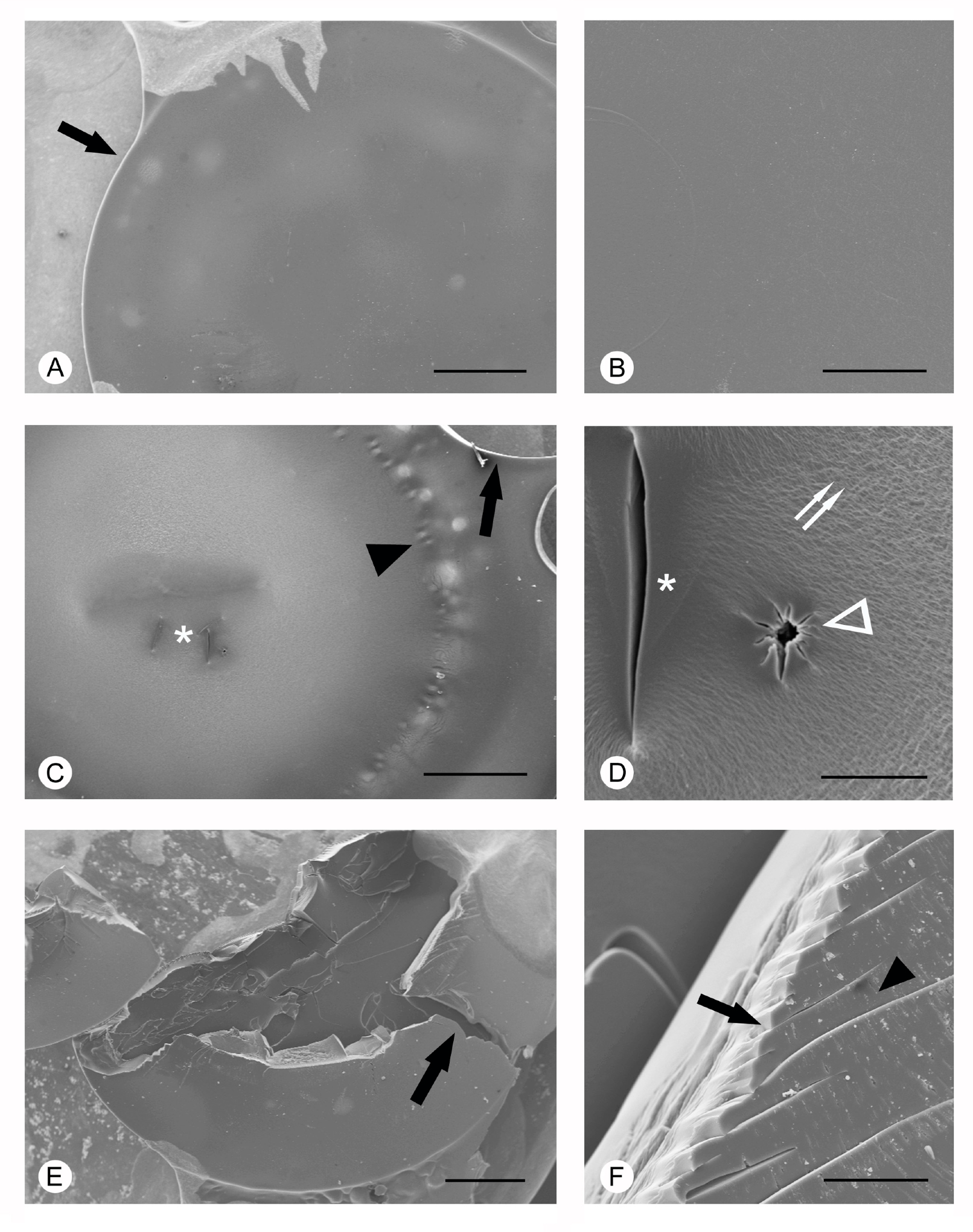
3.1. Scanning Electron Microscopy
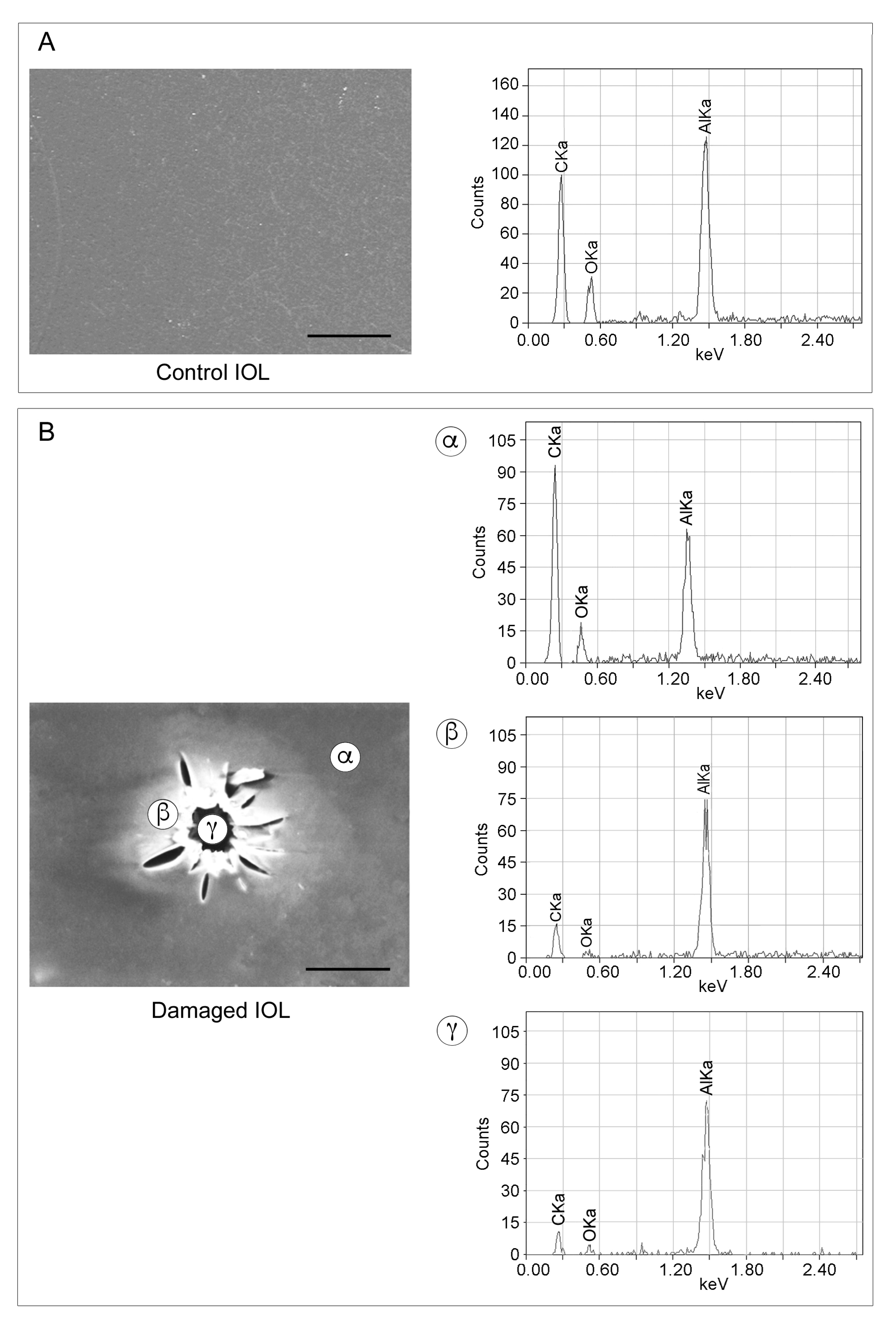
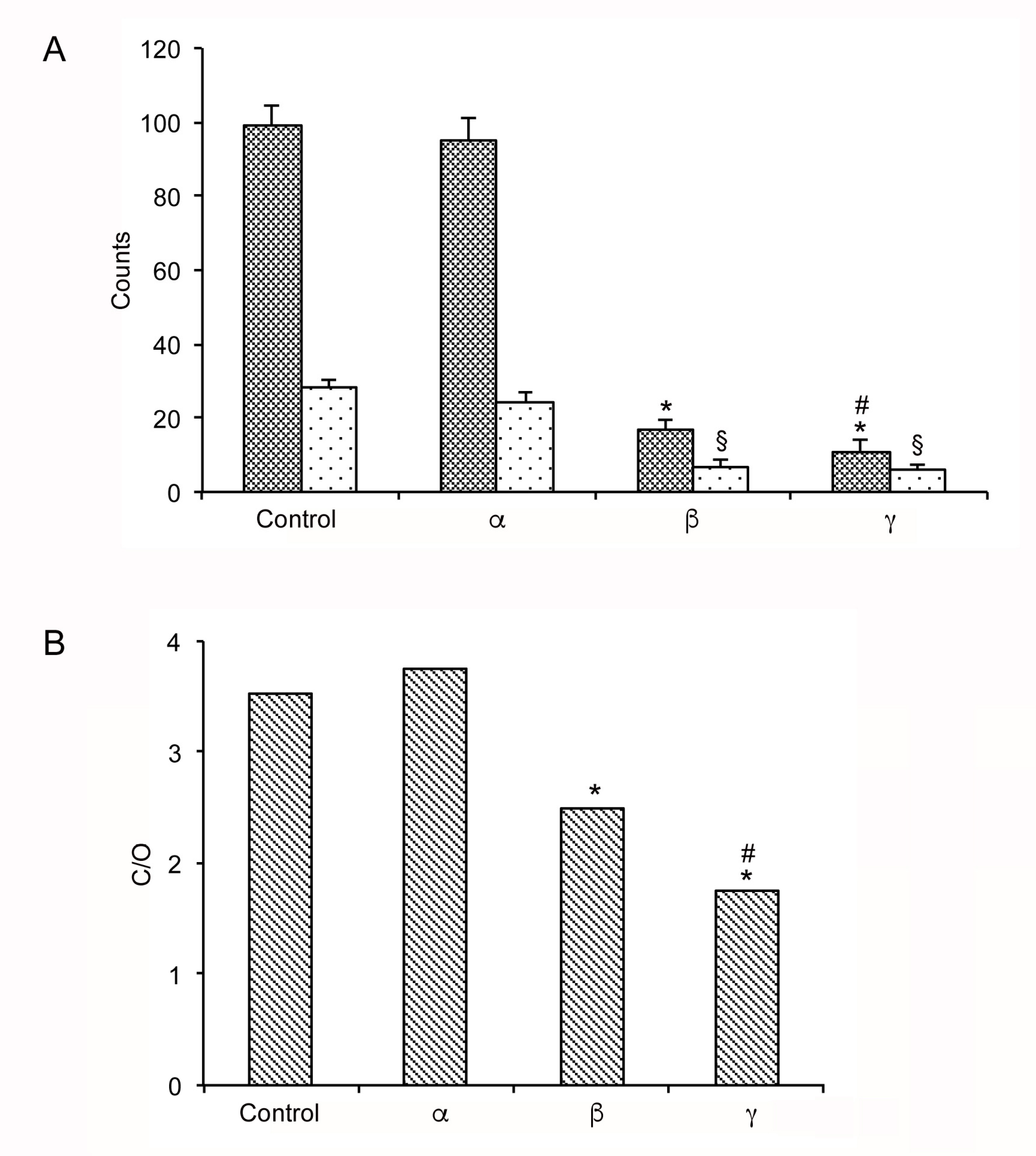
3.2. SEM and EDX Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lee, C.M.; Afshari, N.A. The global state of cataract blindness. Curr. Opin. Ophthalmol. 2017, 28, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.C.; Wilkins, M.; Kim, T.; Malyugin, B.; Mehta, J.S. Cataracts. Lancet 2017, 390, 600–612. [Google Scholar] [CrossRef]
- Lundström, M.; Barry, P.; Henry, Y.; Rosen, P.; Stenevi, U. Evidence-based guidelines for cataract surgery: Guidelines based on data in the European Registry of Quality Outcomes for Cataract and Refractive Surgery database. J. Cataract. Refract. Surg. 2012, 38, 1086–1093. [Google Scholar] [CrossRef] [PubMed]
- Nibourg, L.M.; Gelens, E.; Kuijer, R.; Hooymans, J.M.; van Kooten, T.G.; Koopmans, S.A. Prevention of posterior capsular opacification. Exp. Eye Res. 2015, 136, 100–115. [Google Scholar] [CrossRef]
- Kossack, N.; Schindler, C.; Weinhold, I.; Hickstein, L.; Lehne, M.; Walker, J.; Neubauer, A.S.; Häckl, D. German claims data analysis to assess impact of different intraocular lenses on posterior capsule opacification and related healthcare costs. Z. Gesundh. Wiss. 2018, 26, 81–90. [Google Scholar] [CrossRef]
