Biomechanically-Informed Training: The Four Pillars for Knee and ACL Injury Prevention Built Upon Behavior Change and Motivation Principles
Abstract
1. Background
2. The Context
3. The Problem
4. A Potential Solution
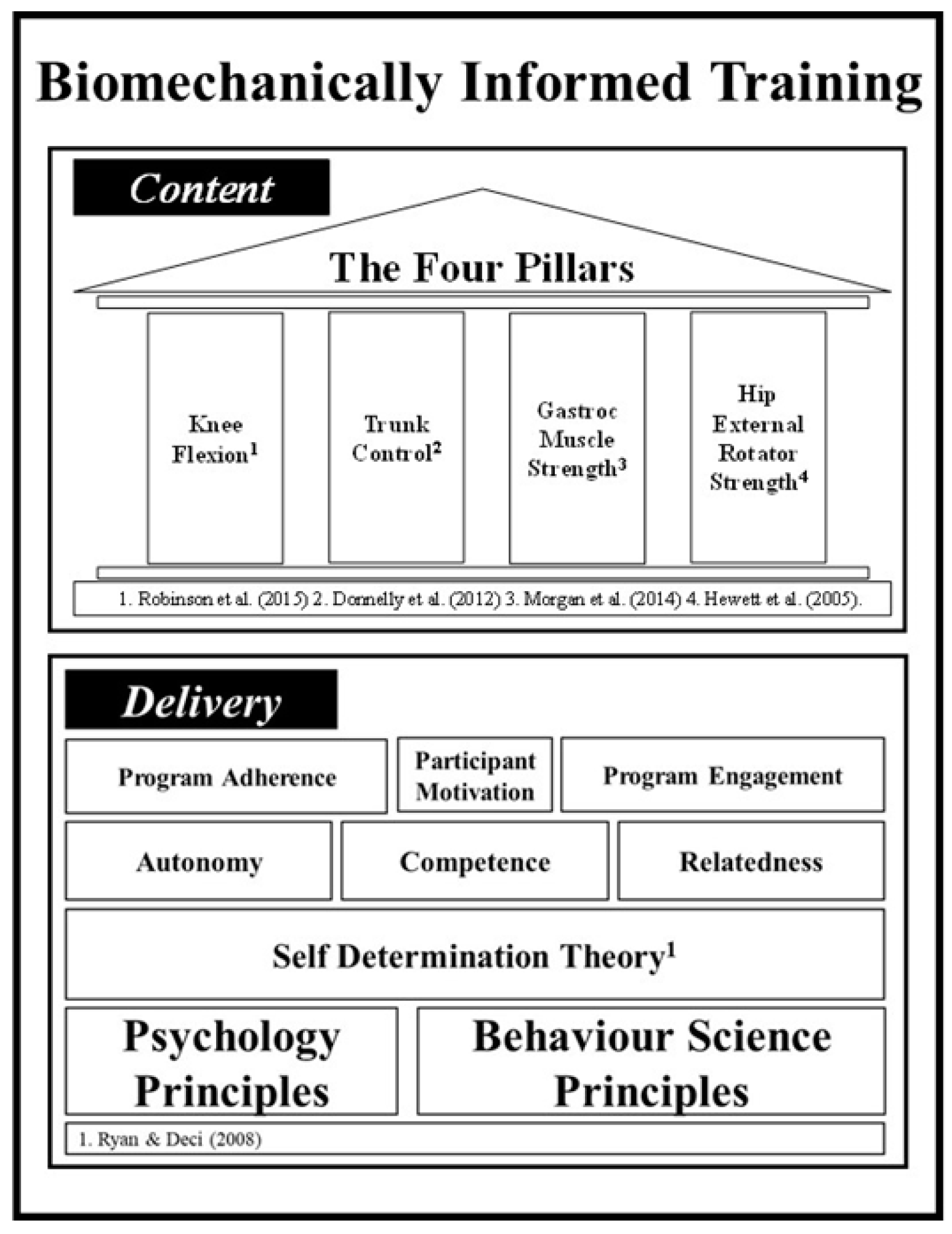
5. Biomechanically-Informed Training
6. Program Content
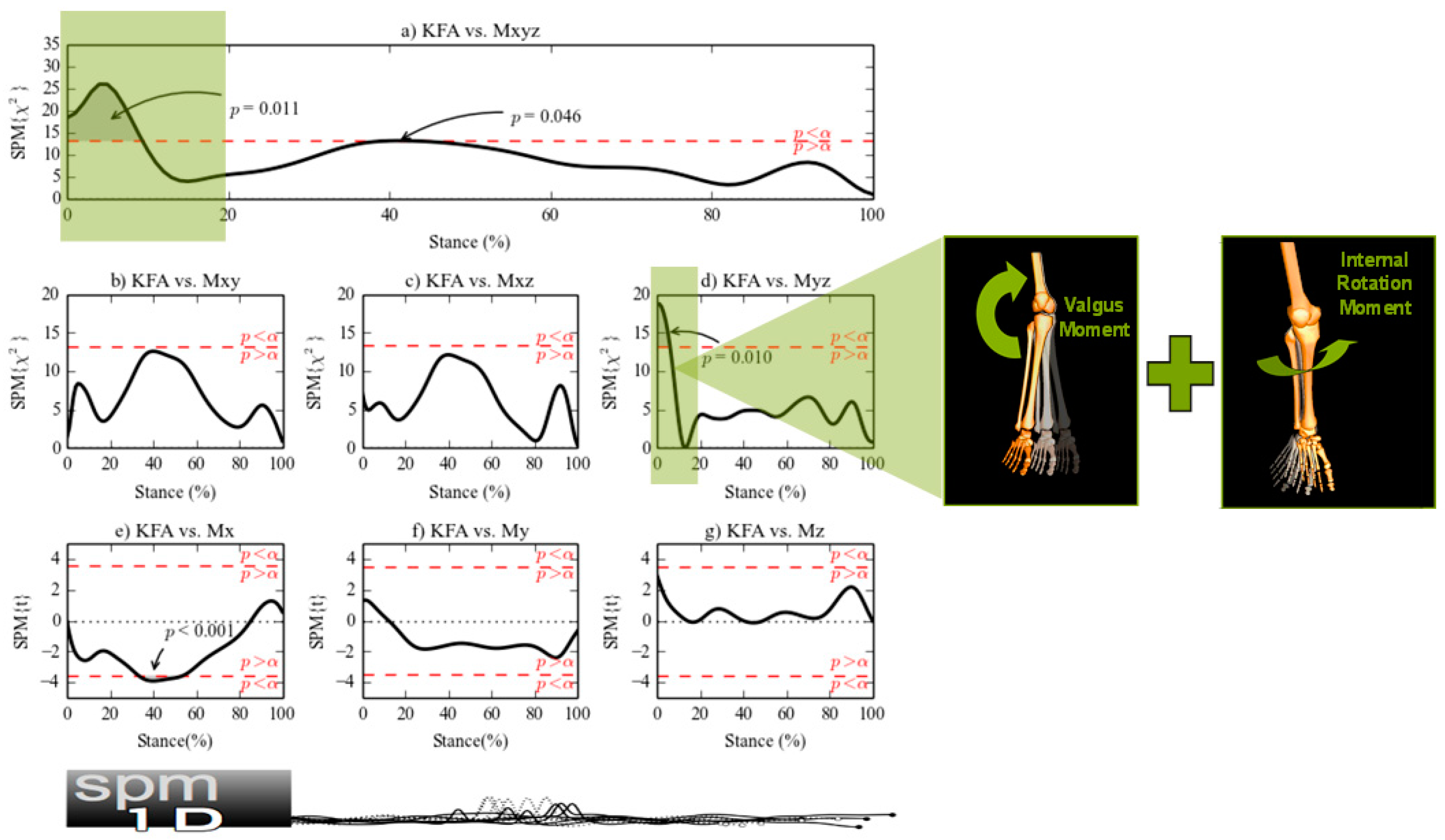
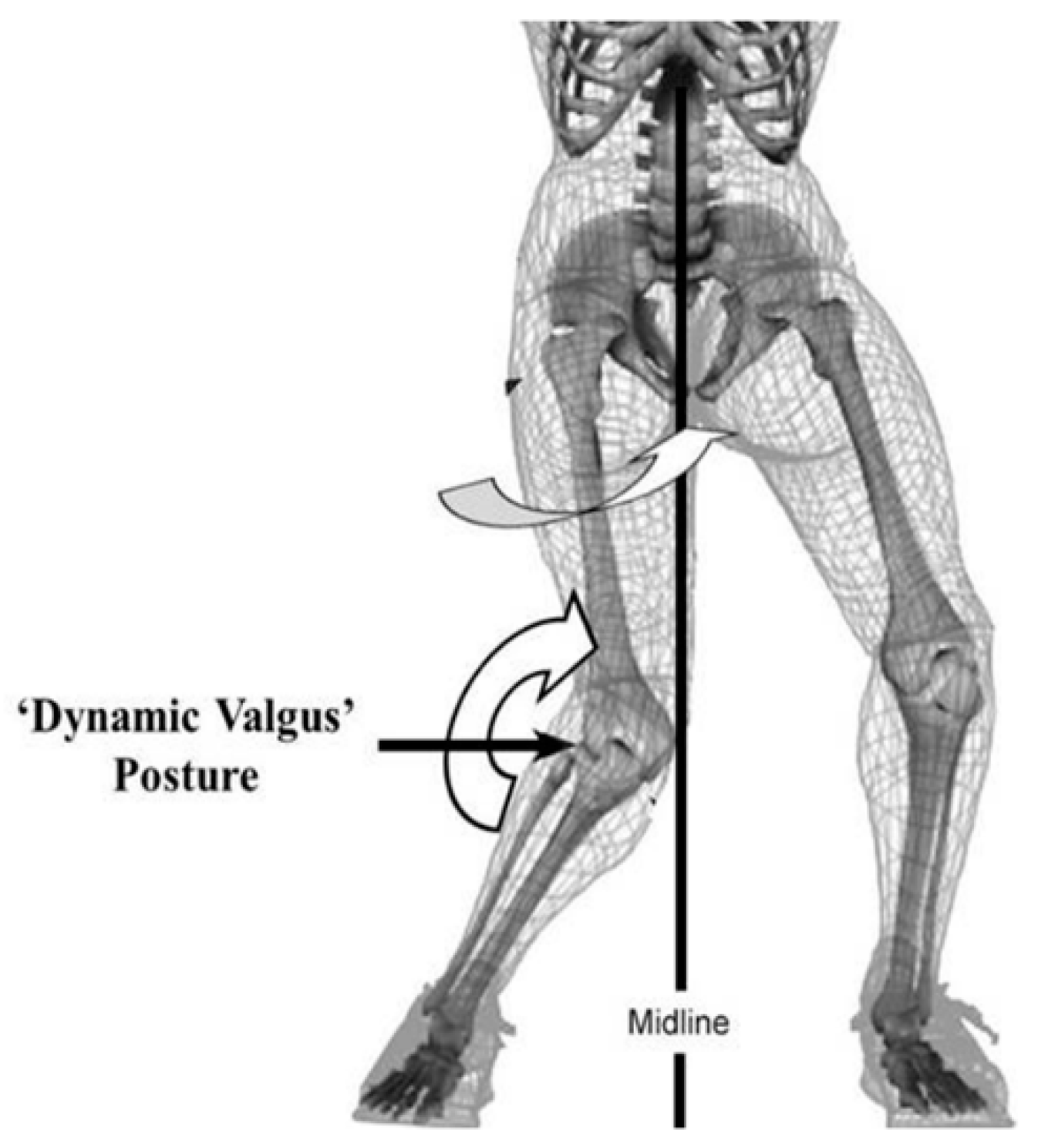
6.1. Training Content Pillar #1: Knee Flexion Dynamics
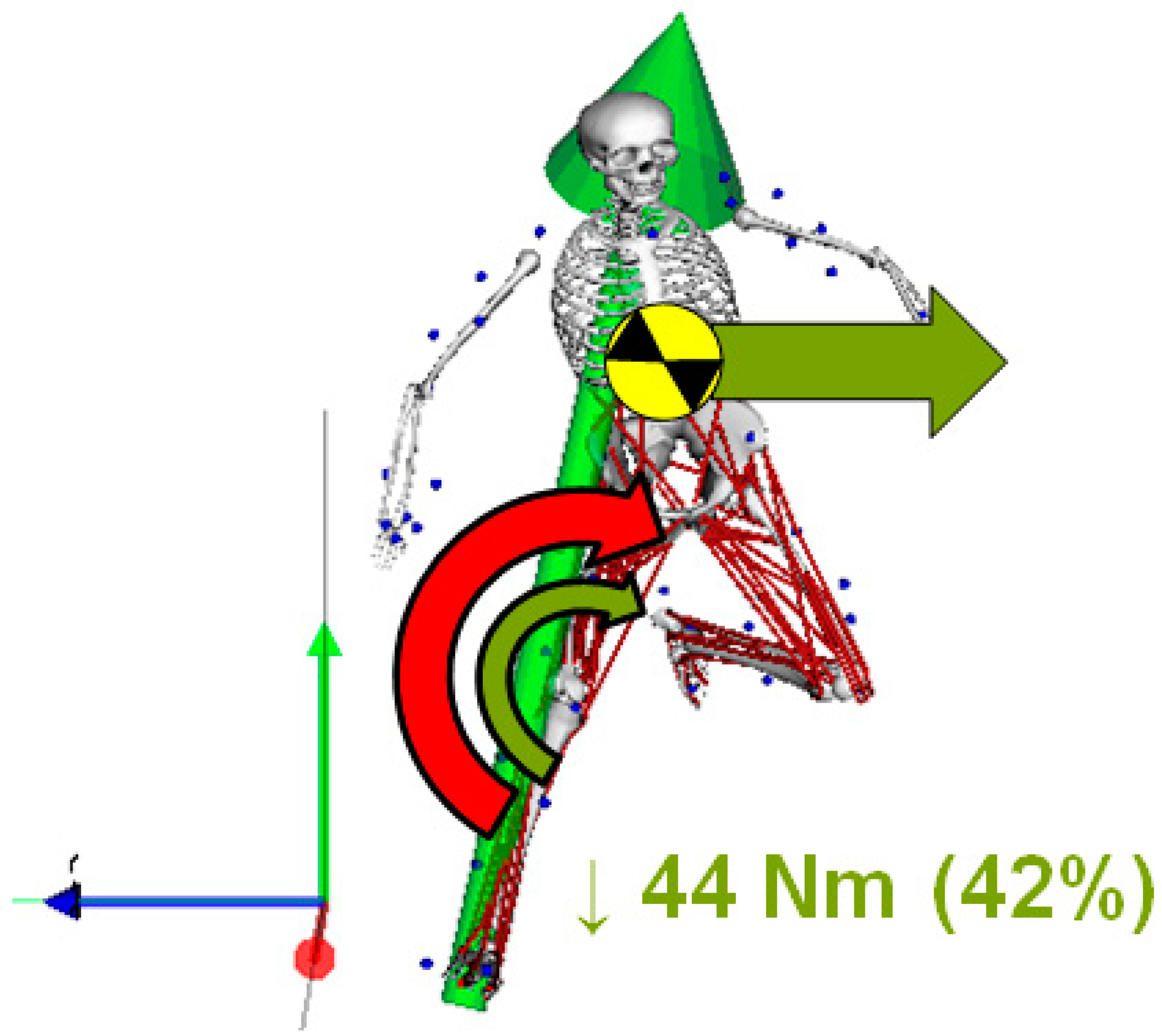
6.2. Training Content Pillar #2: Trunk Control
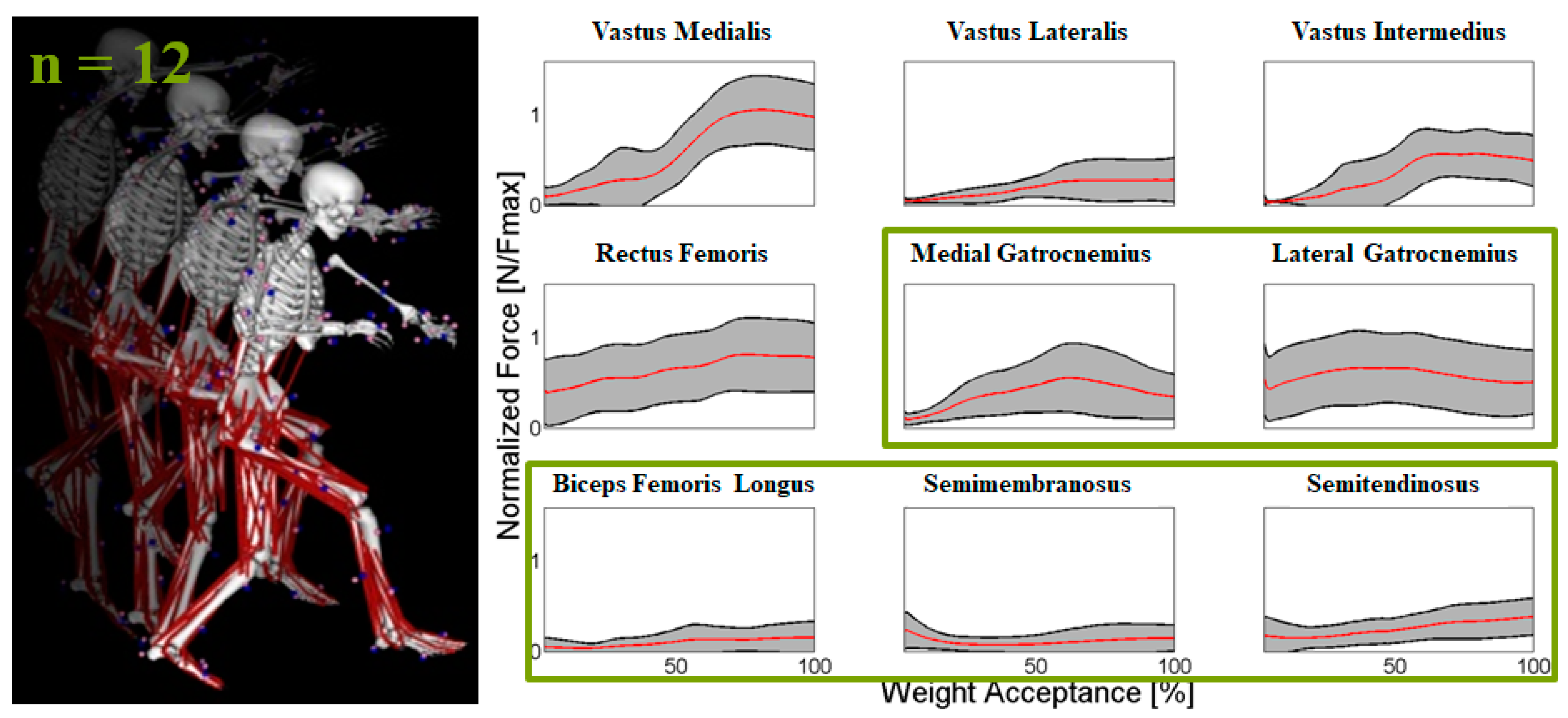
6.3. Training Content Pillar #3: Gastrocnemius Muscle Strength
6.4. Training Content Pillar #4: Hip External Rotator Strength
7. Delivery Principles
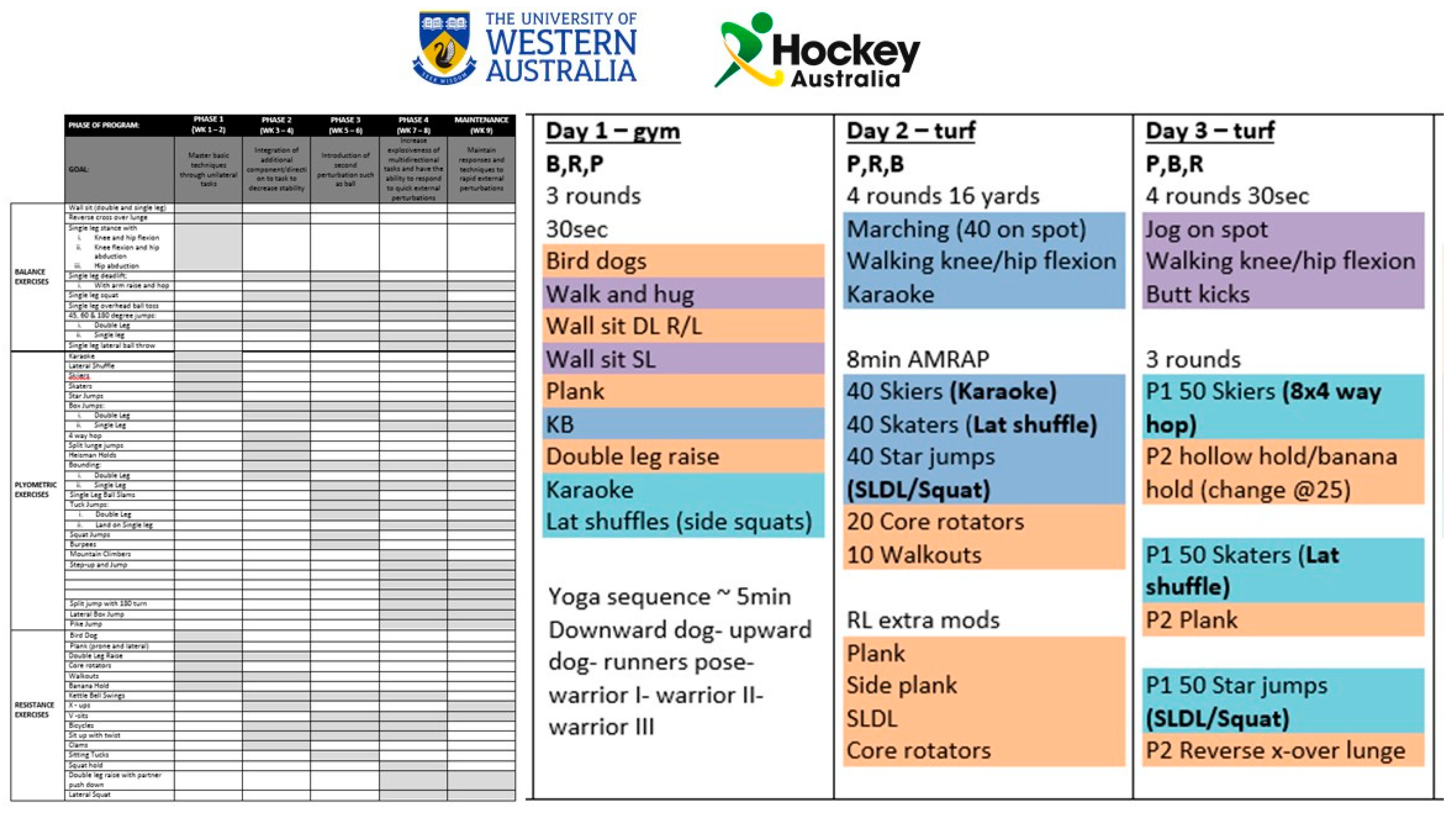
8. Real World Application
9. Summary
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Muybridge, E. The Science of the horse’s Motion. Sci. Am. 1878, 39, 241. [Google Scholar]
- Elfman, H. The measurement of the external forces in walking. Science 1938, 88, 152–153. [Google Scholar] [CrossRef]
- Wolf, S. Handbook of Human Motion; Müller, B., Wolf, S.I., Brüggemann, G.-P., Deng, Z., McIntosh, A.S., Miller, F., Selbie, W.S., Eds.; Springer: Berlin/Heidelberg, Germany, 2018; ISBN 978-3-319-14417-7. [Google Scholar]
