Therapeutic Approach in Language and Cognitive Skills in Premature Twins with ASD: Case Report
Abstract
1. Introduction
2. Description of the Cases
2.1. Perinatal and Family History
2.2. Development History
3. Method
3.1. Study Design
3.2. Participants
3.3. Instruments
- (a)
- Merrill-Palmer scales development (Dempsey et al., 2020): The Global Development Index provides a broad measure of development, while the Adaptive Behavior Index evaluates functional skills in daily life. Internal consistency ranges from 0.85 to 0.94. It was chosen for its ability to capture global developmental patterns and adaptive functioning relevant to early intervention planning. Subtests include cognitive, motor, language, socioemotional, and adaptive domains.
- (b)
- The Adaptive Behavior Assessment System (ABAS-II; Harrison et al., 2013): Assesses adaptive behavior from birth to 89 years. The Global Adaptive Composite (GAC) shows very high internal consistency (0.97–0.99) and high reliability for adaptive domains (0.91–0.98). It evaluates functional independence across conceptual, social, and practical domains, providing relevant information on real-life skills for intervention targeting.
- (c)
- The Behavior Rating Inventory of Executive Function (BRIEF-2; Bausela-Herreras & Luque-Cuenca, 2017): Evaluates observable executive functions in children 5–18 years. Internal consistency coefficients range from 0.80 to 0.98. Selected to measure attention, working memory, planning, and self-regulation in everyday contexts.
- (d)
- Neuropsychological assessment services (Neuro-kid; Portellano Pérez et al., 2021): Screens global development in children 3–7 years, assessing essential cognitive domains for evolutionary development.
- (e)
- Developmental Profile-3 (DP-3; Alpern, 2018): Rapidly assesses cognition, motor skills, socioemotional development, communication, and adaptive behavior in children. Internal consistency ranges from 0.89 to 0.97. Provides a global index of child development.
- (f)
- Child and Adolescent Assessment System (SENA; Rodríguez Camón, 2018): Detects disorders and difficulties that occur at various stages of development, from age 3 up to adulthood. Internal consistency coefficients range from 0.77 to 0.96. The tool has been developed to address the challenges most commonly encountered at each stage of development.
- (g)
