Twenty-Four-Hour Movement Behaviors and Social Functions in Neurodiverse Children: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Information Sources and Search Strategy
2.2. Eligibility Criteria
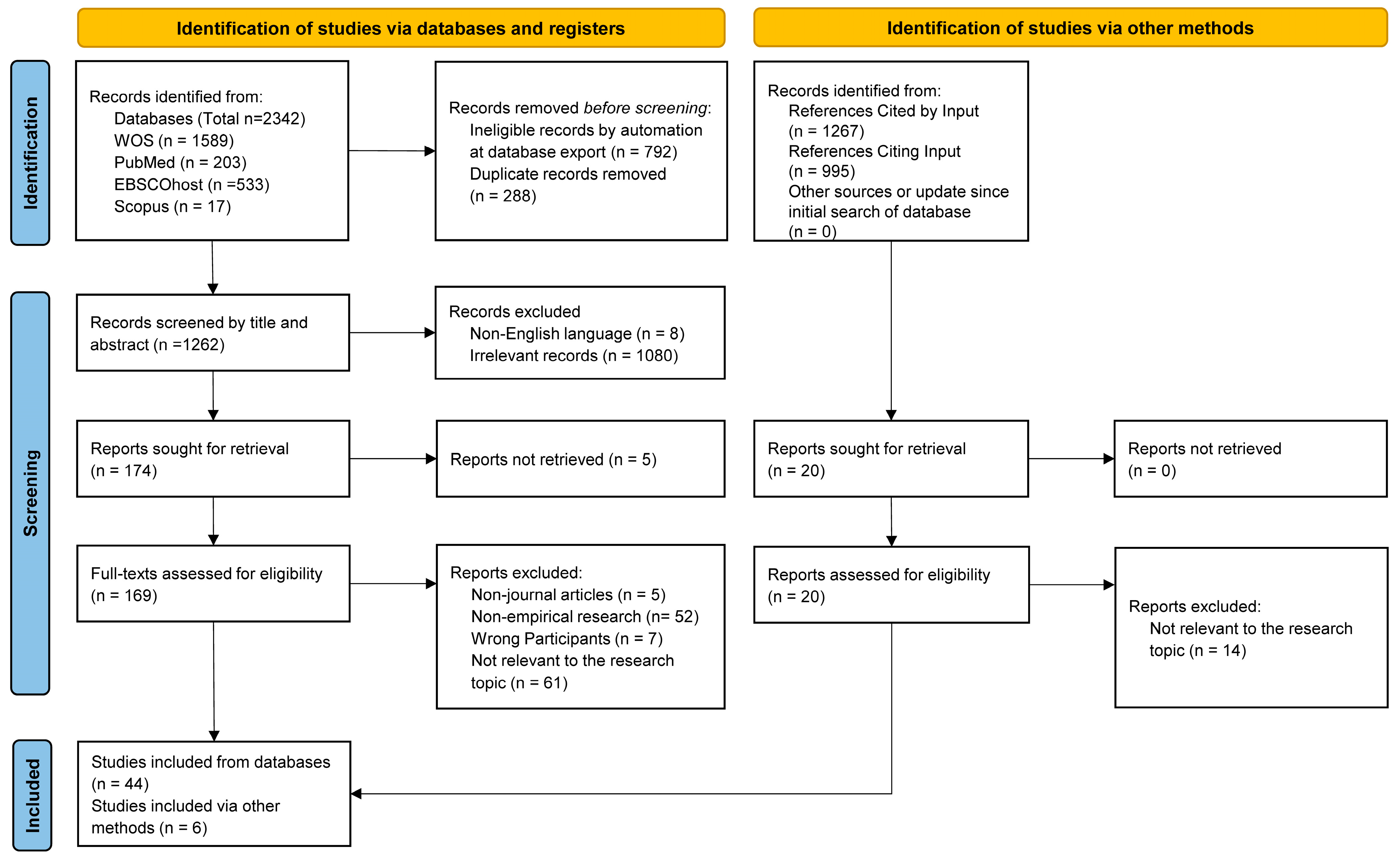
2.3. Screening
2.4. Data Extraction and Synthesis of Results
3. Results
3.1. Study Selection
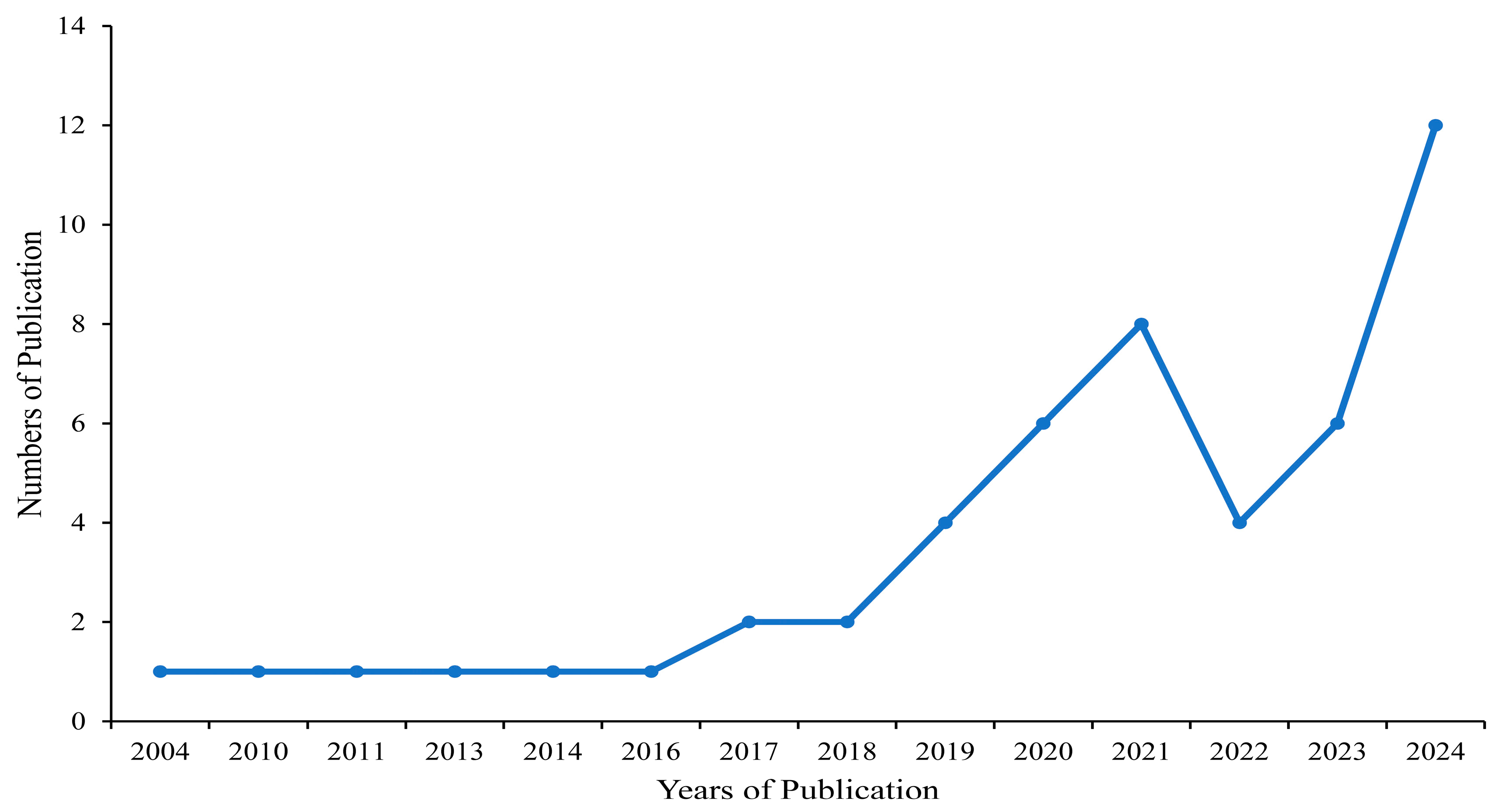
3.2. Study Characteristics
3.3. Characteristics of Participants
3.4. Study Measures
3.5. Design of Interventions
3.6. General Overview of Scoping Review Findings
4. Discussion
4.1. Strength of Evidence and Moving Beyond Physical Activity
4.2. Optimizing Intervention Designs for Neurodiverse Children
4.3. Taking the Advantages of Qualitative Measures
4.4. Breaking the Stigma of “Disorder" or “Disability"
4.5. Strengths, Limitations, and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. [Google Scholar] [CrossRef]
- Armstrong, T. (2012). Neurodiversity in the classroom: Strength-based strategies to help students with special needs succeed in school and life. ASCD. [Google Scholar]
- Bramer, W. M., Giustini, D., de Jonge, G. B., Holland, L., & Bekhuis, T. (2016). De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association, 104(3), 240–243. [Google Scholar] [CrossRef]
- Cei, A., Ruscello, B., & Sepio, D. (2023). The role of football in enhancing psychosocial skills in youth with autism spectrum disorder. International Journal of Sport Psychology, 54(5), 373–388. [Google Scholar] [CrossRef]
- Chaput, J. P., Saunders, T. J., & Carson, V. (2017). Interactions between sleep, movement and other non-movement behaviours in the pathogenesis of childhood obesity. Obesity Reviews, 18(Suppl. S1), 7–14. [Google Scholar] [CrossRef] [PubMed]
- Cherewick, M., & Matergia, M. (2024). Neurodiversity in practice: A conceptual model of autistic strengths and potential mechanisms of change to support positive mental health and wellbeing in autistic children and adolescents. Advances in Neurodevelopmental Disorders, 8(3), 408–422. [Google Scholar] [CrossRef]
- Craig, S. G., Weiss, M. D., Hudec, K. L., & Gibbins, C. (2020). The functional impact of sleep disorders in children with ADHD. Journal of Attention Disorders, 24(4), 499–508. [Google Scholar] [CrossRef]
- Daudt, H. M., van Mossel, C., & Scott, S. J. (2013). Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Medical Research Methodology, 13, 48. [Google Scholar] [CrossRef]
- Gallotta, M. C., Emerenziani, G. P., Franciosi, E., Meucci, M., Guidetti, L., & Baldari, C. (2015). Acute physical activity and delayed attention in primary school students. Scandinavian Journal of Medicine & Science in Sports, 25(3), e331–e338. [Google Scholar] [CrossRef]
- Güeita-Rodríguez, J., Ogonowska-Slodownik, A., Morgulec-Adamowicz, N., Martín-Prades, M., Cuenca-Zaldívar, J., & Palacios-Ceña, D. (2021). Effects of aquatic therapy for children with autism spectrum disorder on social competence and quality of life: A mixed methods study. International Journal of Environmental Research and Public Health, 18(6), 3126. [Google Scholar] [CrossRef]
- Haghighi, A. H., Broughani, S., Askari, R., Shahrabadi, H., Souza, D., & Gentil, P. (2023). Combined physical training strategies improve physical fitness, behavior, and social skills of autistic children. Journal of Autism and Developmental Disorders, 53(11), 4271–4279. [Google Scholar] [CrossRef]
- Hashemi, A., Zamani, M., & Saadatian, A. (2024). Effect of sensory-motor integration trainings on executive functions and social interactions of children with high functioning autism disorder. Journal of Motor Control and Learning, 6, e147293. [Google Scholar] [CrossRef]
- Hirota, T., & King, B. H. (2023). Autism spectrum disorder: A review. JAMA, 329(2), 157–168. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y., Song, Z., Deng, J., & Song, X. (2024). The impact of exercise intervention on social interaction in children with autism: A network meta-analysis. Front Public Health, 12, 1399642. [Google Scholar] [CrossRef]
