The Role of Nurses and the Facilitators and Barriers in Diabetes Care: A Mixed Methods Systematic Literature Review
Abstract
1. Introduction
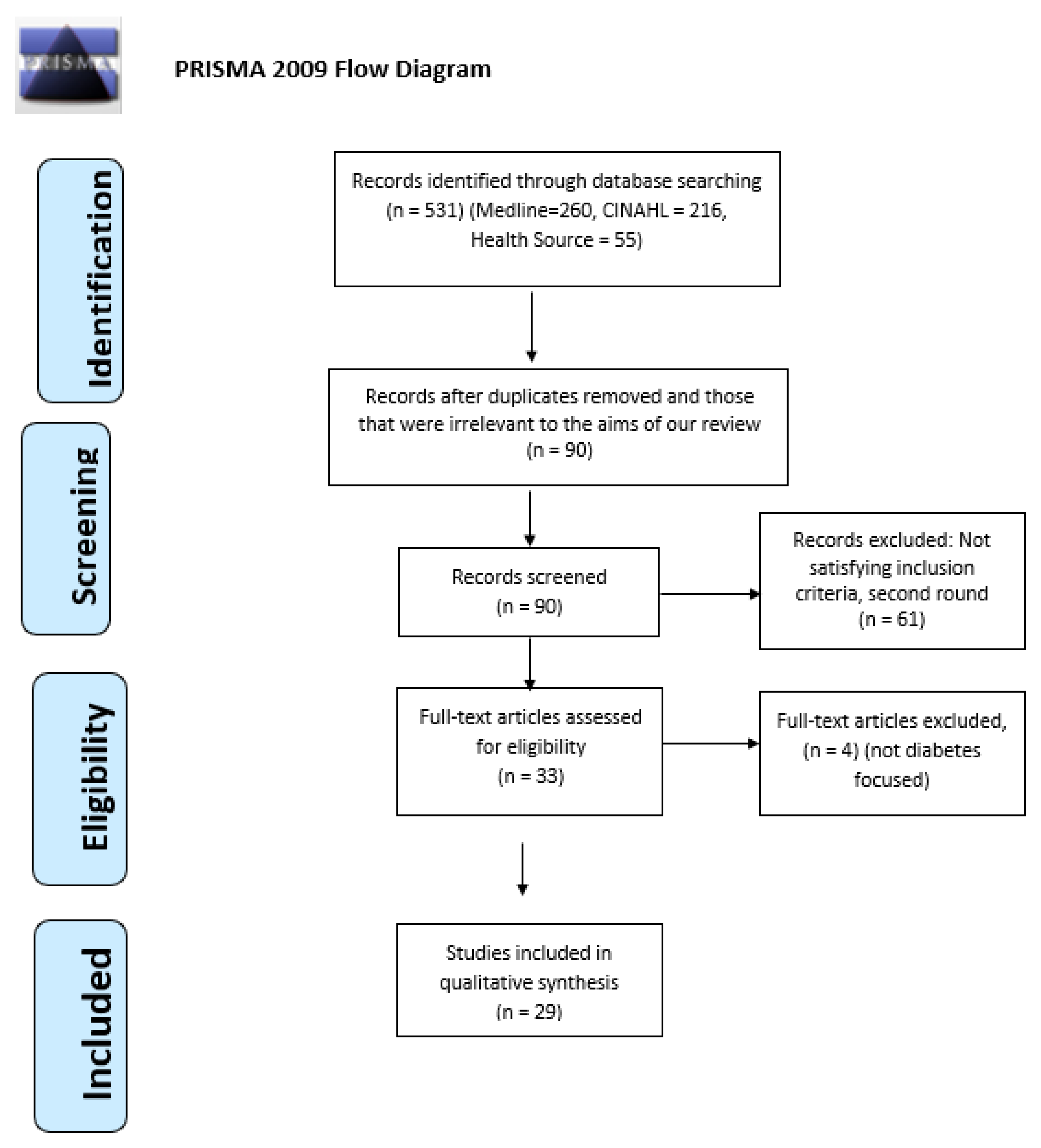
2. Methods
2.1. Type of Review
2.2. Research Questions
- What are the roles and activities of nurses caring for people with diabetes?
- What is the level of knowledge of nurses about diabetes care?
- What are the facilitators or barriers in caring for people with diabetes and in educating them about self-care management?
2.3. Search Strategy
- To be focused on diabetes care;
- To articulate the roles of nurses or their knowledge;
- To include nurses in the study sample;
- To be written in English or Greek;
- To be published between 1999 and 2018;
- To be primary sources.