- Sheeran, P.; Klein, W.M.P.; Rothman, A.J. Health behavior change: Moving from observation to intervention. Annu. Rev. Psychol. 2017, 68, 573–600. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68. [Google Scholar] [CrossRef]
- Finch, C.F.; Kemp, J.L.; Clapperton, A.J. The incidence and burden of hospital-treated sports-related injury in people aged 15+ years in Victoria, Australia, 2004–2010: A future epidemic of osteoarthritis? Osteoarthr. Cartil. 2015, 23, 1138–1143. [Google Scholar] [CrossRef]
- Gianotti, S.M.; Marshall, S.W.; Hume, P.A.; Blunt, L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J. Sci. Med. Sport 2009, 12, 622–627. [Google Scholar] [CrossRef]
- Janssen, K.W.; Orchard, J.W.; Driscoll, T.R.; van Mechelen, W. High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003–2004 to 2007–2008: Time for an anterior cruciate ligament register by Scandinavian model? Scand. J. Med. Sci. Sports 2012, 22, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Strehl, A.; Eggli, S. The value of conservative treatment in ruptures of the anterior cruciate ligament (ACL). J. Trauma 2007, 62, 1159–1162. [Google Scholar] [CrossRef] [PubMed]
- Hartigan, E.H.; Axe, M.J.; Snyder-Mackler, L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J. Orthop. Sport Phys. Ther. 2010, 40, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Orchard, J.; Seward, H.; McGivern, J.; Hood, S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am. J. Sports Med. 2001, 29, 196–200. [Google Scholar] [CrossRef]