- Howells, K., Sivaratnam, C., May, T., Lindor, E., McGillivray, J., & Rinehart, N. (2019). Efficacy of group-based organised physical activity participation for social outcomes in children with autism spectrum disorder: A systematic review and meta-analysis. Journal of Autism and Developmental Disorders, 49(8), 3290–3308. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C. M., & Steinhausen, H. C. (2015). Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. Attention Deficit Hyperactivity Disorder, 7(1), 27–38. [Google Scholar] [CrossRef]
- Johnson, R. B., Onwuegbuzie, A. J., & Turner, L. A. (2007). Toward a definition of mixed methods research. Journal of Mixed Methods Research, 1(2), 112–133. [Google Scholar] [CrossRef]
- Levac, D., Colquhoun, H., & O’Brien, K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5, 69. [Google Scholar] [CrossRef]
- Liu, C., Liang, X., & Sit, C. H. P. (2024). Physical activity and mental health in children and adolescents with neurodevelopmental disorders: A systematic review and meta-analysis. JAMA Pediatr, 178(3), 247–257. [Google Scholar] [CrossRef]
- Liu, Z., Chen, Y., Herold, F., Cheval, B., Falck, R. S., Kramer, A. F., Gerber, M., Werneck, A. O., An, R., Teychenne, M., Owen, N., & Zou, L. (2024). Linking social determinants of health to mental health, movement behaviors, and cognitive function among U.S. youth. Mental Health and Physical Activity, 27, 100639. [Google Scholar] [CrossRef]
- Liu, Z., Herold, F., Healy, S., Haegele, J., Block, M., Ludyga, S., Gerber, M., Werneck, A. O., An, R., Teychenne, M., Owen, N., & Zou, L. (2023). Understanding 24-hour movement guideline adherence and links to school achievement, social-behavioural problems, and emotional functioning among children and adolescents with learning disabilities. International Journal of Sport and Exercise Psychology, 27, 100639. [Google Scholar] [CrossRef]
- Masataka, N. (2017). Implications of the idea of neurodiversity for understanding the origins of developmental disorders. Physics of Life Reviews, 20, 85–108. [Google Scholar] [CrossRef] [PubMed]
- Memari, A., Mirfazeli, F., Kordi, R., Shayestehfar, M., Moshayedi, P., & Mansournia, M. (2017). Cognitive and social functioning are connected to physical activity behavior in children with autism spectrum disorder. Research in Autism Spectrum Disorders, 33, 21–28. [Google Scholar] [CrossRef]
- Merikangas, K. R., Nakamura, E. F., & Kessler, R. C. (2009). Epidemiology of mental disorders in children and adolescents. Dialogues in Clinical Neuroscience, 11(1), 7–20. [Google Scholar] [CrossRef]
- Morris, P. O., Hope, E., Foulsham, T., & Mills, J. P. (2023). Exploring the use of a dance-based exergame to enhance autistic children’s social communication skills in the home and school environments: A feasibility study. International Journal of Developmental Disabilities, 71, 141–158. [Google Scholar] [CrossRef] [PubMed]
- O’Cathain, A., Murphy, E., & Nicholl, J. (2007). Why, and how, mixed methods research is undertaken in health services research in England: A mixed methods study. BMC Health Services Research, 7, 85. [Google Scholar] [CrossRef] [PubMed]
- Padden, C., & James, J. E. (2017). Stress among parents of children with and without autism spectrum disorder: A comparison involving physiological indicators and parent self-reports. Journal of Developmental and Physical Disabilities, 29(4), 567–586. [Google Scholar] [CrossRef]
- Pan, C. Y., Chu, C. H., Tsai, C. L., Lo, S. Y., Cheng, Y. W., & Liu, Y. J. (2016). A racket-sport intervention improves behavioral and cognitive performance in children with attention-deficit/hyperactivity disorder. Research in Developmental Disabilities, 57, 1–10. [Google Scholar] [CrossRef]
- Pellicano, E., & den Houting, J. (2022). Annual Research Review: Shifting from ‘normal science’ to neurodiversity in autism science. Journal of Child Psychology and Psychiatry, 63(4), 381–396. [Google Scholar] [CrossRef]
- Peters, M., Godfrey, C., McInerney, P., Soares, C., Khalil, H., & Parker, D. (2015). Methodology for JBI scoping reviews (pp. 1–24). Joanna Briggs Institute. [Google Scholar]
- Pham, M. T., Rajic, A., Greig, J. D., Sargeant, J. M., Papadopoulos, A., & McEwen, S. A. (2014). A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Research Synthesis Methods, 5(4), 371–385. [Google Scholar] [CrossRef]
