1. Introduction
The healthcare sector, particularly hospitals, faces a critical environmental challenge in managing waste from daily clinical activities [
1,
2]. This waste, more complex and dangerous than urban waste, includes contaminated materials, expired drugs, and specialized equipment.
Healthcare waste is defined as all waste generated by healthcare facilities, including hospitals, outpatient clinics, laboratories, medical and veterinary practices, pharmacies, and research centers, regardless of its hazardous nature [
3]. Approximately 85% of healthcare waste is classified as non-hazardous—mainly plastics, paper, glass, and metals—while the remaining 15% consists of hazardous materials, which may be infectious, toxic, or radioactive [
4]. In high-income countries, hazardous waste production can reach 11 kg/bed/day, compared to 6 kg/bed/day in low-income countries, where lack of segregation often results in underestimation of the actual hazardous fraction [
5].
Production is steadily increasing and contributes 4.4% to global greenhouse gas emissions [
6]. The COVID-19 pandemic has exacerbated this problem, increasing single-use waste and boosting emissions by 10% [
4,
7]. For instance, in Wuhan, healthcare waste generation increased from 40 tons/day in the pre-pandemic period to approximately 240 tons/day at the peak of the emergency, while in Bangladesh, around 14,500 tons of healthcare waste were generated in April 2020 alone [
5].
Hospital waste management generally follows three phases: internal collection and separation, transportation, and final treatment, using color-coding systems [
8,
9]. According to the WHO, general waste containers should be black, sharps and infectious waste yellow, and chemical/pharmaceutical waste brown, with segregation at the point of generation being the most critical step for safety [
5,
10]. Despite well-defined regulatory protocols, significant operational difficulties persist, and the application of circular economy principles—reduction, reuse, recycling—remains limited. Transitioning to a circular approach could reduce environmental impact, but there is a lack of practical and integrated tools that enable hospital environmental managers to apply these principles in daily waste management [
11].
Several tools are available to address these challenges: the WHO’s Health-care Waste Management Rapid Assessment Tool [
12], the digital checklist provided by SafetyCulture [
13], the use of standardized checklists to optimize waste management [
14], practical guidelines compliant with current regulations such as those by Sharpsmart [
15], automated systems based on Support Vector Machine (SVM) techniques to classify waste generated during the COVID-19 pandemic [
16], and integrated solutions that combine sensors, smart containers, genetic algorithms, and explainable artificial intelligence (XAI) to optimize routes and provide real-time analysis [
17].
However, there is a lack of a practical and integrated tool that allows hospital environmental managers to concretely apply the principles of the circular economy to the daily management of waste. This gap limits the ability to translate theory into sustainable actions, hindering effective reduction, reuse, and recycling of healthcare materials. Current systems are often designed mainly to produce documentation for environmental compliance, such as registers, reports, and forms. Their primary function is to meet formal reporting obligations. This limitation arises from the lack of integrated platforms that can connect environmental data with clinical and logistical information. Such platforms could provide managers with concrete operational guidance—for example, indicating which materials to recycle first, where to act to reduce waste, or how to plan environmental improvement measures. The absence of this decision-making support is a major barrier to implementing circular economy strategies in practice.
Our tool distinctly stands out from existing approaches, which primarily focus on document verification or waste volume measurement, by offering concrete operational support. It enables the rapid identification of critical issues in waste management, providing clear, updated, and reliable data. It supports environmental managers in performing targeted checks through a smart, simple, and practical tool to evaluate all critical aspects. A key innovation lies in the integration of ML-based analysis, which assigns quantitative importance to each action. This data-driven approach supports evidence-based prioritization and enhances the strategic planning of waste management interventions. Specifically, the tool uses a Random Forest classifier to evaluate the relative impact of 55 corrective actions, grouped across 13 thematic areas, on regulatory compliance and sustainability goals. The model estimates importance scores for each action based on the structural contribution of each variable to the overall classification process. These scores enable the tool to rank actions by their strategic relevance, guiding environmental managers to focus on the most effective interventions. By translating complex data into clear priorities, the system facilitates informed decision-making, continuous monitoring, and the planning of sustainable waste management strategies aligned with circular economy and Zero-Waste principles.
This study proposes an AI-Driven Circular Waste Management Tool designed for the circular management of hospital waste. The system is based on the latest developments in AI applied to document management and regulatory compliance in regulated sectors [
18,
19,
20,
21,
22]. In this study, we transform qualitative regulatory actions into structured variables and quantify their strategic weight through ML models. This approach enables environmental managers to clearly identify which actions have the greatest impact, facilitating more effective operational planning aligned with the principles of the circular economy. Furthermore, through evaluation models, it helps determine whether the corrective actions taken are genuinely improving the situation. It allows for continuous monitoring of results, ensuring that procedures comply with laws and respect the environment. In this way, the tool facilitates more effective and integrated decision-making, considering not only regulations but also the environmental, health, and organizational impacts. Through simulated case studies, we demonstrate how the AI-Driven Circular Waste Management Tool can improve operational sustainability, ensure regulatory compliance, and effectively implement the principles of the circular economy and the Zero-Waste strategy in hospital waste management.
1.1. Literature Review and Formulation of Research Questions
The scientific literature confirms that the management of hospital healthcare waste represents one of the main environmental and health challenges, particularly in low- and middle-income countries, where infrastructure and regulations often fail to ensure safe management, increasing the risk of exposure for personnel and communities [
23].
This waste includes non-biodegradable materials that persist in the environment, contaminating soil, water, and air, and contributing to the spread of microplastics and nanoplastics [
2,
24,
25]. Inadequate disposal processes, such as uncontrolled incineration, generate toxic substances such as dioxins and furans, while improper management of expired drugs can contaminate aquifers and promote antimicrobial resistance [
6,
9,
23,
26,
27]. Specific categories, such as cytotoxic waste, pose additional complexity due to their toxic impact and difficult degradability [
28,
29]. Infectious and sharp waste carries pathogenic microorganisms, chemical waste can cause intoxication, and radioactive waste is genotoxic, potentially affecting genetic material. Improper handling of pharmaceutical waste contaminates water systems [
5].
To address these challenges, healthcare facilities are increasingly exploring circular economy models as an alternative to traditional linear waste management. These models promote the reuse, repair, and recycling of materials, thereby extending the life cycle of healthcare products and reducing overall waste generation [
11,
30]. A common framework guiding these efforts is the 5Rs rule—reduce, reuse, recycle, rethink, and research—which provides a structured approach to maximize practical benefits while minimizing waste [
31]. A common framework guiding these efforts is the 5Rs rule—reduce, reuse, recycle, rethink, and research—which provides a structured approach to maximize practical benefits while minimizing waste [
32,
33,
34]. Complementary strategies—often cost-neutral or even cost-saving—include conducting regular waste audits, digitalizing paper-based directives, limiting device use to necessary situations, and training staff to prevent waste misclassification [
31]. Building on these principles, the Zero-Waste model emphasizes complete waste elimination through the integrated application of refuse, reduce, reuse, recycle, and rot strategies [
6]. However, despite the potential benefits, the practical adoption of circular and Zero-Waste approaches in hospitals remains limited: one study found that only 25% of the analyzed devices applied at least one circular strategy, and only one-third of these adopted more than one [
35].
The widespread implementation of such practices is hindered by regulatory, cultural, and economic barriers, despite international experiences demonstrating their feasibility [
36,
37]. Despite attention to environmental sustainability, insufficient funding (72%), lack of mandate (64%), and scarce knowledge (60%) are barriers to applying environmentally sustainable practices. The creation of an ’environmental greening team’ to increase knowledge, improve attitudes, and facilitate the success of green initiatives is suggested [
31].
1.2. Research Gaps and Key Questions
The literature highlights significant gaps in the practical translation of the theoretical principles of the circular economy in healthcare facilities contexts. Among the main issues are the following:
Hospital environmental managers lack concrete operational tools to implement specific circular models for departments, operating rooms, and specialized services [
38].
Regulatory divergences and internal cultural resistance among healthcare personnel hinder the adoption of sustainable practices [
5,
38,
39].
