Topical Application of Chlorhexidine Gel with Brush-On Technique in the Tailored Treatment of Plaque Induced Gingivitis
Abstract
:1. Introduction
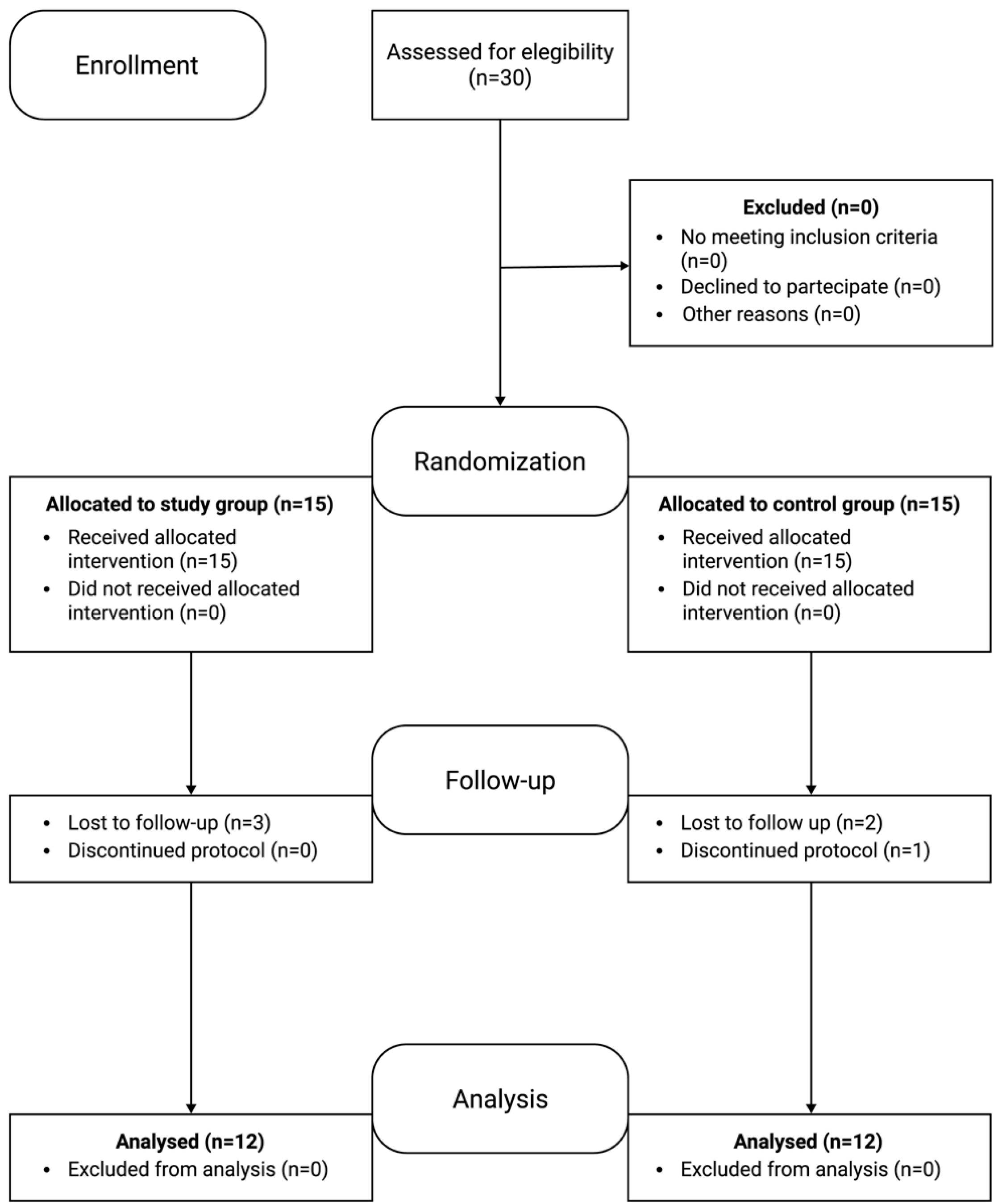
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- White, D.A.; Tsakos, G.; Pitts, N.B.; Fuller, E.; Douglas, G.; Murray, J.J.; Steele, J. Adult Dental Health Survey 2009: Common oral health conditions and their impact on the population. Br. Dent. J. 2012, 213, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Trombelli, L.; Farina, R.; Silva, C.O.; Tatakis, D.N. Plaque-induced gingivitis: Case definition and diagnostic considerations. J. Periodontol. 2018, 89, 46–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L. Dental-plaque induced gingival conditions. J. Periodontol. 2018, 89, 17–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Academy of Periodontology-Research, Science, and Therapy Committee; American Academy of Pediatric Dentistry. Treatment of plaque-induced gingivitis, chronic periodontitis, and other clinical conditions. Pediatr. Dent. 2005, 27, 202–211. [Google Scholar]
- Lang, N.P.; Schätzle, M.A.; Löe, H. Gingivitis as a risk factor in periodontal disease. J. Clin. Periodontol. 2009, 36, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Tatakis, D.N.; Trombelli, L. Modulation of clinical expression of plaque-induced gingivitis. I. Background review and rationale. J. Clin. Periodontol. 2004, 31, 229–238. [Google Scholar] [CrossRef] [PubMed]
- David, S.C.; Mário, T.G.; De Freitas, G.C.; Kantorski, K.Z.; Wikesjö, U.M.E.; Moreira, C.H.C. Correlation between plaque control and gingival health using short and extended oral hygiene intervals. Clin. Oral. Investig. 2018, 22, 2593–2597. [Google Scholar] [CrossRef]
- Graziani, F.; Karapetsa, D.; Alonso, B.; Herrera, D. Nonsurgical and surgical treatment of periodontitis: How many options for one disease? Periodontol. 2000 2017, 75, 152–188. [Google Scholar] [CrossRef]
- Westfelt, E. Rationale of mechanical plaque control. J. Clin. Periodontol. 1996, 23, 263–267. [Google Scholar] [CrossRef]
- Serrano, J.; Escribano, M.; Roldán, S.; Martín, C.; Herrera, D. Efficacy of adjunctive anti-plaque chemical agents in managing gingivitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2015, 42, 106–138. [Google Scholar] [CrossRef]
