Treatment of Symptomatic Vitreous Opacities with Pharmacologic Vitreolysis Using a Mixure of Bromelain, Papain and Ficin Supplement
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Patient Collection Criteria
2.3. Experimental Design and Laboratory Examination
2.4. Statistical Analysis
3. Results and Discussion
3.1. Patient Characteristics
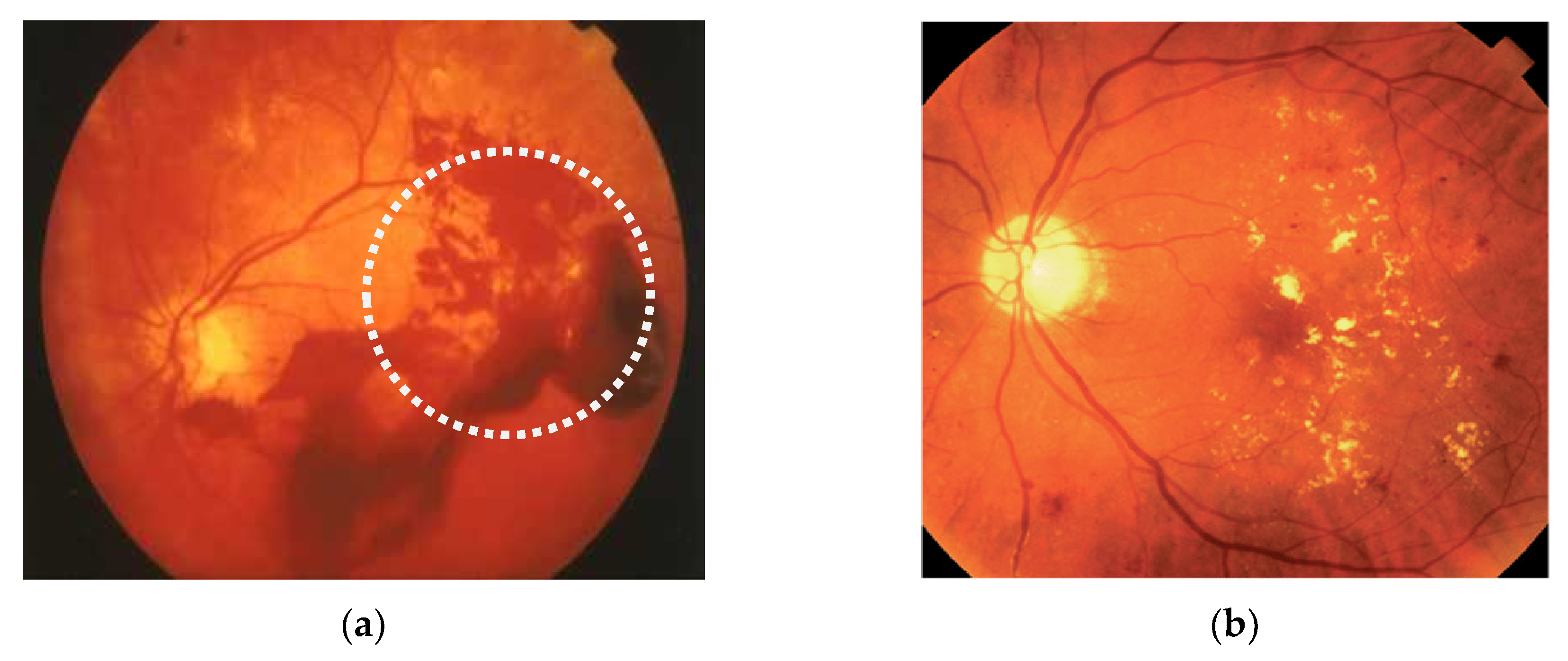
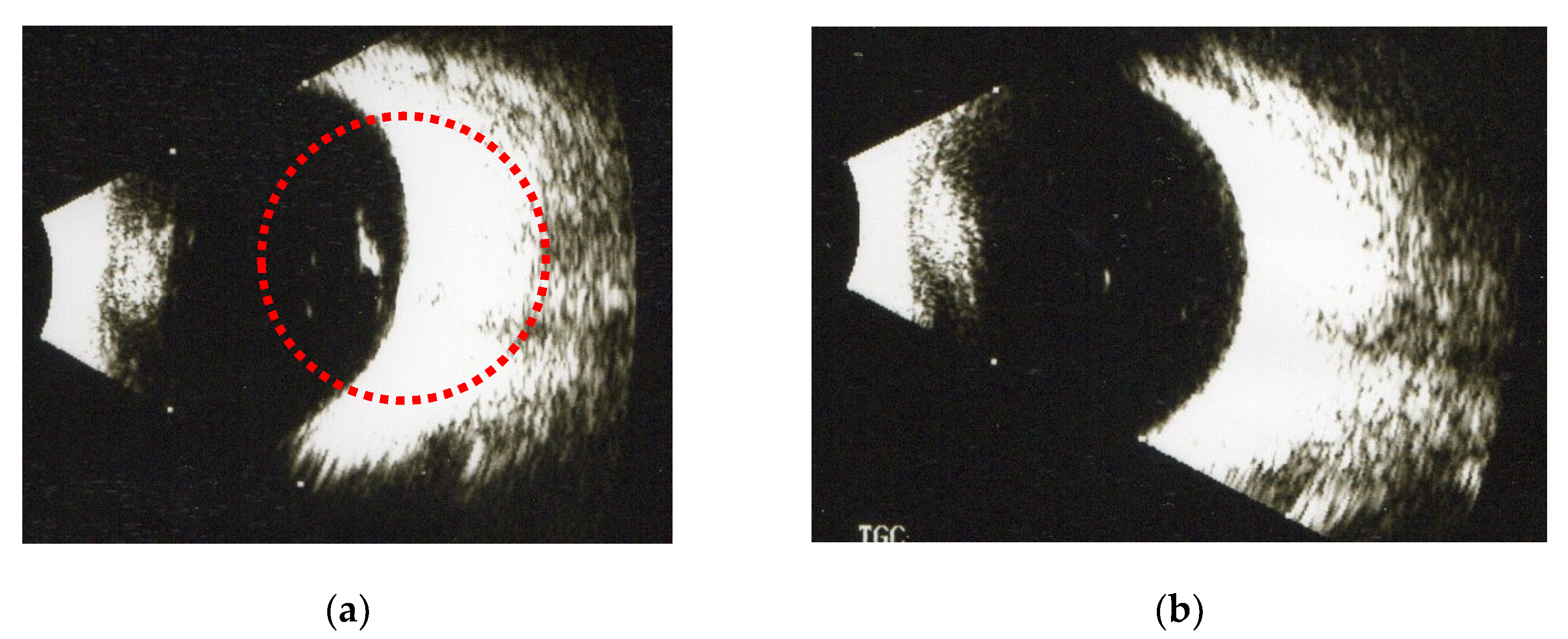
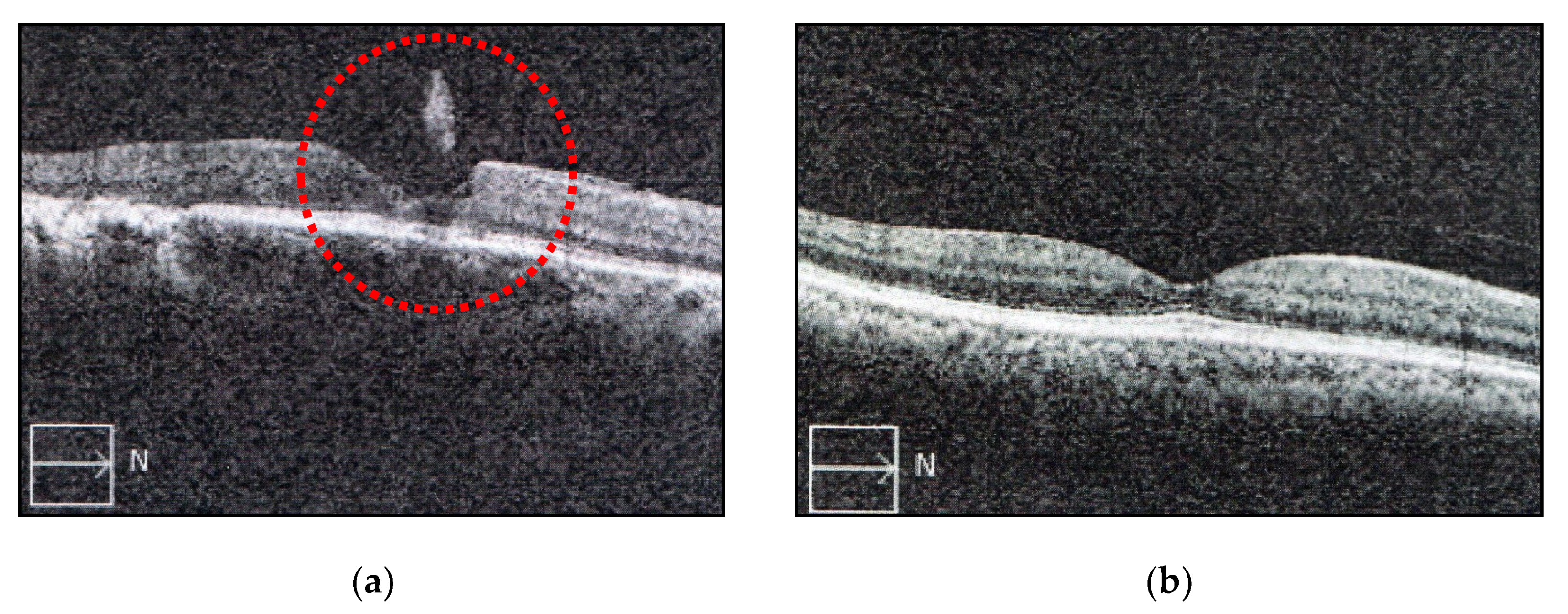
3.2. The Effect of Fruit Enzymes on the Change of Various Floaters
3.3. The Effect of Fruit Enzymes at Differential Concentration on the Change of Various Floaters
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Yamada, S.; Sugahara, K.; Özbek, S. Evolution of glycosaminoglycans. Commun. Integr. Biol. 2011, 4, 150–158. [Google Scholar] [CrossRef]
- Jackson, T.L.; Nicod, E.; Simpson, A.; Angelis, A.; Grimaccia, F.; Kanavos, P. Symptomatic Vitreomacular Adhesion. Retina 2013, 33, 1503–1511. [Google Scholar] [CrossRef]
- Milston, R.; Madigan, M.C.; Sebag, J. Vitreous floaters: Etilogy, diagnosis, and management. Surv. Ophthalmol. 2016, 61, 211–227. [Google Scholar] [CrossRef]
- Turon, P.; Del Valle, L.J.; Aleman, C.; Puiggalí, J. Biodegradable and Biocompatible Systems Based on Hydroxyapatite Nanoparticles. Appl. Sci. 2017, 7, 60. [Google Scholar] [CrossRef]
- Lumi, X.; Hawlina, M.; Glavač, D.; Facsko, A.; Moe, M.C.; Kaarniranta, K.; Petrovski, G. Ageing of the vitreous: From acute onset floaters and flashes to retinal detachment. Ageing Res. Rev. 2015, 21, 71–77. [Google Scholar] [CrossRef]
- Colucciello, M.; Sebag, J.; Koch, F. Controversies in care—Vitrectomy for floaters. Retin. Phys. 2014, 11, 14–17. [Google Scholar]
- Morita, H.; Funata, M.; Tokoro, T. A clinical study of the development of posterior vitreous detachment in high myopia. Retina 1995, 15, 117–124. [Google Scholar] [CrossRef]