- Qi, K., Liu, Y., Wang, Z., Xiong, X., Cai, K., Xu, Y., Shi, Y., Sun, Z., Dong, X., & Chen, A. (2024). Recreational ball games are effective in improving social communication impairments among preschoolers diagnosed with autism spectrum disorder: A multi-arm controlled study. BMC Sports Science Medicine and Rehabilitation, 16(1), 176. [Google Scholar] [CrossRef]
- Qiao, Z., Sun, Z., Cai, K., Zhu, L., Xiong, X., Dong, X., Shi, Y., Yang, S., Cheng, W., Yang, Y., & Xu, D. (2024). Effects of mini-basketball training program on social communication impairments and salience network in preschool children with autism spectrum disorder. International Journal of Developmental Disabilities, 1–14. [Google Scholar] [CrossRef]
- Rivera, P., Renziehausen, J., & Garcia, J. M. (2020). Effects of an 8-week Judo program on behaviors in children with autism spectrum disorder: A mixed-methods approach. Child Psychiatry and Human Development, 51(5), 734–741. [Google Scholar] [CrossRef]
- Rollo, S., Antsygina, O., & Tremblay, M. S. (2020). The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. Journal of Sport and Health Science, 9(6), 493–510. [Google Scholar] [CrossRef]
- Sansi, A., Nalbant, S., & Ozer, D. (2021). Effects of an inclusive physical activity program on the motor skills, social skills and attitudes of students with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 51(7), 2254–2270. [Google Scholar] [CrossRef] [PubMed]
- Schoen, S., Ferrari, V., & Valdez, A. (2022). It’s not just about bicycle riding: Sensory-motor, social and emotional benefits for children with and without developmental disabilities. Children, 9(8), 1224. [Google Scholar] [CrossRef]
- So, S., Truong, S., Woodford, K., & Moore, S. (2024). “It’s such an inclusive and welcoming environment”: Caregiver perspectives of a play-based program for Autistic children and youth. Healthy Populations Journal, 4, 40. [Google Scholar]
- Taylor, A., Kong, C., Zhang, Z., Herold, F., Ludyga, S., Healy, S., Gerber, M., Cheval, B., Pontifex, M., Kramer, A. F., & Chen, S. (2023). Associations of meeting 24-h movement behavior guidelines with cognitive difficulty and social relationships in children and adolescents with attention deficit/hyperactive disorder. Child and Adolescent Psychiatry and Mental Health, 17, 42. [Google Scholar] [CrossRef]
- Thapar, A., Cooper, M., & Rutter, M. (2017). Neurodevelopmental disorders. The Lancet Psychiatry, 4(4), 339–346. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M. S., Carson, V., Chaput, J. P., Connor Gorber, S., Dinh, T., Duggan, M., Faulkner, G., Gray, C. E., Gruber, R., Janson, K., & Janssen, I. (2016). Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism = Physiologie Appliquee, Nutrition et Metabolisme, 41(Suppl. S3), S311–S327. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D., Horsley, T., Weeks, L., & Hempel, S. (2018). PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. [Google Scholar] [CrossRef]
- Tsai, L. Y. (2014). Prevalence of comorbid psychiatric disorders in children and adolescents with autism spectrum disorder. Journal of Experimental & Clinical Medicine, 6(6), 179–186. [Google Scholar] [CrossRef]
- Yin, W., Li, T., Mucha, P. J., Cohen, J. R., Zhu, H., Zhu, Z., & Lin, W. (2022). Altered neural flexibility in children with attention-deficit/hyperactivity disorder. Molecular Psychiatry, 27(11), 4673–4679. [Google Scholar] [CrossRef] [PubMed]
- Zanobini, M., & Solari, S. (2019). Effectiveness of the program “Acqua Mediatrice di Comunicazione” (Water as a Mediator of Communication) on social skills, autistic behaviors and aquatic skills in ASD children. Journal of Autism and Developmental Disorders, 49(10), 4134–4146. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S., Wang, J.-J., & Pitkethly, A. (2020). Task-efficacy predicts perceived enjoyment and subsequently barrier-efficacy: Investigation of a psychological process underpinning schoolchildren’s physical activity. International Journal of Sport and Exercise Psychology, 19, 943–956. [Google Scholar] [CrossRef]
