Abstract
With the global population of older adults projected to double to 2.1 billion by 2050, it becomes crucial to promote healthy aging to alleviate the associated disease burden. In this context, technology, particularly virtual reality (VR) and augmented reality (AR), has garnered attention for its potential to augment physical activity in older adults. These immersive technologies offer interactive and enjoyable exercise experiences, making physical activity more appealing. However, the effectiveness of these interventions is not solely attributed to technology itself but is deeply intertwined with psychological processes. This rapid review examines the effectiveness of VR and AR interventions in enhancing physical exercise among healthy older adults while exploring the role of psychological variables, including mood, self-efficacy, and motivation. The results of the study show that technology-enhanced physical activity interventions hold great promise but call attention to the need for a comprehensive understanding of psychological dynamics that will pave the way for more tailored and effective interventions. Future research endeavors should aim to bridge these gaps in knowledge to optimize the impact of technology on healthy aging.
1. Introduction
In recent years, many advances have been made regarding medicine, technology, and socioeconomic development, and the knowledge of the general public about health-related factors has vastly improved. As a result, innovative therapies and treatments have been successfully implemented in healthcare, leading to an increase in life expectancy across the world. In fact, by the end of the decade (2030), the number of people in the world aged 60 years and older will be 34% higher, increasing from 1 billion in 2019 to 1.4 billion. By 2050, the global population of older people is estimated to double up to 2.1 billion [1]. Aging starts in the later part of the life cycle, around 60 years of age [1]. This period is associated with the emergence of several health-related states, commonly called geriatric syndromes, which are often the consequence of multiple underlying factors and include an increased risk for debilitating conditions such as frailty, delirium, dementia, and cancer, although the most frequent issues faced by individuals aged 65 and over are non-pathological age-related changes, including normal declines in cognition, physical limitations, and loss of partners and friends [2]. With it being a particularly frail condition, in which many factors (i.e., socio-economic and environmental) may contribute to the aggravation of physical and mental health, now more than ever aging represents a challenge to health institutions in which the active and healthy aging policy assumed a fundamental role.
According to the World Health Organization (2020; WHO), healthy aging consists of developing and maintaining the functional ability that enables physical and psychological well-being in older individuals. This ability is strongly influenced by the social and economic resources and opportunities available to people across their life course (e.g., social and family support, health insurance, and high income). Maintaining certain healthy behaviors throughout life contributes to many favorable outcomes regarding older adults’ health conditions [2]. In particular, physical activity stands as a cornerstone in supporting healthy aging, with its primary aim being the maintenance or enhancement of individuals’ functional abilities. This is especially crucial in addressing sedentary lifestyles while concurrently fostering an increased sense of accomplishment, self-assurance, and other social benefits. Physical activity programs yield numerous advantages, such as decelerating degenerative processes, enhancing physical capabilities, and positively influencing functional autonomy and overall quality of life [3,4]. Engaging in physical activity regularly has been linked to numerous health benefits, including reduced risk of obesity, cardiovascular diseases, cancer, and overall mortality [2]. Moreover, PA can enhance functional and cognitive capacities, improve psychological well-being, and increase the likelihood of successful aging [5].
Although the benefits of physical activity in healthy aging are widely recognized, the latest global estimates of the WHO showed that 1.4 billion adults (27.5% of the world’s adult population) fall short of reaching the prescribed standard of physical activity, which tends to decrease among both women and men as they get older [6]. Given these premises, it is important to understand the individual variables that could promote physical activity and healthy lifestyles in the older adult population.
While face-to-face interventions have been evaluated and reported in the scientific literature [7], the opportunities coming from the innovation of new technologies attracted some researchers to evaluate the use of technology to prompt physical activity in older adults [8,9]. Research on the utilization of internet-based resources and new technologies among older adults has shown more favorable attitudes when compared with a decade ago [10]. Additionally, there has been an increase in technological proficiency and openness to innovation within this demographic [11]. These findings support the feasibility of introducing technology-based interventions aimed at fostering physical activity or exercise in older adults in order to prevent health issues [12].
Among the newest digital tools, virtual reality (VR) has gained interest within different health contexts [13,14]. VR creates immersive virtual environments in which the body, environment, and brain are closely related. The simulated environment can be easily manipulated, facilitating experimental tasks that are difficult to implement in real-world settings. Other benefits of VR regard the possibility to participate in potentially dangerous tasks, such as moving in a complex environment or driving a car, in a controlled ecological setting [11], thus allowing one to perform a task safely [12,13,14,15,16]. The virtual environments produced by VR devices can be portrayed as a blend of tangible and computer-generated components, forming a spectrum known as the reality–virtuality continuum. Within this mixed reality setting, elements from both the physical world and the virtual realm are employed, giving rise to concepts like augmented reality and augmented virtuality. In the scientific literature, three distinct categories of VR systems are documented, each providing varying levels of immersion: (1) non-immersive VR systems involve the creation of a 2D virtual environment displayed on a computer screen, as seen in serious video games; (2) immersive VR systems deliver a comprehensive simulated experience through the utilization of various devices, including head-mounted displays, audio equipment, and haptic devices; and (3) semi-immersive systems deliver a mixed reality experience using a stereo image of a 3D simulated environment, which is displayed on a large monitor and adjusted based on the observer’s head position.
Augmented reality is a technological paradigm that overlays digital information or virtual elements onto the real-world environment, enhancing the user’s perception and interaction with their surroundings. Unlike the immersive, fully simulated environments of VR, AR integrates digital elements into the user’s existing reality, creating a blended experience. In the context of healthcare and physical activity promotion, AR operates on the theoretical foundation of enhancing real-world experiences through digitally augmented elements. The theoretical underpinning lies in the potential of AR to seamlessly integrate with daily life, providing users with contextual and personalized information that can influence behavior and decision-making.
These technologies offer opportunities for interactive and enjoyable exercise experiences, making physical activity more appealing and engaging for older adults [15]. VR and AR have shown potential in improving recovery from illness, physical function, balance, and mobility among older adults [16]. In addition, the enjoyable yet challenging nature of VR activities may play a significant role in providing valuable feedback to older adults, as well as enhancing motor learning and adherence to exercise programs [17]. These strategies have shown promising outcomes and contribute to the overall well-being of older individuals; however, it is not clear how the psychological variables could contribute to fostering digital interventions and if this issue has been properly addressed by the literature.
