Exposure to Airborne Contaminants and Respiratory Health Among Lithium Mine Workers in Western Australia
Abstract
1. Introduction
2. Materials and Methods
2.1. Settings
2.2. Study Population
2.3. Exposure Assessment
2.4. Health Monitoring for the Determination of Health Effects
2.5. Statistical Analysis
3. Results
3.1. Exposure Assessment
3.2. Sample Population Characteristics
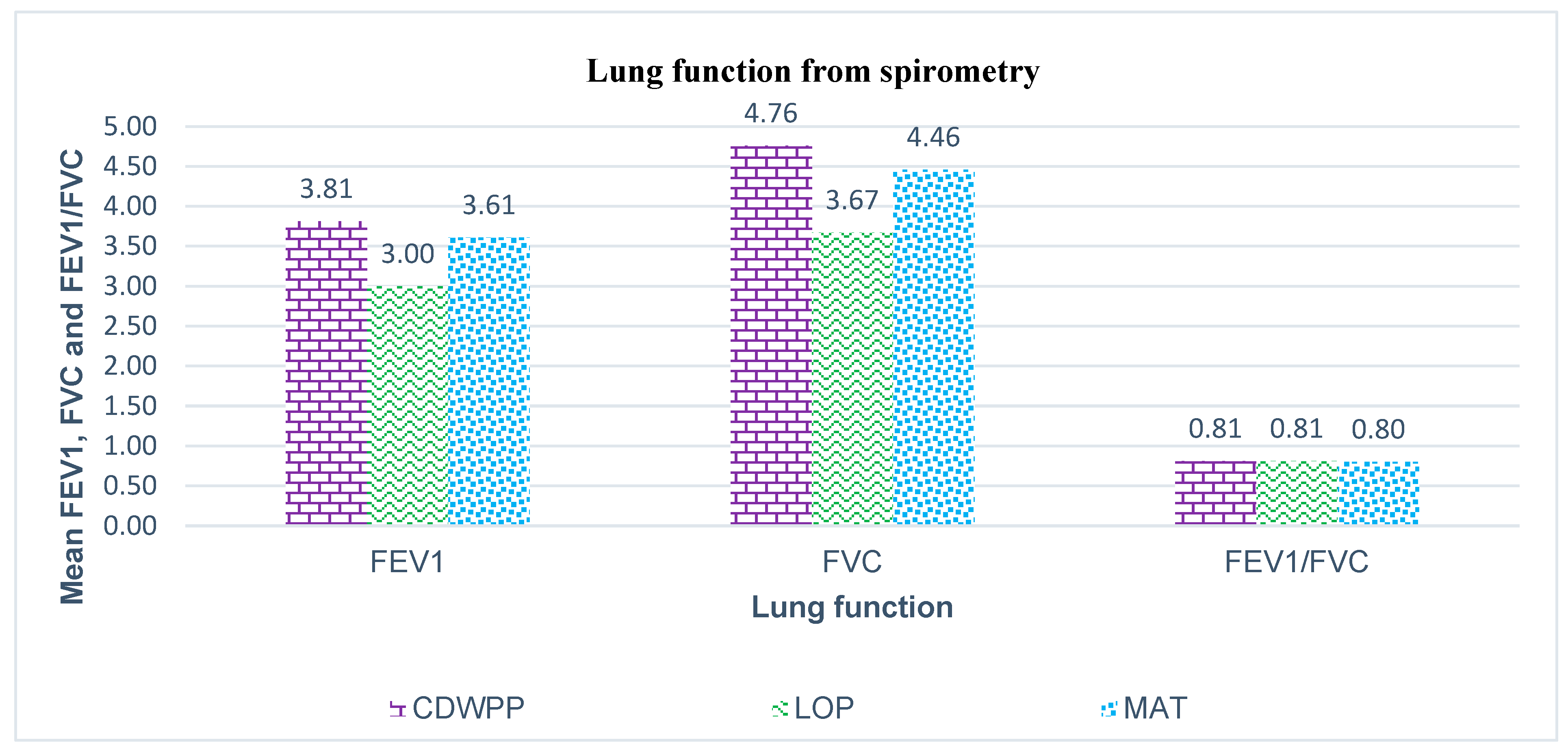
3.3. Lung Function and Respiratory Symptoms
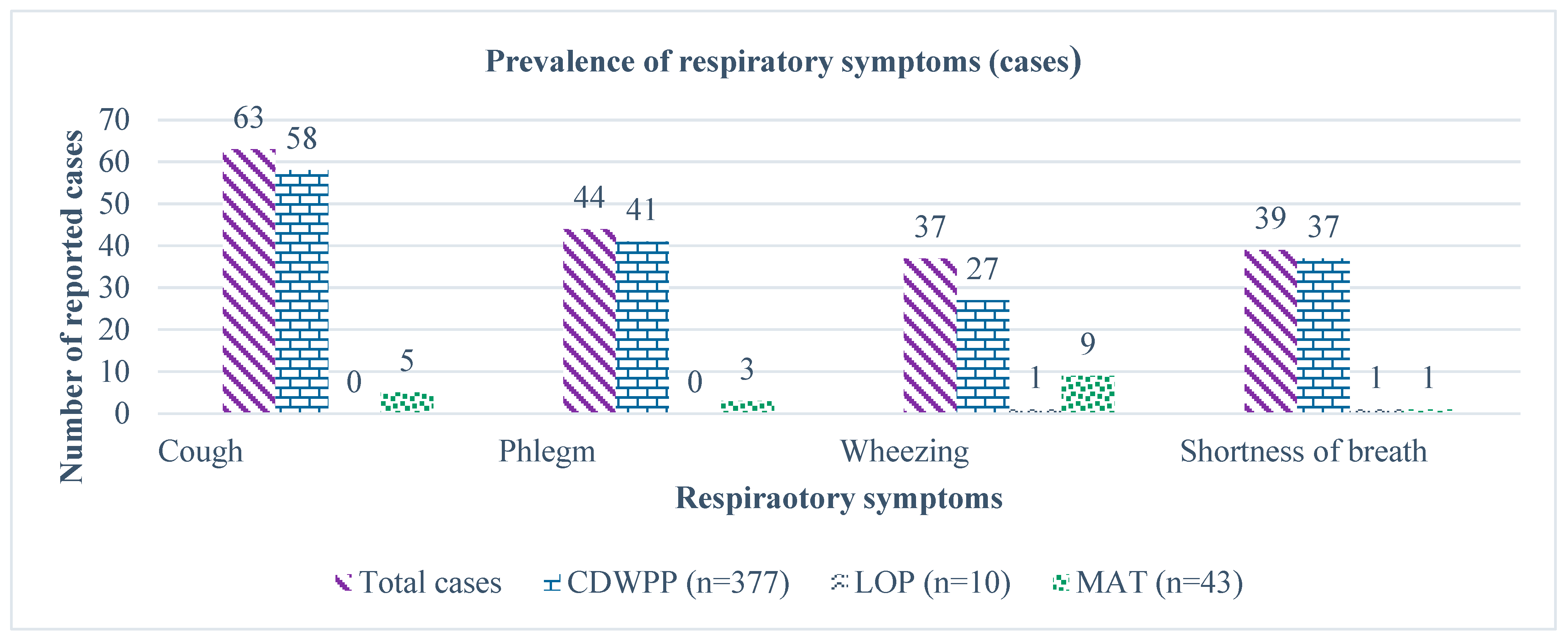
3.4. Prevalence of Respiratory Symptoms and Respiratory Health Determination
3.5. Factors Associated with Miner’s Health Status Revealed by the Multivariable Linear and Logistic Regression Models
4. Discussion
4.1. Exposures, Respiratory Airflow Limitations and Respiratory Symptoms
4.2. Silicosis and Its Global Emergence
4.3. Training and Respiratory Protection Use in Lithium Mining
4.4. Risk Factors for Respiratory Ill Health in Lithium Mining
4.5. The Impact of Smoking on Respiratory Health and Smoking Cessation
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Won, E.; Kim, Y.-K. An Oldie but Goodie: Lithium in the Treatment of Bipolar Disorder through Neuroprotective and Neurotrophic Mechanisms. Int. J. Mol. Sci. 2017, 18, 2679. [Google Scholar] [CrossRef] [PubMed]
- Bojja, S.L.; Singh, N.; Kolathur, K.K.; Rao, C.M. What is the Role of Lithium in Epilepsy? Curr. Neuropharmacol. 2022, 20, 1850–1864. [Google Scholar] [CrossRef] [PubMed]
- Wietelmann, U.; Klett, J. 200 Years of Lithium and 100 Years of Organolithium Chemistry. J. Inorg. Gen. Chem. 2018, 644, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Saaid, F.I.; Kasim, M.F.; Winie, T.; Elong, K.A.; Azahidi, A.; Basri, N.D.; Yaakob, M.K.; Mastuli, M.S.; Shaffee, S.N.A.; Zolkiffly, M.Z.; et al. Ni-rich lithium nickel manganese cobalt oxide cathode materials: A review on the synthesis methods and their electrochemical performances. Heliyon 2024, 10, e23968. [Google Scholar] [CrossRef]
- Opitz, A.; Badami, P.; Shen, L.; Vignarooban, K.; Kannan, A.M. Can Li-Ion batteries be the panacea for automotive applications? Renew. Sustain. Energy Rev. 2017, 68, 685–692. [Google Scholar] [CrossRef]