- The Clinical Evaluation of Language Fundamentals—5 (CELF-5; Wiig et al., 2018): Individually administered assessment of language in children aged 5–15 years. Internal consistency ranges from 0.75 to 0.98. Provides detailed evaluation of expressive language such as lexis, morphosyntax, semantics, and pragmatics, as well as receptive language.
- (h)
- The Illinois Test of Psycholinguistic Aptitudes (ITPA; Kirk et al., 2009): Evaluates linguistic processing and communication skills in children aged 3–10 years. Internal consistency ranges from 0.80 to 0.92. Used to identify strengths and weaknesses in language processing relevant to the intervention’s design.
3.4. Procedure
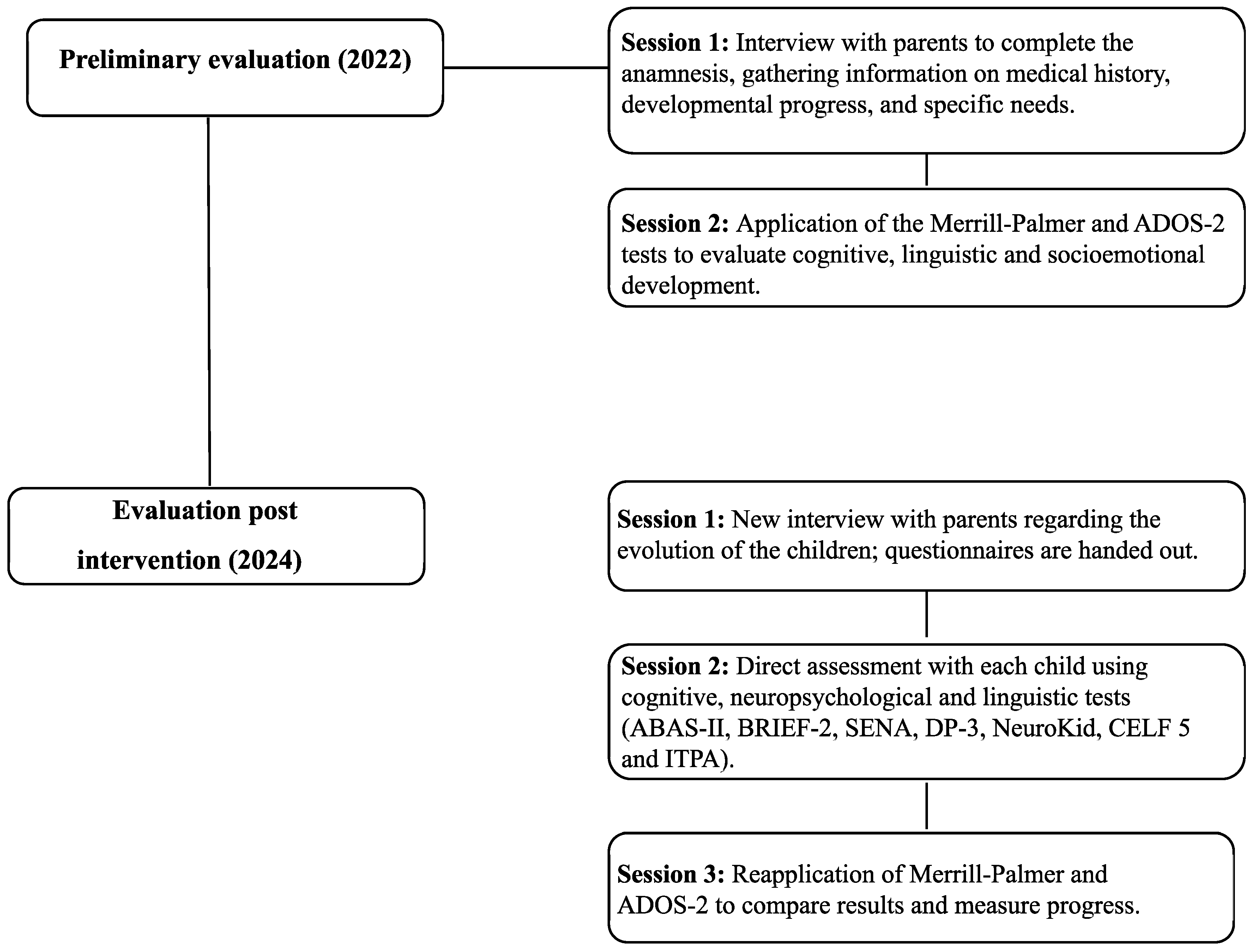
3.4.1. Assessment Procedure
- Session 1: Parent interview to obtain family history, perinatal and developmental information, and anamnesis. This session ensured comprehensive background knowledge to contextualize the twins’ developmental profiles.
- Session 2: Direct assessment of each child using Merrill-Palmer Developmental Scales. These instruments were applied pre-intervention to establish baseline profiles in cognitive, linguistic, and socioemotional domains, allowing for subsequent comparison with post-intervention outcomes.
- Session 1: Follow-up parent interview focusing on developmental progress and intervention effects.
- Session 2: Direct evaluation using ABAS-II, BRIEF-2, SENA, Neuro-Kid, DP-3, CELF-5, and ITPA. These instruments were chosen to provide a detailed profile of cognitive, linguistic, adaptive, and socioemotional outcomes, reflecting changes potentially attributable to the intervention.
- Session 3: Re-administration of Merrill-Palmer to allow for a direct comparison between pre- and post-intervention performance and assess longitudinal changes.
3.4.2. Intervention Procedure
Cognitive Intervention
- ABA Model: Structured tasks using forward and backward chaining were applied with immediate positive reinforcement (verbal praise, tokens, or extra playtime). Examples included simple problem-solving, sustained attention activities (e.g., object search and image matching), and adaptive behavior routines to promote autonomy and tolerance to changes.
- TEACCH Method: The cognitive environment was structured with visual materials to help the understanding of daily and school activities, promote autonomy, and reduce anxiety. Visual schedules, independent task folders, and manipulative materials were used to promote predictability, organization, and independence.
