The Association between a Minimum Amount of Physical Activity and Subsequent Muscle Strength and Balance in Older Adults: A Prospective Study
Abstract
1. Introduction
2. Materials and Methods
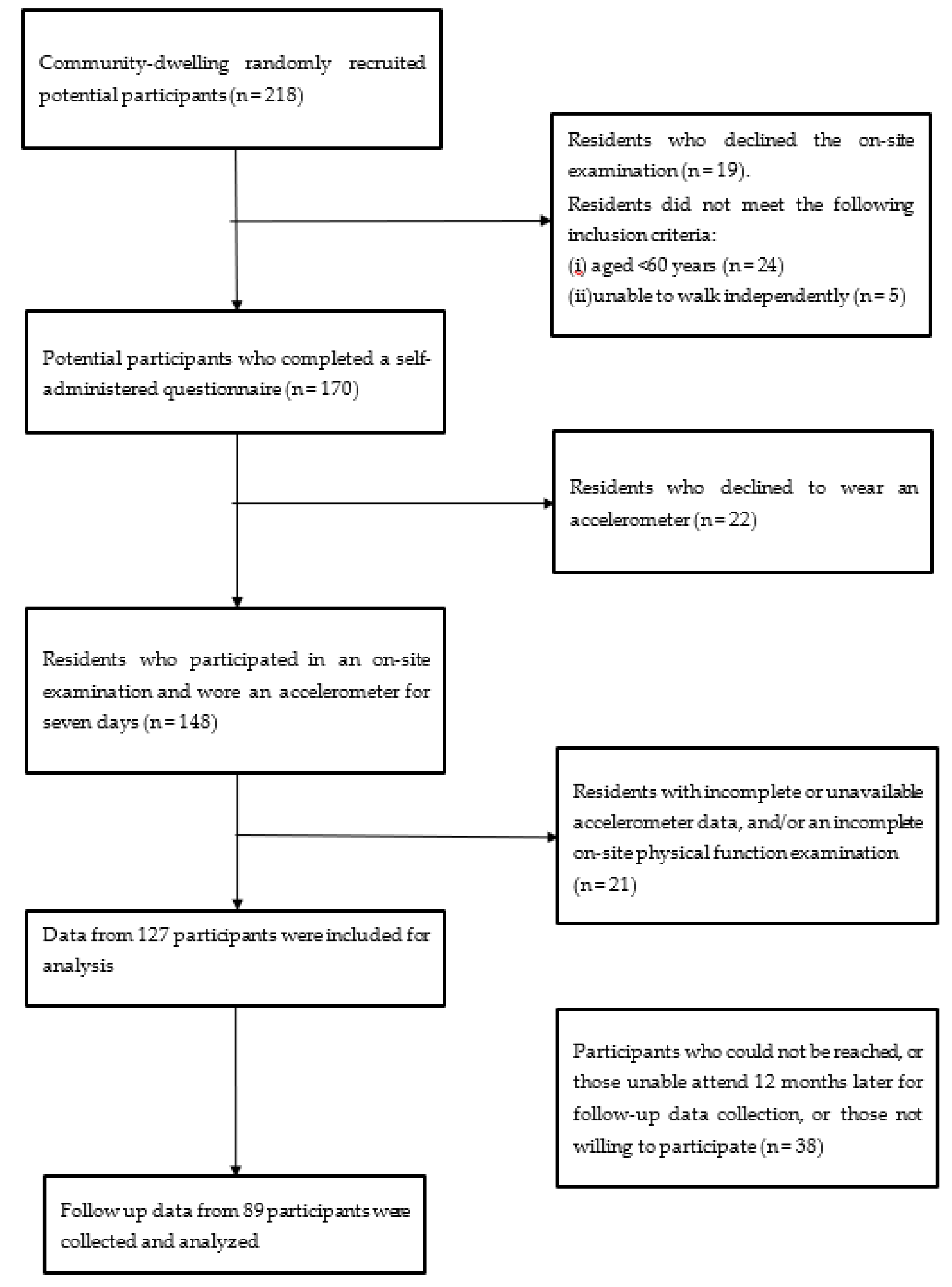
2.1. Participants
2.2. Objectively Measured MVPA
2.3. Muscle Strength
- (a)
- Upper limb strength (hand grip strength test)To estimate upper limb strength, a Jamar Plus+ Digital Hand Dynamometer was used to assessed handgrip strength. This hand grip strength tool is a validated instrument for obtaining rapid results concerning an individual’s general muscle strength [39]. We conducted tests using this tool on both the dominant and non-dominant hands three times, with a timed rest break between each test. Participants were instructed to stand in a natural position and hold the dynamometer in the dominant hand and with the elbow flexed to 90°, while the arm of the non-tested hand rested alongside the body. To ensure a comfortable palm fit on the dynamometer, the width of the dynamometer was adjusted according to the size of the hand. Participants were requested to apply the strongest and fastest possible pressure to the probe and their best test score was used in the analysis [40].