- Evans, R. Lithium’s future supply, demand. North. Min. 2010, 96, 11–12. [Google Scholar]
- Azevedo, M.; Baczynska, M.; Hoffman, K.; Krauze, A. Lithium mining: How New Production Technologies Could Fuel the Global EV Revolution. 2022. Available online: https://www.mckinsey.com/industries/metals-and-mining/our-insights/lithium-mining-how-new-production-technologies-could-fuel-the-global-ev-revolution (accessed on 23 October 2023).
- Gbondo, D.; Zhao, Y.; Pham, M.; Rumchev, K. Trends in Exposure to Respirable Dust and Respirable Crystalline Silica Among Lithium Mine Workers in Western Australia. Saf. Health Work. 2024, 15, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, A. Occupational health hazards in mining: An overview. Occup. Med. 2004, 54, 283–289. [Google Scholar] [CrossRef]
- Gbondo, D.; Pham, M.; Zhao, Y.; Tsurikov, N.; Rumchev, K. Radioactivity and Exposure to Radiation in Lithium Mining in Western Australia. J. Hazard. Mater. Adv. 2025, 18, 100652. [Google Scholar] [CrossRef]
- Wippich, C.; Rissler, J.; Koppisch, D.; Breuer, D. Estimating Respirable Dust Exposure from Inhalable Dust Exposure. Ann. Work. Expo. Health 2020, 64, 430–444. [Google Scholar] [CrossRef]
- Habybabady, R.H.; Sis, H.N.; Paridokht, F.; Ramrudinasab, F.; Behmadi, A.; Khosravi, B.; Mohammadi, M. Effects of Dust Exposure on the Respiratory Health Symptoms and Pulmonary Functions of Street Sweepers. Malays. J. Med. Sci. 2018, 25, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Rumchev, K.; Hoang, D.; Lee, A. Exposure to dust and respiratory health among Australian miners. Int. Arch. Occup. Environ. Health 2023, 96, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Sepadi, M.M.; Chadyiwa, M.; Nkosi, V. Platnum Miner Workers’ Exposure to Dust Particles Emitted at Mine Waste Rock Crusher Plants in Limpopo, South Africa. Int. J. Environ. Res. Public Health 2020, 17, 655. [Google Scholar] [CrossRef]
- Mo-Yeol, K.; Jiyoun, J.; Jung-Wan, K.; Ihan, K.; Hyoung-Ryoul, K.; Jun-Pyo, M. Increased risk of gastric cancer in workers with occupational dust exposure. Korean J. Intern. Med. 2021, 36, S18–S26. [Google Scholar]