The emerging technologies and Life Cycle Assessment (LCA) tools are not integrated sufficiently to evaluate the environmental impact of adopted solutions [
40].
The lack of standardized guidelines and protocols for the sustainable management of healthcare waste is classified as a critical regulatory issue that hinders the adoption of effective, consistent, and safe practices within healthcare facilities. This absence is particularly serious because it prevents the establishment of standardized methods to identify specific problems and plan corrective actions within the circular waste management system. For example, hospitals often lack tools capable of identifying which department or process contributes most to regulatory risk or environmental impact, making it difficult to set intervention priorities and allocate resources efficiently [
41].
Based on this evidence, this study aims to answer three research questions:
RQ1: How can the principles of the circular economy and the Zero-Waste strategy be translated into specific operational practices for healthcare waste management in healthcare facilities?
RQ2: How can an AI-driven tool support hospital environmental managers in identifying problems in departments and planning corrective actions?
RQ3: What is the effectiveness of an intelligent tool in guiding sustainable management choices and improving regulatory and environmental compliance in healthcare facilities?
RQ4: How can a dynamic digital tool, integrated into a platform, contribute to continuous improvement in healthcare waste management?
This study proposes an AI-Driven Circular Waste Management Tool for enhancing circular economy practices in healthcare facilities, designed as an operational decision-support system that integrates principles of the circular economy and Zero-Waste with advanced data analysis techniques. The tool enables the following:
Identifying the main environmental issues in hospital contexts.
Defining measurable indicators for monitoring sustainable performance.
Associating operational actions derived from regulations and best practices.
Quantifying the importance of actions using machine learning (ML) algorithms.
Supporting management choices based on empirical evidence and optimizing intervention priorities.
We illustrate the system through simulated case studies, demonstrating its potential effectiveness in improving operational sustainability and environmental compliance in healthcare facilities. It offers an innovative, data-driven contribution to bridging the gap between theory and practice in hospital waste management. Specifically, our innovative approach does not rely on introducing entirely new variables. It integrates well-known variables into a hierarchical model (theme–indicator–action) and quantifies their importance using supervised machine learning (Random Forest). This method preserves the individual contribution of each variable even when interactions occur, allowing for effective prioritization of corrective actions. This data-driven framework bridges the gap between theory and practice in hospital waste management, offering a structured, transparent, and adaptable tool for diverse healthcare contexts.
Finally, in this context, we applied AI in two key ways. We employed a supervised ML model to analyze a simulated dataset derived from the qualitatively extracted actions. This enabled the identification and prioritization of the most impactful actions on regulatory compliance. Second, we used Chat-GPT-5 [
42], a large language model (LMM), to optimize and improve the front-end user interface code, enhancing readability. Furthermore, all data, analyses, and quantitative validation were developed independently, using traditional manual analysis methods and supervised ML.
2. Materials and Methods
The construction of the AI-Driven Tool proposed in this study followed a systematic approach. We based this approach on the qualitative and structured extraction of strategic information from specific documentary material concerning the management of healthcare waste and the application of circular economy principles in the healthcare sector. We articulated the methodological process in several sequential and integrated phases to define a multidimensional compliance tool, oriented not only towards regulatory compliance but also towards environmental sustainability, safety, and management innovation.
2.1. Source Selection and Content Extraction
We divided the sources used for the development of the smart tool into thematic sections, encompassing a variety of regulatory texts, guidelines, and scientific contributions. These included international frameworks, European Union (EU) regulations and directives, national regulations, and guidelines. Scientific contributions covered a range of topics, including the impact of healthcare waste on the environment and public health, the benefits and challenges of reusable medical devices, and innovative technologies for waste treatment and management. The scientific studies also explored the implications of the COVID-19 pandemic on waste production and management, the role of digital tools and AI in optimizing waste management processes, and the importance of adopting sustainable practices like recycling and the use of biodegradable materials.
For a detailed list of sources and their descriptions, refer to
Table A1 in
Appendix A. These sources serve as the qualitative foundation of our study. They were selected to extract strategic, regulatory, and operational insights concerning healthcare waste management and the application of circular economy principles in the sector. The extracted concepts formed the knowledge base from which structured variables were created for use in the AI model. The sources are thematically organized in the appendix (e.g., Principles of the Circular Economy, Environmental Impact of the Healthcare Sector, Waste Management Practices, International Projects). Each entry includes the reference number, section title, and a concise description of the content. These references correspond to the bibliography at the end of the manuscript. All documents are publicly accessible: regulatory texts can be retrieved from institutional websites such as EUR-Lex for EU legislation or national legal portals, while scientific contributions are available through academic databases.
Specifically, regarding sources on the environmental and health impacts of hospital waste, we examined the WHO reports [
4,
9,
23], which highlight the risks associated with inadequate waste management, such as infections, antibiotic resistance, and environmental contamination [
23]. We also reviewed studies on pharmaceutical contaminants affecting water and soil quality [
28,
29,
43], and the exacerbation of waste production and CO
2 emissions during the COVID-19 pandemic was documented [
7,
44,
45]. Regarding sources on Zero-Waste and circular economy strategies in healthcare, we considered contributions from Bea Johnson [
46,
47,
48] and Paul Connett [
49], who outlined the theoretical basis of the Zero-Waste philosophy, and Hoveling et al. [
35], who reported operational barriers to circularity and traceability in a study on over 1400 medical devices. We also reviewed data on the application of Extended Producer Responsibility (EPR) policies in the EU, USA, and Japan [
50], along with successful case studies from Gundersen Health System and the Cleveland Clinic [
36,
37]. We analyzed studies on emerging technologies and LCA approaches, focusing on the use of IoT and blockchain for medical waste traceability [
40,
51], as well as on advanced treatment techniques such as pyrolysis, cold plasma, and gasification [
52,
53]. We integrated contributions on the growing application of LCA in healthcare [
54] and examined innovative start-ups like Recircula Solutions and Rubicon Global that are developing digital platforms for integrated waste management [
55]. Furthermore, we reviewed some EU directives [
56] and national regulatory frameworks [
57] relevant to the sector.
We conducted data extraction through manual qualitative analysis. Specifically, we systematically analyzed each section of the documentary material to identify key concepts, regulatory obligations, operational strategies, and management issues. We then organized the extracted concepts into a structured scheme. The operational phases of the process were as follows:
Systematically read each reference section.
Identified relevant content, manually selecting concepts applicable to the practical management of healthcare waste.
Extracted and organized the content by theme, associated indicators, and operational actions.
Performed cross-validation to ensure consistency and regulatory alignment between the extracted information and sector best practices.
2.2. Identification of the AI-Driven Circular Waste Management Tool Components
Each extracted concept was categorized into a three-tier structure: (a) themes, (b) indicators, and (c) actions.
Themes represent the main ideas or central topics discussed in the texts. For example, if a section focuses on “reducing waste production,” the theme identified would be “waste prevention.” Themes serve as broad categories grouping related concepts, indicators, and actions addressing the same overall issue. The identification of a theme involves (i) summarizing the core message of a text section; (ii) organizing the information clearly and systematically; and (iii) pinpointing the key topics or concerns addressed by the source. Recurring ideas and key concepts across the texts guided the definition of these themes.
Indicators are the measurable criteria or metrics used to monitor progress or performance related to each theme. They are derived by analyzing the text for quantitative data, regulatory references, or qualitative assessments. Indicators can be the following:
- –
Quantitative: numerical values such as waste volume or percentage reduction.
- –
Normative: compliance with laws, standards, or regulations.
- –
Qualitative: subjective characteristics, like training quality, which cannot be directly measured numerically.
Actions consist of concrete practices or interventions proposed in the sources to address each theme and improve waste management. For example, linked to the theme “waste prevention” and the indicator “reduction of waste generated,” an action could be “prioritize reusable medical devices over single-use items.” Actions reflect practical solutions grounded in regulatory requirements and best practices identified in the literature.