- Zhao, M., Hou, M., Herold, F., Chen, Y., Werneck, A. O., Block, M. E., Kramer, A. F., Taylor, A., Cunha, P. M., Chaput, J.-P., Falck, R. S., Owen, N., & Zou, L. (2024). Associations of meeting 24-hour movement behavior guidelines with social and emotional function in youth with ASD/ADHD. Journal of Affective Disorders, 359, 189–195. [Google Scholar] [CrossRef]
| Study Characteristics | N | % of Studies Sampled |
|---|---|---|
| Types of research | ||
| Observational research | 12 | 24.0 |
| Intervention/experimental research | 30 | 60.0 |
| Mixed-methods research | 8 | 16.0 |
| Design | ||
| Cross-sectional | 9 | 18.0 |
| Quasi-experimental | 15 | 30.0 |
| Mixed methods | 8 | 16.0 |
| RCT | 13 | 26.0 |
| NCT | 1 | 2.0 |
| Case-controlled | 1 | 2.0 |
| Prospective case-control | 1 | 2.0 |
| Retrospective clinical | 1 | 2.0 |
| Mixed experimental design | 1 | 2.0 |
| Measure | ||
| Physical activity only | 38 | 76.0 |
| Sleep only | 8 | 16.0 |
| Sedentary behavior only | 1 | 2.0 |
| PA + SP + SB | 3 | 6.0 |
| Demographic Information | N | % of Studies Sampled | Demographic Information and Measures | N | % of Studies Sampled | |
|---|---|---|---|---|---|---|
| Nationality of study sample | Mean age of study sample * | |||||
| Australia | 3 | 6.0 | 2–7 years | 15 | 30.0 | |
| Brazil | 1 | 2.0 | 7–11 years | 26 | 52.0 | |
| Canada | 1 | 2.0 | 11–18 years | 9 | 18.0 | |
| China | 10 | 20.0 | Gender of participants | |||
| Egypt | 1 | 2.0 | Boys and girls | 35 | 70.0 | |
| India | 2 | 4.0 | Boys only | 8 | 16.0 | |
| Ireland | 1 | 2.0 | No report | 7 | 14.0 | |
| Iran | 7 | 14.0 | Key measures for neurodiversity ** | |||
| Italy | 2 | 4.0 | DSM | 24 | 48.0 | |
| Korea | 2 | 4.0 | GARS | 6 | 12.0 | |
| Spain | 1 | 2.0 | Key measures for social function ** | |||
| Switzerland | 1 | 2.0 | SRS | 8 | 16.0 | |
| Turkey | 4 | 8.0 | CBCL | 4 | 8.0 | |
| Tunisia | 1 | 2.0 | Key measures for movement behavior | |||
| USA | 11 | 22.0 | PA | CBCL | 1 | 2.0 |
| U.K. | 2 | 4.0 | GT3X monitor Actigraph | 1 | 2.0 | |
| Neurodiversity | WOTA 1 | 1 | 2.0 | |||
| ASD | 35 | 70.0 | Not assessed | 37 | 74.0 | |
| ADHD | 8 | 16.0 | SP | CSHQ | 7 | 14.0 |
| ASD+ADHD | 2 | 4.0 | PSQ | 2 | 4.0 | |
| DD | 3 | 6.0 | ST | Parent report | 1 | 2.0 |
| LD | 1 | 2.0 | ||||
| NDDs | 1 | 2.0 | ||||
| Author Location | Neurodiversity ** | Study Design | Intervention | Participants | Key Measures | Key Findings |
|---|---|---|---|---|---|---|
| Cai et al. China | ASD | Quasi-experimental | Mini-Basketball Training Program, MBTP (40 min, 5 days per week for 12 weeks) | 30 children (26 boys and 4 girls), 15 each in intervention and control groups. | PA: NA ND: CARS SF: SRS | The 12-week MBTP significantly improved social communication abilities in preschool children with ASD. |
| Cei et al. Italy | ASD | Mixed methods | Football Program (120 min, 2 days per week for 32 weeks) | 90 children aged 7–18. | PA: NA ND: DSM SF: ASSM | Quantitative results showed no improvement in social functioning, while qualitative results indicated enhancements in psychosocial skills, including communication and social interaction. |
| Coffey et al. Ireland | ASD | Quasi-experimental | Integrative exercise (60 min, 3 days per week for 8 weeks) | 66 children (55 boys and 11 girls), aged 4–12. | PA: NA ND: GARS SF: ABC | Integrative exercise can significantly reduce social withdrawal and related behaviors in children with severe ASD symptoms. |
| Dovgan et al. Australia | ASD | Cross-sectional | NA | 129 children aged 6–18. | PA: CBCL ND: ADI-R and ADOS SF: VABS and CBCL | In children with ASD, more activity participation was linked to more friendships, while higher IQs correlated with greater internalization of social difficulties. |
| Firouzjah et al. Iran | ASD | Quasi-experimental | Sensory–motor integration exercises (45 min, 3 days per week for 4 weeks) | 30 children (all boys), 15 each in intervention and control groups. | PA: NA ND: doctor’s diagnosis SF: SSRS | Sensory–motor integration exercises significantly improved social skills, including determination, cooperation, and self-control, in children with ASD. |
| Goldman et al. USA | ASD | Cross-sectional | NA | 1784 children, aged 2–18. | SP: CSHQ ND: ADOS SF: PCQ | Sleep problems are strongly linked to daytime behavioral issues, including impaired social functioning, in children with ASD. |