- (b)
- Lower limb strength (five-times STS tests)To estimate lower body strength, we used the five-times STS test [41], which is a functional strength measurement that approximates body movement in daily life and has been widely used in previous studies to measure of lower limb strength [42,43]. Participants were asked to rise from an armless chair five times as fast as possible with their arms folded. The time began on the command of “go” and stopped when the participant completed five repetitions. Each participant was allowed to practice before the timing of three trials, and the average rate from three trials was used in the subsequent analysis.
2.4. Balance
2.5. Covariates
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Health Observatory (GHO) Data: Life Expectancy. 2019. Available online: https://www.who.int/gho/mortality_burden_disease/life_tables/situation_trends/en/ (accessed on 8 November 2019).
- Population Reference Bureau. 2018 World Population Data Sheet. 2018. Available online: https://www.prb.org/2018-world-population-data-sheet-with-focus-on-changing-age-structures/#:~:targetText=PRB%20Projects%202.3%20Billion%20More,Population%20Reference%20Bureau%20(PRB) (accessed on 8 November 2022).
- National Development Council. Population Projection in Republic of China (2018–2065); National Development Council, Ed.; National Development Council: Taipei City, Taiwan, 2018.
- Otsu, K.; Shibayama, K. Population Aging and Potential Growth in Asia. Asian Dev. Rev. 2016, 33, 56–73. [Google Scholar] [CrossRef]
- Harris, A.; Sharma, A. Estimating the future health and aged care expenditure in Australia with changes in morbidity. PLoS ONE 2018, 13, e0201697. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Report on Ageing and Health. 2015. Available online: http://www.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1 (accessed on 8 November 2022).
- Sakamoto, Y.; Ohashi, Y. The relationship between physical function in the elderly and judgment error in walking speed. J. Phys. Ther. Sci. 2017, 29, 1176–1180. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-H.; Chow, H.-W. Comparison of the senior functional fitness test in different countries. Q. Chin. Phys. Educ. 2020, 34, 205–216. [Google Scholar]
- Merchant, R.A.; Morley, J.E.; Izquierdo, M. Exercise, Aging and Frailty: Guidelines for Increasing Function. J. Nutr. Health Aging 2021, 25, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.Y.; Kabeto, M.U.; Galecki, A.T.; Langa, K.M. Physical Functioning Decline and Mortality in Older Adults with Multimorbidity: Joint Modeling of Longitudinal and Survival Data. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 226–232. [Google Scholar] [CrossRef]
- den Ouden, M.E.M.; Schuurmans, M.J.; Brand, J.S.; Arts, I.E.; Mueller-Schotte, S.; van der Schouw, Y.T. Physical functioning is related to both an impaired physical ability and ADL disability: A ten year follow-up study in middle-aged and older persons. Maturitas 2013, 74, 89–94. [Google Scholar] [CrossRef]
- Byrne, C.; Faure, C.; Keene, D.J.; Lamb, S.E. Ageing, Muscle Power and Physical Function: A Systematic Review and Implications for Pragmatic Training Interventions. Sport. Med. 2016, 46, 1311–1332. [Google Scholar] [CrossRef]