- Dhatrak, S.; Nandi, S. Assessment of silica dust exposure profile in relation to prevalence of silicosis among Indian sandstone mine workers: Need for review of standards. Am. J. Ind. Med. 2019, 63, 277–281. [Google Scholar] [CrossRef]
- Li, T.; Yang, X.; Xu, H.; Liu, H. Early Identification, Accurate Diagnosis, and Treatment of Silicosis. Can. Respir. J. 2022, 2022, 3769134. [Google Scholar] [CrossRef]
- Radnoff, D.; Todor, M.S.; Beach, J. Occupational Exposure to Crystalline Silica at Alberta Work Sites. Occup. Environ. Hyg. 2014, 11, 557–570. [Google Scholar] [CrossRef]
- Misra, S.; Sussell, A.L.; Wilson, S.E. Occupational exposure to respirable crystalline silica among US metal and nonmetal miners, 2000–2019. Am. J. Ind. Med. 2022, 66, 199–212. [Google Scholar] [CrossRef]
- Ozkaya, S.; Dirican, A.; Tuna, T. The objective evaluation of obstructive pulmonary diseases with spirometry. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 25, 2009–2015. [Google Scholar] [CrossRef]
- Lange, P.; Halpin, D.M.; O’Donnell, D.E.; MacNee, W. Diagnosis, assessment, and phenotyping of COPD: Beyond FEV1. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 11, 3–12. [Google Scholar]
- GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 2017, 5, 691–706. [Google Scholar] [CrossRef] [PubMed]
- Austin, E.K.; James, C.; Tessier, J. Early Detection Methods for Silicosis in Australia and Internationally: A Review of the Literature. Int. J. Environ. Res. Public Health 2021, 18, 8123. [Google Scholar] [CrossRef]
- McMahon, A. Silicosis: Here’s What You Need to Know About the Dust Lung Disease Killing Stonemasons. NEWS. 2018. Available online: https://www.abc.net.au/news/2018-10-12/what-is-the-dust-lung-disease-silicosis/10365604 (accessed on 17 June 2024).
- Australian Government, Department of Employment and Workplace Relations. Work Health and Safety and Workplace Relations Ministers’ Meeting—13 December 2023. Available online: https://www.dewr.gov.au/work-health-and-safety/resources/work-health-and-safety-and-workplace-relations-ministers-meeting-13-december-2023 (accessed on 17 June 2024).