Table A2, presented in full in
Appendix B, summarizes the themes, indicators, and actions extracted through the analysis described above. It represents the operational translation of the information gathered from the analyzed sources, organized into the three-tier structure (themes–indicators–actions) and constitutes the qualitative foundation on which the development of the proposed tool is based.
To test the robustness and operational relevance of the qualitative framework described above, we developed a simulated case study for quantitative validation. We translated the 55 identified actions into variables and created a synthetic dataset representing hypothetical healthcare facilities with varying levels of regulatory compliance. Each facility’s responses simulate different degrees of implementation for each action. Using this dataset, we applied a supervised ML approach to identify which actions most strongly influence overall compliance performance. This step allowed us to move from qualitative structuring to data-driven prioritization, supporting decision-makers in targeting the most impactful areas for intervention.
2.3. Quantitative Validation: Variable Importance Analysis
We performed a quantitative validation of the structured framework of actions by assessing the compliance levels of simulated healthcare facilities with current Waste Management Regulations, based on synthetic data. An interpretable ML model is used in this analysis to identify which actions have the greatest impact on overall compliance levels [
58,
59,
60,
61].
Based on the 55 actions identified in the qualitative analysis, we simulated healthcare facility responses grouped into 13 thematic categories, each representing different aspects required by the regulations, such as separate collection, waste reduction, training, and so forth. Specifically, for each action, healthcare facilities provide a qualitative assessment of the implementation status (Done, Partially implemented, Under implementation, and Not yet implemented), which is then converted into the following numerical values: 1, 0.5, 0.25, and 0, respectively. These actions constitute the input variables for our analysis. We designed this linear scale to preserve the ordinal nature of the responses while allowing us to compute a meaningful aggregate score across actions. For each healthcare facility, we calculated a total compliance score as the sum of the scores obtained on individual responses. This score reflects the degree of compliance with the actions required by the regulations. To facilitate interpretation and modeling, the total score was transformed into a categorical variable Y with three levels: Low (score < 22); Medium (score < 26); and High (score < 26). We chose the thresholds empirically based on the distribution of the score variable. They correspond approximately to the first (22.25) and third (25.75) quartiles. This approach creates segmentation consistent with the empirical distribution of the data and meaningful for the analysis. The Medium class represents the most frequently observed situation, i.e., healthcare facilities that are partially but not fully compliant. The Low and High classes represent, respectively, facilities that have implemented few measures and those that show high levels of compliance. This classification reflects the practical variability in implementation levels among facilities and supports a more nuanced interpretation of the results.
The simulated dataset includes 5000 observations (i.e., healthcare facilities), distributed as shown in
Table 1.
Such a distribution avoids significant class imbalance and enables building a more robust predictive model.
After designing the case study, we trained a classification ML model—Random Forest—and subsequently conducted an importance analysis to identify which actions most significantly influence the level of compliance [
62,
63,
64]. We selected Random Forest among several interpretable models, such as logistic regression, decision trees, and gradient boosting, because it delivers strong predictive and classification performance, resists overfitting, and handles a large number of inputs while modeling complex, nonlinear relationships and interactions among variables. These characteristics make it widely adopted across domains and particularly suitable for our context, where multiple interdependent factors may drive compliance. The importance measures derived from the ML model provide variable importance scores, allowing us to identify which actions most strongly influence compliance classification. These insights support prioritization in training, audits, and policy interventions. Specifically, we used the Mean Decrease Gini coefficient, which quantifies how much each input contributes to reducing node impurity in decision trees. This coefficient is a model-dependent measure because it derives directly from the internal structure and training process. It is less sensitive to fluctuations in predictive performance and more consistent in reflecting how the model uses each variable for classification. Compared to model-independent methods, Mean Decrease Gini is computationally efficient because it does not require retraining or repeated evaluations. It captures the structural contribution of each variable to the classification process and is not directly influenced by predictive accuracy on test data. This is an advantage when the goal is to understand the model’s decision structure rather than validate predictive performance. In our case, which involves identifying and classifying the most relevant actions to support priority setting in training, review, and policy interventions, Mean Decrease Gini provides a practical and interpretable summary of overall importance. To ensure comparability, we normalized the importance estimates globally across all variables to range between 0 and 1 and sorted them in descending order (see
Figure 1). This process facilitates easier comparison and interpretation of the results across different thematic areas.
The ranking in
Figure 1 enables quickly identifying which actions contribute most to distinguishing between “Low,” “Medium,” and “High” classes and setting operational priorities: actions identified as more important by the model deserve more attention, monitoring, or detailed analysis.
Based on the distribution of importance values, we group the actions into three classes using the corresponding first and third quartiles.
Highly Important Actions: importance above the third quartile, contributing significantly above average.
Moderately Important Actions: between the first and third quartiles, with average contribution.
Slightly Important Actions: below the first quartile, with lower influence on the model.
This categorization identifies 14 highly important actions, 27 moderately important actions, and 14 slightly important actions. This helps decision makers focus more concretely on the highly important actions—which are crucial for implementing interventions and setting priorities in healthcare waste management—while monitoring the other actions of moderate or slight importance.
As a result of this analysis,
Table A2 also includes the importance values for each action. These importance scores are calculated relative to the thematic category to which each action belongs, thereby reflecting the contribution of each action within its specific theme.
The results of the variable importance analysis directly informed the architecture and logic of the digital tool. We used the ranking of actions—classified into high, moderate, and low importance—to organize the structure and interaction flow of the AI-Driven Circular Waste Management Tool. In the following section, we present the implementation of this tool, which incorporates the thematic structure, action prioritization, and monitoring system derived from the previous analyses.
2.4. The AI-Driven Circular Waste Management Tool Implementation
We propose a system that has an interactive software interface developed in React, designed for direct use by operators and managers of healthcare waste management. The application is user-facing and offers several features, including a thematic checklist with indicators and corrective actions. Additionally, it allows for the assignment of priorities, calculated based on importance scores, and the recording of progress statuses, dates, notes, and evaluations of the indicators. We optimized the front-end code during the development of the user interface prototype by using ChatGPT-5, a large language model (LLM) developed by OpenAI (San Francisco, CA, USA) and released in August 2025 [
42]. Thereby, the use of the LLM allows us to improve the readability, responsiveness, and efficiency of the user interface.
Structure
The AI-Driven Circular Waste Management Tool is structured into three main elements.
- –
AI-Driven Tool Overview.
The header displays the tool’s title and a progress bar that dynamically reflects the overall completion status of the actions.
- –
Thematic Sections.
The tool presents thematic areas (e.g., regulatory compliance, waste prevention, etc.), each represented by a distinct card component. Within each section,
- *
The system lists the actions in descending order of importance (see
Section 2.3).
- *
For each action, the interface displays the description, a priority indicator, a specific progress bar, and the current status for each action.
- –
Detail Card.
Users can expand each action through a modal interface: progress status (selectable from a drop down menu), dates (start, deadline, expected completion), associated indicators, and textual annotations.
Interaction Workflow
The interface guides the user through a logical sequence of operations, which are described below.
- –
The user accesses a structured set of areas, each containing environmental indicators and an ordered list of priority actions. Actions are classified based on their strategic relevance.
- –
For each action, the user selects the implementation status (e.g., completed, partially started, ongoing, not yet started) and enters complementary information such as start dates, deadlines, and operational notes. A qualitative contribution on the associated indicators is also requested.
- –
The system immediately records every modification the user makes. Data is stored locally, ensuring work continuity even without an internet connection or after closing the interface.
- –
The status of the actions contributes to the calculation of a synthetic indicator of overall progress, expressed as a percentage. This value considers the completion degree of all selected actions, allowing for a quantitative assessment of progress.
- –
Visual elements accompany each action to facilitate the understanding of the current status: progress bars, priority labels, and buttons to access editing modules. The system provides real-time feedback that supports the decision-making process.
- –
The user can revisit each action at any time to update data, review entered information, or adjust deadlines, promoting a virtuous cycle of control, adaptation, and optimization.