- Kim, E.S.; Kawachi, I.; Chen, Y.; Kubzansky, L.D. Association Between Purpose in Life and Objective Measures of Physical Function in Older Adults. JAMA Psychiatry 2017, 74, 1039–1045. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.T.; Wang, H.S. Interference effect of concurrent training on muscle strength in elderly people—A literature review. Q. Chin. Phys. Educ. 2021, 35, 11–20. [Google Scholar]
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 2018, 9, 3–19. [Google Scholar] [CrossRef]
- Yang, N.P.; Hsu, N.W.; Lin, C.H.; Chen, H.C.; Tsao, H.M.; Lo, S.S.; Chou, P. Relationship between muscle strength and fall episodes among the elderly: The Yilan study, Taiwan. BMC Geriatr. 2018, 18, 90. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Araque, A.; Giaquinta-Aranda, A.; Rodríguez-Díez, J.A.; Carretero-Molinero, S.; López-López, J.; Verde, Z. Muscular Strength and Quality of Life in Older Adults: The Role of ACTN3 R577X Polymorphism. Int. J. Environ. Res. Public Health 2021, 18, 1055. [Google Scholar] [CrossRef] [PubMed]
- Halvarsson, A.; Dohrn, I.-M.; Ståhle, A. Taking balance training for older adults one step further: The rationale for and a description of a proven balance training programme. Clin. Rehabil. 2015, 29, 417–425. [Google Scholar] [CrossRef]
- Li, Z.S.; Chiu, W.H.; Chen, Y.Y. The influence of exercise interventions on balance and gait in older adults: A systematic review. Q. Chin. Phys. Educ. 2022, 36, 137–154. [Google Scholar]
- Cofré Lizama, L.E.; Pijnappels, M.; Faber, G.H.; Reeves, P.N.; Verschueren, S.M.; van Dieën, J.H. Age Effects on Mediolateral Balance Control. PLoS ONE 2014, 9, e110757. [Google Scholar] [CrossRef] [PubMed]
- Mayer, F.; Scharhag-Rosenberger, F.; Carlsohn, A.; Cassel, M.; Müller, S.; Scharhag, J. The intensity and effects of strength training in the elderly. Dtsch. Arztebl. Int. 2011, 108, 359–364. [Google Scholar] [CrossRef]
- Bauman, A.; Merom, D.; Bull, F.C.; Buchner, D.M.; Fiatarone Singh, M.A. Updating the Evidence for Physical Activity: Summative Reviews of the Epidemiological Evidence, Prevalence, and Interventions to Promote “Active Aging”. Gerontologist 2016, 56 (Suppl. 2), S268–S280. [Google Scholar] [CrossRef]
- Dipietro, L.; Campbell, W.W.; Buchner, D.M.; Erickson, K.I.; Powell, K.E.; Bloodgood, B.; Hughes, T.; Day, K.R.; Piercy, K.L.; Vaux-Bjerke, A.; et al. Physical Activity, Injurious Falls, and Physical Function in Aging: An Umbrella Review. Med. Sci. Sport. Exerc. 2019, 51, 1303–1313. [Google Scholar] [CrossRef]
- Dugan, S.A.; Gabriel, K.P.; Lange-Maia, B.S.; Karvonen-Gutierrez, C. Physical Activity and Physical Function: Moving and Aging. Obstet. Gynecol. Clin. N. Am. 2018, 45, 723–736. [Google Scholar] [CrossRef]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sport. Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Daskalopoulou, C.; Stubbs, B.; Kralj, C.; Koukounari, A.; Prince, M.; Prina, A.M. Physical activity and healthy ageing: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 2017, 38, 6–17. [Google Scholar] [CrossRef] [PubMed]
- McMullan, I.I.; McDonough, S.M.; Tully, M.A.; Cupples, M.; Casson, K.; Bunting, B.P. The association between balance and free-living physical activity in an older community-dwelling adult population: A systematic review and meta-analysis. BMC Public Health 2018, 18, 431. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed.; U.S. Department of Health and Human Services: Washington, DC, USA, 2018.