- Dunn, W.R.; Spindler, K.P.; MOON Consortium. Predictors of Activity Level 2 Years after Anterior Cruciate Ligament Reconstruction (ACLR): A Multicenter Orthopaedic Outcomes Network (MOON) ACLR Cohort Study. Am. J. Sports Med. 2010, 38, 2040–2050. [Google Scholar] [CrossRef]
- Roos, H.; Ornell, M.; Gardsell, P.; Lohmander, L.S.; Lindstrand, A. Soccer after anterior cruciate ligament injury—An incompatible combination? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. Acta Orthop. Scand. 1995, 66, 107–112. [Google Scholar] [CrossRef]
- Donnelly, C.J.; Elliott, B.C.; Ackland, T.R.; Doyle, T.L.A.; Besier, T.F.; Finch, C.F.; Cochrane, J.L.; Dempsey, A.R.; Lloyd, D.G. An anterior cruciate ligament injury prevention framework: Incorporating the recent evidence. Res. Sports Med. 2012, 20, 239–262. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Lindenfeld, T.N.; Riccobene, J.V.; Noyes, F.R. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am. J. Sports Med. 1999, 27, 699–706. [Google Scholar] [CrossRef]
- Mandelbaum, B.R.; Silvers, H.J.; Watanabe, D.S.; Knarr, J.F.; Thomas, S.D.; Griffin, L.Y.; Garrett, W., Jr. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am. J. Sports Med. 2005, 33, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Finch, C.F. No longer lost in translation: The art and science of sports injury prevention implementation research. Br. J. Sports Med. 2011, 45, 1253–1257. [Google Scholar] [CrossRef] [PubMed]