| Güeita-Rodríguez et al. Spain | ASD | Mixed methods | Water Specific Therapy, WST (60 min, 2 days per week for 28 weeks) | 6 children (5 boys and 1 girl), aged 6–12. | PA: NA ND: DSM SF: PSPCSA and PedsQL | Quantitative results showed no improvement in peer or maternal acceptance, while qualitative results noted better social communication and interaction in children with ASD after the WST intervention. |
| Gundogmus et al. Turkey | ASD | Case-controlled | NA | 60 adolescents (34 boys and 26 girls), 30 each in intervention and control groups, aged 10–15. | PA: NA ND: ABC SF: SSAS | Children with ASD who participate in physical activity show better social skills and behaviors compared to those who do not. |
| Özcan et al. UK | ASD | RCT | Motor Intervention Program, MIP (60 min, 2 days per week for 12 weeks) | 34 children (32 boys and 2 girls), 17 each in intervention and control groups, aged 3–6. | PA: NA ND: GARS SF: SSRS | MIP significantly enhanced social skills in children with ASD, particularly in cooperation, self-control, and social interaction. |
| Haghighi et al. Iran | ASD | RCT | Combined Physical Training, CPT (80 min, 3 days per week for 8 weeks) | 16 children (9 boys and 7 girls), 8 each in intervention and control groups, aged 6–10. | PA: NA ND: GARS SF: GARS | CPT significantly enhances social skills in children with ASD by reducing stereotypical behaviors and improving communication. |
| Hashemi et al. Iran | ASD | Quasi-experimental | Sensory–motor integration training (60 min, 3 days per week for 8 weeks) | 50 children (all boys), 25 each in intervention and control groups, aged 7–12. | PA: NA ND: GARS SF: GARS | Sensory–motor integration training significantly improves social interactions and communication skills in children with high-functioning autism. |
| Heffler et al. USA | ASD | Quasi-experimental | Comprehensive Intervention (60 min, 2 days per week for 24 weeks) | 9 children (8 boys and 1 girl), aged 1.5–3.5. | ST: parent report ND: ADOS SF: VABS | Interventions that reduce screen time and increase social interaction can significantly improve the social skills of children with ASD. |
| Howells et al. Australia | ASD | Quasi-experimental | Auskick (60–90 min, 1 day per week for 6–22 weeks (average 12 weeks)) | 40 children (37 boys and 3 girls), 19 in intervention and 21 in control group, aged 5–12. | PA: NA ND: DSM SF: VABS-3 and CBCL | Children with ASD in the Auskick program showed significant improvements in social skills, particularly in reducing negative experiences like loneliness and dependency. |
| Kaur et al. USA | ASD | RCT | Yoga Exercise and Academic Activities (75 min, 4 days per week for 8 weeks) | 24 children (21 boys and 3 girls), 12 each in yoga and academic groups, aged 5–13. | PA: NA ND: ADOS SF: SCBE | Creative yoga interventions significantly improve verbal communication, joint attention, and social skills, and reduced negative emotions in children with ASD. |
| Lee et al. China | ASD | Quasi-experimental | Cooperative physical activities (25 min, 3 days per week for 16–20 weeks) | 3 children aged 2–5. | PA: NA ND: DSM SF: teacher report | Cooperative physical activities improve social interactions and may reduce inappropriate behaviors in preschoolers with ASD during physical education and free play. |
| Lee et al. USA | ASD | Quasi-experimental | Movement-based intervention program (75 min, 2 days per week for 8 weeks) | 19 children (16 boys and 3 girls), aged 5–16. | PA: NA ND: doctor’s diagnosis SF: SSIS | Engagement in a movement-based intervention program resulted in significant improvements in physical activity-related social skills among children with ASD. |
| Marzouki et al. Tunisia | ASD | RCT | Technical Aquatic Training, TAT; Game-Based Aquatic Training, GAT (50 min, 2 days per week for 8 weeks) | 22 children (20 boys and 2 girls), 8 each in TAT and GAT groups, and 7 in control group, aged 6–7. | PA: NA ND: DSM SF: GARS | Both types of aquatic training can improve social functioning in children with ASD by reducing stereotypical behaviors and providing opportunities for social interaction. |