- Iliescu, I.M.; Constantin, M.A.; Cozma, C.; Moraru, O.M.; Moraru, C.M. Posterior Capsule Opacification and Nd-YAG rates evaluation in a large series of pseudophakic cases. Rom. J. Ophthalmol. 2017, 61, 267–274. [Google Scholar] [CrossRef]
- Aslam, T.M.; Devlin, H.; Dhillon, B. Use of Nd:YAG laser capsulotomy. Surv. Ophthalmol. 2003, 48, 594–612. [Google Scholar] [CrossRef]
- Karahan, E.; Er, D.; Kaynak, S. An Overview of Nd:YAG Laser Capsulotomy. Med. Hypothesis Discov. Innov. Ophthalmol. 2014, 3, 45–50. [Google Scholar]
- Bath, P.E.; Boerner, C.F.; Dang, Y. Pathology and physics of YAG-laser intraocular lens damage. J. Cataract Refract. Surg. 1987, 13, 47–49. [Google Scholar] [CrossRef]
- Bath, P.E.; Hoffer, K.J.; Aron-Rosa, D.; Dang, Y. Glare disability secondary to YAG laser intraocular lens damage. J. Cataract Refract. Surg. 1987, 13, 309–313. [Google Scholar] [CrossRef]
- Capon, M.R.; Docchio, F.; Leoni, G.; Trabucchi, G.; Brancato, R. Comprehensive study of damage to intraocular lenses by single and multiple nanosecond neodymium: YAG laser pulses. J. Cataract Refract. Surg. 1990, 16, 603–610. [Google Scholar] [CrossRef]
- Newland, T.J.; Auffarth, G.U.; Wesendahl, T.A.; Apple, D.J. Neodymium:YAG laser damage on silicone intraocular lenses. A comparison of lesions on explanted lenses and experimentally produced lesions. J. Cataract Refract. Surg. 1994, 20, 527–533. [Google Scholar] [CrossRef]