- Myklebust, G.; Engebretsen, L.; Braekken, I.H.; Skjolberg, A.; Olsen, O.E.; Bahr, R. Prevention of anterior cruciate ligament injuries in female team handball players: A prospective intervention study over three seasons. Clin. J. Sport Med. 2003, 13, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Junge, A.; Rosch, D.; Peterson, L.; Graf-Baumann, T.; Dvorak, J. Prevention of soccer injuries: A prospective intervention study in youth amateur players. Am. J. Sports Med. 2002, 30, 652–659. [Google Scholar] [CrossRef]
- Soderman, K.; Werner, S.; Pietila, T.; Engstrom, B.; Alfredson, H. Balance board training: Prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 356–363. [Google Scholar] [CrossRef]
- Steffen, K.; Myklebust, G.; Olsen, O.E.; Holme, I.; Bahr, R. Preventing injuries in female youth football—A cluster-randomized controlled trial. Scand. J. Med. Sci. Sports 2008, 18, 605–614. [Google Scholar] [CrossRef]
- Ntoumanis, N.; Ng, Y.Y.; Prestwich, A.; Quested, E.; Hancox, J.E.; Thøgersen-Ntoumani, C.; Deci, E.L.; Ryan, R.M.; Lonsdale, R.M.; Williams, G.C. A meta-analysis of self-determination theory-informed intervention studies in the health domain: Effects on motivation, health behavior, physical, and psychological health. Health Psychol. Rev. 