- Overdam, K.; Bettink-Remeijer, M.W.; Klaver, C.C.W.; Mulder, P.G.; Moll, A.C.; Van Meurs, J.C. Symptoms and Findings Predictive for the Development of New Retinal Breaks. Arch. Ophthalmol. 2005, 123, 479–484. [Google Scholar] [CrossRef]
- Ponsioen, T.L.; Van Luyn, M.J.A.; Van Der Worp, R.; Van Meurs, J.C.; Hooymans, J.; Los, L.I. Collagen Distribution in the Human Vitreoretinal Interface. Investig. Opthalmol. Vis. Sci. 2008, 49, 4089–4095. [Google Scholar] [CrossRef]
- Akiba, J.; Ueno, N.; Chakrabarti, B. Mechanisms of photo-induced vitreous liquefaction. Curr. Eye Res. 1994, 13, 505–512. [Google Scholar] [CrossRef]
- Mason, J.O., III; Neimkin, M.G.; Mason, J.O., IV; Friedman, D.A.; Feist, R.M.; Thomley, M.L.; Albert, M.A. Safety, efficacy, and quality of life following sutureless vitrevtomy for symptomatic vitreous floater. Retina 2014, 34, 1055–1061. [Google Scholar] [CrossRef]
- Vandorselaer, T.; Van De Velde, F.; Tassignon, M.J. Eligibility criteria for Nd-YAG laser treatment of highly symptomatic vitreous floaters. Bull. Soc. Belg. D’ophtalmol. 2001, 280, 15–22. [Google Scholar]
- Stoffelns, B.M.; Vetter, J.; Keicher, A.; Mirshahi, A. Pars plana vitrectomy for visually disturbing vitreous floaters in pseudophakic eyes. Klinische Monatsblätter für Augenheilkunde 2011, 228, 293–297. [Google Scholar] [CrossRef]
- Shi, X.-Y.; Zhao, H.-S.; Wei, W.-B. Analysis of post-operative endophthalmitis after pars plana vitrectomy: A 10-year experience at a single center. Chin. Med. J. 2013, 126, 2890–2893. [Google Scholar]
- Goh, Y.W.; Ehrlich, R.; Stewart, J.; Polkinghorne, P. The Incidence of Retinal Breaks in the Presenting and Fellow Eyes in Patients With Acute Symptomatic Posterior Vitreous Detachment and Their Associated Risk Factors. Asia Pac. J. Ophthalmol. 2015, 4, 5–8. [Google Scholar] [CrossRef]