- Trinavarat, A.; Atchaneeyasakul, L.; Udompunturak, S. Neodymium:YAG laser damage threshold of foldable intraocular lenses. J. Cataract Refract. Surg. 2001, 27, 775–780. [Google Scholar] [CrossRef]
- Nweke, M.C.; Turmaine, M.; McCartney, R.G.; Bracewell, D.G. Drying techniques for the visualisation of agarose-based chromatography media by scanning electron microscopy. Biotechnol. J. 2017, 12, 1600583. [Google Scholar] [CrossRef] [PubMed]
- Beale, A.B.; Salmon, J.; Michau, T.M.; Gilger, B.C. Effect of ophthalmic Nd:YAG laser energy on intraocular lenses after posterior capsulotomy in normal dog eyes. Vet. Ophthalmol. 2006, 9, 335–340. [Google Scholar] [CrossRef]
- Bozzola, J.J. Conventional specimen preparation techniques for scanning electron microscopy of biological specimens. In Electron Microscopy: Methods and Protocols, Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2014; pp. 133–150. [Google Scholar]
- Pinna, A.; Sechi, L.A.; Zanetti, S.; Delogu, D.; Carta, F. Adherence of ocular isolates of staphylococcus epidermidis to ACRYSOF intraocular lenses. A scanning electron microscopy and molecular biology study. Ophthalmology 2000, 107, 2162–2166. [Google Scholar] [CrossRef]
