Physical Activity Behaviour and Motivation During and Following Pulmonary and Cardiac Rehabilitation: A Repeated Measures Study
Abstract
1. Background
2. The Present Study
3. Methods
3.1. Study Design and Procedure
3.2. Participants, Setting, and Recruitment
3.3. Measures
3.3.1. Lifestyle Physical Activity
3.3.2. Rehabilitation Exercise
3.3.3. Self-Determined Motivation
3.3.4. Intention Strength
3.3.5. Habit Strength
3.4. Data Management and Analyses
4. Results
4.1. Sample Characteristics
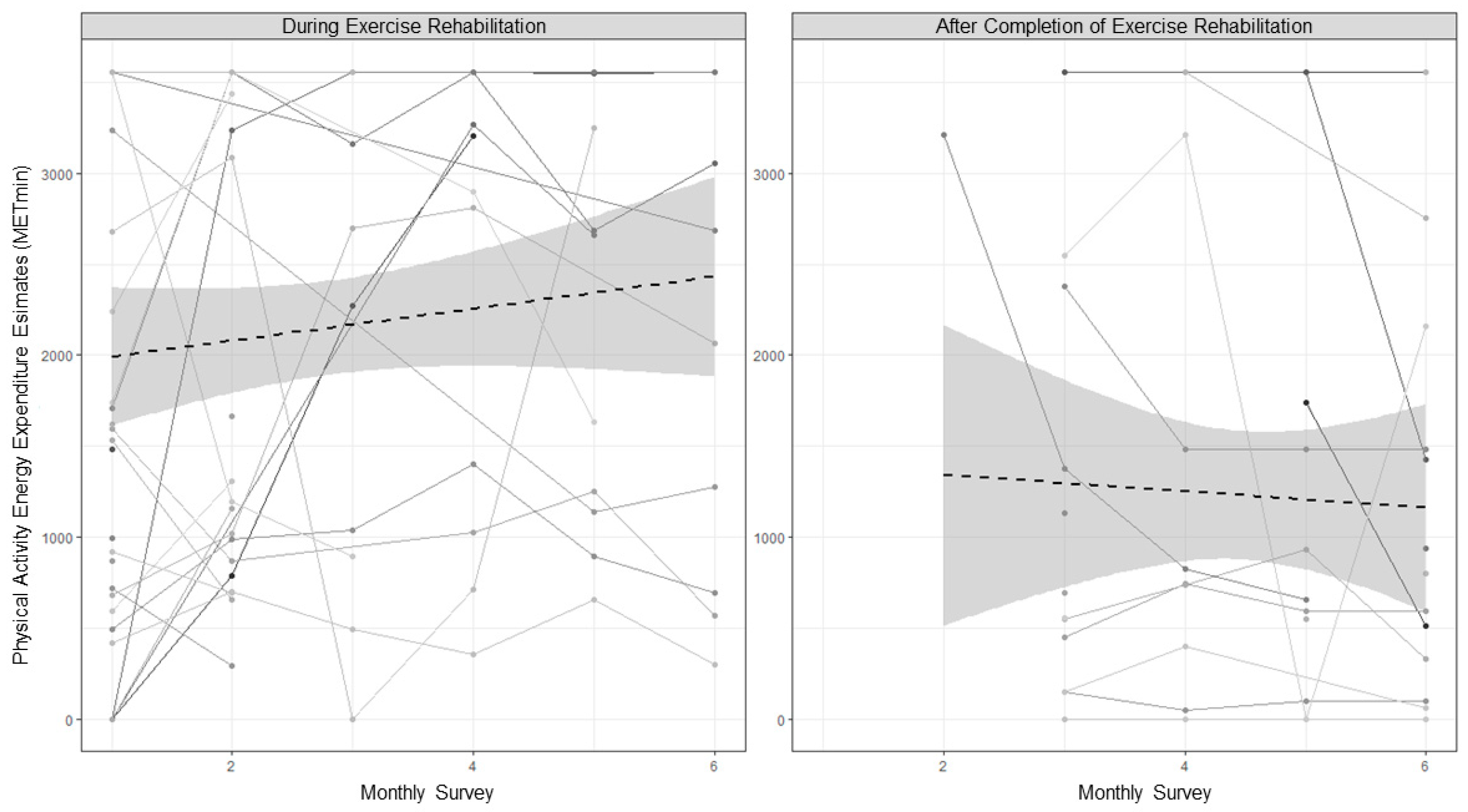
4.2. Change in Physical Activity Behaviour
4.3. Physical Activity Behaviour and Motivation
4.4. Self-Determined Motivation
4.5. Intention
4.6. Habit Strength
5. Discussion
5.1. Conclusions
5.2. Study Limitations and Biases
5.3. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The Top 10 Causes of Death; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Nowbar, A.N.; Gitto, M.; Howard, J.P.; Francis, D.P.; Al-Lamee, R. Mortality from Ischemic Heart Disease. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005375. [Google Scholar] [CrossRef]
- Li, X.; Cao, X.; Guo, M.; Xie, M.; Liu, X. Trends and Risk Factors of Mortality and Disability Adjusted Life Years for Chronic Respiratory Diseases from 1990 to 2017: Systematic Analysis for the Global Burden of Disease Study 2017. BMJ 2020, 368, m234. [Google Scholar] [CrossRef]
- Bahall, M.; Legall, G.; Khan, K. Quality of Life among Patients with Cardiac Disease: The Impact of Comorbid Depression. Health Qual. Life Outcomes 2020, 18, 189. [Google Scholar] [CrossRef]
- Blakemore, A.; Dickens, C.; Guthrie, E.; Bower, P.; Kontopantelis, E.; Afzal, C.; Coventry, P.A. Depression and Anxiety Predict Health-Related Quality of Life in Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 501–512. [Google Scholar] [CrossRef]
- Bize, R.; Johnson, J.A.; Plotnikoff, R.C. Physical Activity Level and Health-Related Quality of Life in the General Adult Population: A Systematic Review. Prev. Med. 2007, 45, 401–415. [Google Scholar] [CrossRef]
- Winzer, E.B.; Woitek, F.; Linke, A. Physical Activity in the Prevention and Treatment of Coronary Artery Disease. J. Am. Heart Assoc. 2018, 7, e007725. [Google Scholar] [CrossRef]
- Salcedo, P.A.; Lindheimer, J.B.; Klein-Adams, J.C.; Sotolongo, A.M.; Falvo, M.J. Effects of Exercise Training on Pulmonary Function in Adults with Chronic Lung Disease: A Meta-Analysis of Randomized Controlled Trials. Arch. Phys. Med. Rehabil. 2018, 99, 2561–2569.e7. [Google Scholar] [CrossRef]
- Jeong, S.-W.; Kim, S.-H.; Kang, S.-H.; Kim, H.-J.; Yoon, C.-H.; Youn, T.-J.; Chae, I.-H. Mortality Reduction with Physical Activity in Patients with and without Cardiovascular Disease. Eur. Heart J. 2019, 40, 3547–3555. [Google Scholar] [CrossRef]
- Geidl, W.; Schlesinger, S.; Mino, E.; Miranda, L.; Pfeifer, K. Dose–Response Relationship between Physical Activity and Mortality in Adults with Noncommunicable Diseases: A Systematic Review and Meta-Analysis of Prospective Observational Studies. Int. J. Behav. Nutr. Phys. Act. 2020, 17, e109. [Google Scholar] [CrossRef]