- Jentsch, H.F.; Eckert, F.R.; Eschrich, K.; Stratul, S.I.; Kneist, S. Antibacterial action of Chlorhexidine/thymol containing varnishes in vitro and in vivo. Int. J. Dent. Hyg. 2014, 12, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Park, E.; Na, H.S.; Kim, S.M.; Wallet, S.; Cha, S.; Chung, J. Xylitol, an anticaries agent, exhibits potent inhibition of inflammatory responses in human THP-1-derived macrophages infected with Porphyromonas gingivalis. J. Periodontol. 2014, 85, 212–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Löe, H. The Gingival Index, the Plaque Index and the Retention Index Systems. J. Periodontol. 1967, 38, 610–616. [Google Scholar] [CrossRef]
- Nardi, G.M.; Sabatini, S.; Guerra, F.; Tatullo, M.; Ottolenghi, L. Tailored Brushing Method (TBM): An innovative simple protocol to improve oral care. J. Biomed. 2016, 1, 26–31. [Google Scholar] [CrossRef] [Green Version]
- Frencken, J.E.; Sharma, P.; Stenhouse, L.; Green, D.; Laverty, D.; Dietrich, T. Global epidemiology of dental caries and severe periodontitis - a comprehensive review. J. Clin. Periodontol. 2017, 44, 94–105. [Google Scholar] [CrossRef]
- Durham, J.; Fraser, H.M.; McCracken, G.I.; Stone, K.M.; John, M.T.; Preshaw, P.M. Impact of periodontitis on oral health-related quality of life. J. Dent. 2013, 41, 370–376. [Google Scholar] [CrossRef]
- Chapple, I.L. Primary prevention of periodontitis: Managing gingivitis. J. Clin. Periodontol. 2015, 42, 71–76. [Google Scholar] [CrossRef] [Green Version]
- Van der Weijden, F.A.; Slot, D.E. Efficacy of homecare regimens for mechanical plaque removal in managing gingivitis a meta review. J. Clin. Periodontol. 2015, 42, 77–91. [Google Scholar] [CrossRef]
- Ribeiro, L.G.; Hashizume, L.N.; Maltz, M. The effect of different formulations of chlorhexidine in reducing levels of mutans streptococci in the oral cavity: A systematic review of the literature. J. Dent. 2007, 35, 359–370. [Google Scholar] [CrossRef]
- Supranoto, S.; Slot, D.; Addy, M.; Van der Weijden, G. The effect of chlorhexidine dentifrice or gel versus chlorhexidine mouthwash on plaque, gingivitis, bleeding and tooth discoloration: A systematic review. Int. J. Dent. Hyg. 2014, 13, 83–92. [Google Scholar] [CrossRef]
- Campus, G.; Cagetti, M.G.; Sale, S.; Petruzzi, M.; Solinas, G.; Strohmenger, L.; Lingström, P. Six months of high-dose xylitol in high-risk caries subjects—A 2-year randomised, clinical trial. Clin. Oral. Investig. 2013, 17, 785–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hallström, H.; Lindgren, S.; Twetman, S. Effect of a chlorhexidine-containing brush-on gel on peri-implant mucositis. Int. J. Dent. Hyg. 2017, 15, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Clavero, J.; Baca, P.; Paloma González, M.; Valderrama, M.J. Efficacy chlorhexidine-thymol varnish (Cervitec) against plaque accumulation and gingival inflammation in a geriatric population. Gerodontology 2006, 23, 43–47. [Google Scholar] [CrossRef] [PubMed]