2.4. Critical Appraisal
2.5. Data Extraction
2.6. Data Synthesis
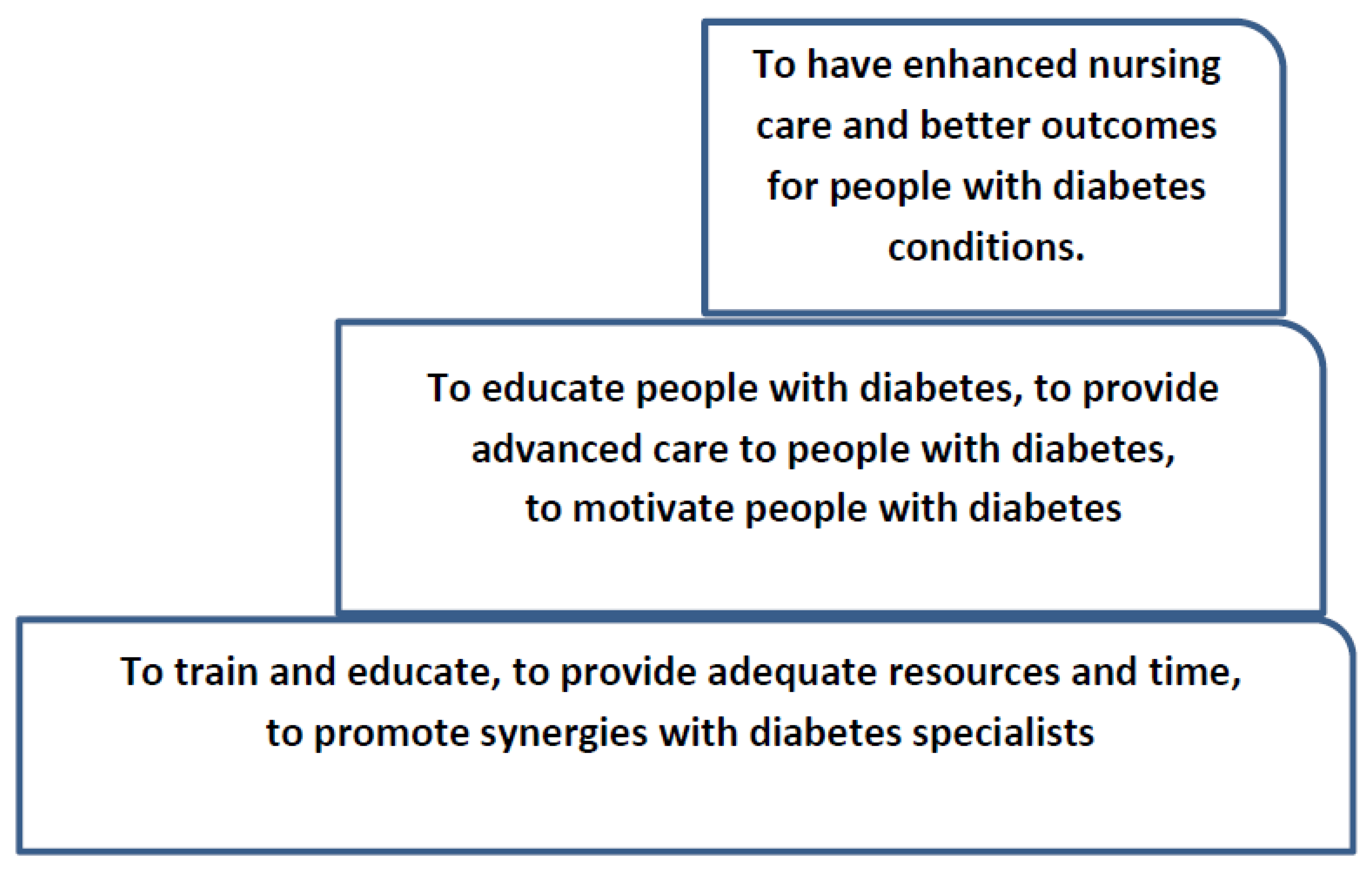
3. Results
3.1. Nurses’ Roles in Diabetes Care
3.1.1. Nurses as Educators
3.1.2. Nurses as Advanced Caregivers
3.1.3. Nurses as Motivators
3.2. Barriers or Facilitators for Nurses to Diabetes Care
3.2.1. Nurses’ Lack of Knowledge
3.2.2. Lack of Resources
3.2.3. Lack of Time
3.3. Collaboration with Diabetes Specialists
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
| Chan, M. F. and Zang, Y (2007) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Lipman, T. H, and Mahon, M. M. (1999) | √ | √ | √ | √ | √ | √ | √ | √ | No |
| Fisher, K. L (2006) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| El-Deirawi, K.M and Zuraikat, N. (2001) | √ | √ | √ | √ | √ | √ | √ | √ | No |
| Speight, J. and Bradley C. (2001) | √ | √ | √ | √ | √ | √ | √ | √ | No |
| Joshi, A., Komlodi, A., and Arora, M. (2008) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Derr R., Sivanandy M., Bronich-Hall L., and Rondriguez A. (2007) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Nash M. (2009) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Shiu, A. and Wong, R. (2011) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Findlow, L. and McDowell, J. (2002) | √ | √ | √ | √ | √ | √ | √ | √ | No |
| Kenealy, T., Arroll, B., Kenealy, H, Docherty, B., Scott, D., Scragg, R., and Simmons, D. (2004) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| James J., Gosden C., Winocour P., Walton C., Nagi D., Turner B., Williams R., and Holt RI. (2009) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Carey, N. and Courtenay, M. (2008) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Chinnasamy E., Mandal A., Khan S., Iqbal F., and Patel N. (2011) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Ndebu, J. and Jones, C. (2018) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Modic, M. B., Vanderbilt, A., Siedlecki, S. L, Sauvey R., Kaser N., and Yager C., (2014) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Roopnarinesingh, N, Brennan, N., Khan, C., Ladenson, PW, and Hill-Briggs, F. (2015) | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 |
| Wexller, D, Veauharnais, C., Regan, S., Nathan, D., Cagliero, E., and Larkin, M. E. (2012) | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Raballo, M, Trevisan, M, Trinetta, A, Charrier, L, Cavallo, F, Porta, M, and Trento, M. (2012) | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 |
| Peyrot, M., Rubin, R., and Simnierio, L. (2006) | √ | √ | √ | √ | √ | No | No | √ | √ | √ |
| Mutea N. and Baker C. (2007) | √ | √ | √ | √ | √ | No | No | √ | √ | √ |
| Kassean H. K. (2005) | √ | √ | √ | √ | √ | No | No | √ | √ | √ |
| Bostrom, E., Isaksson, U., Sjolander, A., and Hornsten, A. (2012) | √ | √ | √ | √ | √ | No | No | √ | √ | √ |
| Siminerio, L., Funnel, M., Peyrot, M., and Rubin, R. (2007) | √ | √ | √ | √ | √ | No | No | √ | √ | √ |
| Raaijmakers, L.G.M., Hamers, F.J.M., Martens, M. K., Bagchus, C., de Vries, N.K., and Kremers, S.P.J. (2013) | √ | √ | √ | √ | √ | No | No | √ | √ | √ |
| O’Connor, R., Mannix, M, Mullen, J, Powys, L, Mannion, M, Nolan, HA, Kearney, E, Cullen, W, Griffin, M, and Saunders, J. (2013) | √ | √ | √ | √ | √ | No | No | √ | √ | √ |
| Donohue-Porter P. (2013) | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 |