- Ostman, C.; Jewiss, D.; Smart, N.A. The Effect of Exercise Training Intensity on Quality of Life in Heart Failure Patients: A Systematic Review and Meta-Analysis. CRD 2017, 136, 79–89. [Google Scholar] [CrossRef]
- Driver, C.N.; Novotny, P.J.; Benzo, R.P. Differences in Sedentary Time, Light Physical Activity, and Steps Associated with Better COPD Quality of Life. Chronic Obstr. Pulm. Dis. 2021, 9, 34–44. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V. Effects of Cardiac Rehabilitation, Exercise Training, and Weight Reduction on Exercise Capacity, Coronary Risk Factors, Behavioral Characteristics, and Quality of Life in Obese Coronary Patients. Am. J. Cardiol. 1997, 79, 397–401. [Google Scholar] [CrossRef]
- Pitta, F.; Troosters, T.; Probst, V.S.; Langer, D.; Decramer, M.; Gosselink, R. Are Patients with COPD More Active after Pulmonary Rehabilitation? Chest 2008, 134, 273–280. [Google Scholar] [CrossRef]
- Chatziefstratiou, A.A.; Giakoumidakis, K.; Brokalaki, H. Cardiac Rehabilitation Outcomes: Modifiable Risk Factors. Br. J. Nurs. 2013, 22, 200–207. [Google Scholar] [CrossRef]
- Hamburg, N.M.; Balady, G.J. Exercise Rehabilitation in Peripheral Artery Disease: Functional Impact and Mechanisms of Benefits. Circulation 2011, 123, 87–97. [Google Scholar] [CrossRef]
- McDermott, M.M. Exercise Rehabilitation for Peripheral Artery Disease: A Review. J. Cardiopulm. Rehabil. Prev. 2018, 38, 63–69. [Google Scholar] [CrossRef]
- Rochester, C.L. Exercise Training in Chronic Obstructive Pulmonary Disease. J. Rehabil. Res. Dev. 2003, 40, 59–80. [Google Scholar] [CrossRef]
- Dibben, G.O.; Dalal, H.M.; Taylor, R.S.; Doherty, P.; Tang, L.H.; Hillsdon, M. Cardiac Rehabilitation and Physical Activity: Systematic Review and Meta-Analysis. Heart 2018, 104, 1394–1402. [Google Scholar] [CrossRef]
- Ayabe, M.; Brubaker, P.H.; Dobrosielski, D.; Miller, H.S.; Ishi, K.; Yahiro, T.; Kiyonaga, A.; Shindo, M.; Tanaka, H. The Physical Activity Patterns of Cardiac Rehabilitation Program Participants. J. Cardiopulm. Rehabil. Prev. 2004, 24, 80–86. [Google Scholar] [CrossRef]
- Gray, P.; Murphy, M.; Gallagher, A.; Simpson, E.E.A. A Qualitative Investigation of Physical Activity Compensation among Older Adults. Br. J. Health Psychol. 2018, 23, 208–224. [Google Scholar] [CrossRef]
- Gomersall, S.R.; Rowlands, A.V.; English, C.; Maher, C.; Olds, T.S. The Activitystat Hypothesis. Sports Med. 2013, 43, 135–149. [Google Scholar] [CrossRef]
- Gomersall, S.R.; Maher, C.; English, C.; Rowlands, A.V.; Dollman, J.; Norton, K.; Olds, T. Testing the Activitystat Hypothesis: A Randomised Controlled Trial. BMC Public Health 2016, 16, e900. [Google Scholar] [CrossRef]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F. Theoretical Explanations for Maintenance of Behaviour Change: A Systematic Review of Behaviour Theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Self-Determination Theory: When Mind Mediates Behavior. J. Mind Behav. 1980, 1, 33–43. [Google Scholar]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Biddle, S.; Soos, I.; Chatzisarantis, N. Predicting Physical Activity Intentions Using Goal Perspectives and Self-Determination Theory Approaches. Eur. Psychol. 1999, 4, 83–89. [Google Scholar] [CrossRef]