- Arshad, Z.I.M.; Amid, A.; Yusof, F.; Jaswir, I.; Ahmad, K.; Show, P.L. Bromelain: An overview of industrial application and purification strategies. Appl. Microbiol. Biotechnol. 2014, 98, 7283–7297. [Google Scholar] [CrossRef]
- Doneva, M.; Nacheva, I.; Dyankova, S.; Metodieva, P.; Miteva, D. Application of plant proteolytic enzymes for tenderization of rabbit meat. Biotechnol. Anim. Husb. 2018, 34, 229–238. [Google Scholar] [CrossRef]
- Hafid, K.; John, J.; Sayah, T.M.; Domínguez, R.; Becila, S.; Lamri, M.; Dib, A.L.; Lorenzo, J.M.; Gagaoua, M. One-step recovery of latex papain from Carica papaya using three phase partitioning and its use as milk-clotting and meat-tenderizing agent. Int. J. Biol. Macromol. 2020, 146, 798–810. [Google Scholar] [CrossRef]
- Gagaoua, M.; Boucherba, N.; Bouanane-Darenfed, A.; Ziane, F.; Nait-Rabah, S.; Hafid, K.; Boudechicha, H.R. Three-phase partitioning as an efficient method for the purification and recovery of ficin from Mediterranean fig (Ficus carica L.) latex. Sep. Purif. Technol. 2014, 132, 461–467. [Google Scholar] [CrossRef]
- Morellon-Sterling, R.; El-Siar, H.; Tavano, O.L.; Berenguer-Murcia, Á.; Fernández-Lafuente, R. Ficin: A protease extract with relevance in biotechnology and biocatalysis. [published online ahead of print, 20 June 2020]. Int. J. Biol. Macromol. 2020, 162, 394–404. [Google Scholar] [CrossRef]
- Ivanova, T.; Jalil, A.; Antoniou, Y.; Bishop, P.N.; Vallejo-Garcia, J.L.; Patton, N. Vitrectomy for primary symptomatic opacities: An evidence-bsed review. Eye 2016, 30, 645–655. [Google Scholar] [CrossRef]
- Wagle, A.M.; Lim, W.-Y.; Yap, T.-P.; Neelam, K.; Eong, K.-G.A. Utility Values Associated With Vitreous Floaters. Am. J. Ophthalmol. 2011, 152, 60–65. [Google Scholar] [CrossRef]
- Saglar, E.; Ünlü, S.; Babalioglu, I.; Gokce, S.C.; Mergen, H. Assessment of ER Stress and Autophagy Induced by Ionizing Radiation in Both Radiotherapy Patients and Ex Vivo Irradiated Samples. J. Biochem. Mol. Toxicol. 2014, 28, 413–417. [Google Scholar] [CrossRef]