- DIR/Floortime approach: It allowed us to work on cognitive development in motivating and meaningful play contexts, favoring problem solving in a natural way and linked to the individual interests of each child. This facilitated the integration of cognitive functions with the emotional and social dimensions, fundamental aspects for the development of mental flexibility and symbolic thinking. Activities included guided play following children’s interests, the creation of “communication circles”, and symbolic play to encourage flexible thinking and emotional regulation.
Linguistic Intervention
- ABA model: Applied verbal shaping, echoic training, and reinforcement techniques. Structured tasks targeted naming, categorization, sentence construction, and comprehension through visual prompts.
- TEACCH: Provided visual and routine-based supports to aid understanding, such as communication boards, “First–Then” routines, and story sequencing.
- DIR/Floortime: Promoted the development of language in its functional and social dimension, addressing pragmatic aspects, the use of gestures, non-verbal language and symbolic functions, in emotionally meaningful play contexts. Symbolic games, role-play, and turn-taking activities enhanced intentional communication and social reciprocity.
- The Hannen program involved the parents, teaching them language stimulation strategies through guided sessions, home recordings, and joint analysis of interactions. This allowed for a reinforcement of the achievements of the therapeutic approach in daily life and for the generation of an environment rich in communicative opportunities.
Socioemotional Focus
4. Results
4.1. Development and Maturational Profile
- PATIENT 1—JR
- PATIENT 2—SR
4.2. Cognitive Development and Profile
- PATIENT 1—JR
- PATIENT 2—SR
4.3. Linguistic Development and Profile
- PATIENT 1—JR
- PATIENT 2—SR
4.4. Differential Diagnosis
- PATIENT 1—JR
- PATIENT 2—SR
4.5. Analysis of Comorbidities
- PATIENT 1—JR
- PATIENT 2—SR
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Allen, L., Leon-Attia, O., Shaham, M., Shefer, S., & Gabis, L. V. (2020). Autism risk linked to prematurity is more accentuated in girls. PLoS ONE, 15(8), e0236994. [Google Scholar] [CrossRef]
- Alpern, G. D. (2018). DP-3, perfil de desarrollo—3: Manual (F. Sánchez-Sánchez, Adapt.). TEA Ediciones. [Google Scholar]
- Bausela-Herreras, E., & Luque-Cuenca, T. (2017). Evaluación conductual de la función ejecutiva-versión infantil (BRIEF-P, versión española): Fiabilidad y validez. Acta de Investigación Psicológica, 7(3), 2811–2822. [Google Scholar] [CrossRef]
- Cano-Villagrasa, A., Moya-Faz, F. J., & López-Zamora, M. (2023). Relationship of epilepsy on the linguistic-cognitive profile of children with ASD: A systematic review of the literature. Frontiers in Psychology, 14, 1101535. [Google Scholar] [CrossRef]
- Cano-Villagrasa, A., Porcar-Gozalbo, N., López-Chicheri, I., & López-Zamora, M. (2024). Executive functioning and language in a pediatric population with autism spectrum disorders and epilepsy: A comparative study. Children, 11(3), 306. [Google Scholar] [CrossRef]
- Cooper, J. O., Heron, T. E., & Heward, W. L. (2019). Applied behavior analysis (3rd ed.). Pearson. [Google Scholar]
- Dempsey, E. E., Smith, I. M., Flanagan, H. E., Duku, E., Lawrence, M. A., Szatmari, P., Zwaigenbaum, L., Vaillancourt, T., Volden, J., Mirenda, P., Waddell, C., Georgiades, S., Elsabbagh, M., Ungar, W. J., & Bennett, T. (2020). Psychometric properties of the Merrill-Palmer-Revised scales of development in preschool children with autism spectrum disorder. Assessment, 27(8), 1796–1809. [Google Scholar] [CrossRef]
- Foster-Cohen, S., Edgin, J. O., Champion, P. R., & Woodward, L. J. (2007). Early delayed language development in very preterm infants: Evidence from the MacArthur-Bates CDI. Journal of Child Language, 34(3), 655–675. [Google Scholar] [CrossRef] [PubMed]
- Giuffrè, M., Piro, E., & Corsello, G. (2012). Prematurity and twinning. The Journal of Maternal-Fetal & Neonatal Medicine, 25(Suppl. 3), 6–10. [Google Scholar] [CrossRef] [PubMed]