- Kortajarena, M.; Zarrazquin, I.; Irazusta, J.; Gil-Goikouria, J.; Irazusta, A.; Hervás, G.; Iturburu, M.; Yanguas, J.J.; Hoyos Cillero, I.; Fraile-Bermúdez, A.B. Objectively and subjectively measured physical activity and its relation to cardiovascular risk factors in older people—Which is most appropriate? Maturitas 2019, 123, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Annear, M. Sedentary Behavior and Physical Inactivity in the Asia-Pacific Region: Current Challenges and Emerging Concerns. Int. J. Environ. Res. Public Health 2022, 19, 9351. [Google Scholar] [CrossRef] [PubMed]
- Solberg, P.A.; Kvamme, N.H.; Raastad, T.; Ommundsen, Y.; Tomten, S.E.; Halvari, H.; Loland, N.W.; Hallén, J. Effects of different types of exercise on muscle mass, strength, function and well-being in elderly. Eur. J. Sport Sci. 2013, 13, 112–125. [Google Scholar] [CrossRef]
- Thomas, E.; Battaglia, G.; Patti, A.; Brusa, J.; Leonardi, V.; Palma, A.; Bellafiore, M. Physical activity programs for balance and fall prevention in elderly: A systematic review. Medicine 2019, 98, e16218. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Norman, I.J.; While, A.E. Physical activity in older people: A systematic review. BMC Public Health 2013, 13, 449. [Google Scholar] [CrossRef]
- Wen, C.P.; Wai, J.P.M.; Tsai, M.K.; Yang, Y.C.; Cheng, T.Y.D.; Lee, M.C.; Chan, H.T.; Tsao, C.K.; Tsai, S.P.; Wu, X.; et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet 2011, 378, 1244–1253. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sport. Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Lai, T.F.; Liao, Y.; Lin, C.Y.; Huang, W.C.; Hsueh, M.C.; Chan, D.C. Moderate-to-vigorous physical activity duration is more important than timing for physical function in older adults. Sci. Rep. 2020, 10, 21344. [Google Scholar] [CrossRef]
- Lai, T.F.; Liao, Y.; Hsueh, M.C.; Yen, H.Y.; Park, J.H.; Chang, J.H. Substituting sedentary time with physical activity in youngest-old to oldest-old community-dwelling older adults: Associations with body composition. Front. Public Health 2022, 10, 837213. [Google Scholar] [CrossRef]
- Wind, A.E.; Takken, T.; Helders, P.J.; Engelbert, R.H. Is grip strength a predictor for total muscle strength in healthy children, adolescents, and young adults? Eur. J. Pediatr. 2010, 169, 281–287. [Google Scholar] [CrossRef]
- Gafner, S.C.; Bastiaenen, C.H.; Ferrari, S.; Gold, G.; Terrier, P.; Hilfiker, R.; Allet, L. Hip muscle and hand-grip strength to differentiate between older fallers and non-fallers: A cross-sectional validity study. Clin. Interv. Aging 2017, 13, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Yee, X.S.; Ng, Y.S.; Allen, J.C.; Latib, A.; Tay, E.L.; Bakar, H.M.A.; Ho, C.Y.J.; Koh, W.C.C.; Kwek, H.H.T.; Tay, L. Performance on sit-to-stand tests in relation to measures of functional fitness and sarcopenia diagnosis in community-dwelling older adults. Eur. Rev. Aging Phys. Act. 2021, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- Thaweewannakij, T.; Suwannarat, P.; Mato, L.; Amatachaya, S. Functional ability and health status of community-dwelling late age elderly people with and without a history of falls. Hong Kong Physiother. J. 2016, 34, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.R.; Murray, S.M.; Chapman, K.; Munro, B.; Tiedemann, A. Sit-to-Stand Performance Depends on Sensation, Speed, Balance, and Psychological Status in Addition to Strength in Older People. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2002, 57, M539–M543. [Google Scholar] [CrossRef]
- Vellas, B.J.; Wayne, S.J.; Romero, L.; Baumgartner, R.N.; Rubenstein, L.Z.; Garry, P.J. One-Leg Balance Is an Important Predictor of Injurious Falls in Older Persons. J. Am. Geriatr. Soc. 1997, 45, 735–738. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.; Hsueh, M.C.; Liao, Y. Associations between objectively measured sedentary behavior patterns and depressive symptoms in older adults: A cross sectional study. Ment. Health Phys. Act. 2022, 23, 100471. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Gouveia, B.R.; Gonçalves Jardim, H.; Martins, M.M.; Gouveia, É.R.; de Freitas, D.L.; Maia, J.A.; Rose, D.J. An evaluation of a nurse-led rehabilitation programme (the ProBalance Programme) to improve balance and reduce fall risk of community-dwelling older people: A randomised controlled trial. Int. J. Nurs. Stud. 2016, 56, 1–8. [Google Scholar] [CrossRef]
- Lin, E.S.; Fang, I.Y.; Chen, J.F. Interventional benefits of ecological models applied to community-based exercise programs for elderly. Q. Chin. Phys. Educ. 2022, 36, 233–242. [Google Scholar]
- Loprinzi, P.D.; Brosky, J.A., Jr. Objectively measured physical activity and balance among U.S. adults. J. Strength Cond. Res. 2014, 28, 2290–2296. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Michaleff, Z.A.; Fairhall, N.; Paul, S.S.; Tiedemann, A.; Whitney, J.; Cumming, R.G.; Herbert, R.D.; Close, J.C.T.; Lord, S.R. Exercise to prevent falls in older adults: An updated systematic review and meta-analysis. Br. J. Sport. Med. 2017, 51, 1750–1758. [Google Scholar] [CrossRef]
- Hills, A.P.; Street, S.J.; Byrne, N.M. Chapter Three—Physical Activity and Health: “What is Old is New Again”. In Advances in Food and Nutrition Research; Henry, J., Ed.; Academic Press: Cambridge, MA, USA; pp. 77–95.