- Chatzisarantis, N.L.D.; Biddle, S.J.H.; Meek, G.A. A Self-Determination Theory Approach to the Study of Intentions and the Intention–Behaviour Relationship in Children’s Physical Activity. Br. J. Health Psychol. 1997, 2, 343–360. [Google Scholar] [CrossRef]
- Daley, A.J.; Duda, J.L. Self-Determination, Stage of Readiness to Change for Exercise, and Frequency of Physical Activity in Young People. Eur. J. Sport Sci. 2006, 6, 231–243. [Google Scholar] [CrossRef]
- Gardner, B.; Lally, P. Does Intrinsic Motivation Strengthen Physical Activity Habit? Modeling Relationships between Self-Determination, Past Behaviour, and Habit Strength. J. Behav. Med. 2013, 36, 488–497. [Google Scholar] [CrossRef]
- Sweet, S.N.; Tulloch, H.; Fortier, M.S.; Pipe, A.L.; Reid, R.D. Patterns of Motivation and Ongoing Exercise Activity in Cardiac Rehabilitation Settings: A 24-Month Exploration from the TEACH Study. Ann. Behav. Med. 2011, 42, 55–63. [Google Scholar] [CrossRef]
- Russell, K.L.; Bray, S.R. Self-Determined Motivation Predicts Independent, Home-Based Exercise Following Cardiac Rehabilitation. Rehabil. Psychol. 2009, 54, 150–156. [Google Scholar] [CrossRef]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Triandis, H.C. Interpersonal Behavior; Brooks/Cole Publishing Company: Monterey, CA, USA, 1977. [Google Scholar]
- Fishbein, M.; Ajzen, I. Predicting and Changing Behavior: The Reasoned Action Approach; Taylor & Francis: Abingdon, UK, 2011; ISBN 978-1-136-87473-4. [Google Scholar]
- Blanchard, C.M.; Courneya, K.S.; Rodgers, W.M.; Daub, B.; Knapik, G. Determinants of Exercise Intention and Behavior during and after Phase 2 Cardiac Rehabilitation: An Application of the Theory of Planned Behavior. Rehabil. Psychol. 2002, 47, 308–323. [Google Scholar] [CrossRef]
- Blanchard, C.M.; Courneya, K.S.; Rodgers, W.M.; Fraser, S.N.; Murray, T.C.; Daub, B.; Black, B. Is the Theory of Planned Behavior a Useful Framework for Understanding Exercise Adherence during Phase II Cardiac Rehabilitation? J. Cardiopulm. Rehabil. Prev. 2003, 23, 29–39. [Google Scholar] [CrossRef]
- Rothman, A.J.; Sheeran, P.; Wood, W. Reflective and Automatic Processes in the Initiation and Maintenance of Dietary Change. Ann. Behav. Med. 2009, 38, s4–s17. [Google Scholar] [CrossRef]
- Gardner, B. A Review and Analysis of the Use of ‘Habit’ in Understanding, Predicting and Influencing Health-Related Behaviour. Health Psychol. Rev. 2015, 9, 277–295. [Google Scholar] [CrossRef]
- Gardner, B.; Lally, P.; Rebar, A.L. Does Habit Weaken the Relationship between Intention and Behaviour? Revisiting the Habit-Intention Interaction Hypothesis. Soc. Personal. Psychol. Compass 2020, 14, e12553. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Baranova, M.; Christian, H.; Westgarth, C. Increasing Physical Activity by Four Legs Rather than Two: Systematic Review of Dog-Facilitated Physical Activity Interventions. Br. J. Sports Med. 2020, 54, 1202–1207. [Google Scholar] [CrossRef]