- Government of Western Australia. Work Health and Safety (Mines) Regulations 2022. WALW—Work Health and Safety (Mines) Regulations 2022—Home Page. 2020. Available online: https://www.legislation.wa.gov.au/legislation/statutes.nsf/law_s53266.html (accessed on 7 March 2025).
- U.S. Department of Labor. Permissible Exposure Limits—Annotated Tables. Retrieved from Occupational Safety and Health Administration: Permissible Exposure Limits—Annotated Tables|Occupational Safety and Health Administration. Available online: https://www.osha.gov/ (accessed on 4 June 2025).
- Driscoll, P.T. Safe Work Australia. Deemed Diseases in Australia. 2015. Available online: https://www.safeworkaustralia.gov.au/resources-and-publications/reports/deemed-diseases-australia (accessed on 17 June 2024).
- Government of Western Australia. Department of Energy, Mines, Industry Regulation and Safety. Health Monitoring Guide for Registered Medical Practitioners: Silica (Respirable Crystalline). 2022. Available online: https://www.commerce.wa.gov.au/publications/health-monitoring-guide-registered-medical-practitioners-silica-respirable-crystalline (accessed on 12 March 2025).
- The Thoracic Society and New Zealand. Standards for the Delivery of Spirometry for Mine Workers. 2017. Available online: https://thoracic.org.au/ (accessed on 12 March 2025).
- Government of Western Australia. Health Surveillance Requirements for Silica Strengthened. Media Statements. 2021. Available online: https://www.wa.gov.au/government/media-statements/McGowan%20Labor%20Government/Health-surveillance-requirements-for-silica-strengthened-20210115 (accessed on 17 June 2024).
- Chen, C.H.; Tsai, P.J.; Chang, W.W.; Chen, C.Y.; Chen, C.Y.; Yates, D.; Guo, Y. Dose-response relationship between lung function and chest imaging response to silica exposures in artificial stone manufacturing workers. Environ. Health 2024, 23, 25. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H. Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 2019, 72, 558–569. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software, Release 18; StataCorp LLC: College Station, TX, USA, 2023.