The present study aims to provide a rapid review of the literature regarding the effectiveness of interventions employing VR (either immersive or non-immersive) or AR technology to improve physical exercise in healthy older adults (>60 years), investigating psychological predictors (e.g., mood) or outcomes (e.g., well-being) of engagement in the physical activity. To comprehensively address the research objectives within a limited time frame, a rapid review approach was chosen for this study. Rapid reviews are particularly suitable when timely insights are needed, as in the case of emerging technologies and interventions. The rapid review method was chosen to efficiently gather and present relevant insights into the effectiveness of VR and AR interventions in promoting physical exercise among healthy older adults, recognizing the need for timely information in the rapidly evolving landscape of technology-based healthcare interventions. The choice of a rapid review methodology comes with inherent advantages and limitations. On the positive side, rapid reviews allow for a quicker synthesis of existing evidence, making them well suited for informing timely decision-making and policy development. The streamlined process involves more focused search strategies and inclusion criteria, facilitating a faster turnaround [18]. On the other hand, the expedited nature of the process may result in a trade-off between speed and comprehensiveness. While we aim to capture the essential findings within the available time frame, the condensed approach may not cover the breadth of literature that a traditional systematic review would [18]. The decision to opt for a rapid review, as opposed to a standard systematic review, was driven by the urgency of understanding the current state of the literature on the effectiveness of VR and AR interventions in promoting physical exercise among healthy older adults, given the rapidity of the advancement of technology.
2. Materials and Methods
The rapid review process was designed to be completed within a condensed time frame, balancing the need for timely results with methodological rigor. While a standard systematic review often takes several months to years, the rapid review was conducted within a more expedited schedule; specifically, it took three full months, recognizing the rapid advancement of the technology devices. This study was conducted according to PRISMA guidelines, which report the preferred reporting items for rapid reviews [19]. To identify the papers for this rapid review the authors searched the relevant literature in the Scopus and Medline databases from 2000 to 2023, considering the technological advancements in VR and AR. This limited time frame was chosen to ensure relevance to the rapidly evolving field. Search terms were as follows: “older” AND “adults” OR “elderly” AND “physical” AND “activity” OR “physical” AND “exercise” OR “exercise” OR “fitness” AND “virtual” AND “reality” OR “augmented” AND “reality”. This strategic choice aimed to streamline the search process while capturing the essence of the study’s focus. In line with Cochrane rapid review methods recommendations [18], before performing the screening of the studies, the authors used standardized titles and abstract forms with the same pool of studies for the entire research group to calibrate and test the review form. The first and the second authors independently screened 80% of titles and abstracts, with conflict resolution. Then, the first author screened the remaining abstracts, and the second author screened all excluded abstracts and if needed resolved conflicts. Relating to the full-text inclusion, a standardized full-text form was used in order to test and calibrate the review form. Then, the first author screened all included full-text articles, and the second author screened all excluded full-text articles. The present screening procedure was performed using the Rayyan.ai tool [20]. All tables and figures were uploaded to OSF at the following link: https://osf.io/fqas4/.
Table 1 shows the summary of the inclusion and exclusion criteria of the study characteristics based on the PICOS framework (i.e., populations/participants, interventions and comparators, outcome(s) of interest, and study designs/type) [18,21]. Peer-reviewed articles written in the English language were included. Key stakeholders were involved and consulted during the review process in order to set and refine the review question, eligibility criteria, and the outcomes of interest.

Table 1.
Summary of inclusion and exclusion criteria according to the PICOS framework.
2.1. Data Extraction
The first and second authors checked for the correctness and completeness of the extracted data. For each selected study, socio-demographic (e.g., sample mean age), methodological (e.g., VR/AR software employed, hardware, a primary and secondary outcome, PA procedure for experimental group [EG] and control group [CG], and assessment of PA and psychological variables), and statistical variables (e.g., data analysis and significant results) were extracted.
Risk of Bias Assessment
The risk of biases was assessed through a checklist derived from integrating the quality assessment tool for quantitative studies and the Cochrane Collaboration’s tool for assessing the risk of bias [22,23].
The tool used in the present rapid review assessed the following potential areas of bias: (1) randomization process, (2) deviations from the intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported results.
The second author rated the risk of bias in the included studies, with the first author fully verifying all judgments (and support statements). Interrater agreement was excellent (r = 0.9). The final score identified whether a study was either at low, moderate, or high risk of bias.
3. Results
3.1. Database Searching
Database searching yielded a total of 346 abstracts. Of these, n = 2 duplicates were excluded. Then, n = 342 records were independently screened for the abstract, and n = 271 were excluded because of the defined exclusion criteria: wrong study population (40%), wrong study design (21%), wrong outcome (36%), or wrong publication type (3%). Therefore, the n = 71 remaining records were screened for the full text, and n = 36 were excluded for the following reasons: did not meet the inclusion criteria for age population, wrong study design, wrong outcome, did not employ VR/AR technology, or foreign language. Finally, n = 35 records were included in the review (see Figure 1 for the flow diagram).
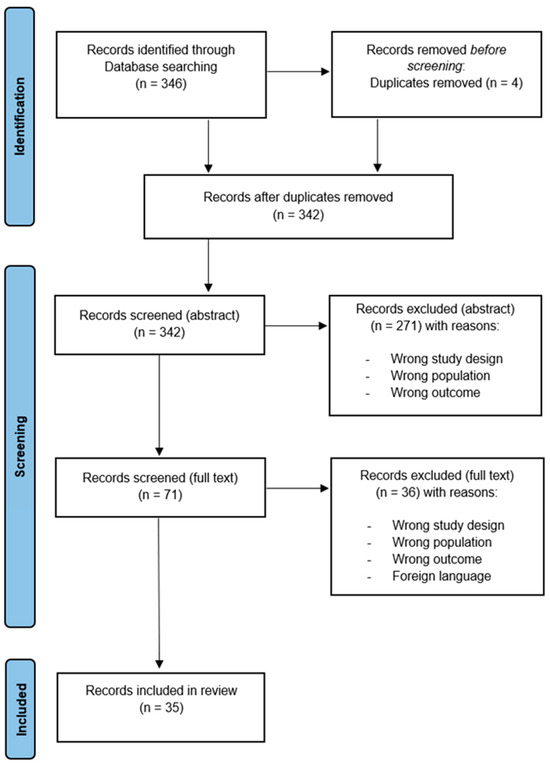
Figure 1.
Flow diagram of the selection process.
Table 2 provides a synoptic summary of the search results.

Table 2.
Table summarizing characteristics of the included studies.
3.2. Risk of Bias Assessment
Most of the studies did not follow strictly methodological criteria, showing a moderate overall risk of bias. Considering the Cochrane Collaboration’s tool for assessing the risk of bias [22,23], only the study of Park and Yim [31] was evaluated as having an overall “low risk” of bias fulfilling all the defined criteria. Considering all the criteria screened following the procedure (i.e., 1: randomization process; 2: deviations from the intended interventions; 3: missing outcome data; 4: measurement of the outcome; 5: selection of the reported results), the studies were evaluated as follows:
- (a)
- 27 studies (77%) were evaluated as having moderate risk of bias; 7 studies (20%) were evaluated at high risk.
- (b)
- Considering each of the domains evaluated:
- a.
- Randomization process: Seven studies (20%) were evaluated as “low concerns”, 22 studies (62.7%) were evaluated as “some concerns”, and 6 (17.3%) were evaluated as being at “high risk” of bias.
- b.