2020, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Ntoumanis, N.; Quested, E.; Reeve, J.; Cheon, S.H. Need supportive communication: Implications for motivation in sport, exercise, and physical activity. In Persuasion and Communication in Sport, Exercise, and Physical Activity; Jackson, B., Dimmock, J.A., Compton, J., Eds.; Routledge: Abingdon, UK, 2018; pp. 155–169. [Google Scholar]
- Teixeira, P.J.; Marques, M.M.; Silva, M.N.; Brunet, J.; Duda, J.; Haerens, L.; La Guardia, J.; Lindwall, M.; Londsdale, C.; Markland, D.; et al. Classification of techniques used in self-determination theory-based interventions in health contexts: An expert consensus study. Motiv. Sci. 2019. [Google Scholar] [CrossRef]
- Robinson, M.A.; Donnelly, C.J.; Vanrenterghem, J.; Pataky, T.C. Sagittal plane knee kinematics predict non-sagittal knee joint moments in unplanned sidestepping. In Proceedings of the XXV Congress of the International Society of Biomechanics, Glasgow, UK, 12–16 July 2015. [Google Scholar]
- Donnelly, C.J.; Elliott, B.; Lloyd, D.G.; Reinbolt, J.A. Optimizing Whole body Kinematics to minimize valgus knee loading during sidestepping: Implications for ACL injury risk. J. Biomech. 2012, 45, 1491–1497. [Google Scholar] [CrossRef] [PubMed]