| Memari et al. Iran | ASD | Cross-sectional | NA | 68 children (42 boys and 26 girls), aged 6–16. | PA: GT3X monitor Actigraph ND: DSM SF: ASSP | Higher levels of physical activity are associated with better social functioning in children with ASD. |
| Mohamed et al. Egypt | ASD | RCT | Group exercise (60 min, 3 days per week for 12 weeks) | 30 children (24 boys and 6 girls), 15 each in intervention and control groups, aged 8–10. | PA: NA ND: DSM SF: ASSP | Group exercise programs significantly improve social skills in children with ASD. |
| Morris et al. UK | ASD | Mixed methods | Just Dance: home-based (25 min, 2 days per week for 6 weeks); school-based (10 min, 2 days per week for 6 weeks) | 35 children (26 boys and 9 girls), 4 in home-based and 31 in school-based intervention, aged 8–10. | PA: NA ND: DSM SF: ERSSQ | Quantitative results showed improved social communication skills in children with ASD after the Just Dance intervention, while qualitative findings noted its enjoyment and ease of implementation. |
| Movahedi et al. Iran | ASD | RCT | Kata technique training (30–90 min, 4 days per week for 14 weeks) | 30 children (26 boys and 4 girls), 15 each in intervention and control groups, aged 5–16. | PA: NA ND: DSM SF: GARS | Kata technique training improved social skills, emotional regulation, and social engagement in children with ASD. |
| Najafabadi et al. Iran | ASD | Quasi-experimental | Sports, Play and Active Recreation for Kids, SPARK (40 min, 3 days per week for 12 weeks) | 26 children (all boys), 12 in intervention and 14 in control group, aged 5–12. | PA: NA ND: DSM SF: GARS and ATEC | The 12-week SPARK program effectively enhances the social interaction skills of children with autism spectrum disorders. |
| Narasingharao et al. India | ASD | Quasi-experimental | Structured yoga (75 min, 1 day per week for 12 weeks) | 64 children (all boys), 32 each in intervention and control groups, aged 5–16. | PA: NA ND: ICD-10 SF: self-developed questionnaire | A structured yoga intervention improved social skills in children with ASD, reducing aggression and self-injury and enhancing eye contact and social interactions. |
| Pan et al. China | ASD | Mixed methods | Water Exercise Swimming Program, WESP (45 min, 2 days per week for 10 weeks) | 16 children (all boys), 8 each in intervention and control groups, aged 6–9. | PA: NA ND: DSM SF: SSBS | Quantitative findings showed that the WESP improved social interactions and behaviors in children with ASD, while qualitative findings revealed more positive daily social behaviors. |
| Phung et al. USA | ASD | RCT | Mixed Martial Arts, MMA (45 min, 2 days per week for 13 weeks) | 34 children (28 boys and 6 girls), 14 in intervention and 20 in control group, aged 8–11. | PA: NA ND: ADOS and SCQ SF: SSIS | The MMA intervention significantly enhanced social skills and reduced negative social behaviors in boys with ASD. |
| Qiao et al. China | ASD | Mixed experimental design | Mini-Basketball Training, MBTP (40 min, 5 days per week for 12 weeks) | 34 children (29 boys and 5 girls), 19 in intervention group and 15 in control group, aged 3–6. | PA: NA ND: DSM SF: SRS | A 12-week mini-basketball program improves social cognition in preschool children with ASD. |
| Qi et al. China | ASD | RCT | Ball Combination Training, BCT, and Mini-Basketball Training, MBT (40–45 min, 5 days per week for 12 weeks) | 41 children (35 boys and 6 girls), 13 in intervention group 1, 14 in intervention group 2, and 14 in control group, aged 4.23–5.76. | PA: NA ND: doctor’s diagnosis SF: SRS | Children with ASD in BCT and MBT showed greater improvements in social communication than those receiving standard rehabilitation. |
| Rivera et al. USA | ASD | Mixed methods | Judo Program (45 min, 1 day per week for 8 weeks) | 25 children (22 boys and 3 girls), aged 8–17 (12.67). | PA: NA ND: doctor’s diagnosis SF: ABC | Quantitative analysis found no behavioral improvements, while qualitative feedback from parents indicated improvements in social skills and self-esteem. |