- Harel-Gadassi, A., Friedlander, E., Yaari, M., Bar-Oz, B., Eventov-Friedman, S., Mankuta, D., & Yirmiya, N. (2018). Risk for ASD in preterm infants: A three-year follow-up study. Autism Research and Treatment, 2018, 8316212. [Google Scholar] [CrossRef]
- Hariningtyas, N. H., Kusmiyati, Y., Djanah, N., & Apay, S. E. (2022). Prematurity and language development of 9–18 months child: A correlation study. Jurnal Kesehatan Ibu Dan Anak, 16(1), 56–63. [Google Scholar] [CrossRef]
- Harrison, P. L., Oakland, T., Montero Centeno, D., & Fernández-Pinto, I. (2013). ABAS II: Sistema para la evaluación de la conducta adaptativa. TEA. [Google Scholar]
- Joseph, R. M., Lai, E. R., Bishop, S., Yi, J., Bauman, M. L., Frazier, J. A., Santos, H. P., Jr., Douglas, L. M., Kuban, K. K. C., Fry, R. C., & O’Shea, T. M. (2023). Comparing autism phenotypes in children born extremely preterm and born at term. Autism Research: Official Journal of the International Society for Autism Research, 16(3), 653–666. [Google Scholar] [CrossRef]
- Joseph, R. M., O’Shea, T. M., Allred, E. N., Heeren, T., Hirtz, D., Paneth, N., Leviton, A., & Kuban, K. C. K. (2017). Prevalence and associated features of autism spectrum disorder in extremely low gestational age newborns at age 10 years. Autism Research: Official Journal of the International Society for Autism Research, 10(2), 224–232. [Google Scholar] [CrossRef]
- Kalish, B. T., Angelidou, A., & Stewart, J. (2017). Autism spectrum disorder in preterm children. NeoReviews, 18(7), e431–e437. [Google Scholar] [CrossRef]
- Kirk, S., McCarthy, J., & Kirk, W. (2009). Test de Illinois de Aptitudes Psicolingüísticas (S. Ballesteros, & A. Cordero, Trans.; 7th ed.). TEA Ediciones. [Google Scholar]
- Liao, S.-T., Hwang, Y.-S., Chen, Y.-J., Lee, P., Chen, S.-J., & Lin, L.-Y. (2014). Home-based DIR/Floortime™ intervention program for preschool children with autism spectrum disorders: Preliminary findings. Physical & Occupational Therapy in Pediatrics, 34(4), 356–367. [Google Scholar] [CrossRef]
- Lord, C., Brugha, T. S., Charman, T., Cusack, J., Dumas, G., Frazier, T., Jones, E. J. H., Jones, R. M., Pickles, A., State, M. W., Taylor, J. L., & Veenstra-VanderWeele, J. (2020). Autism spectrum disorder. Nature Reviews Disease Primers, 6(1), 5. [Google Scholar] [CrossRef] [PubMed]
- Luu, J., Jellett, R., Yaari, M., Gilbert, M., & Barbaro, J. (2020). A comparison of children born preterm and full-term on the autism spectrum in a prospective community sample. Frontiers in Neurology, 11, 597505. [Google Scholar] [CrossRef] [PubMed]
- Maggiolo, L. M., Varela, M. V., Arancibia, S. C., & Ruiz, M. F. (2014). Dificultades de lenguaje en niños preescolares con antecedente de prematuridad extrema. Revista Chilena de Pediatria, 85(3), 319–327. [Google Scholar] [CrossRef] [PubMed]
- March of Dimes. (2020). The grants register 2021 (p. 545). Palgrave Macmillan. [Google Scholar]
- Meçe, D., & Sherifi, E. (2022). Effectiveness of the ABA method and individual education programs for the treatment of autistic children: A case study. Journal of Educational and Social Research, 12(3), 182. [Google Scholar] [CrossRef]
- Nowakowski-Sims, E., & Gregan, A. (2017). Touching autism through DIRFloortime®. In Touch in child counseling and play therapy (pp. 76–88). Routledge. [Google Scholar]
- Ouss-Ryngaert, L., Alvarez, L., & Boissel, A. (2012). Autisme et prématurité: État des lieux. Archives de Pediatrie: Organe Officiel de la Societe Francaise de Pediatrie, 19(9), 970–975. [Google Scholar] [CrossRef]
- Portellano Pérez, J. A., Mateos Mateos, R., & Martínez-Arias, R. (2021). NEURO-KID. Screening neuropsicológico infantil. TEA Ediciones. [Google Scholar]
- Reidy, N., Morgan, A., Thompson, D. K., Inder, T. E., Doyle, L. W., & Anderson, P. J. (2013). Impaired language abilities and white matter abnormalities in children born very preterm and/or very low birth weight. The Journal of Pediatrics, 162(4), 719–724. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Camón, E. (2018, March 1). El SENA: Un sistema de evaluación clínica eficaz en población infanto-juvenil. Portal Psicología y Mente. Available online: https://psicologiaymente.com/clinica/SENA-evaluacion-clinica (accessed on 11 November 2025).