- Morgan, K.; Donnelly, C.J.; Reinbolt, J.A. Elevated Gastrocnemius Forces Compensate for Decreased Hamstrings Forces during the Weight-Acceptance Phase of Single-Leg Jump Landing: Implications for Anterior Cruciate Ligament Injury Risk. J. Biomech. 2014, 47, 3295–3302. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Pataky, T.C.; Vanrenterghem, J.; Robinson, M.A. Zero- vs. one-dimensional, parametric vs. non-parametric, and confidence interval vs. hypothesis testing procedures in one-dimensional biomechanical trajectory analysis. J. Biomech. 2015, 48, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Delp, S.L.; Anderson, F.C.; Arnold, A.S.; Loan, P.; Habib, A.; John, C.T.; Guendelman, E.; Thelen, D.G. OpenSim: Open-source software to create and analyze dynamic simulations of movement. IEEE Trans. Biomed. Eng. 2007, 54, 1940–1950. [Google Scholar] [CrossRef]
- Krosshaug, T.; Nakamae, A.; Boden, B.P.; Engebretsen, L.; Smith, G.; Slauterbeck, J.R.; Bahr, R. Mechanisms of anterior cruciate ligament injury in basketball: Video analysis of 39 cases. Am. J. Sports Med. 2007, 35, 359–367. [Google Scholar] [CrossRef]
- Cochrane, J.L.; Lloyd, D.G.; Buttfield, A.; Seward, H.; McGivern, J. Characteristics of anterior cruciate ligament injuries in Australian football. J. Sci. Med. Sport 2007, 10, 96–104. [Google Scholar] [CrossRef]
- Teixeira, P.; Marques, M.M.; Silva, M.N.; Brunet, J. A Classification of Motivation and Behavior Change Techniques Used in Self- Determination Theory-Based Interventions in Health Contexts. Motiv. Sci. 2020. [Google Scholar] [CrossRef]