- Hahn, P.; Schneider, E.W.; Tabandeh, H.; Wong, R.W.; Emerson, G.G. American Society of Retina Specialists Research and Safety in Therapeutics (ASRS ReST) Committee Reported Complications Following Laser Vitreolysis. JAMA Ophthalmol. 2017, 135, 973–976. [Google Scholar] [CrossRef]
- Bennison, C.; Stephens, S.J.; Lescrauwaet, B.; Van Hout, B.; Jackson, T.L. Cost-effectiveness of ocriplasmin for the treatment of vitreomacular traction and macular hole. J. Mark. Access Health Policy 2016, 4, 215. [Google Scholar] [CrossRef]
- Koss, M.J.; Falabella, P.; Pfister, M.; Niemeyer, M.; Kashani, A.H.; Humayun, M.S.; Maia, M.; Stefanini, F.R. Profile of ocriplasmin and its potential in the treatment of vitreomacular adhesion. Clin. Ophthalmol. 2014, 8, 847–856. [Google Scholar] [CrossRef][Green Version]
- Gishti, O.; Nieuwenhof, R.V.D.; Verhoekx, J.S.N.; Overdam, K. Symptoms related to posterior vitreous detachment and the risk of developing retinal tears: A systematic review. Acta Ophthalmol. 2019, 97, 347–352. [Google Scholar] [CrossRef]
- Sharma, M.C.; Regillo, C.D.; Shuler, M.F.; Borrillo, J.; Benson, W.E. Determination of the incidence and clinical characteristics of subsequent retinal tears following treatment of the acute posterior vitreous detachment-related initial retinal tears. Am. J. Ophthalmol. 2004, 138, 280–284. [Google Scholar] [CrossRef]
- Nita, M.; Grzybowski, A. The Role of the Reactive Oxygen Species and Oxidative Stress in the Pathomechanism of the Age-Related Ocular Diseases and Other Pathologies of the Anterior and Posterior Eye Segments in Adults. Oxid. Med. Cell. Longev. 2016, 2016, 3164734. [Google Scholar] [CrossRef]
- Bottós, J.M.; Elizalde, J.; Rodrigues, E.B.; Maia, M. Current concepts in vitreomacular traction syndrome. Curr. Opin. Ophthalmol. 2012, 23, 195–201. [Google Scholar] [CrossRef]