- Deviation from intended intervention: Ten studies (8.5%) were evaluated as “low concerns”; twenty-four studies (68.4%) were evaluated as “moderate risk”, and one study (2.85%) was evaluated as being at “high risk”.
- c.
- Missing outcome data: Four studies (11.4%) were evaluated as “some concerns”, while all the others were evaluated as being at “low risk”.
- d.
- Measurement of the outcome: Four studies (11.4%) were evaluated as “some concerns”, while all the others were evaluated as being at “low risk”.
- e.
- Selection of the reported result: Twenty-nine studies (82.65%) were evaluated as “some concerns”; six (17.1%) were evaluated as “low risk”.
The results show as more frequent a low risk of bias in terms of “measurement of the outcome” and “missing outcome data”, while most biases rely on the randomization process poorly implemented by the studies. See Figure 2 and Figure 3 for the complete evaluation.
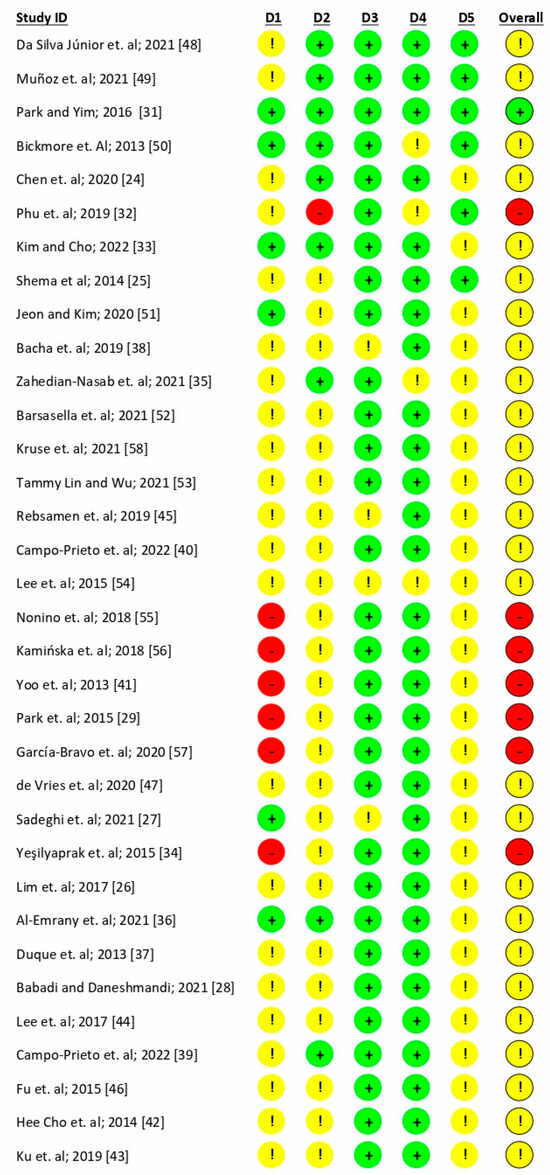
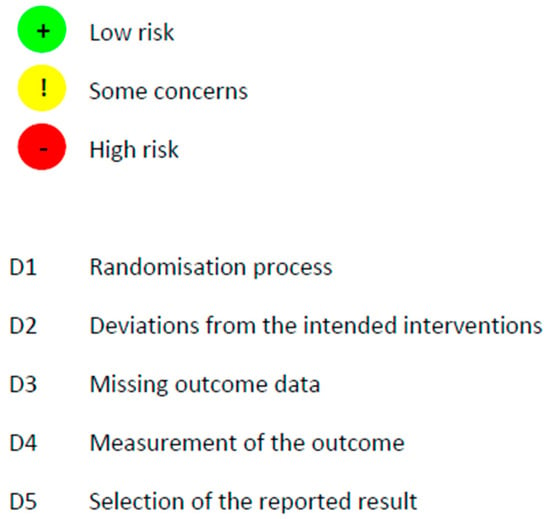
Figure 2.
Risk of bias assessment [24,25,26,27,28,29,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58].
Figure 3.
Risk of bias assessment and distribution of the studies.
3.3. Participants
The included studies evaluated a total of 1712 participants, of which 950 (55.5%) belonged to experimental groups (PA with VR/AR) and 753 (44%) belonged to the control group (traditional PA or no intervention). A total of 1063 participants were female (62%) and 633 (37%) were male. The mean age of participants was 75.12 years.
3.4. Study Design
Of the included articles, 68% (n = 24) consisted of randomized controlled trials (RCTs) [24,26,27,28,30,31,32,33,34,35,36,37,38,40,41,42,43,46,50,51,52,54,55]. Other studies included (N = 4) cross-over designs (alone versus with peers [48], immersive versus non-immersive [58], young avatar versus old avatar [53], and young versus old [47]), 9% were observational studies [49,56,57], two were feasibility trials [40,45], and one was based on retrospective data [25].
3.5. Immersive, Virtual, or Augmented Reality
Among the included studies, seven (20%) employed immersive VR [31,39,40,52,53,57,58]. Twenty-four studies (68.5%) employed non-immersive VR [25,26,27,28,31,32,33,34,35,36,37,38,42,47,48,49,50,53,54,55,56,58], while four (11.5%) employed AR technology [24,41,43,51].
Of the thirty-five studies selected, 46% (N = 16) assessed physical and psychological variables [27,32,34,35,36,37,40,41,48,50,51,52,53,54,55,56], while the others did not consider psychological variables.
3.6. Psychological Variables Included in the Study
Mood-related symptoms have been evaluated by four studies [37,50,53,56], a measure of the quality of life has been evaluated by four studies [36,40,54,57], two studies included a measure of satisfaction with life [52,55], two studies evaluated motivation [48,58], self-efficacy in avoid falling was evaluated by five studies [32,33,34,35,41], while two evaluated self-efficacy related to physical activity [41,53]; see Table 1 for the complete list of constructs evaluated by each study.
3.7. Psychological Tools Implemented
In the selected studies, mood was measured by the Psychological Health Questionnaire [59], the Geriatric Depression Scale (GDS) [60], the Beck Depression Inventory (BDI) [61], the Affect Grid [62], and the Positive Affect Negative Affect Schedule (PANAS) [63]. Quality of life, was assessed with the Short Form Health Survey 12 [64], the Short Form Health Survey (SF-36) [65], and EQ-5D-3L [66]. Motivation was assessed through the Intrinsic Motivation Inventory (IMI) [67], the Physical Exercise Adherence Questionnaire [68], and the Player Experience of Needs Satisfaction (PENS) [69]. Self-efficacy was measured trough the Falling Efficacy Scale-International (FES-I) [70], exercise self-efficacy (ESE) [71], and Tinetti falls efficacy scale [72]. For the complete list of questionnaires used in the different studies, see Table 2.