- Ulvestad, B.; Bakke, B.; Eduard, W.; Kongerud, J.; Lund, M. Cumulative exposure to dust causes accelerated decline in lung function in tunnel workers. Occup. Environ. Med. 2001, 58, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Leso, V.; Fontana, L.; Romano, R.; Gervetti, P.; Iavicoli, I. Artificial Stone Associated Silicosis: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 568. [Google Scholar] [CrossRef]
- Mastrantonio, R.; Civisca, A.; Siciliano, E.; Inglese, E.; Lippolis, T.; Pompei, D.; Cococcetta, L.; Scatigna, M.; Fabiani, L. Exposure assessment to inhalable and respirable dust in the post—Earthquake construction sites in the city of l’Aquila. J. Occup. Health 2021, 63, e12296. [Google Scholar] [CrossRef]
- Wizner, K.; Nasarwanji, M.; Fisher, E.; Steege, A.L.; Boiano, J.M. Exploring respiratory protection practices for prominent hazards in healthcare settings. J. Occup. Environ. Hyg. 2018, 15, 588–597. [Google Scholar] [CrossRef]
- Li, Y.; Bakos-Block, C.; Rammah, A.; Magal, R.; Adekanye, J.; Esquenazi, S.; McDaniel, M.R.; Zhang, K.; Symanski, E.; Perkison, W.B. The Post Hurricane Harvey Respiratory Protection Training Program. J. Occup. Environ. Med. 2020, 62, 842–846. [Google Scholar] [CrossRef]
- Jain, S.; Dempsey, K.; Clezy, K.; Bradd, P. Implementation of a respiratory protection program within healthcare facilities during the COVID-19 pandemic—Lessons learned. Am. J. Infect. Control. 2022, 50, 1067–1069. [Google Scholar] [CrossRef]
- Marshall, H.M.; Vemula, M.; Hay, K.; McCaul, E.; Passmore, L.; Yang, I.A.; Bowman, R.V.; Fong, K.M. Active screening for lung cancer increases smoking abstinence in Australia. Asia. Pac. J. Clin. Oncol. 2023, 19, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; Li, X.; Wu, H.; Meng, Z.; Li, Y.; Pan, H.; Liang, H.; Wang, Y.; Zhao, F.-H.; Qiao, Y.; et al. The impact of low-dose CT on smoking behavior among non-smokers, and smokers: A population-based screening cohort in rural China. Cancer Med. 2023, 12, 4667–4678. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, W.; Stewart, T. Exposure Assessment in Occupational and Environmental Epidemiology; Nieuwenhuijsen, M., Ed.; Oxford University Press: New York, NY, USA, 2003; pp. 103–118. [Google Scholar]

| Workgroup | Occupations in Workgroup | Activities |
|---|---|---|
| MAT | Manager Mining Engineer Metallurgist Site Administrator Health & Safety Advisor Environment Advisor Occupational Hygienist Compliance Trainer Emergency Services Officer Medic Maintenance planner Facilities Technician Service Personnel Warehouse personnel | Safe and efficient operation of surface and process plant operations. Ensuring compliance with mining regulations. Overseeing scheduling, planning and budgeting. Planning, design and overseeing mining operations. Processing grade control. Management of health and safety, and environment. Emergency preparedness and response. Training and compliance tracking. Medical treatment. Maintenance planning. Facilities maintenance and management. Management of warehouse. |