- Page-McCaw, A.; Ewald, A.J.; Werb, Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat. Rev. Mol. Cell Biol. 2007, 8, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Shekhter, A.B.; Balakireva, A.V.; Kuznetsova, N.V.; Vukolova, M.N.; Litvitsky, P.F.; Zamyatnin, A.A., Jr. Collagenolytic Enzymes and their Applications in Biomedicine. Curr. Med. Chem. 2019, 26, 487–505. [Google Scholar] [CrossRef] [PubMed]
- Hale, L.P.; Greer, P.K.; Trinh, C.T.; James, C.L. Proteinase activity and stability of natural bromelain preparations. Int. Immunopharmacol. 2005, 5, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Mótyán, J.; Toth, F.; Tőzsér, J. Research Applications of Proteolytic Enzymes in Molecular Biology. Biomolecules 2013, 3, 923–942. [Google Scholar] [CrossRef]
- Rao, M.B.; Tanksale, A.M.; Ghatge, M.S.; Deshpande, V.V. Molecular and Biotechnological Aspects of Microbial Proteases. Microbiol. Mol. Biol. Rev. 1998, 62, 597–635. [Google Scholar] [CrossRef] [PubMed]
- Korenč, M.; Lenarčič, B.; Novinec, M. Human cathepsin L, a papain-like collagenase without proline specificity. FEBS J. 2015, 282, 4328–4340. [Google Scholar] [CrossRef]
- Novinec, M.; Lenarčič, B. Papain-like peptidases: Structure, function, and evolution. Biomol. Concepts 2013, 4, 287–308. [Google Scholar] [CrossRef]
- Zare, H.; Moosavi-Movahedi, A.A.; Salami, M.; Sheibani, N.; Khajeh, K.; Habibi-Rezaei, M. Autolysis control and structural changes of purified ficin from Iranian fig latex with synthetic inhibitors. Int. J. Biol. Macromol. 2016, 84, 464–471. [Google Scholar] [CrossRef][Green Version]
- Cho, U.M.; Choi, D.H.; Yoo, D.S.; Park, S.J.; Hwang, H.S. Inhibitory Effect of Ficin Derived from Fig Latex on Inflammation and Melanin Production in Skin Cells. Biotechnol. Bioprocess Eng. 2019, 24, 288–297. [Google Scholar] [CrossRef]