- Keyworth, C.; Epton, T.; Goldthorpe, J.; Calam, R.; Armitage, C.J. Acceptability, reliability, and validity of a brief measure of capabilities, opportunities, and motivations (“COM-B”). Br. J. Health Psychol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Knittle, K.; Heino, M.; Marques, M.M. The compendium of self-enactable techniques to change and self-manage motivation and behaviour v.1.0. Nat. Hum. Behav. 2020, 4, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Weir, G.; Alderson, J.; Elliott, B.C.; Lee, S.; Devaprakash, D.; Starre, K.; Cooke, J.; Goodman, C.; Armstrong, J.; Jackson, B.; et al. A two-year biomechanically informed ACL injury prevention program in female field hockey players. Transl. J. Am. Coll. Sports Med. 2019, 4, 206–214. [Google Scholar]
- Staynor, J.M.D.; Nicholas, J.C.; Weir, G.; Alderson, J.A.; Donnelly, C.J. Targeting associated mechanisms of anterior cruciate ligament injury in female community-level athletes. Sports Biomech. 2017, 16, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, C.J.; Elliott, B.C.; Doyle, T.L.A.; Finch, C.F.; Dempsey, A.R.; Lloyd, D.G. Changes in muscle activation following balance and technique training and a season of Australian football. J. Sci. Med. Sport 2015, 18, 348–352. [Google Scholar] [CrossRef]