| Sansi et al. Turkey | ASD | Mixed methods | Inclusive Physical Activity, IPA (60 min, 2 days per week for 12 weeks) | 45 children (22 boys and 23 girls), 13 in intervention and 9 in control group for ASD, 14 in intervention and 9 in control group for TD, aged 6–11. | PA: NA ND: SSRS SF: SSRS, FAS, and ACL | Quantitative analyses found no improvement in social skills, while qualitative results indicated IPA’s effectiveness in developing social skills in children with ASD. |
| Toscano et al. Brazil | ASD | NCT | Physical exercise (48 min, 2 days per week for 48 weeks) | 229 children (196 boys and 33 girls), 127 in intervention group, 62 in control group 1, and 40 in control group 2, aged 2.3–17.3. | PA: NA ND: DSM SF: ATA | Physical exercise significantly improved social functioning in children and adolescents with ASD, especially in social interaction, attention, and behavior. |
| Wang et al. China | ASD | Quasi-experimental | Mini-Basketball Training Program, MBTP (40 min, 5 days per week for 12 weeks) | 33 children (28 boys and 5 girls), 18 in intervention and 15 in control group, aged 3–6. | PA: NA ND: DSM SF: SRS | MBTP significantly enhanced social communication skills and reduced repetitive behaviors in children with ASD. |
| Yang et al. China | ASD | Quasi-experimental | Mini-Basketball Training Program, MBTP (40 min, 5 days per week for 12 weeks) | 30 children (25 boys and 5 girls), 15 each in intervention and control groups, aged 3–6. | PA: NA ND: DSM SF: SRS | MBTP improved social communication skills in children with ASD, particularly in the social cognition and social communication dimensions. |
| Yang et al. China | ASD | Quasi-experimental | Mini-Basketball Training Program, MBTP (40 min, 5 days per week for 12 weeks) | 30 children (26 boys and 4 girls), 15 each in intervention and control groups, aged 3–6. | PA: NA ND: DSM SF: SRS | MBTP significantly reduced social communication deficits in children with ASD, particularly in social cognition and autistic behavior patterns. |
| Zanobini et al. Italy | ASD | RCT | Acqua Mediatrice di Comunicazione (30 min, 1 day per week for 12 weeks) | 25 children (19 boys and 6 girls), 13 in intervention and 12 in control group, aged 3–8. | PA:NA ND: ABC SF: SRS | The "Acqua Mediatrice di Comunicazione" swimming program enhanced social skills in children with ASD, with benefits sustained six months post-intervention. |
| Zhao et al. China | ASD | Quasi-experimental | Structured physical activity program (60 min, 2 days per week for 12 weeks) | 41 children (29 boys and 12 girls), 21 in intervention and 20 in control group, aged 5–8. | PA: NA ND: DSM SF: SSIS and ABLLS-R | Structured physical activity programs significantly improve social interaction, communication, responsiveness, and expression in children with ASD. |
| Craig et al. Canada | ADHD | Cross-sectional | NA | 192 children, mean age is 10.23. | SP: PSQ ND: SNAP-Iv SF: WFIRS-P | Sleep problems, especially insomnia and daytime sleepiness, significantly affect social functioning in children with ADHD. |
| Keshavarzi et al. Iran | ADHD | RCT | Sleep training (once a week for 12 weeks) | 40 children (38 boys and 2 girls), 20 each in intervention and control groups, aged 8–13. | SP: CSHQ ND: DSM SF: KID-SCREEN-52 | A twelve-week sleep training enhances sleep quality and social behavior, as well as emotional and behavioral functioning, in children with ADHD. |
| Lucas et al. Australia | ADHD | Cross-sectional | NA | 257 children (189 boys and 68 girls), aged 5–13. | SP: CSHQ ND: DSM SF: SDQ | In children with ADHD, daytime sleepiness was linked to social difficulties at school, while parent-reported sleep problems showed no significant association. |
| Majorek et al. Switzerland | ADHD | Quasi-experimental | Therapeutic Eurythmy, TE (30 min, 1 day per week for 36 weeks) | 5 children (all boys), aged 8.5–10. | PA: NA ND: doctor’s diagnosis SF: CRS | TE significantly enhances social behavior and reduces hyperactivity symptoms in children with ADHD. |
| Pan et al. China | ADHD | RCT | Table Tennis Exercise (70 min, 2 days per week for 24 weeks) | 32 children (all boys), 16 each in intervention and control groups, aged 6–12 (8.9). | PA: NA ND: DSM SF: CBCL | The table tennis training program significantly reduced social problems and aggression in children with ADHD, with lasting improvements. |