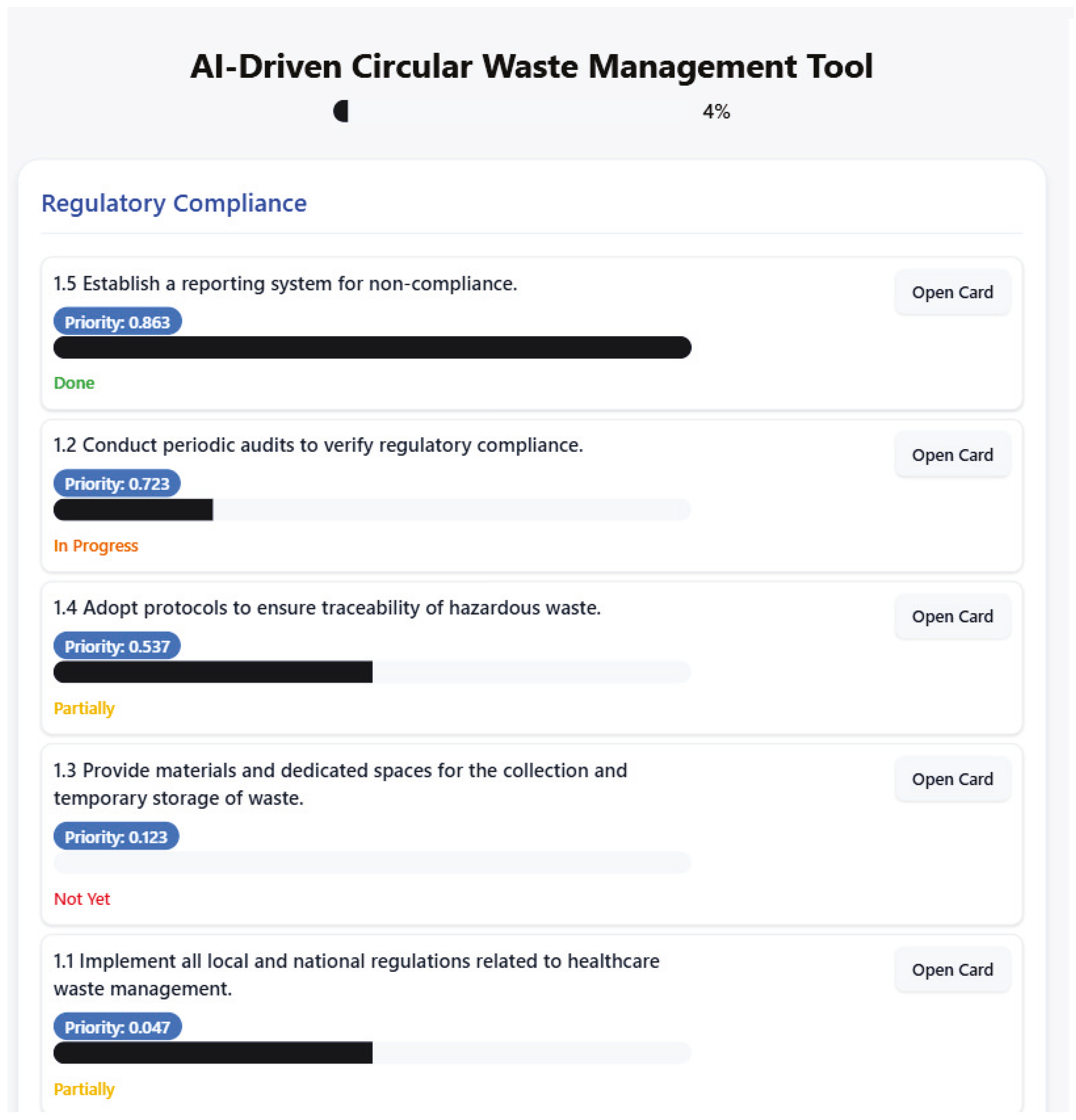
Figure 2 shows a user interface of an AI-Driven Circular Waste Management Tool prototype.
The interface features a progress indicator at the top, signaling a 4% completion rate and providing an immediate perception of the overall status of activities. The section dedicated to regulatory compliance includes a set of tasks aimed at ensuring alignment with current regulations on healthcare waste management.
Each activity is accompanied by a priority score, indicating its relative importance within the system, and a status indicator, useful for monitoring its execution level.
The first task involves establishing a reporting system for non-compliance and has a priority of 0.863, the highest in the section. This task is marked as “Done,” indicating it has been completed. The second task involves conducting periodic audits to verify regulatory compliance and has a priority of 0.723. This task is currently “In Progress”, showing that it is actively being addressed. The third task, which involves adopting protocols to ensure the traceability of hazardous waste, has a priority of 0.537 and is “Partially” completed. The fourth task involves providing materials and dedicated spaces for the collection and temporary storage of waste. This task has a priority of 0.123 and is marked as “Not Yet” started. Finally, the fifth task involves implementing all local and national regulations related to healthcare waste management. This task has a priority of 0.047 and is “Partially” completed. Each activity is equipped with an “Open Card” button, allowing users to access detailed information or perform specific actions related to the task. By clicking the “Open Card” button, users can manage tasks effectively. The status of each task is indicated, providing insight into its current progress. The start date and deadline for these tasks are not specified in the image, but placeholders suggest that specific dates have not yet been set. The expected completion dates are also not provided in the image. The card includes a section labeled “Indicators,” which lists compliance with environmental and safety laws. This indicates that the tasks are focused on ensuring adherence to specific regulations or standards. Additionally, there is a section for the “number of detected non-compliance,” which is currently empty, suggesting that it is intended to track non-compliance issues but none have been recorded yet.
The tool helps end users clearly understand the importance of various factors influencing waste management. It communicates the importance of variables through an automatically calculated priority score displayed next to each recommended action. The tool orders actions in descending order of relevance, placing higher-impact interventions at the top of the list. The interface uses visual elements such as progress bars, status indicators, and thematic groupings to enhance readability. This setup acts like a simplified dashboard, enabling hospital managers to quickly identify critical areas, monitor progress, and allocate resources efficiently. By linking the importance of each input variable to specific operational recommendations, the tool translates analytical output into practical decisions, supporting the planning of targeted interventions that address the most urgent waste management issues first.
This prioritization in the interface is the direct outcome of the tool’s decision-support process. When the input of a case is known—that is, the theme it belongs to and the relevant data or indicators—the process for identifying the recommended corrective actions unfolds as follows. First, we identify the relevant theme from the case input, determining which area of healthcare waste management it refers to (for example, regulatory compliance or waste prevention). Next, for each theme, the tool lists the available corrective actions, ranked by their importance, which defines the intervention priority. Actions with higher importance scores represent the top recommendations to resolve or improve the specific situation. Through the user interface, we can explore each action in detail by opening its dedicated “card,” which displays its implementation status, relevant dates, specific indicators to monitor, and additional notes. This functionality helps contextualize each action within the specific case and supports monitoring its implementation. By knowing the input of a case, the tool enables us to pinpoint the corresponding theme and access the corrective actions ranked by priority, thereby providing targeted and effective recommendations. This operational approach makes healthcare waste management more structured, transparent, and data-driven, supporting informed and goal-oriented decision-making.
3. Results
Although we have not yet applied the AI-Driven Circular Waste Management Tool in real contexts, we constructed simulated case studies for illustrative purposes in this work. These examples demonstrate how the tool functions in practice and highlight its potential utility in supporting decisions related to the circular management of healthcare waste.
For each simulated case study, we began with a qualitative assessment to identify operational, managerial, or regulatory deficiencies. Each deficiency was then formulated as a clear, verifiable statement and mapped to one of the predefined themes in the AI-Driven Circular Waste Management Tool (e.g., regulatory compliance, waste separation, monitoring and traceability). Once the relevant theme was identified, the tool’s knowledge base was used to retrieve all associated corrective actions. These actions were then filtered to retain only those directly pertinent to the specific conditions of the case. The selected actions were subsequently evaluated based on their importance scores, calculated through a Random Forest model trained on simulated compliance datasets. Actions with an importance score ≥ 0.5 were prioritized, while lower-scoring measures were included only when strictly necessary to address specific operational or regulatory gaps. By combining thematic analysis with quantitative scoring, this approach allows a single issue to span multiple areas (for example, “lack of disposal records” relates to both regulatory compliance and monitoring and evaluation). When a management issue arises, the system presents the set of relevant corrective actions together with their respective importance scores, enabling users to identify high-impact measures while also incorporating lower-scoring but contextually critical interventions. This process supports the creation of cross-cutting, tailored solutions that integrate immediate operational fixes with strategic, long-term improvements, with importance scores serving as evidence-based guidance rather than rigid prescriptions.