3.8. Neuropsychological Assessment
Cognitive status was assessed by 17% (N = 6) of the records [31,38,45,50,55,58]. Questionnaires mainly adopted were the Montreal Cognitive Assessment (MoCA) [73], Mini Mental State Examination (MMSE), Mini-Cog [74], and the MEC Spatial Presence Questionnaire (MEC-SPQ) [75].
3.9. Subjective Variables Related to the Device
The acceptability and usability of the employed VR and/or AR technology were measured by six of the selected articles [39,40,45,48,49,58], mainly using the System Usability Scale (SUS) [76], the Simulator Sickness Questionnaire (SSQ) [77], and the Game Experience Questionnaire [78]
Narrative results related to the outcomes of the records are presented below separately for psychological outcomes, cognitive functions, and physical and functional abilities.
3.10. Psychological Outcomes
3.10.1. Self-Efficacy
In five out of the seven studies assessing self-efficacy, a notable improvement was observed in the intervention group(s) in comparison with the control group. Among these, four studies utilized an active non-virtual reality (non-VR) control group [26,32,35,36], and one study had a control group with no exercise ([51]. Conversely, one study did not identify significant differences between the intervention and control groups [34]. Another study had a distinct focus on investigating the effectiveness of a specific virtual reality (VR) environment, comparing outcomes between a young and old avatar [53]. All the studies implemented interventions using VR.
3.10.2. Mood
Two of the five studies evaluating mood did not search the evidence for improvement in mood [37,50] but assessed depression as exclusion criteria; considering the remaining two studies, one of them found an improvement in mood after the VR intervention [56]. All the studies implemented interventions using VR.
3.10.3. Quality of Life
Furthermore, six studies included measures of quality of life; two of them found significant differences between the VR intervention group and the control group [36,52]. Studies conducted by Campo-Prieto and colleagues and Garcia-Bravo and colleagues found an increased QoL in both the intervention group and the control group [40,57], while Lee found mixed results [30], and Nonino evaluated only satisfaction with life with a non-validated questionnaire [55]. All the studies implemented interventions using VR.
3.11. Neuropsychological Outcomes
Neuropsychological assessments were performed by four studies [31,38,50,58] of the included records. However, one evaluated global cognitive evaluation as part of the exclusion criteria [50], and the remaining found significant positive differences in favor of the intervention group compared with the control group [31].
3.12. Physical Activity, Balance, and Gait
Out of the 35 studies included in the review, all found significant improvement in indexes of physical activity, functionality, or balance after the intervention with immersive, non-immersive, or augmented reality but not two that were feasibility studies [49,58].
Thirteen studies included exclusively PA or balance-related outcomes, with no attention given to psychological variables [24,25,26,27,28,30,31,39,42,43,44,45,47]. Among these studies, five found significant differences regarding different measures of PA practiced with and without immersive VR by older adults. Among studies that employed non-immersive VR (e.g., motion sensors, Kinect, and the Wii Balance Board), three found significative results between groups for shoulder (flexion, abduction, and rotation joint movements) and knee (retraction, extension, and protraction) exertion using Kinect [49]; strength of bilateral knee, isokinetic peak torque, flexibility, endurance, and total work using Wii Fit Plus [26]; and muscle strength and reaction times using the Wii Balance Board [46].
3.13. Feasibility Studies
Three studies evaluated the feasibility of virtual reality interventions to enhance physical activity. The first study by Munoz and colleagues evaluated mainly the usability of the devices, in an observational study design [49] with a VR non-immersive system (RGBD Microsoft Kinect version 2), and assessed its effectiveness in correctly performing various exercises while also assessing their physical achievements. The degree of acceptance of the procedure was measured through a survey based on the System Usability Scale (SUS), whereas the physical performance was monitored by the system. The results showed positive outcomes in terms of usability.
The second study was a cross-over study design (immersive vs. non-immersive) by Kruse and colleagues [58] aimed to compare a traditional, recorded 2D exercise video with a VR exergame. The comparison regards enjoyment, attention allocation, perceived workload, and preference. The outcome measurements included physical functioning with different tests, the Simulator Sickness Questionnaire (SSQ) for motion sickness, the Intrinsic Motivation Inventory (IMI), and the MEC Spatial Presence Questionnaire (MEC-SPQ). The results showed slight or no differences between the two modalities (immersive vs. non-immersive).
The third study, an RCT proposed by Campo-Prieto [40], aimed to analyze the effects of an immersive VR exergaming program on physical function, quality of life, and parameters related to VR exposure. The outcome measurements included for assessing balance and gait were lower limb function, hand grip strength, the time up and go (TUG) test, and the five times sit-to-stand test (FTSTS). The results showed improvement of physical functioning and balance but no significant differences in the quality of life between groups.
4. Discussion
Promoting physical activity in older adults is crucial for maintaining good health and overall well-being. The scientific literature is advancing the concept of digital intervention using more often recent technologies such as Virtual Reality or Augmented Reality. As stated, there are recent reviews of the literature that provide evidence for the efficacy of the use of VR in older adults in enhancing physical activity [79].
Results on physical activity have been confirmed by the present study. Our rapid review delves into the efficacy of virtual reality (VR) and augmented reality (AR) interventions for promoting physical activity among healthy older adults, by focusing on the role of psychological factors as either mediators or moderators of intervention efficacy. Our results identified key insights, challenges, and gaps in the existing literature. Overall, most of the identified studies presented some difficulties: (i) they considered people aged 50–55 as older adults, while common research criteria establish older age as a process that begins from age 60 to 65 [80,81]; (ii) they considered PA as an outcome or a status, i.e., the difficulty encountered by an individual in executing a task or action due to old age limitations; (iii) they did not take psychological variables (e.g., mood or self-efficacy) into account for enhancing PA in older adults but rather as an outcome; and (iv) most of the studies lacked strict methodology, and the risk of a biased conclusion was high.
Our rapid review adds a timely perspective to the evolving landscape of research on technology-driven interventions for older adults. Specifically, it contributes by emphasizing the importance of considering psychological variables in the adoption and sustainability of physical activity habits through VR and AR interventions. This nuanced focus distinguishes our review from previous works and sheds light on the intricacies of technology’s impact on older adults’ physical activity.
Given this premise, in the realm of enhancing physical activity in older adults, technology stands as a promising ally. However, it is essential to recognize that its efficacy transcends the mere presence of gadgets or applications. Instead, the profound influence technology exerts on physical activity in this population is intricately tied to the underlying psychological processes it activates. However, despite the evidence of the relevance of psychological variables involved in the adoption of physical activity habits [82,83,84], it is noteworthy that the existing literature often falls short in investigating these multifaceted psychological processes. Our results showed that fewer than half of the included studies in the rapid review considered these variables; furthermore, when these variables were considered, they were often treated as secondary outcomes, focusing solely on the effects of physical activity on mental health rather than examining how they can directly influence, moderate, or mediate adherence to physical activity [85]. In other cases, these variables were only evaluated as exclusion criteria and were not considered primary outcome measures [43].