| CDWPP | Fitter Electrician Process operator Boilermaker Mobile machine operator Maintenance personnel Control room operator Supervisor | Monitoring and adjusting the day-to-day operation of the plant. Undertaking inspections of the plant and carrying out maintenance. Clearing blockages from the crushing circuit. Conducting continuous monitoring of conveyors. Completing daily shift log. Completing general housekeeping duties. |
| LOP | Laboratory Technician Laboratory supervisor | Preparing samples. Weighing samples in balance room. Operating jaw crusher, pulverisers, shakers and riffle splitters. Sampling, reagent preparation and analysis. Quality control of data and reporting. |
| Sample Characteristics | Total (n = 430) | CDWPP (n = 377) | LOP (n = 10) | MAT (n = 43) |
|---|---|---|---|---|
| Age in years, mean ± SD | 41.41 ± 10.59 | 41.05 ± 10.63 | 49.90 ± 10.46 | 42.56 ± 9.51 |
| Age in years, n (%) | ||||
| <40 | 202 (46.98) | 180 (47.75) | 2 (20.00) | 20 (46.51) |
| ≥40 | 228 (53.02) | 197 (52.25) | 8 (80.00) | 23 (53.49) |
| Gender, n (%) | ||||
| Female | 32 (7.44) | 17 (4.51) | 5 (50.00) | 10 (23.26) |
| Male | 398 (92.56) | 360 (95.49) | 5 (50.00) | 33 (76.74) |
| Employment duration in years, median (IQR) | 2.40 (2.53) | 2.40 (2.45) | 6.10 (4.23) | 2.30 (2.90) |
| Employment duration in years, n (%) | ||||
| <10 | 418 (97.21) | 366 (97.08) | 10 (100.00) | 42 (97.67) |
| ≥10 | 12 (2.79) | 11 (2.92) | 0 (0.00) | 1 (2.33) |
| * Smoking, n (%) | ||||
| Current smoker | 95 (22.09) | 82 (21.75) | 3 (30.00) | 10 (23.26) |
| Ex smoker | 129 (30.00) | 116 (30.77) | 5 (50.00) | 8 (18.60) |
| Never smoked | 204 (47.44) | 177 (46.95) | 2 (20.00) | 25 (58.14) |
| * Existing respiratory condition, n (%) | ||||
| Yes | 144 (33.49) | 125 (33.16) | 9 (90.00) | 18 (41.86) |
| No | 286 (66.51) | 252 (66.84) | 1 (10.00) | 25 (58.14) |
| * Training and respiratory protection, n (%) | ||||
| Trained in airborne contaminants (yes) | 290 (67.44) | 254 (67.37) | 8 (80.00) | 28 (65.12) |
| Trained in respiratory protection use (yes) | 299 (69.53) | 261 (69.23) | 9 (90.00) | 29 (67.44) |
| Respiratory protection fit testing provided (yes) | 220 (51.16) | 195 (51.72) | 9 (90.00) | 16 (37.21) |
| Respiratory protection provided (yes) | 365 (84.88) | 324 (85.94) | 9 (90.00) | 32 (74.42) |
| Variable | FVC1 | FVC | FEV1/FVC | Cough | Phlegm | Wheezing | Shortness of Breath | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | n (%) | n (%) | n (%) | n (%) | |
| Age group (in years) | ||||||||||
| <40 | 4.14 ± 0.67 | 4.15 (0.90) | 5.10 ± 0.93 | 4.13 (1.23) | 0.82 ± 0.07 | 0.81 (0.07) | 30 (14.85) | 28 (13.86) | 16 (7.92) | 17 (8.42) |
| ≥40 | 3.45 ± 0.63 | 3.48 (0.92) | 4.35 ± 0.84 | 4.29 (1.11) | 0.80 ± 0.08 | 0.80 (0.07) | 33 (14.47) | 16 (7.02) | 21 (9.21) | 22 (9.65) |