| Cardwell J., Hardy K., Ford N., and O’Brien S. (2016) | √ | √ | √ | √ | √ | √ | √ | √ |
| Authors and Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 |
| Livingston, R. and Dunning, T. (2010) | √ | √ | √ | √ | √ | √ | √ | √ |
References
- International Diabetes Federation. IDF Diabetes Edition, 8th ed.; IDF: Brussels, Belgium, 2017. [Google Scholar]
- Schneider, A.; Kalyani, R.; Golden, S.; Stearns, S.C.; Wruck, L.; Yeh, H.C.; Coresh, J.; Selvin, E. Diabetes and prediabetes and risk of hospitalization: The atherosclerosis risk in communities (ARIC) study. Diabetes Care 2016, 39, 772–779. [Google Scholar] [CrossRef] [PubMed]
- NHS Institute for Innovation and Improvement. Delivering Quality and Value. In Focus on: Inpatient Care for People with Diabetes; NHS Institute for Innovation and Improvement: London, UK, 2008. [Google Scholar]
- World Health Organization. Global Report on Diabetes; WHO: Paris, France, 2016. [Google Scholar]
- Carey, N.; Courtenay, M. An exploration of the continuing professional development needs of nurse independent prescribers and nurse supplementary prescribers who prescribe medicines for patients with diabetes. J. Clin. Nurs. 2010, 19, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Patlak, M. New weapons to combat an ancient disease: Treating diabetes. FASEB J. 2002, 16, 1853. [Google Scholar] [CrossRef] [PubMed]
- Riordan, F.; McHugh, S.M.; Murphy, K.; Barrett, J.; Kearney, P.M. The role of nurse specialist of integrated diabetes care: A cross sectional survey of diabetes nurse specialist services. Br. Med. J. Open 2017, 7, e015049. [Google Scholar] [CrossRef] [PubMed]
- Watts, S.A.; Sood, A. Diabetes nurse case management: Improving glucose control: 10 years of quality improvement follow-up data. Appl. Nurs. Res. 2016, 29, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Aliha, J.M.; Asgari, M.; Khayeri, F.; Ramazani, M.; Farajzadegan, Z.; Javaheri, J. Group education and nurse-telephone follow-up effects on blood glucose control and adherence to treatment in type 2 diabetes patients. Int. J. Prev. Med. 2013, 4, 797–802. [Google Scholar]
- Washburn, S.C.; Hornberger, C.A. Nurse educator guidelines for the management of heart failure. J. Contin. Educ. Nurs. 2008, 39, 263–267. [Google Scholar] [CrossRef]
- Hainsworth, T.A. New model of care for people who have long-term conditions. Nurs. Times 2005, 101, 28–29. [Google Scholar]
- Ginzburg, T.; Hoffman, R.; Azuri, J. Improving Diabetes Control in the community a nurse managed intervention model in a multidisciplinary clinic. Aust. J. Adv. Nurs. 2007, 35, 23–30. [Google Scholar]
- Lipman, T.H.; Mahon, M.M. Nurses’ knowledge of diabetes. J. Nurs. Educ. 1999, 38, 92–95. [Google Scholar]
- Findlow, L.; McDowel, J.R.S. Determining registered nurses’ knowledge of diabetes mellitus. J. Diabetes Nurs. 2002, 6, 170–175. [Google Scholar]
- Eldeirawi, K.; Zuraikat, N. Registered nurses’ actual and perceived knowledge of diabetes mellitus. J. Nurses Staff Dev. JNSD Off. J. Natl. Nurs. Staff Dev. Organ. 2001, 17, 5–11. [Google Scholar] [CrossRef]
- Pledger, J. The effect on inpatient care of dedicated diabetes specialist nurse. J. Diabetes Nurs. 2005, 9, 252–256. [Google Scholar]
- The Joanna Briggs Institute. Critical Appraisal Checklist for Qualitative Research. 2016. Available online: http://joannabriggs.org/research/critical-appraisaltools.html (accessed on 18 April 2019).