Case Study no. 1
In the intensive care unit of Hospital X, which has 10 high-intensity care beds, the production of infectious waste has significantly increased compared to the previous year. The staff operates in continuous shifts, with a constant flow of critical patients and intensive use of disposable materials.
The staff on duty informally manages waste, without following written procedures or relying on designated responsible individuals. They dispose of waste in generic containers, which lack distinguishable colors or coding. The unit does not display visual indications for waste separation, nor does it post signs identifying collection or temporary storage areas. The facility does not maintain an internal register to track the quantity or types of waste disposed of. Staff members carry out collection and disposal activities based on orally transmitted practices, without oversight or verification from the health management. The institution has not provided the staff with specific training on the subject, and no one has clearly assumed the role of contact person for waste management.
From the case study, we identify the following critical issues related to waste management:
- –
Input:
- *
Significant increase in infectious waste compared to the previous year.
- *
Absence of separate containers for hazardous and non-hazardous waste.
- *
Absence of an internal monitoring system for waste separation and traceability.
- *
Absence of visual signs, posters, or operational instructions in the unit.
- *
No register for the quantity or types of waste produced.
- *
No identified responsible person for waste management.
- *
Staff not trained and lacking written procedural guidelines.
- *
Management based on non-standardized oral practices.
- *
High risk of exposure and regulatory non-compliance.
To integrate the importance of actions and indicate how these impact the case study of the Intensive Care Unit at Hospital X, we can use out system to implement specific actions.
Appendix C contains
Table A3 showing the recommended actions to implement and their importance values.
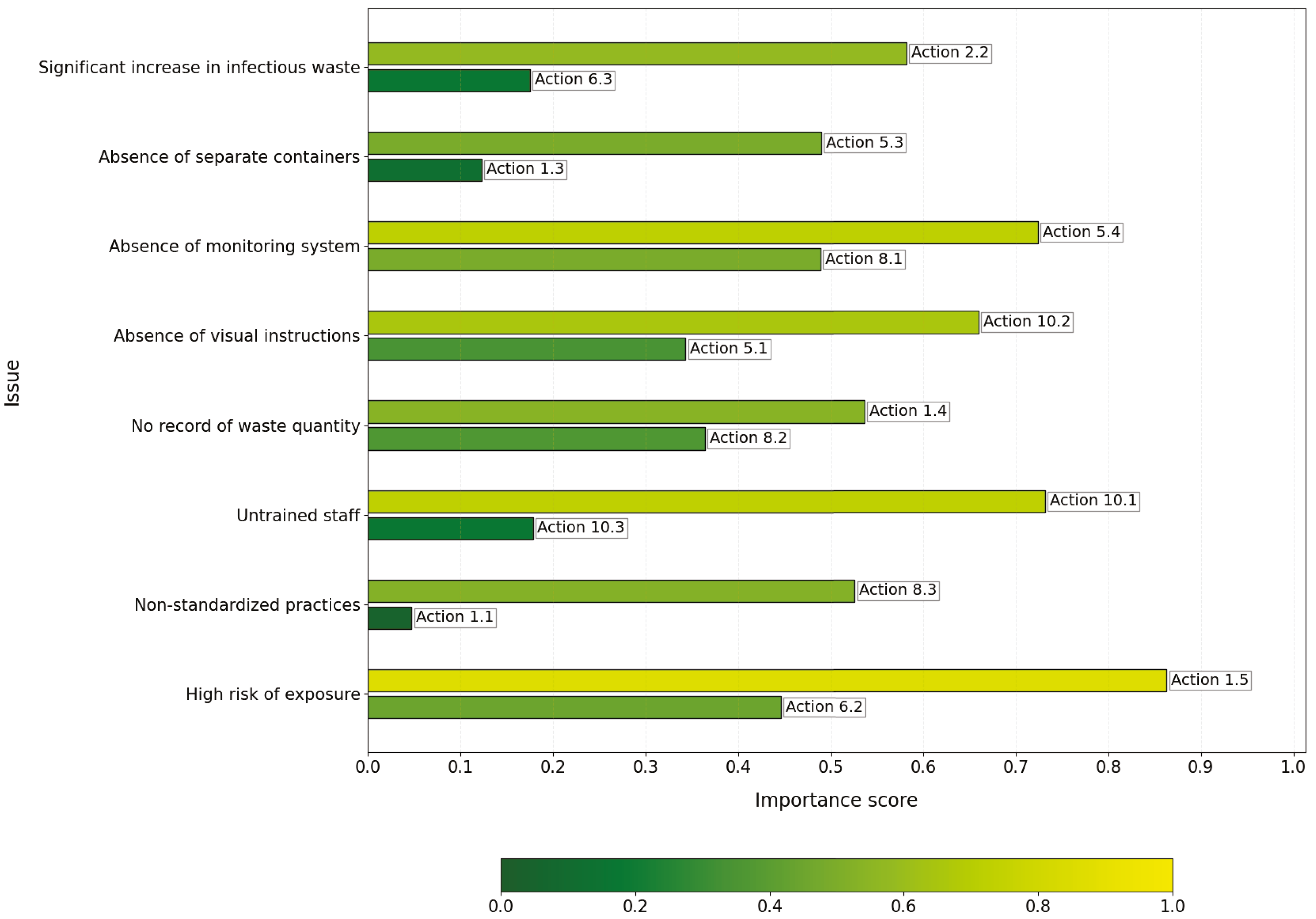
Figure 3 shows the corrective actions recommended by our tool.
Most choices are based on the importance score. However, we do not use criteria in some cases. For the issue “Significant increase in infectious waste,” even though action 6.3 has a lower importance score, it is considered more relevant for specifically addressing the management of infectious waste, so it remains a priority. For the issue “Absence of separate containers,” action 1.3 was retained despite its low score because the dedicated space effectively supports segregation. For the issue “Absence of visual signs,” priority was given to action 10.2 (awareness) because creating awareness is often more urgent before implementing detailed operational instructions. For “Management based on oral practices,” action 8.3 (effectiveness monitoring) has a higher priority than 1.1 (regulations) because measuring effectiveness is a more immediate operational step to improve the situation, even though compliance is fundamental.
Case Study no. 2
In the internal pharmaceutical service of a medium-sized hospital, staff have adopted a consolidated but inadequate practice for managing expired drugs, systematically disposing of them in containers intended for infectious risk sanitary waste. Currently, the facility lacks a specific and separate system for collecting and disposing of pharmaceutical waste, whether hazardous or non-hazardous. This indiscriminate handling of discontinued drugs violates current regulations on sanitary and hazardous waste management.
Staff manage expired drugs without using dedicated containers specifically coded for such waste, including cytostatic and cytotoxic substances. Moreover, the facility does not maintain a formal register documenting withdrawal, temporary storage, or disposal activities, which prevents any form of traceability. Operational units act independently of the pharmacy service, proceeding with disposal without following any shared protocol. This lack of coordination leads to the mixing of infectious and hazardous chemical waste, undermining both the safety of final treatment and the correct classification of waste.
Furthermore, the hospital has not implemented written procedures or posted visible operational instructions for differentiated pharmaceutical waste management. Healthcare and technical personnel rely on long-standing but informal and unvalidated practices, which increases the risk of operational errors and potential sanctions during inspections by the competent authorities. Finally, the management does not carry out internal control activities or provide specific training: it has not recorded any internal audits or refresher courses for the involved personnel, thereby limiting both risk awareness and the adoption of proper procedures.
From the case study, we identify the following issues related to waste management:
- –
Input
- *
Absence of dedicated and coded containers for the collection of expired drugs and cytotoxic/cytostatic waste.