- Fleig, L.; Lippke, S.; Pomp, S.; Schwarzer, R. Intervention Effects of Exercise Self-Regulation on Physical Exercise and Eating Fruits and Vegetables: A Longitudinal Study in Orthopedic and Cardiac Rehabilitation. Prev. Med. 2011, 53, 182–187. [Google Scholar] [CrossRef]
- Kaushal, N.; Payer, M.; Bérubé, B.; Juneau, M.; Bherer, L. Facilitating Exercise Habit Formation among Cardiac Rehabilitation Patients: A Randomized Controlled Pilot Trial. Int. J. Environ. Res. Public Health 2021, 18, 6440. [Google Scholar] [CrossRef]
- Deci, E.L.; Koestner, R.; Ryan, R.M. A Meta-Analytic Review of Experiments Examining the Effects of Extrinsic Rewards on Intrinsic Motivation. Psychol. Bull. 1999, 125, 627–668. [Google Scholar] [CrossRef]
- Rebar, A.L.; Rosenbaum, S.; Maher, J.P. Responsiveness to Change of the Psychological Determinants and Outcomes of Physical Activity and Sedentary Behavior. Psychol. Sport Exerc. 2020, 49, e101706. [Google Scholar] [CrossRef]
- Keller, J.; Kwasnicka, D.; Klaiber, P.; Sichert, L.; Lally, P.; Fleig, L. Habit Formation Following Routine-Based versus Time-Based Cue Planning: A Randomized Controlled Trial. Br. J. Health Psychol. 2021, 26, 807–824. [Google Scholar] [CrossRef]
- Judah, G.; Gardner, B.; Aunger, R. Forming a Flossing Habit: An Exploratory Study of the Psychological Determinants of Habit Formation. Br. J. Health Psychol. 2013, 18, 338–353. [Google Scholar] [CrossRef]
- Revelle, W. Psych: Procedures for Personality and Psychological Research 2021; Northwestern University: Evanston, IL, USA, 2017. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjorstrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Markland, D.; Tobin, V. A Modification to the Behavioural Regulation in Exercise Questionnaire to Include an Assessment of Amotivation. J. Sport Exerc. Psychol. 2004, 26, 191–196. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Rebar, A.L. Conceptualizing and Defining the Intention Construct for Future Physical Activity Research. Exerc. Sport Sci. Rev. 2017, 45, 209–216. [Google Scholar] [CrossRef]
- Gardner, B.; Abraham, C.; Lally, P.; de Bruijn, G.-J. Towards Parsimony in Habit Measurement: Testing the Convergent and Predictive Validity of an Automaticity Subscale of the Self-Report Habit Index. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 102–113. [Google Scholar] [CrossRef]
- Verplanken, B.; Orbell, S. Reflections on Past Behavior: A Self-Report Index of Habit Strength. J. Appl. Soc. Psychol. 2003, 33, 1313–1330. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2023. [Google Scholar]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Lenth, R. Emmeans: Estimated Marginal Means, Aka Least-Squares Means. 2022. Available online: https://cran.r-project.org/web/packages/emmeans/emmeans.pdf (accessed on 12 January 2019).