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and metaanalyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- De Chesnay, M. Nursing Research Using Data Analysis: Qualitative Designs and Methods in Nursing; Springer Publishing Company: New York, NY, USA, 2014. [Google Scholar]
- Zhang, Y.; Wildemuth, B.M. Qualitative analysis of content. In Applications of Social Research Methods to Questions in Information and Library Science; Wildemuth, B., Ed.; Libraries Unlimited: Westport, CT, USA, 2009; pp. 308–319. [Google Scholar]
- Boström, E.; Isaksson, U.; Lundman, B. Diabetes specialist nurses’ perceptions of their multifaceted role. Eur. Diabetes Nurs. 2012, 9, 39–44b. [Google Scholar] [CrossRef]
- James, J.; Gosden, C.; Winocour, P.; Walton, C.; Nagial, D.; Turner, B.; Williams, R.; Holt, R.I.G. Diabetes specialist nurses and role evolvement: A survey by Diabetes UK and ABCD of specialist diabetes services 2007. J. Diabetes Med. 2009, 26, 560–565. [Google Scholar] [CrossRef]
- Wexller, D.; Veauharnais, C.; Regan, S.; Beauharnais, C.C.; Nathan, D.M.; Cagliero, E.; Larkin, M.E. Impact of inpatient diabetes management, education, and improved discharge transition on glycemic control 12 months after discharge. Diabetes Res. Clin. Pract. 2012, 98, 249–256. [Google Scholar] [CrossRef]
- Kenealy, T.; Arroll, B.; Kenealy, H.; Docherty, B.; Scott, D.; Scragg, R.; Simmons, D. Diabetes care: Practice nurse roles, attitudes and concerns. J. Adv. Nurs. 2004, 48, 68–75. [Google Scholar] [CrossRef]
- Raballo, M.; Trevisan, M.; Trinetta, A.; Charrier, L.; Cavallo, F.; Porta, M.; Trento, M. A study of patients’ perceptions of diabetes care delivery and diabetes. Propositional analysis in people with type 1 and 2 diabetes managed by group or usual care. Diabetes Care 2012, 35, 242–247. [Google Scholar] [CrossRef]
- NMC. Nursing and Midwifery Council Definition of Advanced Nurse Practitioners; NMC: London, UK, 2005. [Google Scholar]
- Duffield, C.; Roche, M.; O’Brien-Pallas, L.; Catling-Paull, C.; King, M. Staff satisfaction and retention and the role of the Nursing Unit Manager. Collegian 2009, 16, 11–17. [Google Scholar] [CrossRef]
- Mutea, N.K.; Baker, C.M. Kenyan nurses’ involvement in managing hospitalized diabetic patients. Int. J. Nurs. Pract. 2008, 14, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Carey, N.; Courtenay, M. Nurse supplementary prescribing for patients with diabetes: A national questionnaire survey. J. Clin. Nurs. 2008, 17, 2185–2193. [Google Scholar] [CrossRef] [PubMed]
- Livingston, R.; Dunning, T. Practice nurses’ role and knowledge about diabetes management within rural and remote Australian general practices. Eur. Diabetes Nurs. 2010, 7, 55–62. [Google Scholar] [CrossRef]
- Siminerio, L.M.; Funnell, M.M.; Peyrot, M.; Rubin, R.R. US nurses’ perceptions of their role in diabetes care: Results of the cross-national Diabetes Attitudes Wishes and Needs (DAWN) study. Diabetes Educ. 2007, 33, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Kassean, H. Nurses’ Perceptions of the role in caring for diabetic patients at the primary care level: A case study from Mauritius. J. Health Manag. 2005, 7, 207–213. [Google Scholar] [CrossRef]
- Peyrot, M.; Rubin, R.R.; Lauritzen, T.; Skovlund, S.E.; Snoek, F.J.; Matthews, D.R.; Landgraf, R. Patient and provider perceptions of care for diabetes: Results of the cross-national DAWN Study. Diabetologia 2006, 49, 279–288. [Google Scholar] [PubMed]
- Donohue-Porter, P. Nursing’s Role in Courage Development in Patients Facing Complications of Diabetes. J. Holist. Nurs. 2013, 31, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Cardwell, J.; Hardy, K.; Ford, N.; O’Brien, S. Assessment of diabetes knowledge in trained and untrained ward nurses before and after intensive specialist support. J. Diabetes Nurs. 2016, 20, 60–64. [Google Scholar]
- Chinnasamy, E.; Mandal, A.; Khan, S.; Iqbal, F. Nurses’ knowledge of inpatient hypoglycaemia management. J. Diabetes Nurs. 2011, 15, 313–317. [Google Scholar]
- Ndebu, J.; Jones, C. Inpatient nursing staff knowledge on hypoglycaemia management. J. Diabetes Nurs. 2018, 22. ISSN 1368-1109. [Google Scholar]
- Derr, R.L.; Sivanandy, M.S.; Bronich-Hall, L.; Rodriguez, A. Insulin-Related Knowledge Among Health Care Professionals in Internal Medicine. Diabetes Spectr. 2007, 20, 177–185. [Google Scholar] [CrossRef]
- Shiu, A.T.; Wong, R.Y. Diabetes foot care knowledge: A survey of registered nurses. J. Clin. Nurs. 2011, 20, 2367–2370. [Google Scholar] [CrossRef] [PubMed]