Factors such as self-efficacy, motivation, and mood emerged as central determinants in this context. As older adults engage with technology, they often experience a notable surge in self-efficacy, fostering a newfound confidence in their ability to adopt and sustain an active lifestyle. This increase in self-assurance is attributed to the opportunity to visualize their progress thanks to the technology and also to gain confidence in a safe environment [86].
Moreover, technology empowers older adults with enhanced motivation. The gamification elements incorporated into many fitness applications transform physical activity into an engaging challenge. Goal-setting features provide a clear sense of purpose, while real-time feedback and rewards offer immediate gratification, reinforcing the motivation to stay active. Additionally, the social connectivity facilitated by technology contributes significantly to mood enhancement.
A comprehensive understanding of how self-efficacy, motivation, and mood mediate the relationship between technological interventions and the intention to engage in physical activity among older adults remains an underexplored frontier. Thus, future research endeavors hold the potential to unearth the intricate dynamics at play, shedding light on the nuanced ways in which technology drives and sustains physical activity in this population.
Another of the main challenges identified throughout this literature review is the lack of standardized and defined assessment measures for psychological variables in the context of physical activity validated for the older adult population. Currently, there are no tools considered “gold standards” for the assessment of these variables in older adults, making it difficult to compare and generalize study results. This lack of consolidated assessment measures represents a significant limitation in scientific research on the subject.
Furthermore, most studies included these side effects and other health conditions in their exclusion criteria. A low incidence of adverse effects, with no impact on adherence and no significant difference between groups, was found. Our analysis suggests that AR and VR protocols, regardless of their efficacy in enhancing physical activity, balance, or other psychological variables, were generally well tolerated by older adults.
5. Strengths and Limitations of the Study
The rapid review methodology used in this study had advantages and trade-offs, resulting in a nuanced evaluation of the research process. One of the significant gains of opting for a rapid review was the timely acquisition of relevant insights. In a field where technology evolves rapidly, synthesizing the literature quickly helped us capture the most recent advancements and evidence on the effectiveness of virtual reality (VR) and augmented reality (AR) interventions in promoting physical activity for older adults. In addition, the rapid review allowed for a focused investigation, honing in on the literature dealing specifically with VR-based interventions for enhancing physical activity among healthy older individuals. This specificity facilitated a targeted exploration of the role of psychological factors as mediators or moderators of intervention efficacy. The discussion effectively highlighted critical challenges and gaps in the existing literature, including the limited consideration of psychological variables, methodological shortcomings in the identified studies also evidenced in some of the bias assessed, impacting mostly the sampling procedure (i.e., randomization process), and the absence of standardized assessment measures. This awareness sets the stage for future research endeavors to address these limitations. While the rapid review provides a timely overview, the condensed nature of the methodology may have limited the depth of analysis into certain aspects. Complex relationships between technological interventions and psychological variables may benefit from a more comprehensive exploration than a standard systematic review might afford. The discussion reveals that fewer than half of the included studies in the rapid review considered psychological variables. Furthermore, when these variables were considered, they were often treated as secondary outcomes, potentially overlooking their direct impact on adherence to physical activity. This limitation points to a missed opportunity for a more nuanced understanding. In summary, the rapid review approach facilitated a quick and targeted exploration of the literature, providing timely insights into the efficacy of VR-based interventions for promoting physical activity in older adults. However, the condensed methodology raised considerations about the depth of analysis and the adequacy of exploring psychological variables, in addition to categorization. These trade-offs underscore the need for a balanced approach that aligns with the specific goals and constraints of the research.
6. Conclusions
The present study used a rapid review approach to provide a roadmap for future research endeavors, by evaluating the role of psychological variables in the improvement of physical activity in older adults using VR or AR. Overall, our findings highlight the need for a more comprehensive exploration of psychological processes, urging researchers to delve deeper into the dynamics of self-efficacy, motivation, and mood as central determinants and not only as an outcome. Additionally, our identification of challenges, such as the lack of standardized assessment measures, offers a practical foundation for refining research methodologies (see BREQ3). Considering the actual scientific literature, our rapid review claims for further investigating the role of psychological and cognitive variables, as well as the validation of outcome measures for psychological aspects, as crucial for advancing our understanding of promoting physical activity in older adults and enhancing their overall well-being through new technologies (i.e., VR or AR). In the realm of practice, our findings underscore the potential of technology to enhance physical activity, emphasizing the need for interventions that leverage psychological factors to maximize effectiveness. Finally, our research holds potential benefits for the target population of healthy older adults. By acknowledging the influence of technology on psychological variables, particularly self-efficacy, motivation, and mood, our findings suggest that technology-driven interventions can empower older adults with increased confidence, enhanced motivation, and improved mood. These factors, in turn, may contribute to the adoption and maintenance of an active lifestyle, promoting overall well-being in the aging population.
Author Contributions
All the authors contributed to the study’s conception and design. All the authors participated in the material preparation and data collection. Methodology, formal analyses, and investigation: A.C., M.A., T.P., F.A. and F.L.; writing—original draft preparation: A.C., T.P. and M.A.; writing—review and editing: R.B., F.A., T.P. and F.L. All the authors reviewed the manuscript. Supervision: F.L., R.B. and F.A. All authors have read and agreed to the published version of the manuscript.
Funding
We acknowledge co-funding from Next Generation EU, in the context of the National Recovery and Resilience Plan, Investment PE8—Project Age-It: “Ageing Well in an Ageing Society”. This resource was co-financed by the Next Generation EU [DM 1557 11 October 2022]. The views and opinions expressed are only those of the authors and do not necessarily reflect those of the European Union or the European Commission. Neither the European Union nor the European Commission can be held responsible for them.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization United Nation’s Decade of Healthy Ageing (2021–2030); Wolrd Health Organization: Geneva, Switzerland, 2020.