| Sahin et al. Turkey | ADHD | Cross-sectional | NA | 85 children (55 boys and 30 girls), aged 7–12 (9.49). | SP: CSHQ ND: DSM SF: TBAG, FPRT and RMET | Sleep disorders are linked to decreased social cognitive abilities in children with ADHD, potentially affecting social functioning. |
| Shah et al. India | ADHD | RCT | Sleep training (face-to-face sessions: weeks 2, 4, 8, total of 12 weeks; telephone sessions: 45 min, weeks 1, 3, 6, 10 total, 12 weeks) | 100 children, 50 each in intervention and control groups, aged 8–12 (10.66). | SP: CSHQ ND: DSM SF: SDQ and PQLI | The sleep training program significantly improved sleep quality, quality of life, and social, emotional, behavioral, and executive functioning in children with ADHD. |
| Taylor et al. USA | ADHD | Cross-sectional | NA | 3470 children (2376 boys and 1094 girls), aged 6–17 (11.97). | PA: NA ND: NA SF: NA | Meeting the 24 h movement behavior guidelines is linked to improved social cognition and reduced social difficulties in children with ADHD. |
| Ng et al. USA | ADHD + ASD | Retrospective clinical | NA | 114 children (93 boys and 21 girls), aged 7–17 (11.26). | SP: PSQ ND: DSM SF: CBCL | Sleep disorders are strongly linked to behavioral and emotional regulation problems in children with ASD and ADHD. |
| Zhao et al. USA | ASD + ADHD | Cross-sectional | NA | 979 children (795 boys and 184 girls), aged 6–17 (12.3). | PA: NA ND: NA SF: NA | Adhering to 24 h movement guidelines, particularly sleep and screen time, was strongly linked to improved social functioning in children with ASD and ADHD. |
| Meng et al. Korea | DD | RCT | Service-learning soccer training (90 min, 1 day per week for 12 weeks) | 36 children (all boys), 18 each in intervention and control groups, mean age 11.5. | PA: NA ND: doctor’s diagnosis SF: KBASC | The service-learning soccer training program helps improve the social skills and self-regulation of children with developmental disabilities. |
| Oh et al. Korea | DD | Mixed methods | Parent-led Aquatic Activities (60 min, 2 days per week for 8 weeks) | 14 children (9 boys and 5 girls), aged 9–15 (11.07). | PA: NA ND: doctor’s diagnosis SF: KNISE-SAB | Quantitative results showed no impact of parent-led water activities on social behaviors, while qualitative findings highlighted parental involvement in boosting resilience. |
| Schoen et al. USA | DD | Mixed methods | Bicycle Riding Training (60 min per week for 5 days) | 19 children (12 boys and 7 girls), aged 4.43–10.6 (6.49). | PA: NA ND: SP3D SF: SP3D and VAS | The Bicycle Riding Program enhances the social skills and self-esteem of children with developmental disabilities. |
| Z. Liu et al. USA | LD | Cross-sectional | NA | 4999 children aged 6–17 (12.0, gender not reported). | PA: NA ND: NA SF: NA | Adherence to 24 h movement guidelines is linked to improved social functioning and emotional wellbeing in children with learning disabilities. |
| Kara et al. Turkey | NDDs | Prospective case-control | NA | 317 children (211 boys and 106 girls), 166 in case and 151 in control group, aged 4–6. | SP: CSHQ ND: DSM SF: SCBE | Sleep disturbances in children with neurodevelopmental disorders are strongly linked to social deficits and behavioral issues, including aggression and anxiety. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, C.; Liu, P.; Yang, Z.; Yin, L.; Zhang, S. Twenty-Four-Hour Movement Behaviors and Social Functions in Neurodiverse Children: A Scoping Review. Behav. Sci. 2025, 15, 592. https://doi.org/10.3390/bs15050592
Fan C, Liu P, Yang Z, Yin L, Zhang S. Twenty-Four-Hour Movement Behaviors and Social Functions in Neurodiverse Children: A Scoping Review. Behavioral Sciences. 2025; 15(5):592. https://doi.org/10.3390/bs15050592
Chicago/Turabian StyleFan, Chengwen, Pan Liu, Zongyu Yang, Liqin Yin, and Shuge Zhang. 2025. "Twenty-Four-Hour Movement Behaviors and Social Functions in Neurodiverse Children: A Scoping Review" Behavioral Sciences 15, no. 5: 592. https://doi.org/10.3390/bs15050592
APA StyleFan, C., Liu, P., Yang, Z., Yin, L., & Zhang, S. (2025). Twenty-Four-Hour Movement Behaviors and Social Functions in Neurodiverse Children: A Scoping Review. Behavioral Sciences, 15(5), 592. https://doi.org/10.3390/bs15050592