- Speight, J.; Bradley, C. The ADKnowl: Identify knowledge deficits in diabetes care. Diabetes Med. 2001, 18, 626–633. [Google Scholar] [CrossRef]
- Nash, M. Mental Health nurses’ diabetes care skills—A training needs analysis. Br. J. Nurs. 2009, 18, 626–630. [Google Scholar] [CrossRef] [PubMed]
- Modic, M.B.; Vanderbilt, A.; Siedlecki, S.L.; Sauvey, R.; Kaser, N.; Yager, C. Diabetes management unawareness: What do bedside nurses know? Appl. Nurs. Res. 2014, 27, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.F.; Zang, Y.L. Nurses’ perceived and actual level of diabetes mellitus knowledge: Results of a cluster analysis. J. Clin. Nurs. 2007, 16, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Fisher, K.L. School Nurses’ Perceptions of Self-Efficacy in Providing Diabetes care. J. School Nurs. 2006, 22, 223–228. [Google Scholar] [CrossRef]
- Raaijmakers, L.G.M.; Hamers, F.J.M.; Martens, M.K.; Bagchus, C.; de Vries, N.K.; Kremers, S.P. Perceived facilitators and barriers in diabetes care: A qualitative study among health care professionals in the Netherlands. BMC Family Pract. 2013, 14, 1–9. [Google Scholar] [CrossRef]
- O’Connor, R.; Mannix, M.; Mullen, J.; Powys, L.; Mannion, M.; Nolan, H.A.; Kearney, E.; Cullen, W.; Griffin, M.; Saunders, J. Structured care of diabetes in general practice: A qualitative study of the barriers and facilitators. Ir. Med. J. 2013, 106, 77–80. [Google Scholar]
- Roopnarinesingh, N.; Brennan, N.; Khan, C.; Ladenson, P.W.; Hill-Briggs, F.; Kalyani, R.R. Barriers to optimal diabetes care in Trinidad and Tobago: A health care Professionals’ perspective. BMC Health Serv. Res. 2015, 15, 396. [Google Scholar] [CrossRef]
- Joshi, A.; Komlodi, A.; Arora, M. School nurses’ perceived barriers to diabetes knowledge, communication and management in children with type 1 diabetes. School Nurs. News 2008, 25, 24–29. [Google Scholar]
| N | Authors and Year | Methodology | Sample | Relevant Findings |
|---|---|---|---|---|
| 1 | Livingston, R. and Dunning, T. (2010) | Mixed | 21 nurses | • Inadequate knowledge • Deficit in nurses’ knowledge (risk factors, treatment, complications) • Distance from education • Difficulties collaborating with diabetes specialist services • Lack of experience and age |
| 2 | Chan, M. F. and Zang, Y (2007) | Quantitative | 245 nurses | Cluster 1: Highly competent and knowledgeable about diabetes (40.4%) Cluster 2: Moderately competent and knowledgeable (43%) Cluster 3: Low competence and low diabetes knowledge. (16.3%) Also fewer years of work experience and lower education level • Question on competence: more than 57% of all nurses reported somewhat/not very/not at all competent but there were differences between clusters–statistically significant differences found on the competence between the three Clusters (p < 0.001). • Perceived knowledge was significant and positively correlated with their actual knowledge (rs = 0.32, p < 0.001). |
| 3 | Lipman, T. H, and Mahon, M. M. (1999) | Quantitative | 155: Nurses, nursing students, and non-nursing students | • Diabetes knowledge found to be lacking in all groups The mean scores were as follows: Group I = 65.3% (±14.4%); Group II = 57.4% (±17.3%); Group III = 13.1% (±11.0%). The scores for practicing RNs ranged from 20% to 95% (mean = 64.3% ±14.4%). • RNs’ knowledge was poorest regarding insulin action and in signs, symptoms and treatment of hyperglycemia. • Deficient knowledge either of diabetes education in nursing school or in the retention of what has been taught • Misinformation/ outdated textbooks • Student nurses’ poor knowledge of what glucagon is and when it should be used • Staff nurses are not motivated to learn about diabetes. |
| 4 | Fisher, K. L (2006) | Quantitative | 70 school nurses | • Nurses perceived they were moderately confident regarding diabetes care and education for children—total score on Self-Efficacy on Diabetes Education (SEDE) (mean = 36.30, SD 9.99). • Respondents reported lower confidence scores for (a) educating about diabetes when they cannot access measuring equipment, (b) inaccessible resources (mean = 2.78, SD 1.09). |