- Lee, I.M.; Skerrett, P.J. Physical Activity and All-Cause Mortality: What Is the Dose-Response Relation? Med. Sci. Sports Exerc. 2001, 33, S459–S471. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ballesteros, R.; Caprara, M.G.; Iñiguez, J.; García, L.F. Promoción Del Envejecimiento Activo: Efectos Del Programa Vivir Con Vitalidad®. Rev. Esp. Geriatr. Gerontol. 2005, 40, 92–103. [Google Scholar] [CrossRef]
- Bherer, L.; Erickson, K.I.; Liu-Ambrose, T. A Review of the Effects of Physical Activity and Exercise on Cognitive and Brain Functions in Older Adults. J. Aging Res. 2013, 2013, 657508. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, S.; Chun, S.; Han, A.; Heo, J. The Effects of Leisure-Time Physical Activity for Optimism, Life Satisfaction, Psychological Well-Being, and Positive Affect among Older Adults with Loneliness. Ann. Leis. Res. 2017, 20, 406–415. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Status Report on Physical Activity 2022: Country Profiles; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Chase, J.A.D. Interventions to Increase Physical Activity Among Older Adults: A Meta-Analysis. Gerontologist 2015, 55, 706–718. [Google Scholar] [CrossRef] [PubMed]
- McGarrigle, L.; Todd, C. Promotion of Physical Activity in Older People Using MHealth and EHealth Technologies: Rapid Review of Reviews. J. Med. Internet Res. 2020, 22, e22201. [Google Scholar] [CrossRef] [PubMed]
- D’Amore, C.; Reid, J.C.; Chan, M.; Fan, S.; Huang, A.; Louie, J.; Tran, A.; Chauvin, S.; Beauchamp, M.K. Interventions Including Smart Technology Compared With Face-to-Face Physical Activity Interventions in Older Adults: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2022, 24, e36134. [Google Scholar] [CrossRef]
- Mitzner, T.L.; Boron, J.B.; Fausset, C.B.; Adams, A.E.; Charness, N.; Czaja, S.J.; Dijkstra, K.; Fisk, A.D.; Rogers, W.A.; Sharit, J. Older Adults Talk Technology: Technology Usage and Attitudes. Comput. Human. Behav. 2010, 26, 1710–1721. [Google Scholar] [CrossRef]
- Pargaonkar, A.; Mishra, W.; Kadam, S. A Study on Elderly Individuals’ Attitude towards ICTs. In Proceedings of the 7th International Conference on Research into Design, Bangalore, India, 9–11 January 2019; pp. 723–734. [Google Scholar]
- Garçon, L.; Khasnabis, C.; Walker, L.; Nakatani, Y.; Lapitan, J.; Borg, J.; Ross, A.; Velazquez Berumen, A. Medical and Assistive Health Technology: Meeting the Needs of Aging Populations: Table 1. Gerontologist 2016, 56, S293–S302. [Google Scholar] [CrossRef]
- Indovina, P.; Barone, D.; Gallo, L.; Chirico, A.; De Pietro, G.; Giordano, A. Virtual Reality as a Distraction Intervention to Relieve Pain and Distress during Medical Procedures. Clin. J. Pain. 2018, 34, 858–877. [Google Scholar] [CrossRef]
- Chirico, A.; Lucidi, F.; De Laurentiis, M.; Milanese, C.; Napoli, A.; Giordano, A. Virtual Reality in Health System: Beyond Entertainment. A Mini-Review on the Efficacy of VR During Cancer Treatment. J. Cell Physiol. 2016, 231, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; George, S.; Thomas, S.; Deutsch, J.E.; Crotty, M. Virtual Reality for Stroke Rehabilitation. Cochrane Database Syst. Rev. 2015, 2015, 11. [Google Scholar] [CrossRef] [PubMed]
- Galica, J.; Brennenstuhl, S.; Maheu, C.; Townsley, C.; Metcalfe, K. Examining the Dimensionality of the Fear of Cancer Recurrence Inventory. Psychooncology 2018, 27, 2602–2608. [Google Scholar] [CrossRef] [PubMed]
- Peek, K.; Sanson-Fisher, R.; Mackenzie, L.; Carey, M. Interventions to Aid Patient Adherence to Physiotherapist Prescribed Self-Management Strategies: A Systematic Review. Physiotherapy 2016, 102, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Garritty, C.; Gartlehner, G.; Nussbaumer-Streit, B.; King, V.J.; Hamel, C.; Kamel, C.; Affengruber, L.; Stevens, A. Cochrane Rapid Reviews Methods Group Offers Evidence-Informed Guidance to Conduct Rapid Reviews. J. Clin. Epidemiol. 2021, 130, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO Framework to Improve Searching PubMed for Clinical Questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions. Version 6.4 (Updated August 2023). Cochrane. 2023. Available online: www.training.cochrane.org/handbook (accessed on 20 October 2023).
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Chen, P.J.; Penn, I.W.; Wei, S.H.; Chuang, L.R.; Sung, W.H. Augmented Reality-Assisted Training with Selected Tai-Chi Movements Improves Balance Control and Increases Lower Limb Muscle Strength in Older Adults: A Prospective Randomized Trial. J. Exerc. Sci. Fit. 2020, 18, 142–147. [Google Scholar] [CrossRef]
- Shema, S.R.; Brozgol, M.; Dorfman, M.; Maidan, I.; Sharaby-Yeshayahu, L.; Malik-Kozuch, H.; Yannai, O.W.; Giladi, N.; Hausdorff, J.M.; Mirelman, A. Clinical Experience Using a 5-Week Treadmill Training Program With Virtual Reality to Enhance Gait in an Am-bulatory Physical Therapy Service. Phys. Ther. 2014, 94, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Cho, J.J.; Kim, J.; Kim, Y.; Yoon, B.C. Design of Virtual Reality Training Program for Prevention of Falling in the Elderly: A Pilot Study on Complex versus Balance Exercises. Eur. J. Integr. Med. 2017, 15, 64–67. [Google Scholar] [CrossRef]
- Sadeghi, H.; Jehu, D.A.; Daneshjoo, A.; Shakoor, E.; Razeghi, M.; Amani, A.; Hakim, M.N.; Yusof, A. Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial. Sports Health 2021, 13, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Yousefi Babadi, S.; Daneshmandi, H. Effects of Virtual Reality versus Conventional Balance Training on Balance of the Elderly. Exp. Gerontol. 2021, 153, 111498. [Google Scholar] [CrossRef] [PubMed]
- Park, E.-C.; Kim, S.-G.; Lee, C.-W. The Effects of Virtual Reality Game Exercise on Balance and Gait of the Elderly. J. Phys. Ther. Sci. 2015, 27, 1157–1159. [Google Scholar] [CrossRef] [PubMed]
- Lee, K. Virtual Reality Gait Training to Promote Balance and Gait among Older People: A Randomized Clinical Trial. Geriatrics 2021, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Yim, J.E. A New Approach to Improve Cognition, Muscle Strength, and Postural Balance in Community-Dwelling Elderly with a 3-D Virtual Reality Kayak Program. Tohoku J. Exp. Med. 2015, 238, 1–8. [Google Scholar] [CrossRef]
- Phu, S.; Vogrin, S.; Al Saedi, A.; Duque, G. Balance Training Using Virtual Reality Improves Balance and Physical Performance in Older Adults at High Risk of Falls. Clin. Interv. Aging 2019, 14, 1567–1577. [Google Scholar] [CrossRef]
- Kim, S.H.; Cho, S.H. Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial. Medicina 2022, 58, 1545. [Google Scholar] [CrossRef]
- Yeşilyaprak, S.S.; Yildirim, M.Ş.; Tomruk, M.; Ertekin, Ö.; Algun, Z.C. Comparison of the Effects of Virtual Reality-Based Balance Exercises and Conventional Exercises on Balance and Fall Risk in Older Adults Living in Nursing Homes in Turkey. Physiother. Theory Pract. 2016, 32, 191–201. [Google Scholar] [CrossRef]
- Zahedian-Nasab, N.; Jaberi, A.; Shirazi, F.; Kavousipor, S. Effect of Virtual Reality Exercises on Balance and Fall in Elderly People with Fall Risk: A Randomized Controlled Trial. BMC Geriatr. 2021, 21, 509. [Google Scholar] [CrossRef]