- Bartoń, K. MuMIn: Multi-Model Inference. 2023. Available online: https://cran.r-project.org/web/packages/MuMIn/MuMIn.pdf (accessed on 12 January 2019).
- Arend, M.G.; Schäfer, T. Statistical Power in Two-Level Models: A Tutorial Based on Monte Carlo Simulation. Psychol. Methods 2019, 24, 1–19. [Google Scholar] [CrossRef]
- Snijders, T.A.B. Power and Sample Size in Multilevel Modeling. In Encyclopedia of Statistics in Behavioral Science; Everitt, B.S., Howell, D.C., Eds.; Wiley: Chicester, UK, 2005; Volume 3, pp. 1570–1573. [Google Scholar]
- Grady, P.A.; Gough, L.L. Self-management: A comprehensive approach to management of chronic conditions. Am. J. Pub. Health 2014, 104, e25–e31. [Google Scholar] [CrossRef]
- McEachan, R.R.C.; Taylor, N.; Harrison, R.; Lawton, R.; Gardner, P.; Conner, M. Meta-Analysis of the Reasoned Action Approach (RAA) to Understanding Health Behaviors. Ann. Behav. Med. 2016, 50, 592–612. [Google Scholar] [CrossRef]
- Rebar, A.L.; Dimmock, J.A.; Jackson, B.; Rhodes, R.E.; Kates, A.; Starling, J.; Vandelanotte, C. A Systematic Review of the Effects of Non-Conscious Regulatory Processes in Physical Activity. Health Psychol. Rev. 2016, 10, 395–407. [Google Scholar] [CrossRef]
- Rebar, A.L.; Rhodes, R.E. Progression of Motivation Models in Exercise Science: Where We Have Been and Where We Are Heading. In The Handbook of Sport Psychology; Tenenbaum, G., Eklund, R.C., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2019; Volume 4. [Google Scholar]
- Teixeira, P.J.; Carraça, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, Physical Activity, and Self-Determination Theory: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78–107. [Google Scholar] [CrossRef]
- Teo, J.L.; Zheng, Z.; Bird, S.R. Identifying the Factors Affecting ‘Patient Engagement’ in Exercise Rehabilitation. BMC Sports Sci. Med. Rehabil. 2022, 14, 18–28. [Google Scholar] [CrossRef]
- Schwarzer, R.; Luszczynska, A.; Ziegelmann, J.P.; Scholz, U.; Lippke, S. Social-Cognitive Predictors of Physical Exercise Adherence: Three Longitudinal Studies in Rehabilitation. Health Psychol. 2008, 27, S54–S63. [Google Scholar] [CrossRef]
- Rahman, R.J.; Hudson, J.; Thøgersen-Ntoumani, C.; Doust, J.H. Motivational Processes and Well-Being in Cardiac Rehabilitation: A Self-Determination Theory Perspective. Psychol. Health Med. 2015, 20, 518–529. [Google Scholar] [CrossRef]
- Barbour, K.A.; Miller, N.H. Adherence to Exercise Training in Heart Failure: A Review. Heart Fail. Rev. 2008, 13, 81–89. [Google Scholar] [CrossRef]
- McGregor, G.; Powell, R.; Finnegan, S.; Nichols, S.; Underwood, M. Exercise Rehabilitation Programmes for Pulmonary Hypertension: A Systematic Review of Intervention Components and Reporting Quality. BMJ Open Sport Exerc. Med. 2018, 4, e000400. [Google Scholar] [CrossRef]
- Fleig, L.; Pomp, S.; Parschau, L.; Barz, M.; Lange, D.; Schwarzer, R.; Lippke, S. From Intentions via Planning and Behavior to Physical Exercise Habits. Psychol. Sport Exerc. 2013, 14, 632–639. [Google Scholar] [CrossRef]