| 5 | El-Deirawi, K.M and Zuraikat, N. (2001) | Quantitative | 79 Nurses: 32 community hospital nurses, 47 home health care agency nurses | • Small but significant, positive correlation (r = 0.402, p < 0.0001) between perceived and actual knowledge of diabetes Participants’ lack of knowledge about insulin injections sites and etiology of type 1 diabetes mellitus • Home health nurses achieved higher scores than hospital nurses on the DSRT (Diabetes Self-report Tool) (t = 3.835, p < 0.0001). • The level of education was found to be positively correlated with the level of knowledge of diabetes. • The participants either attended not in-service education about diabetes or attended in-service programmes more than 2 years ago. |
| 6 | Speight, J. and Bradley C. (2001) | Quantitative | 789 patients and 16 health professionals | • Knowledge scores were higher in insulin-treated than in non-insulin-treated patients (U = 34875.0; n = 422 and 323, respectively; p < 0.0001). • Knowledge of foot care, hypoglycemia, and diet and food were the most problematic topics, with patients achieving mean scores of 59.5%, 62.4%, and 64.5%, respectively, for these topics. • Patients and health professionals show deficit knowledge on items that might have serious short and long terms consequences. |
| 7 | Joshi, A., Komlodi, A. and Arora, M. (2008) | Quantitative | 43 school nurses | • 79% use internet as the main information source • Barriers of communication between health care providers of the diabetic students • Providers lack access and time. • Time constraints and lack of access to diabetes education in acquiring diabetes knowledge • Lack of updated relevant clinical information |
| 8 | Derr R., Sivanandy M., Bronich-Hall L., and Rondriguez A. (2007) | Quantitative | 377: 73 faculty, 113 residents, and 191 nurses | • The majority of general medicine faculty felt very comfortable in managing diabetes and the majority of other categories described themselves as somewhat comfortable. • For the 16 knowledge-based questions, the overall percentages answered correctly was 51% for faculty, 59% house staff and 47% for nurses. • Nurses scored worse than physicians on questions testing knowledge of inpatient insulin use (34% vs. 57%, p < 0.0001). |
| 9 | Nash M. (2009) | Quantitative | 138 mental health nurses | • The majority of the sample self-rated their knowledge of diabetes knowledge as fair (40%). • 64% of the sample felt that they had not received appropriate training. • 86% indicated that they required further training. |
| 10 | Shiu, A. and Wong, R. (2011) | Quantitative | 65 Registered nurses | • 57% claimed that they had never received any training in diabetes foot care knowledge. • The level of registered nurses’ foot care knowledge was fair. • RNs with (n = 22, mean DFKS = 41.5, SD 7.3) and without (n = 43, mean DFKS = 41.3, SD 6.1) work experience in diabetes care specialty services obtained similar DFKS marks, p = 0.924. (DFKS = Diabetes Foot Care Knowledge Scale). |
| 11 | Findlow, L. and McDowell, J. (2002) | Quantitative | 133 registered nurses | • Only 5.2% attended a diabetes course within the preceding five years. • The overall pass rate was 69%. • Comparison of results by grade showed that there was no statistically significant difference in knowledge between the two groups of nurses (grades D/E and F/G, p = 0.255). (Grades are according to the nurses’ enrolment status). • Almost half of the respondents (48.4%) were unaware of how to carry out blood glucose monitoring accurately and precisely. |
| 12 | Wexller, D, Veauharnais, C., Regan, S., Nathan, D., Cagliero, E., and Larkin, M. E. (2012) | Quantitative | 31 patients | • Mean inpatient glucose was lower in the IDMET than in the UC group (p = 0.001). • After one year of discharge, the average HbA1c reduction was greater in IDMET compared to the UC group (p = 0.5). • Newly discharged patients on insulin; the average HbA1c reduction was greater in the IDMET than in the UC group. |
| 13 | Peyrot, M., Rubin, R., and Simnierio, L. (2006) | Qualitative | 2,705 physicians, 1,122 nurses | • Nurses perceived significantly higher prevalence and severity of psychosocial problems and used psychosocial strategies significantly more frequently than physicians. • Both physicians and nurses diabetes specialists were significantly more likely than generalists to utilize psychosocial strategies. |
| 14 | Mutea N. and Baker C. (2007) | Qualitative | 15 registered nurses | Content analysis produced 8 categories of nurses’ involvement in managing diabetic patients: • Knowledge of DM • Management of DM • Continuity of care • Quality of care • Patient accessibility to diabetic care • Patient support activities • Resources • Condition of service |