- Al-Emrany, A.M.; Badr, N.M.; Farghaly, A.; Abed El Ghaffar, H. Effect of Virtual Reality Training on Risk of Falls and Quality of Life Among Elderly. Fizjoterapia Pol. 2021, 21, 138–143. [Google Scholar]
- Duque, G.; Boersma, D.; Loza-Diaz, G.; Hassan, S.; Suarez, H.; Geisinger, D.; Suriyaarachchi, P.; Sharma, A.; Demontiero, O. Effects of Balance Training Using a Virtual-Reality System in Older Fallers. Clin. Interv. Aging 2013, 8, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Bacha, J.M.R.; Gomes, G.C.V.; De Freitas, T.B.; Viveiro, L.A.P.; Da Silva, K.G.; Bueno, G.C.; Varise, E.M.; Torriani-Pasin, C.; Alonso, A.C.; Luna, N.M.S.; et al. Effects of Kinect Adventures Games versus Conventional Physical Therapy on Postural Control in Elderly People: A Randomized Controlled Trial. Games Health J. 2018, 7, 24–36. [Google Scholar] [CrossRef] [PubMed]
- Campo-Prieto, P.; Ma Cancela-Carral, J.; Alsina-Rey, B.; Rodríguez-Fuentes, G. Immersive Virtual Reality as a Novel Physical Therapy Approach for Nonagenarians: Usability and Effects on Balance Outcomes of a Game-Based Exercise Program. J. Clin. Med. 2022, 11, 3911. [Google Scholar] [CrossRef] [PubMed]
- Campo-Prieto, P.; Cancela-Carral, J.M.; Rodríguez-Fuentes, G. Feasibility and Effects of an Immersive Virtual Reality Exergame Program on Physical Functions in Institutionalized Older Adults: A Randomized Clinical Trial. Sensors 2022, 22, 6742. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.; Chung, E.; Lee, B.-H. The Effects of Augmented Reality-Based Otago Exercise on Balance, Gait, and Falls Efficacy of Elderly Women. J. Phys. Ther. Sci. 2013, 25, 797–801. [Google Scholar] [CrossRef]
- Hee CHo, G.; HwanGbo, G.; Soo SHin, H. The Effects of Virtual Reality-Based Balance Training on Balance of the Elderly. J. Phys. Ther. Sci. 2014, 26, 615–617. [Google Scholar] [CrossRef]
- Ku, J.; Kim, Y.J.; Cho, S.; Lim, T.; Lee, H.S.; Kang, Y.J. Three-Dimensional Augmented Reality System for Balance and Mobility Rehabilitation in the Elderly: A Randomized Controlled Trial. Cyberpsychol Behav. Soc. Netw. 2019, 22, 132–141. [Google Scholar] [CrossRef]
- Lee, J.; Yoo, H.-N.; Lee, B.-H. Effects of Augmented Reality-Based Otago Exercise on Balance, Gait, and Physical Factors in Elderly Women to Prevent Falls: A Randomized Controlled Trial. J. Phys. Ther. Sci. 2017, 29, 1586–1589. [Google Scholar] [CrossRef]
- Rebsamen, S.; Knols, R.H.; Pfister, P.B.; de Bruin, E.D. Exergame-Driven High-Intensity Interval Training in Untrained Community Dwelling Older Adults: A Formative One Group Quasi-Experimental Feasibility Trial. Front. Physiol. 2019, 10, 1019. [Google Scholar] [CrossRef] [PubMed]
- Fu, A.S.; Gao, K.L.; Tung, A.K.; Tsang, W.W.; Kwan, M.M. Effectiveness of Exergaming Training in Reducing Risk and Incidence of Falls in Frail Older Adults with a History of Falls. Arch. Phys. Med. Rehabil. 2015, 96, 2096–2102. [Google Scholar] [CrossRef] [PubMed]
- De Vries, A.W.; Willaert, J.; Jonkers, I.; Van DIeën, J.H.; Verschueren, S.M.P. Virtual Reality Balance Games Provide Little Muscular Challenge to Prevent Muscle Weakness in Healthy Older Adults. Games Health J. 2020, 9, 227–236. [Google Scholar] [CrossRef] [PubMed]
- da Silva, J.L.A.; Biduski, D.; Bellei, E.A.; Becker, O.H.C.; Daroit, L.; Pasqualotti, A.; Filho, H.T.; de Marchi, A.C.B. A Bowling Exergame to Improve Functional Capacity in Older Adults: Co-Design, Development, and Testing to Compare the Progress of Playing Alone versus Playing with Peers. JMIR Serious Games 2021, 9, e23423. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, G.F.; Cardenas, R.A.M.; Pla, F. A Kinect-Based Interactive System for Home-Assisted Active Aging. Sensors 2021, 21, 417. [Google Scholar] [CrossRef] [PubMed]
- Bickmore, T.W.; Silliman, R.A.; Nelson, K.; Cheng, D.M.; Winter, M.; Henault, L.; Paasche-Orlow, M.K. A Randomized Controlled Trial of an Automated Exercise Coach for Older Adults. J. Am. Geriatr. Soc. 2013, 61, 1676–1683. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.; Kim, J. Effects of Augmented-Reality-Based Exercise on Muscle Parameters, Physical Performance, and Exercise Self-Efficacy for Older Adults. Int. J. Environ. Res. Public. Health 2020, 17, 3260. [Google Scholar] [CrossRef]
- Barsasella, D.; Liu, M.F.; Malwade, S.; Galvin, C.J.; Dhar, E.; Chang, C.C.; Li, Y.C.J.; Syed-Abdul, S. Effects of Virtual Reality Sessions on the Quality of Life, Happiness, and Functional Fitness among the Older People: A Randomized Controlled Trial from Taiwan. Comput. Methods Programs Biomed. 2021, 200, 105892. [Google Scholar] [CrossRef]
- Tammy Lin, J.H.; Wu, D.Y. Exercising With Embodied Young Avatars: How Young vs. Older Avatars in Virtual Reality Affect Perceived Exertion and Physical Activity Among Male and Female Elderly Individuals. Front. Psychol. 2021, 12, 693545. [Google Scholar] [CrossRef]
- Lee, M.; Son, J.; Kim, J.; Yoon, B.C. Individualized Feedback-Based Virtual Reality Exercise Improves Older Women’s Self-Perceived Health: A Randomized Controlled Trial. Arch. Gerontol. Geriatr. 2015, 61, 154–160. [Google Scholar] [CrossRef]
- Nonino, F.; Gomes Bertolini, S.M.M.; Bortolozzi, F.; Magnani Branco, B.H. The Effectiveness of a Home Exercise Program for Sedentary Elderly with Nintendo Wii. J. Phys. Educ. 2018, 29, 2971. [Google Scholar] [CrossRef][Green Version]
- Kamińska, M.S.; Miller, A.; Rotter, I.; Szylińska, A.; Grochans, E. The Effectiveness of Virtual Reality Training in Reducing the Risk of Falls among Elderly People. Clin. Interv. Aging 2018, 13, 2329–2338. [Google Scholar] [CrossRef] [PubMed]
- Garciá-Bravo, S.; Garciá-Bravo, C.; Molina-Rueda, F.; Cuesta-Gómez, A. Training with Wii Balance Board for Dynamic Balance in Older Adults. Top. Geriatr. Rehabil. 2020, 36, 79–85. [Google Scholar] [CrossRef]
- Kruse, L.; Karaosmanoglu, S.; Rings, S.; Ellinger, B.; Steinicke, F. Enabling Immersive Exercise Activities for Older Adults: A Comparison of Virtual Reality Exergames and Traditional Video Exercises. Societies 2021, 11, 134. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and Validation of a Geriatric Depression Screening Scale: A Preliminary Report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Russell, J.A.; Weiss, A.; Mendelsohn, G.A. Affect Grid: A Single-Item Scale of Pleasure and Arousal. J. Pers. Soc. Psychol. 1989, 57, 493–502. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A. The PANAS-X: Manual for the Positive and Negative Affect Schedule-Expanded Form the PANAS-X Manual for the Positive and Negative Affect Schedule-Expanded Form. Dep. Psychol. Brain Sci. Publ. 1999. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- McHorney, C.A.; Ware, J.E.; Raczek, A.E. The MOS 36-Item Short-Form Health Survey (Sf-36): II. Psychometric and Clinical Tests of Validity in Measuring Physical and Mental Health Constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef]
- van Reenen, M.; Oppe, M. EQ-5D-3L User Guide: Basic Information on How to Use the EQ-5D-3L Instrument. EuroQol Res. Found.. 2015. Available online: https://euroqol.org/publications/user-guides (accessed on 26 September 2023).