- Donnelly, C.J.; Elliott, B.C.; Doyle, T.L.A.; Finch, C.F.; Dempsey, A.R.; Lloyd, D.G. Changes in knee joint biomechanics following balance and technique training and a season of Australian football. Br. J. Sports Med. 2012, 46, 917–922. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donnelly, C.J.; Jackson, B.S.; Gucciardi, D.F.; Reinbolt, J. Biomechanically-Informed Training: The Four Pillars for Knee and ACL Injury Prevention Built Upon Behavior Change and Motivation Principles. Appl. Sci. 2020, 10, 4470. https://doi.org/10.3390/app10134470
Donnelly CJ, Jackson BS, Gucciardi DF, Reinbolt J. Biomechanically-Informed Training: The Four Pillars for Knee and ACL Injury Prevention Built Upon Behavior Change and Motivation Principles. Applied Sciences. 2020; 10(13):4470. https://doi.org/10.3390/app10134470
Chicago/Turabian StyleDonnelly, Cyril J., Ben S. Jackson, Daniel F. Gucciardi, and Jeff Reinbolt. 2020. "Biomechanically-Informed Training: The Four Pillars for Knee and ACL Injury Prevention Built Upon Behavior Change and Motivation Principles" Applied Sciences 10, no. 13: 4470. https://doi.org/10.3390/app10134470
APA StyleDonnelly, C. J., Jackson, B. S., Gucciardi, D. F., & Reinbolt, J. (2020). Biomechanically-Informed Training: The Four Pillars for Knee and ACL Injury Prevention Built Upon Behavior Change and Motivation Principles. Applied Sciences, 10(13), 4470. https://doi.org/10.3390/app10134470