| 15 | Kenealy, T., Arroll, B., Kenealy, H, Docherty, B., Scott, D., Scragg, R., and Simmons, D. (2004) | Quantitative | 86 PNs in 1990 77 PNs in 1999 | • In 1999, nurses looked after more patients with diabetes without spending more time on diabetes care than nurses in 1990. • Nurses in 1999 reported increased involvement in the more complex areas of diabetes care such as foot care (61% vs. 40% x2 = 7.339, d.f. 1, p = 0.021). • In 1999, nurses were no more likely than those in 1990 to adjust treatment. Proposals were debated to allow nurses to prescribe. |
| 16 | Kassean H. K. (2005) | Qualitative | 10 nurses | Four main themes emerged: (1) Management of care (2) Barriers to care (3) Communication skills (4) Training and educational needs • The majority of nurses did not feel knowledgeable. • Deficit in their knowledge |
| 17 | James J., Gosden C., Winocour P., Walton C., Nagi D., Turner B., Williams R., and Holt RI. (2009) | Quantitative | 159 (DSNs, Nurse consultants and diabetes health care assistants) | • 78% and 76% DSNs planned and delivered education sessions compared with 13% in 2000. • 22% of DSN had a formal role in diabetes research compared with 48% in 2000 (p <0.000). • 49% of hospital DSNs, 56% of Community DSNs, and 66% of nurse-consultants are involved in prescribing. |
| 18 | Carey, N. and Courtenay, M. (2008) | Quantitative | 214 Nurses located throughout the UK | • The majority of nurses prescribe between one and five items a week–differences between groups were statistically significant (p = 0.001). • Oral anti-diabetic drugs, hypertension and lipid regulating drugs, and insulin were often prescribed. (p = 0.031). |
| 19 | Bostrom, E., Isaksson, U., Sjolander, A., and Hornsten, A. (2012) | Qualitative | 29 DSNs | • DSNs identify five major roles of their profession: expert, fosterer, executive, leader, and role model. • Challenges interpreted as role ambiguities included feeling uninformed, fragmented, resigned, pressed for time, and self-reproachful. |
| 20 | Siminerio, L., Funnel, M., Peyrot, M. and Rubin, R. (2007) | Qualitative | 51 generalist nurses, 50 specialist nurses, 166 generalist physicians, 50 diabetes specialist physicians | • Nurses and physicians agreed that nurses should take a larger role in managing diabetes. • Nurses provide better education, spend more time with patients, were better listeners, and knew their patients better than physicians. • All nurses had a high perceived need for better understanding of psychosocial issues. • Generalist nurses report that they act as intermediaries and facilitate patient appointment keeping. |
| 21 | Raaijmakers, L.G.M., Hamers, F.J.M., Martens, M. K., Bagchus, C., de Vries, N.K., and Kremers, S.P.J. (2013) | Qualitative | 18 Health professionals: 3 Family Physicians, 3 Practice Nurses, 2 Diabetes Nurses, 3 Dieticians, 2 Physical Therapist, 3 Internal Medicine Physicians, 2 Pharmacists | • Major facilitators: More prominent role of practice nurses and diabetes nurses in diabetes care • Certain professional groups collaborate (i.e., dieticians, physical therapists, and pharmacists); there is collaboration between primary and secondary care, but could improve. • Health insurers’ bundled payment system for funding diabetes care was perceived as a major barrier within the health care system. • Patients’ lack of motivation and their lack of awareness of lifestyle programmes and prevention initiatives were barriers. |
| 22 | O’Connor, R., Mannix, M, Mullen, J, Powys, L, Mannion, M, Nolan, HA, Kearney, E, Cullen, W, Griffin, M, and Saunders, J. (2013) | Qualitative | GPs (n = 55) practice nurses (n = 11) | Distinct barriers and facilitators emerged in relation to the proposed change in structured diabetes care within general practice. They fell into three domains: practitioner factors, practice factors, and systemic factors. |
| 23 | Roopnarinesingh, N, Brennan, N., Khan, C., Ladenson, PW, and Hill-Briggs, F. (2015) | Quantitative | 198 Participants physicians (44%, n = 88) or nurses (40%, n = 79) | Barriers reported: Limited access to blood testing (75%), ophthalmological evaluations (96%), ECGs (69%), and cardiac stress tests (92%); inadequate time to screen and evaluate DM complications (95%), poor access to consultants for referral of difficult cases (77%), and lack of provider education regarding cardiovascular complications of DM (57%). HCP agreed that nurses could have a more active role in the care and prevention of cardiovascular disease and diabetes through leading patient education efforts (98%), screening patients for complications (91%), coordinating care efforts (99%), and educating family members (98%). |