- Arnautovska, U.; Fleig, L.; O’Callaghan, F.; Hamilton, K. A Longitudinal Investigation of Older Adults’ Physical Activity: Testing an Integrated Dual-Process Model. Psychol. Health 2017, 32, 166–185. [Google Scholar] [CrossRef]
- Sniehotta, F.F.; Scholz, U.; Schwarzer, R. Action Plans and Coping Plans for Physical Exercise: A Longitudinal Intervention Study in Cardiac Rehabilitation. Br. J. Health Psychol. 2006, 11, 23–37. [Google Scholar] [CrossRef]
- Fleig, L.; Pomp, S.; Schwarzer, R.; Lippke, S. Promoting Exercise Maintenance: How Interventions with Booster Sessions Improve Long-Term Rehabilitation Outcomes. Rehabil. Psychol. 2013, 58, 323–333. [Google Scholar] [CrossRef]
- Carter, P.; Lagan, J.; Fortune, C.; Bhatt, D.L.; Vestbo, J.; Niven, R.; Chaudhuri, N.; Schelbert, E.B.; Potluri, R.; Miller, C.A. Association of Cardiovascular Disease with Respiratory Disease. J. Am. Coll. Cardiol. 2019, 73, 2166–2177. [Google Scholar] [CrossRef]
| n (N = 31) | % | ||
|---|---|---|---|
| Rehabilitation Group | Pulmonary | 16 | 51.6 |
| Cardiac | 15 | 48.4 | |
| Primary Diagnosis | Chronic Obstructive Pulmonary | 9 | 29.0 |
| Disease | |||
| Coronary Artery Bypass Graft | 1 | 3.2 | |
| Diabetes | 1 | 3.2 | |
| Emphysema | 4 | 12.9 | |
| High Cholesterol | 2 | 6.5 | |
| Hypertension | 7 | 22.6 | |
| Obstructive Sleep Apnea | 3 | 9.7 | |
| Data not Available | 4 | 12.9 | |
| Gender | Male | 22 | 71.0 |
| Female | 9 | 29.0 | |
| Age (years) | 36–48 | 1 | 3.0 |
| 49–60 | 1 | 3.0 | |
| 61–72 | 14 | 45.0 | |
| 73–84 | 15 | 48.0 | |
| Marital Status | Married | 20 | 64.5 |
| Partnered | 4 | 12.9 | |
| Single | 7 | 22.6 | |
| Employment Status | Retired | 26 | 83.9 |
| Unemployed | 2 | 6.5 | |
| Other | 3 | 9.7 | |
| Highest Level of Education | High School (≤Year 12) | 20 | 64.5 |
| TAFE/Certificate/Diploma | 2 | 6.5 | |
| University Degree | 5 | 16.1 | |
| Post Graduate Degree | 4 | 12.9 | |
| Ethnicity | White | 30 | 96.8 |
| Other | 1 | 3.2 |
| Variable | Rehabilitation Exercise | For Lifestyle Physical Activity (Outside of Rehabilitation) | Δ | |
|---|---|---|---|---|
| During Rehabilitation | Following Rehabilitation | Significant Differences | ||
| M (SD) | M (SD) | M (SD) | ||
| Self-reported physical activity behaviour | 604.12 (495.54) | 1165.74 (683.43) | 946.79 (710.31) | Rehab Ex < PA Dur Rehab Ex < PA Post PA Dur = PA Post |
| Intrinsic regulation | 3.35 (0.87) | 2.46 (1.25) | 2.34 (1.15) | Rehab Ex < PA Dur Rehab Ex < PA Post PA Dur = PA Post |
| Introjected regulation | 0.80 (1.05) | 1.11 (1.15) | 0.78 (1.11) | Rehab Ex = PA Dur Rehab Ex = PA Post PA Dur = PA Post |
| Identified regulation | 3.22 (0.55) | 2.99 (0.90) | 2.57 (1.04) | Rehab Ex < PA Dur Rehab Ex < PA Post PA Dur = PA Post |
| External regulation | 0.31 (0.70) | 0.69 (1.03) | 0.22 (0.58) | Rehab Ex = PA Dur Rehab Ex = PA Post PA Dur = PA Post |
| Relative autonomy | 14.82 (4.60) | 9.86 (6.82) | 9.85 (6.47) | Rehab Ex < PA Dur Rehab Ex < PA Post PA Dur = PA Post |
| Intention strength | 5.99 (1.74) | 4.57 (1.89) | 4.35 (1.91) | Rehab Ex < PA Dur Rehab Ex < PA Post PA Dur = PA Post |