- Rogers, C. E., Lean, R. E., Wheelock, M. D., & Smyser, C. D. (2018). Aberrant structural and functional connectivity and neurodevelopmental impairment in preterm children. Journal of Neurodevelopmental Disorders, 10(1), 38. [Google Scholar] [CrossRef]
- Roman, A., Ramirez, A., & Fox, N. S. (2022). Screening for preterm birth in twin pregnancies. American Journal of Obstetrics & Gynecology MFM, 4(2S), 100531. [Google Scholar] [CrossRef]
- Rosenberg, R. E., Law, J. K., Yenokyan, G., McGready, J., Kaufmann, W. E., & Law, P. A. (2009). Characteristics and concordance of autism spectrum disorders among 277 twin pairs. Archives of Pediatrics & Adolescent Medicine, 163(10), 907–914. [Google Scholar] [CrossRef]
- Sansavini, A., Guarini, A., Zuccarini, M., Lee, J. Z., Faldella, G., & Iverson, J. M. (2019). Low rates of pointing in 18-month-olds at risk for Autism spectrum disorder and extremely preterm infants: A common index of language delay? Frontiers in Psychology, 10, 2131. [Google Scholar] [CrossRef] [PubMed]
- Schopler, E., Mesibov, G. B., & Hearsey, K. (1995). Structured teaching in the TEACCH system. In E. Schopler, & G. B. Mesibov (Eds.), Learning and cognition in autism (pp. 243–268). Springer. [Google Scholar]
- Souza, A. C. F., Casais-e-Silva, L. L., & Sena, E. P. d. (2019). Description of the linguistic and neurological findings of twins born preterm at two years of age. Journal of Human Growth and Development, 29(3), 338–345. [Google Scholar] [CrossRef]
- Sussman, F. (2012). More than words: Helping parents promote communication and social skills in children with autism spectrum disorder. SAGE Publications. [Google Scholar]
- Vandormael, C., Schoenhals, L., Hüppi, P. S., Filippa, M., & Borradori Tolsa, C. (2019). Language in preterm born children: Atypical development and effects of early interventions on neuroplasticity. Neural Plasticity, 2019, 6873270. [Google Scholar] [CrossRef]
- Wiig, E. H., Semel, E., & Secord, W. A. (2018). CELF-5: Evaluación clínica de los fundamentos del lenguaje [Versión española]. Pearson Educación. [Google Scholar]
- Zeng, H., Liu, S., Huang, R., Zhou, Y., Tang, J., Xie, J., Chen, P., & Yang, B. X. (2021). Effect of the TEACCH program on the rehabilitation of preschool children with autistic spectrum disorder: A randomized controlled trial. Journal of Psychiatric Research, 138, 420–427. [Google Scholar] [CrossRef] [PubMed]
| Area | 2022—PT/PC/EE | 2024—PT/PC/EE |
Interpretation (Post-Intervention) |
|---|---|---|---|
| MP Global Development | 96/39/47 months | 102/55/51 months | Average |
| MP Adaptive Behavior | 26/2/20 months | 40/9/28 months | Very low |
| ABAS-II Conceptual | - | 64/1/- | Very low |
| ABAS-II Social | - | 56/<1/- | Very low |
| ABAS-II Practical | - | 58/<1/- | Very low |
| ABAS-II Adaptive Behavior | - | 57/<1/- | Very low |
| BRIEF-2 Behavioral Regulation | - | 66/2/- | Very low |
| BRIEF-2 Emotional Regulation | - | 71/4/- | Very low |
| DP-3 Adaptative Behavior | - | 112/79/- | High average |
| DP-3 Socioemotional | - | 88/21/- | Low |
| SENA Behavioral Problems | - | 67/4/- | Low |