| 24 | Cardwell J., Hardy K., Ford N., and O’Brien S. (2016) | Quantitative | 26 RGNs and 17 HCAs from general medical or surgical ward | • Both wards scored 100% on knowledge about physiology of diabetes, but they did not understand more practical elements. • This included knowledge about the timing and administration of some insulins, use of metformin in renal impairment, and when to escalate blood ketone results. • There was no significant difference in scores between the medical and surgical wards. |
| 25 | Chinnasamy E., Mandal A., Khan S., Iqbal F., and Patel N. (2011) | Quantitative | 100 responses were received from participants: 80% staff nurses, 20% senior or charge nurses | • 51% had formal training in hypoglycemia management. • 28% nurses knew the common symptoms of hypoglycemia listed in the questionnaire. • 73% of the hypoglycemic episodes were detected by routine checks and this was predicted by nurses in the survey. Conclusion: There is a lack of knowledge among ward nurses regarding hypoglycemia management and further training is necessary. |
| 26 | Ndebu, J. and Jones, C. (2018) | Quantitative | 40 responses received. The breakdown of staff was: 5% Ward Manager, 7.5% Senior Nurse; 75% Staff Nurse, 2.5% HCA (Band 4) and 10% HCA | 93.75% (15/16) of diabetes ward nurses recognized all hypoglycemia symptoms. Only 58.3% (7/12) from vascular and 25% (3/12) from critical care wards recognized the symptoms. 58.3% (7/12) of critical care nursing staff recognized just 3 or fewer hypoglycemia symptoms. Although everyone used some form of rapid-acting carbohydrates for hypoglycemia treatment and were aware to recheck CBG after treatment, only 77.5% (31/40) of the nursing staff rechecked the CBG after 15 minutes as per this hospital’s guidelines, while 17.5% (7/40) rechecked after 20–30 minutes. Moreover, 10% (4/40) stated they would have omitted insulin after this treatment. |
| 27 | Modic, M. B., Vanderbilt, A., Siedlecki, S. L, Sauvey R., Kaser N., and Yager C., (2014) | Quantitative | 2250 registered nurses working in a quaternary health care centre | • Nurses’ knowledge of inpatient diabetes management principles was low. No correlation between knowledge scores and age, education, employment status, years of experience, or clinical specialty. • Pearson’s correlation was conducted to determine if there was a relationship between comfort level or familiarity and diabetes management knowledge: there was no correlation between comfort (r = 0.002; p = 0.912) and familiarity (r = −0.013; p = 0.556) and diabetes management knowledge; correlation found between comfort and familiarity (r = 0.706; p < 0.001) |
| 28 | Raballo, M, Trevisan, M, Trinetta, A, Charrier, L, Cavallo, F, Porta, M, and Trento, M. (2012) | Mixed | 241 patients | Patients on group care showed more positive attitudes, higher sense of empowerment, and more internal locus of control than those on usual care. In addition, they expressed a wider and more articulated range of concepts associated with the care received and made less use of medical terminology. |
| 29 | Donohue-Porter P. (2013) | Qualitative | 14 nurses | • Educating for empowerment • Advocating and reflecting action • Treasuring the relationship • Humanizing the complexity |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nikitara, M.; Constantinou, C.S.; Andreou, E.; Diomidous, M. The Role of Nurses and the Facilitators and Barriers in Diabetes Care: A Mixed Methods Systematic Literature Review. Behav. Sci. 2019, 9, 61. https://doi.org/10.3390/bs9060061
Nikitara M, Constantinou CS, Andreou E, Diomidous M. The Role of Nurses and the Facilitators and Barriers in Diabetes Care: A Mixed Methods Systematic Literature Review. Behavioral Sciences. 2019; 9(6):61. https://doi.org/10.3390/bs9060061
Chicago/Turabian StyleNikitara, Monica, Costas S Constantinou, Eleni Andreou, and Marianna Diomidous. 2019. "The Role of Nurses and the Facilitators and Barriers in Diabetes Care: A Mixed Methods Systematic Literature Review" Behavioral Sciences 9, no. 6: 61. https://doi.org/10.3390/bs9060061
APA StyleNikitara, M., Constantinou, C. S., Andreou, E., & Diomidous, M. (2019). The Role of Nurses and the Facilitators and Barriers in Diabetes Care: A Mixed Methods Systematic Literature Review. Behavioral Sciences, 9(6), 61. https://doi.org/10.3390/bs9060061