| Habit strength | 5.73 (1.19) | 3.98 (1.93) | 3.46 (1.85) | Rehab Ex < PA Dur Rehab Ex < PA Post PA Dur = PA Post |
| Outcome | Monthly Change During Exercise Rehabilitation | Monthly Change After Exercise Rehabilitation |
|---|---|---|
| Estimate (95% CI) | Estimate (95% CI) | |
| Physical activity behaviour | 67.83 (−42.11 to 179.42) | −199.74 (−362.12 to −27.37) * |
| Intrinsic regulation | 0.04 (−0.03 to 0.12) | −0.07 (−0.18 to 0.04) |
| Introjected regulation | −0.03 (−0.11 to 0.05) | −0.05 (−0.17 to 0.05) |
| Identified regulation | 0.06 (−0.00 to 0.12) | −0.07 (−0.20 to 0.06) |
| External regulation | −0.05 (−0.13 to 0.03) | −0.03 (−0.06 to −0.00) * |
| Relative autonomy | 0.65 (0.23 to 1.05) * | 0.14 (−0.50 to 0.79) |
| Intention strength | −0.10 (−0.30 to 0.10) | 0.32 (−0.00 to 0.66) |
| Habit strength | 0.03 (−0.10 to 0.16) | 0.17 (−0.03 to 0.38) |
| Predictor | Rehabilitation Exercise | Lifestyle Physical Activity During Rehabilitation | Lifestyle Physical Activity After Completion of Rehabilitation |
|---|---|---|---|
| Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | |
| Intrinsic Regulation | −109.60 (−379.06 to 159.77) | 87.05 (−67.94 to 242.04) | 237.80 * (15.88 to 459.64) |
| Introjected Regulation | 201.90 (−12.61 to 416.42) | 157.43 (−15.44 to 330.21) | 191.00 (−35.53 to 417.59) |
| Identified Regulation | 97.47 (−346.28 to 541.22) | 213.92 * (15.30 to 412.53) | 378.00 * (151.86 to 604.23) |
| External Regulation | 45.33 (−183.90 to 274.56) | 209.60 (−16.53 to 435.83) | −0.62 (−330.96 to 329.71) |
| Relative Autonomy Index | −24.65 (−77.51 to 28.22) | 14.07 (−14.19 to 42.33) | 43.14 * (5.47 to 80.81) |
| Intention Strength | −39.41 (−187.97 to 109.16) | 157.18 * (52.77 to 261.60) | 216.72 * (104.08 to 329.36) |
| Habit Strength | −57.80 (−257.49 to 141.90) | 118.64 * (20.14 to 217.15) | 205.00 * (92.42 to 317.57) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfrey, K.L.; Gardner, B.; Judd, J.; Askew, C.D.; Vandelanotte, C.; Rebar, A.L. Physical Activity Behaviour and Motivation During and Following Pulmonary and Cardiac Rehabilitation: A Repeated Measures Study. Behav. Sci. 2024, 14, 965. https://doi.org/10.3390/bs14100965
Alfrey KL, Gardner B, Judd J, Askew CD, Vandelanotte C, Rebar AL. Physical Activity Behaviour and Motivation During and Following Pulmonary and Cardiac Rehabilitation: A Repeated Measures Study. Behavioral Sciences. 2024; 14(10):965. https://doi.org/10.3390/bs14100965
Chicago/Turabian StyleAlfrey, Kristie Lee, Benjamin Gardner, Jenni Judd, Christopher D. Askew, Corneel Vandelanotte, and Amanda L. Rebar. 2024. "Physical Activity Behaviour and Motivation During and Following Pulmonary and Cardiac Rehabilitation: A Repeated Measures Study" Behavioral Sciences 14, no. 10: 965. https://doi.org/10.3390/bs14100965
APA StyleAlfrey, K. L., Gardner, B., Judd, J., Askew, C. D., Vandelanotte, C., & Rebar, A. L. (2024). Physical Activity Behaviour and Motivation During and Following Pulmonary and Cardiac Rehabilitation: A Repeated Measures Study. Behavioral Sciences, 14(10), 965. https://doi.org/10.3390/bs14100965