| Group | n. Patients | Decrease t0–t3 (%) | p Value | |
|---|---|---|---|---|
| FMPS | Study Control | 12 12 | 87% 75% | 0.03 * 0.03 * |
| GI | Study Control | 12 12 | 84% 80% | 0.03 * 0.03 * |
| Patients | Plaque Score (Means) | Gingival Index (Means) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean Age | Sex | t0 | t1 | t2 | t3 | Δ(t0–t3) | t0 | t1 | t2 | t3 | Δ(t0–t3) | |
| Study group | 12 | 50 | F = 7 M = 5 | 2.11 SD = 0.6 | 1.09 SD = 0.3 | 0.63 SD = 0.2 | 0.31 SD = 0.1 | 1.83 SD = 0.5 | 1.6 SD = 0.5 | 0.9 SD = 0.3 | 0.54 SD = 0.2 | 0.26 SD = 0.1 | 1.34 SD = 0.4 |
| Control group | 12 | 46 | F = 6 M = 6 | 1.16 SD = 0.5 | 0.58 SD = 0.4 | 0.46 SD = 0.4 | 0.48 SD = 0.3 | 0.87 SD = 0.3 | 1.87 SD = 1.1 | 1.46 SD = 1.4 | 0.87 SD = 0.5 | 0.68 SD = 0.5 | 1.17 SD = 0.6 |
| p value | 0.21 | 0.68 | 0.16 | 0.5 | 0.5 | 0.42 | 0.049 | 0.13 | 0.34 | 0.48 | 0.29 | 0.17 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nardi, G.M.; Grassi, R.; Campus, G.; Pareti, M.L.; Stasio, D.D.; Petruzzi, M.; della Vella, F. Topical Application of Chlorhexidine Gel with Brush-On Technique in the Tailored Treatment of Plaque Induced Gingivitis. Appl. Sci. 2020, 10, 6014. https://doi.org/10.3390/app10176014
Nardi GM, Grassi R, Campus G, Pareti ML, Stasio DD, Petruzzi M, della Vella F. Topical Application of Chlorhexidine Gel with Brush-On Technique in the Tailored Treatment of Plaque Induced Gingivitis. Applied Sciences. 2020; 10(17):6014. https://doi.org/10.3390/app10176014
Chicago/Turabian StyleNardi, Gianna Maria, Roberta Grassi, Guglielmo Campus, Maria Letizia Pareti, Dario Di Stasio, Massimo Petruzzi, and Fedora della Vella. 2020. "Topical Application of Chlorhexidine Gel with Brush-On Technique in the Tailored Treatment of Plaque Induced Gingivitis" Applied Sciences 10, no. 17: 6014. https://doi.org/10.3390/app10176014
APA StyleNardi, G. M., Grassi, R., Campus, G., Pareti, M. L., Stasio, D. D., Petruzzi, M., & della Vella, F. (2020). Topical Application of Chlorhexidine Gel with Brush-On Technique in the Tailored Treatment of Plaque Induced Gingivitis. Applied Sciences, 10(17), 6014. https://doi.org/10.3390/app10176014