| p | <0.001 | <0.001 | 0.002 | 0.912 | 0.019 | 0.634 | 0.657 | |||
| Employment duration (in years) | ||||||||||
| <10 | 3.78 ± 0.73 | 3.79 (1.05) | 4.72 ± 0.96 | 4.70 (1.29) | 0.81 ± 0.08 | 0.80 (0.07) | 60 (14.35) | 43 (10.29) | 34 (8.13) | 38 (9.09) |
| ≥10 | 3.43 ± 0.76 | 3.51 (1.36) | 4.16 ± 0.82 | 4.19 (1.55) | 0.82 ± 0.07 | 0.83 (0.07) | 3 (25.00) | 1 (8.33) | 3 (25.00) | 1 (8.33) |
| p | 0.100 | 0.047 | 0.180 | 0.396 | 1.000 | 0.040 | 1.000 | |||
| Gender | ||||||||||
| Female | 3.04 ± 0.57 | 2.94 (0.68) | 3.73 ± 0.77 | 3.67 (0.63) | 0.82 ± 0.08 | 0.81 (0.08) | 3 (9.38) | 3 (9.38) | 2 (6.25) | 5 (15.62) |
| Male | 3.83 ± 0.72 | 3.83 (0.98) | 4.78 ± 0.93 | 4.81 (1.24) | 0.81 ± 0.08 | 0.80 (0.07) | 60 (15.08) | 41 (10.30) | 35 (8.79) | 34 (8.54) |
| p | <0.001 | <0.001 | 0.308 | 0.602 | 1.000 | 1.000 | 0.194 | |||
| * Smoking status | ||||||||||
| Current smoker | 3.82 ± 0.70 | 3.71 (1.07) | 4.78 ± 0.99 | 4.66 (1.22) | 0.81 ± 0.10 | 0.80 (0.06) | 30 (31.58) | 19 (20.00) | 10 (10.53) | 9 (9.47) |
| Ex smoker | 3.72 ± 0.77 | 3.85 (1.17) | 4.71 ± 0.94 | 4.79 (1.38) | 0.79 ± 0.08 | 0.79 (0.07) | 12 (9.30) | 7 (5.43) | 13 (10.08) | 14 (10.85) |
| Never smoked | 3.79 ± 0.73 | 3.77 (1.11) | 4.67 ± 0.96 | 4.67 (1.34) | 0.82 ± 0.07 | 0.81 (0.06) | 21 (10.29 | 18 (8.82) | 14 (6.86) | 16 (7.84) |
| p | 0.560 | 0.644 | <0.001 | <0.001 | 0.001 | 0.454 | 0.643 | |||
| Existing respiratory condition | ||||||||||
| Yes | 3.82 ± 0.73 | 3.82 (1.14) | 4.86 ± 0.98 | 4.89 (1.39) | 0.79 ± 0.10 | 0.79 (0.07) | 26 (18.06) | 15 (10.42) | 25 (17.36) | 30 (14.85) |
| No | 3.75 ± 0.74 | 3.75 (1.05) | 4.63 ± 0.94 | 4.54(1.28) | 0.81 ± 0.07 | 0.81 (0.07) | 37 (12.94) | 29 (10.14) | 12 (4.20) | 33 (14.47) |
| p | 0.390 | 0.016 | <0.001 | 0.157 | 0.929 | <0.001 | ||||
| Lung Functions | ||||||||
|---|---|---|---|---|---|---|---|---|
| Social-Demographic Factors | FEV1 | FVC | Abnormal Ratio of FEV1/FVC (≤0.7) | Abnormal Spirometry Result (Obstructive or Restrictive) | ||||
| Adj-Beta (95% CI) | * p Value | Adj-Beta (95% CI) | * p Value | Adj-OR (95% CI) | # p Value | Adj-OR (95% CI) | # p Value | |
| Age (years) | ||||||||
| ≥40 | −0.713 (−0.833, −0.593) | <0.001 | −0.779 (−0.939, −0.618) | <0.001 | 5.167 (1.445, 18.483) | 0.012 | 3.942 (1.932, 8.040) | <0.001 |
| <40 | ref | ref | ref | |||||
| Employment duration (years) | ||||||||
| ≥10 | −0.141 (−0.498, 0.2155) | 0.437 | −0.340 (−0.818, 0.137) | 0.162 | 1.214 (0.133, 11.114) | 0.864 | 1.575 (0.395, 6.274) | 0.520 |
| <10 | ref | ref | ref | |||||
| Gender | ||||||||
| Female | −0.829 (−1.065, −0.593) | <0.001 | −1.082 (−1.398, −0.767) | <0.001 | 0.642 (0.072, 5.723) | 0.691 | 0.172 (0.020, 1.487) | 0.110 |
| Male | ref | ref | ref | ref | ||||
| Smoking status | ||||||||
| Current smoker | 0.054 (−0.096, 0.204) | 0.478 | 0.137 (−0.064, 0.338) | 0.182 | 2.387 (0.602, 9.467) | 0.216 | 1.728 (0.810, 3.688) | 0.157 |