- Ryan, R.M. Control and Information in the Intrapersonal Sphere: An Extension of Cognitive Evaluation Theory. J. Pers. Soc. Psychol. 1982, 43, 450–461. [Google Scholar] [CrossRef]
- Picorelli, A.M.A.; Pereira, D.S.; Felício, D.C.; Gomes, D.A.; Dias, R.C.; Pereira, L.S.M. Adhesion of Older Women to a Home Exercise Program Post Ambulatory Training. Fisioter. E Pesqui. 2015, 22, 291–308. [Google Scholar]
- Deci, E.L.; Ryan, R.M. The “What” and “Why” of Goal Pursuits: Human Needs and the Self-Determination of Behavior. Psychol. Inq. 2000, 11, 227–268. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and Initial Validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Guide for Constructing Self-Efficacy Scales. Self-Effic. Beliefs Adolesc 2006, 5, 307–337. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Richman, D.; Powell, L. Falls Efficacy as a Measure of Fear of Falling. J. Gerontol. 1990, 45, P239–P243. [Google Scholar] [CrossRef]
- Freitas, S.; Simões, M.R.; Alves, L.; Santana, I. Montreal Cognitive Assessment: Validation Study for Mild Cognitive Impairment and Alzheimer Disease. Alzheimer Dis. Assoc. Disord. 2013, 27, 37–43. [Google Scholar] [CrossRef]
- Borson, S.; Scanlan, J.; Brush, M.; Vitaliano, P.; Dokmak, A. The Mini-Cog: A Cognitive “vital Signs” Measure for Dementia Screening in Multi-Lingual Elderly. Int. J. Geriatr. Psychiatry 2000, 15, 1021–1027. [Google Scholar] [CrossRef]
- Vorderer, P.; Wirth, W.; Gouveia, F.R.; Biocca, F.; Saari, T.; Jäncke, L.; Böcking, S.; Schramm, H.; Gysbers, A.; Hartmann, T.; et al. Mec Spatial Presence Questionnaire (MEC-SPQ): Short Documentation and Instruction for Application. Retrieved Sept. 2004. Report to the European Community, Project Presence: MEC (IST-2001-37661). 2004.
- Bangor, A.; Kortum, P.T.; Miller, J.T. An Empirical Evaluation of the System Usability Scale. Int. J. Hum. Comput. Interact. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Kennedy, R.S.; Lane, N.E.; Berbaum, K.S.; Lilienthal, M.G. Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int. J. Aviat. Psychol. 1993, 3, 203–220. [Google Scholar] [CrossRef]
- IJsselsteijn, W.A.; de Kort, Y.A.W.; Poels, K. Game Experience Questionnaire: Development of a Self-Report Measure to Assess the Psychological Impact of Digital Games—Eindhoven University of Technology Research Portal. In In Proceedings of the PRESENCE 2007, 2007, Barcelona, Spain, 25–27 October.
- Liu, M.; Zhou, K.; Chen, Y.; Zhou, L.; Bao, D.; Zhou, J. Is Virtual Reality Training More Effective Than Traditional Physical Training on Balance and Functional Mobility in Healthy Older Adults? A Systematic Review and Meta-Analysis. Front. Hum. Neurosci. 2022, 16, 843481. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Bajorek, B. Defining ‘Elderly’ in Clinical Practice Guidelines for Pharmacotherapy. Pharm Pr. 2014, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- WHO Ageing. Available online: https://www.who.int/health-topics/ageing#tab=tab_1 (accessed on 26 September 2023).
- Knittle, K.; Nurmi, J.; Crutzen, R.; Hankonen, N.; Beattie, M.; Dombrowski, S.U. How Can Interventions Increase Motivation for Physical Activity? A Systematic Review and Meta-Analysis. Health Psychol. Rev. 2018, 12, 211–230. [Google Scholar] [CrossRef] [PubMed]
- Marquez, D.X.; Aguinãga, S.; Vásquez, P.M.; Conroy, D.E.; Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Sheppard, B.B.; Petruzzello, S.J.; et al. A Systematic Review of Physical Activity and Quality of Life and Well-Being. Transl. Behav. Med. 2020, 10, 1098–1109. [Google Scholar] [CrossRef]
- Hennessy, E.A.; Johnson, B.T.; Acabchuk, R.L.; McCloskey, K.; Stewart-James, J. Self-Regulation Mechanisms in Health Behavior Change: A Systematic Meta-Review of Meta-Analyses, 2006–2017. Health Psychol Rev 2020, 14, 6–42. [Google Scholar] [CrossRef]
- Yen, H.Y.; Chiu, H.L. Virtual Reality Exergames for Improving Older Adults’ Cognition and Depression: A Systematic Review and Meta-Analysis of Randomized Control Trials. J. Am. Med. Dir. Assoc. 2021, 22, 995–1002. [Google Scholar] [CrossRef]
- Schultheis, M.T.; Rizzo, A.A. The Application of Virtual Reality Technology in Rehabilitation. Rehabil. Psychol. 2001, 46, 296–311. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).