| SENA Emotional Problems | - | 77/9/- | Low average |
| SENA Personal Resources | - | 15/<1/- | Very low |
| Area | 2022—PT/PC/EE | 2024—PT/PC/EE |
Interpretation (Post-Intervention) |
|---|---|---|---|
| MP Global Development | 101/53/46 months | 110/75/54 months | High average |
| MP Adaptive Behavior | 68/25/30 months | 80/40/40 months | Low average |
| ABAS-II Conceptual | - | 64/1/- | Very low |
| ABAS-II Social | - | 56/<1/- | Very low |
| ABAS-II Practical | - | 58/<1/- | Very low |
| ABAS-II Adaptive Behavior | - | 57/<1/- | Very low |
| BRIEF-2 Behavioral Regulation | - | 93/32/- | Very low |
| BRIEF-2 Emotional Regulation | - | 99/47/- | Very low |
| DP-3 Adaptative Behavior | - | 50/1/- | Very low |
| DP-3 Socioemotional | - | 50/1/- | Very low |
| SENA Behavioral Problems | - | 69/5/- | Low average |
| SENA Emotional Problems | - | 57/2/- | Very low |
| SENA Personal Resources | - | 25/<1/- | Very low |
| Area | 2022—PT/PC/EE | 2024—PT/PC/EE |
Interpretation (Post-Intervention) |
|---|---|---|---|
| MP Cognition | 90/25/43months | 95/37/48 months | Average |
| MP Memory | 97/42/46 months | 96/46/47 months | Average |
| MP Speed Processing | 91/27/44 months | 96/40/47 months | Average |
| NeuroKid Executive Functions | - | 6/37/- | Average |
| NeuroKid Visuoperception | - | 7/50/- | Average |
| NeuroKid Memory | - | 6/37/- | Average |
| BRIEF-2 Cognitive Regulation | - | 77/<1/- | Very low |
| BRIEF-2 Executive Functions | - | 78/<1/- | Very low |
| DP-3 Cognition | 105/63/- | Average | |
| ITPA Auditory Integration | - | 65/1/- | Very low |
| ITPA Visual Association | - | 82/12/- | Low |
| ITPA Visual Memory | 75/5/- | Very low | |
| SENA Executive Functions | - | 80/9/- | Low average |
| Area | 2022—PT/PC/EE | 2024—PT/PC/EE |
Interpretation (Post-Intervention) |
|---|---|---|---|
| MP Cognition | 99/47/44 months | 106/66/52 months | High average |
| MP Memory | 99/47/44 months | 104/61/50 months | Low average |
| MP Speed Processing | 97/42/43 months | 102/55/48 months | Average |
| NeuroKid Executive functions | - | 8/75/- | Average |
| NeuroKid Visuoperception | - | 7/50/- | Average |
| NeuroKid Memory | - | 6/37/- | Average |
| BRIEF-2 Cognitive Regulation | - | 99/50/- | Average |
| BRIEF-2 Executive Functions | - | 99/50/- | Average |
| DP-3 Cognition | 50/1/- | Very low | |
| ITPA Auditory Integration | - | 80/10/- | Low |
| ITPA Visual Association | - | 90/25/- | Average |
| ITPA Visual Memory | 95/37/- | Average | |
| SENA Executive Functions | - | 92/30/- | Average |
| Area | 2022—PT/PC/EE | 2024—PT/PC/EE |
Interpretation (Post-Intervention) |
|---|---|---|---|
| MP Receptive Language | 99//43 months | 107/68/53 months | High average |
| MP Expressive Language (Clinical Eval.) | 105//49 months | 112/79/56 months | High average |
| MP Expressive Language (Parents) | 20//19 months | 50/10/36 months | Low |
| MP Total Language Index | 70//34 months | 88/31/44 months | Very low |
| NeuroKid Articulatory Language | - | 1/<1/- | Very low |
| NeuroKid Visual Language | - | 6/37/- | Average |
| DP-3 Communication | 110/75/- | High average | |
| ITPA Auditory Association | - | 70/2/- | Very low |