- *
Lack of a formal register to document disposal operations.
- *
Uncoordinated disposal between operational units and the pharmacy service.
- *
Mixing of infectious waste and hazardous chemical waste, with the risk of contamination and problems in final treatment.
- *
Absence of written procedures or visible instructions for the differentiated management of pharmaceutical waste.
- *
Management entrusted to non-formalized internal practices, lacking validation.
- *
Lack of internal audit activities to monitor operational practices.
- *
Absence of specific training and updating of healthcare and technical personnel.
Appendix C includes
Table A4 showing the recommended actions to implement and their importance values.
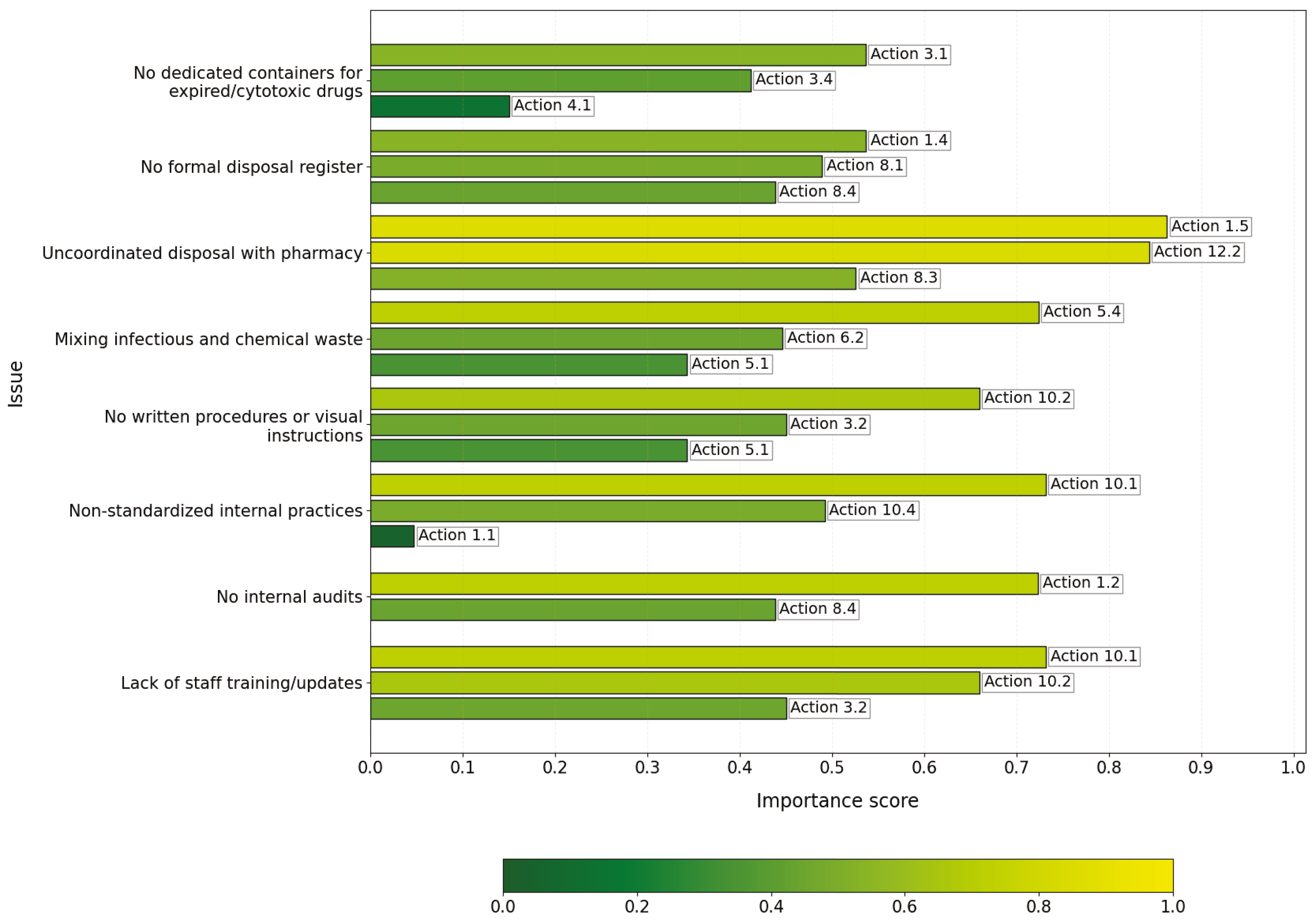
Figure 4 reports the corrective actions recommended by our tool.
The importance criterion guided most choices. However, we integrated this criterion with the assessment of regulatory criticality and functional coverage in two situations. We selected action 4.1 because we considered it essential for complying with legal obligations. Action 5.1 has a medium–low score, but it addresses the complete absence of written procedures and visual instructions, a direct critical issue in the case study. We chose action 5.3 because the main problem was the absence of dedicated and coded containers for expired drugs and cytotoxic substances. Action 3.2 does not have the highest score, but it is fundamental because, in this case, there is a complete lack of specific training, leading to high operational risk. We included action 8.3, despite its medium value, because the problem indicated an absence of records and traceability, necessitating the introduction of a minimum system of indicators to start monitoring. Finally, we included complementary actions to close an operational gap. Sometimes, combining only high-scoring actions did not cover all aspects of the issue. Therefore, we inserted low-scoring actions as a “complement” to cover a weak point, such as the lack of signage or the absence of written procedures, which, despite having a low score, significantly impacts operational risk.
Case Study no. 3
Over the past six months, a public hospital introduced new national waste tracking software to comply with current regulatory provisions, including the implementation of an electronic waste register. The system digitally manages the entire cycle of healthcare waste—from production to disposal—by tracking European Waste Catalog (EWC) codes, hazard levels, and the operational unit of origin.
However, the implementation of this new tool revealed significant operational and managerial issues. Specifically, staff increased the classification of waste as hazardous by 30%, not because of actual changes in healthcare processes but due to categorization errors. Their excessive use of “hazardous” codes—often driven by caution or interpretative uncertainty—disrupted disposal logistics, slowed down execution, and raised overall costs.
Staff encountered practical difficulties while using the system. They took longer to enter data, frequently made saving errors, and often failed to correctly record loading and unloading dates. These issues caused misalignment in workflows and delays in daily operations. Furthermore, many operational units failed to fully integrate the new software with existing management practices. They continued to rely on a hybrid paper–digital system, which duplicated processes and increased the risk of information loss. Staff still used paper forms as references or support tools, resulting in an uncoordinated overlap with the digital system.
Finally, there is a lack of structured and continuous training for the involved operators. From the case study, we identify the following issues related to waste management:
- –
Input
- *
Incorrect classification of waste with a 30% increase in hazardous waste.
- *
Improper attribution of EWC codes due to excessive caution or regulatory uncertainty.
- *
Increase in costs and slowdown of logistics operations.
- *
Operational difficulties in using the software.
- *
Loading and unloading dates.
- *
Misalignment in information flows and daily processes.
- *
Poor integration of the software with pre-existing procedures.
- *
Persistence of a hybrid paper–digital management.
- *
Risk of information loss and duplication of activities.
- *
Absence of a unified and coordinated procedure between systems.
- *
Inadequate or absent training for the involved personnel.
- *
Poor knowledge of regulations and waste classification criteria.
In
Appendix C,
Table A5 shows the recommended actions to implement and their importance values.