- Chirila, T.V.; Constable, I.J.; van Saarloos, P.P.; Barrett, G.D. Laser-induced damage to transparent polymers: Chemical effect of short-pulsed (Q-switched) Nd:YAG laser radiation on ophthalmic acrylic biomaterials. I. A review. Biomaterials 1990, 11, 305–312. [Google Scholar] [CrossRef]
- Núñez-López, M.T.; del Rosario-Hernández, G.; López-Gómez, L.; Mestres-Ventura, P. Specimen preparation for “block face” scanning electron microscopy (BFSEM). An energy-dispersive X-ray spectroscopy study. Eur. J. Anat. 2018, 22, 471–481. [Google Scholar]
- Gartaganis, S.P.; Prahs, P.; Lazari, E.D.; Gartaganis, P.S.; Helbig, H.; Koutsoukos, P.G. Calcification of Hydrophilic Acrylic Intraocular Lenses with a Hydrophobic Surface: Laboratory Analysis of 6 Cases. Am. J. Ophthalmol. 2016, 168, 68–77. [Google Scholar] [CrossRef]
- Rapado, M.; Peniche, C. Synthesis and characterization of pH and temperature responsive poly(2-hydroxyethyl methacrylate-co-acrylamide) hydrogels. Polímeros 2015, 25, 547–555. [Google Scholar] [CrossRef]
- Faraguna, F.; Siuc, V.; Vidović, E.; Jukić, A. Reactivity ratios and properties of copolymers of 2-ethoxyethyl methacrylate with dodecyl methacrylate or styrene. J. Polym. Res. 2015, 22, 245. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meduri, A.; Severo, A.A.; De Maria, A.; Perroni, P.; Acri, G.; Testagrossa, B.; Puzzolo, D.; Montalbano, G.; Aragona, P.; Micali, A.G. PMMA Intraocular Lenses Changes after Treatment with Nd:Yag Laser: A Scanning Electron Microscopy and X-ray Spectrometry Study. Appl. Sci. 2020, 10, 6321. https://doi.org/10.3390/app10186321
Meduri A, Severo AA, De Maria A, Perroni P, Acri G, Testagrossa B, Puzzolo D, Montalbano G, Aragona P, Micali AG. PMMA Intraocular Lenses Changes after Treatment with Nd:Yag Laser: A Scanning Electron Microscopy and X-ray Spectrometry Study. Applied Sciences. 2020; 10(18):6321. https://doi.org/10.3390/app10186321
Chicago/Turabian StyleMeduri, Alessandro, Alice Antonella Severo, Antonio De Maria, Pietro Perroni, Giuseppe Acri, Barbara Testagrossa, Domenico Puzzolo, Giuseppe Montalbano, Pasquale Aragona, and Antonio Girolamo Micali. 2020. "PMMA Intraocular Lenses Changes after Treatment with Nd:Yag Laser: A Scanning Electron Microscopy and X-ray Spectrometry Study" Applied Sciences 10, no. 18: 6321. https://doi.org/10.3390/app10186321
APA StyleMeduri, A., Severo, A. A., De Maria, A., Perroni, P., Acri, G., Testagrossa, B., Puzzolo, D., Montalbano, G., Aragona, P., & Micali, A. G. (2020). PMMA Intraocular Lenses Changes after Treatment with Nd:Yag Laser: A Scanning Electron Microscopy and X-ray Spectrometry Study. Applied Sciences, 10(18), 6321. https://doi.org/10.3390/app10186321