- Cho, D.-Y.; Jo, K.; Cho, S.Y.; Kim, J.M.; Lim, K.; Suh, H.; Oh, S. Antioxidant Effect and Functional Properties of Hydrolysates Derived from Egg-White Protein. Food Sci. Anim. Resour. 2014, 34, 362–371. [Google Scholar] [CrossRef]
- Horng, C.T.; Chen, F.A.; Kuo, D.H.; Chen, L.C.; Yeh, S.S.; Shieh, P. Pharmacologic vitreolysis of vitreous floaters by 3-month pineapple supplement in Taiwan—A pilot study. J. Am. Sci. 2019, 15, 17–30. [Google Scholar]
| Numbers of SOVs 1 | Before | 1st Month | 2nd Month | 3rd Month |
|---|---|---|---|---|
| One | 80 | 78 | 68 | 24 * (30.0%) |
| Multiple 2 | 40 | 37 | 30 | 11 * (27.5%) |
| Numbers of Capsules Each Day | Before | 1st Month | 2nd Month | 3rd Month |
|---|---|---|---|---|
| none | 40 | 40 | 40 | 38 (95.0%) |
| 1 capsule | 40 | 38 | 33 | 14 * (35.0%) # |
| 2 capsules | 40 | 35 | 32 | 12 * (30.0%) # |
| 3 capsules | 40 | 34 | 30 | 10 * (25.0%) # |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takeuchi, M.; Shieh, P.-C.; Horng, C.-T. Treatment of Symptomatic Vitreous Opacities with Pharmacologic Vitreolysis Using a Mixure of Bromelain, Papain and Ficin Supplement. Appl. Sci. 2020, 10, 5901. https://doi.org/10.3390/app10175901
Takeuchi M, Shieh P-C, Horng C-T. Treatment of Symptomatic Vitreous Opacities with Pharmacologic Vitreolysis Using a Mixure of Bromelain, Papain and Ficin Supplement. Applied Sciences. 2020; 10(17):5901. https://doi.org/10.3390/app10175901
Chicago/Turabian StyleTakeuchi, Masaru, Po-Chuen Shieh, and Chi-Ting Horng. 2020. "Treatment of Symptomatic Vitreous Opacities with Pharmacologic Vitreolysis Using a Mixure of Bromelain, Papain and Ficin Supplement" Applied Sciences 10, no. 17: 5901. https://doi.org/10.3390/app10175901
APA StyleTakeuchi, M., Shieh, P.-C., & Horng, C.-T. (2020). Treatment of Symptomatic Vitreous Opacities with Pharmacologic Vitreolysis Using a Mixure of Bromelain, Papain and Ficin Supplement. Applied Sciences, 10(17), 5901. https://doi.org/10.3390/app10175901