| ITPA Verbal Expression | - | 60/<1/- | Very low |
| ITPA Grammatical Organization | - | 68/2/- | Very low |
| Subtest | Scaled Score | Percentile | Performance |
|---|---|---|---|
| Sentence Comprehension | 4 | 2 | Very low |
| Sentence Structure | 3 | 1 | Very low |
| Sentence Formulation | 5 | 5 | Low |
| Related Words | 4 | 2 | Very low |
| Auditory Comprehension | 3 | 1 | Very low |
| Sentence Repetition | 2 | <1 | Very low |
| Repetition of phrases and pseudowords | 3 | 1 | Very low |
| Index of Receptive Language (IRL) | 63 | 1 | Very low |
| Index of Expressive Language (IEL) | 60 | <1 | Very low |
| Index of Language Content (ILC) | 65 | 1 | Very low |
| Index of Total Language (ITL) | 61 | <1 | Very low |
| Area | 2022—PT/PC/EE | 2024—PT/PC/EE |
Interpretation (Post-Intervention) |
|---|---|---|---|
| MP Receptive Language | 89//42 months | 93/32/46 months | Low average |
| MP Expressive Language (Clinical Eval.) | 74//33 months | 82/12/40 months | Low |
| MP Expressive Language (Parents) | 19//20 months | 35/<1/28 months | Very low |
| MP Total Language Index | 42//32 months | 60/<1/38 months | Very low |
| NeuroKid Articulatory Language | - | 4/16/- | Low |
| NeuroKid Visual Language | - | 6/37/- | Average |
| DP-3 Communication | 50/1/- | Very low | |
| ITPA Auditory Association | - | 85/16/- | Low average |
| ITPA Verbal Expression | - | 78/7/- | Low |
| ITPA Grammatical Organization | - | 84/14/- | Low |
| Subtest | Scaled Score | Percentile | Performance |
| Sentence Comprehension | 7 | 16 | Low average |
| Sentence Structure | 6 | 9 | Low |
| Sentence Formulation | 8 | 25 | Average |
| Related Words | 9 | 37 | Average |
| Auditory Comprehension | 6 | 9 | Low |
| Sentence Repetition | 7 | 16 | Low average |
| Repetition of phrases and pseudowords | 5 | 5 | Low |
| Index of Receptive Language (IRL) | 73 | 4 | Very low |
| Index of Expressive Language (IEL) | 78 | 7 | Low |
| Index of Language Content (ILC) | 82 | 12 | Low |
| Index of Total Language (ITL) | 76 | 5 | Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cano-Villagrasa, A.; Ben-Mansour, F.; López-Zamora, M.; López-Chicheri, I. Therapeutic Approach in Language and Cognitive Skills in Premature Twins with ASD: Case Report. Behav. Sci. 2025, 15, 1587. https://doi.org/10.3390/bs15111587
Cano-Villagrasa A, Ben-Mansour F, López-Zamora M, López-Chicheri I. Therapeutic Approach in Language and Cognitive Skills in Premature Twins with ASD: Case Report. Behavioral Sciences. 2025; 15(11):1587. https://doi.org/10.3390/bs15111587
Chicago/Turabian StyleCano-Villagrasa, Alejandro, Fatma Ben-Mansour, Miguel López-Zamora, and Isabel López-Chicheri. 2025. "Therapeutic Approach in Language and Cognitive Skills in Premature Twins with ASD: Case Report" Behavioral Sciences 15, no. 11: 1587. https://doi.org/10.3390/bs15111587
APA StyleCano-Villagrasa, A., Ben-Mansour, F., López-Zamora, M., & López-Chicheri, I. (2025). Therapeutic Approach in Language and Cognitive Skills in Premature Twins with ASD: Case Report. Behavioral Sciences, 15(11), 1587. https://doi.org/10.3390/bs15111587