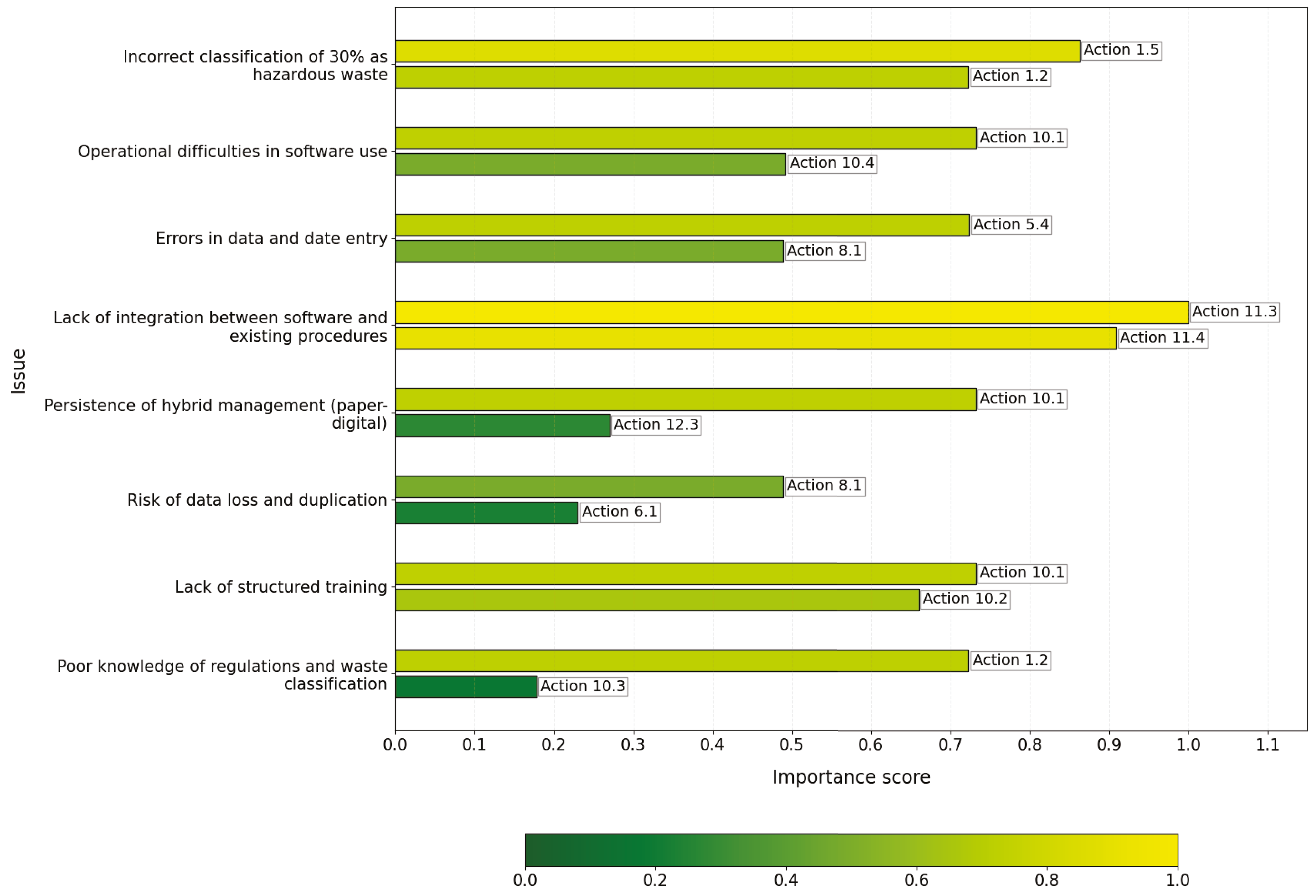
Figure 5 illustrates the corrective actions recommended by our tool.
We primarily selected actions based on a balance between the numerical importance score and operational relevance in the specific context. For instance, we chose high-importance actions, such as action 1.5, because they provide essential monitoring to quickly detect and correct critical errors like the misclassification of hazardous waste. We included some actions with lower importance scores but high contextual relevance, such as action 6.1 “Adopt technologies to monitor waste flows”. Although its priority score is low, it supports precise monitoring necessary in cases of data loss risk. We consistently prioritized training-related actions, such as action 10.1, because proper staff competence is fundamental to solving operational difficulties and reducing errors across multiple issues. In some cases, we selected strategic or enabling actions with very high importance, like action 11.3, despite them not being immediately operational due to their critical role in integrating complex systems and future-proofing waste management.
Case Study no. 4
A hospital is currently evaluating the purchase and installation of an internal sterilizer to treat infected healthcare waste. The hospital launched this initiative to reduce the costs associated with external disposal—including transportation and treatment at authorized facilities—and to strengthen its autonomy in managing the healthcare waste supply chain.
The administration has included the project within a broader ecological transition strategy adopted at the strategic level. In this framework, the hospital views internal sterilization as a viable solution to lower its overall environmental impact, aligning with the principles of the circular economy promoted by the EU [
65], the Best Available Techniques (BAT) for waste treatment [
66], and current national regulations.
However, the facility has not integrated the digital waste traceability system (already in use) with the sterilizer. Specifically, the system does not enable interoperability between the data generated during sterilization cycles and the national monitoring software, making it difficult to automate the information flow and ensure full traceability of operations.
Moreover, the hospital has not provided specific technical training to the healthcare and technical staff responsible for daily operations, maintenance, and validation of sterilization cycles. This lack of training is particularly critical, as the effectiveness of the treatment depends heavily on the proper application of procedures and familiarity with control protocols.
Lastly, the hospital has not conducted an LCA to scientifically compare the environmental impact of internal waste management with the current outsourced model. This missing analysis prevents the hospital from accurately estimating the potential environmental benefits of the investment and may hinder both decision-making and authorization processes.
From the case study, we identify the following issues related to waste management:
- –
Input
- *
Lack of integration between the sterilizer and the digital waste traceability system (absence of interoperability between treatment cycle data and the software).
- *
Difficulty in ensuring complete traceability of operations due to the lack of automation in the information flow.
- *
Absence of specific technical training for healthcare and technical staff responsible for the management, maintenance, and validation of the sterilizer.
- *
Risk of treatment inefficacy due to incorrect use of technology and failure to apply control protocols.
- *
Lack of an LCA assessment to estimate and compare the environmental impact of internal treatment versus outsourced treatment.
- *
Difficulty in supporting strategic choices and authorization requests for the introduction of the new technology with objective data.
In
Appendix C,
Table A6 illustrates the recommended actions to implement and their importance values.
Figure 6 reports the corrective actions recommended by our tool.
In some cases, the selection was guided exclusively by the numerical importance score because the specific operational relevance and practical effectiveness of the action in the described context were carefully evaluated. For example, actions with low priority scores were chosen because they represent fundamental steps or essential prerequisites for the proper management of the issue. Specifically, action 6.1 was selected as it is a critical step to ensure complete traceability of waste flows, especially after the sterilization process. Similarly, action 10.3 was chosen because providing updated, multidisciplinary training enables healthcare and technical staff to correctly use new technologies and adhere to procedures, thereby reducing the risk of errors that could compromise treatment effectiveness. Furthermore, the urgency and strategic role of certain actions were considered. For instance, action 11.4, although not an immediate operational intervention, is crucial for integrating complex systems and improving management in the medium to long term.
4. Discussion
The application of the healthcare waste management tool across the four case studies demonstrated its capacity to automate processes and integrate data from multiple sources, thereby facilitating continuous monitoring of activities. The tool’s importance measures actively guide decision-making by directing resources toward high-impact actions. A further strength lies in its adaptability to hospitals of varying sizes, resource availability, and organizational complexity.
While the numerical importance scores provide a crucial quantitative foundation to prioritize actions and ensure resources focus on the most impactful interventions, the case studies reveal that these values are complemented by careful consideration of operational context and specific criticalities. In certain instances, actions with lower importance scores were prioritized because they addressed fundamental prerequisites or urgent contextual needs, such as ensuring traceability after sterilization (action 6.1) or raising staff awareness (action 10.2). Conversely, high-importance actions were consistently selected when they represented strategic enablers, like system integration (action 11.3) or rigorous monitoring (action 1.5). This nuanced approach enhances the practical effectiveness of the tool, balancing quantitative prioritization with real-world applicability.
The results from the four case studies directly address the initial research questions.