| Ex-smoker | 0.061 (−0.077, 0.199) | 0.388 | 0.192 (0.007, 0.377) | 0.042 | 4.112 (1.234, 13.704) | 0.021 | 1.502 (0.747, 3.021) | 0.254 |
| Non-smoker | ref | ref | ref | ref | ||||
| Existing medical condition | ||||||||
| Yes | 0.038 (−0.087, 0.162) | 0.552 | 0.202 (0.036, 0.368) | 0.017 | 5.427 (1.971, 14.945) | 0.001 | 2.165 (1.177, 3.984) | 0.013 |
| No | ref | ref | ref | ref | ||||
| Respiratory Symptoms | ||||||||
| Social-Demographic Factors | Cough | Phlegm | Wheezing | Shortness of Breath | ||||
| Adj-OR (95% CI) | # p Value | Adj-OR (95% CI) | # p Value | Adj-OR (95% CI) | # p Value | Adj-OR (95% CI) | # p Value | |
| Age (years) | ||||||||
| ≥40 | 0.997 (0.562, 1.767) | 0.991 | 0.504 (0.257, 0.987) | 0.046 | 0.998 (0.475, 2.098) | 0.996 | 1.183 (0.595, 2.350) | 0.632 |
| <40 | ref | ref | ref | ref | ||||
| Employment duration (years) | ||||||||
| ≥10 | 2.264 (0.554, 9.250) | 0.255 | 1.186 (0.142, 9.909) | 0.875 | 4.376 (0.919, 20.846) | 0.064 | 0.918 (0.112, 7.528) | 0.936 |
| <10 | ref | ref | ref | ref | ||||
| Gender | ||||||||
| Female | 0.832 (0.225, 3.070) | 0.782 | 1.209 (0.324, 4.511) | 0.777 | 0.389 (0.078, 1.940) | 0.250 | 2.834 (0.924, 8.691) | 0.068 |
| Male | ref | ref | ref | ref | ||||
| Smoking status | ||||||||
| Current smoker | 4.200 (2.229, 7.912) | <0.001 | 2.751 (1.354, 5.588) | 0.005 | 1.624 (0.655, 4.028) | 0.295 | 1.218 (0.511, 2.901) | 0.656 |
| Ex-smoker | 0.898 (0.421, 1.913) | 0.780 | 0.661 (0.265, 1.650) | 0.375 | 1.724 (0.742, 4.009) | 0.206 | 1.327 (0.613, 2.872) | 0.473 |
| Non-smoker | ref | ref | ref | ref | ||||
| Existing medical condition | ||||||||
| Yes | 1.528 (0.541, 4.317) | 0.423 | 0.994 (0.505, 1.955) | 0.985 | 4.873 (2.311, 10.274) | <0.001 | 1.276(0.639, 2.550) | 0.490 |
| No | ref | ref | ref | ref | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gbondo, D.; Cerpa-Perez, V.; Pham, N.M.; Zhao, Y.; Rumchev, K. Exposure to Airborne Contaminants and Respiratory Health Among Lithium Mine Workers in Western Australia. Environments 2025, 12, 206. https://doi.org/10.3390/environments12060206
Gbondo D, Cerpa-Perez V, Pham NM, Zhao Y, Rumchev K. Exposure to Airborne Contaminants and Respiratory Health Among Lithium Mine Workers in Western Australia. Environments. 2025; 12(6):206. https://doi.org/10.3390/environments12060206
Chicago/Turabian StyleGbondo, David, Viviana Cerpa-Perez, Ngoc Minh Pham, Yun Zhao, and Krassi Rumchev. 2025. "Exposure to Airborne Contaminants and Respiratory Health Among Lithium Mine Workers in Western Australia" Environments 12, no. 6: 206. https://doi.org/10.3390/environments12060206
APA StyleGbondo, D., Cerpa-Perez, V., Pham, N. M., Zhao, Y., & Rumchev, K. (2025). Exposure to Airborne Contaminants and Respiratory Health Among Lithium Mine Workers in Western Australia. Environments, 12(6), 206. https://doi.org/10.3390/environments12060206