RQ1: How can the principles of the circular economy and the Zero-Waste strategy be translated into specific operational practices for healthcare waste management in healthcare facilities? The data indicate that hospitals can translate circular economy and Zero-Waste principles into concrete operational practices focused on prevention, reuse, recycling, and traceability. Specifically, hospitals have reduced the use of single-use materials by introducing reusable devices and implementing waste-to-energy processes. They have also leveraged software tools to continuously monitor waste streams and maintain digital records, enhancing control capabilities and making sustainability progress measurable.
RQ2: How can an AI-driven tool support hospital environmental managers in identifying problems in departments and planning corrective actions? The case studies show that environmental managers actively use the tool—equipped with dynamic features and weighted measures—as an operational guide. They systematically assess departmental compliance and identify intervention priorities. By integrating the tool with tracking software, managers can plan targeted corrective actions, design customized training programs, and standardize protocols, thus minimizing errors and subjective interpretation.
RQ3: What is the effectiveness of an intelligent tool in guiding sustainable management choices and improving regulatory and environmental compliance in healthcare facilities? The results confirm that the compliance tool effectively supports both regulatory adherence and sustainability-oriented organizational change. The digital system provides detailed operational instructions that encourage best practices and enable automated control processes. Hospitals using the tool report increased operational efficiency, more rational resource use, and improved internal transparency. Moreover, the tool facilitates LCA analyses, which further inform strategic decisions regarding in-house or outsourced waste treatment.
RQ4: How can a dynamic digital tool, integrated into a platform, contribute to continuous improvement in healthcare waste management? The platform drives continuous and adaptive improvement by collecting real-time data, generating automated reports, and suggesting corrective measures. Its flexibility allows healthcare facilities of diverse sizes and organizational structures to implement it effectively.
A promising strategic evolution for the healthcare waste management tool lies in its integration with additive manufacturing (AM) and smart manufacturing platforms, enabling upstream interventions that directly address the root causes of waste generation. By connecting waste management data with production planning, hospitals could request the on-demand fabrication of specific devices—such as reusable surgical trays—only when required. This approach reduces storage costs, prevents overproduction, and supports a circular supply chain in which products are manufactured, used, and reintroduced into the system through reuse or recycling. The COVID-19 crisis illustrated the value of such integration: redesigning and 3D-printing ventilator components enhanced supply resilience while reducing waste [
67]. By incorporating life-cycle data—covering device longevity, reuse cycles, and end-of-life outcomes—the tool could provide feedback to product designers, fostering the development of durable, high-performance devices. Specific indicators could then measure the impact of AM adoption, including reductions in waste materials, procurement times, and supply vulnerabilities. This broader application positions the tool as a strategic enabler for systemic change toward healthcare sustainability. Procurement choices could be informed by detailed analyses of waste quantities, types, and sources, guiding investments towards durable, reusable, and standardized medical devices. Such evidence-driven decisions also facilitate the definition of shared operational standards and encourage long-term adoption of sustainable technologies.
At its current stage, the tool primarily serves an operational role, focusing on the regulatory and practical aspects of healthcare waste management. It monitors thematic indicators—such as regulatory compliance, waste prevention, medication management, safety, and recycling—through checklists covering management practices, training, monitoring, and control. Progress is tracked manually, classifying actions as “Done” or “In Progress,” with reporting centered on indicators and operational achievements. While these functionalities already deliver efficiency gains and improve resource allocation, their integration with upstream design and manufacturing strategies would allow the tool to fully realize its potential as both a compliance mechanism and a driver of circular economy principles.
5. Conclusions
This study introduced and validated, through four simulated case studies, a digital tool to support healthcare waste management in healthcare facilities. The system combines operational guidance with priority indicators to support decision-making. The results show that it can help hospitals adopt safer, more efficient, and more sustainable practices while ensuring regulatory compliance and aligning with circular economy principles and the Zero-Waste strategy.
The approach, based on a flexible digital platform and priority-based indicators, offers practical support for improving the environmental and operational performance of waste management. It encourages waste reduction and promotes practices consistent with EU policies and the SDGs.
This study has some limitations that should be acknowledged. First, the case studies were developed under idealized conditions, characterized by stable operations, readily available data, and the capacity to apply corrective actions. In real-world scenarios, implementation may face significant challenges, such as staff resistance, limited integration with existing digital systems, or constrained financial and human resources.
A second limitation concerns the regulatory framework embedded in the tool. While it is based on shared general rules, it does not account for specific national or regional regulations. To ensure full compliance, users must manually adapt the tool to reflect the laws and rules of the jurisdiction in which it is deployed, as the current version does not include automated mechanisms for detecting or applying local requirements. Although the tool is adaptable, this adjustment step is essential and places a greater responsibility on the end user.
Language and localization represent an additional challenge. The current version is available only in English and may require translation and contextual adaptation for non-English-speaking users or for deployment in diverse operational environments.
From an operational standpoint, the tool supports many processes but does not fully automate waste management. Critical tasks such as interpreting data, planning interventions, and supervising implementation require the active involvement of qualified personnel, particularly environmental or waste managers. In the current implementation, the tool automates the organization and prioritization of actions based on predefined indicators and importance scores. It supports users in data monitoring and progress visualization. Human control remains essential, particularly in choosing the most appropriate action for the specific case. In critical situations, users can evaluate various proposed corrective actions, each associated with an importance indicator. Users have the freedom to select an action with a lower score if they deem it more suitable. They can exclude actions with higher scores if they consider them irrelevant. The system facilitates informed decisions without imposing rigid choices. It allows room for expert judgment and contextualization. Therefore, the tool supports many processes but does not fully automate waste management. Key activities such as data interpretation, intervention planning, and implementation supervision still require the involvement of qualified personnel, particularly environmental or waste managers. Human oversight remains crucial for adapting the tool’s recommendations to the specific needs of each facility.
Scalability and transferability also remain to be validated. The system’s performance in healthcare settings with limited digital infrastructure (e.g., small rural hospitals) or in non-European contexts may be constrained by differences in regulatory frameworks, operational capacity, and resource availability. Although the core methodology is adaptable, localized customization will be necessary to ensure both legal compliance and functional effectiveness.
Finally, data interoperability poses a significant limitation. Integrating the tool with heterogeneous hospital information systems—such as electronic medical records (EMRs) or enterprise resource planning (ERP) platforms—can be challenging due to the lack of common data standards and dedicated application programming interfaces (APIs). These constraints may hinder information exchange and automatic data updates, ultimately limiting the efficiency of the system.
Future work will focus on real-world testing in hospitals, involving staff and environmental managers directly. This will help assess its practical effectiveness, measure economic sustainability, and understand its impact on daily operations. Planned improvements include adding features for predicting waste flows and generating reports to support audits and environmental monitoring, with the goal of making the tool even more useful across different regulatory and organizational settings. Real-world tests will adopt user-centered design principles. They will include participatory design approaches. They will involve co-development with environmental managers. They will encompass usability studies. This approach will ensure that the tool fully meets operational needs. It will integrate effectively into daily workflows.
Planned functional enhancements include the addition of predictive modules for waste flow forecasting and automated reporting tools to support environmental audits and ongoing monitoring. These features will improve traceability, simplify compliance procedures, and reduce the administrative burden on staff. A key milestone will be the development of a smart module for automatic regulatory adaptation. By enabling the system to detect and apply relevant legal requirements based on geographical and institutional context, this feature will enhance scalability and reduce the risk of non-compliance across diverse regulatory environments.
Another development direction involves extending the system’s scope upstream to incorporate Design for Circularity principles [
68]. This will include decision-support features for procurement, allowing the selection of products based on durability, reparability, and recyclability, alongside the introduction of sustainability rating systems for suppliers.
Furthermore, future work will explore adapting the proposed tool for use in non-hospital healthcare facilities—such as clinics and long-term care centers—which generate significant waste but face distinct organizational and infrastructural constraints. Tailored configurations will be developed to address these specific contexts.
Finally, efforts will be made to enhance the interpretability and transparency of the AI models underpinning the tool. This will involve integrating complementary interpretability techniques—such as SHAP values, permutation importance, and variance-based methods—to provide deeper insights at both the global and local levels. In parallel, the adoption of more complex AI architectures will be investigated to improve predictive performance and generate additional, actionable insights from the data.