- Dishman, R.K.; Heath, G.W.; Lee, I.-M. Physical Activity Epidemiology; Human Kinetics: Champaign, IL, USA, 2012. [Google Scholar]
- Spartano, N.L.; Lyass, A.; Larson, M.G.; Tran, T.; Andersson, C.; Blease, S.J.; Esliger, D.W.; Vasan, R.S.; Murabito, J.M. Objective physical activity and physical performance in middle-aged and older adults. Exp. Gerontol. 2019, 119, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Pescatello, L.S.; Riebe, D.; Thompson, P.D. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
| Variables | Total Sample (N = 89) | MVPA < 15 min/day (N = 31) | MVPA ≥ 15 min/day (N = 58) | p (<0.05) |
|---|---|---|---|---|
| Baseline-Age (M ± SD) | 69.54 ± 4.88 | 71.94 ± 5.35 | 68.26 ± 4.11 | 0.012 * |
| Ages 65–74 | 84.3% | 71.0% | 91.4% | |
| Aged ≥75 | 15.7% | 29.0% | 8.6% | |
| Sex (%) | 0.013 * | |||
| Men | 29.2% | 12.9% | 37.9% | |
| Women | 70.8% | 87.1% | 62.1% | |
| Educational level (%) | 0.035 * | |||
| University | 22.5% | 9.7% | 29.3% | |
| Up to high school | 77.5% | 90.3% | 70.7% | |
| Marital status (%) | 0.001 ** | |||
| Married | 67.4% | 45.2% | 79.3% | |
| Not married | 32.6% | 54.8% | 20.7% | |
| Employment (%) | 0.649 | |||
| Full-time job | 2.2% | 3.2% | 1.7% | |
| Not full-time | 97.8% | 96.8% | 98.3% | |
| Living status (%) | 0.345 | |||
| Living with others | 91.0% | 87.1% | 93.1% | |
| Living alone | 9.0% | 12.9% | 6.9% | |
| Depression (%) | 0.032 * | |||
| Yes | 12.4% | 22.6% | 6.9% | |
| No | 87.6% | 77.4% | 93.1% | |
| Hypertension (%) | 0.915 | |||
| Yes | 42.7% | 41.9% | 43.1% | |
| No | 57.3% | 58.1% | 56.9% | |
| Diabetes (%) | 0.805 | |||
| Yes | 18.0% | 19.4% | 17.2% | |
| No | 82.0% | 80.6% | 82.8% | |
| Hyperlipidemia (%) | 0.857 | |||
| Yes | 27.0% | 25.8% | 27.6% | |
| No | 73.0% | 74.2% | 72.4% | |
| Alcohol | 0.868 | |||
| Yes | 9.0% | 9.7% | 8.6% | |
| No | 91.0% | 90.3% | 91.4% | |
| Smoking | 0.419 | |||
| Yes | 6.7% | 9.7% | 5.2% | |
| No | 93.3 | 90.3% | 94.8% | |
| Sedentary Time (M±SD) | 10.07 ± 1.26 | 10.51 ± 1.48 | 9.84 ± 1.07 | 0.602 |
| <9 h/day | 19.1% | 16.1% | 20.7% | |
| ≥9 h/day | 80.9% | 83.9% | 79.3%i | |
| Health Intake | 0.497 | |||
| Yes | 69.7% | 74.2% | 67.2% | |
| No | 30.3% | 25.8% | 32.8% | |
| BMI (kg/m2) M ± SD | 24.29 ± 3.26 | 25.00 ± 3.72 | 23.92 ± 2.95 | 0.443 |
| Normal weight (%) | 53.9% | 48.4% | 56.9% | |
| Overweight (%) | 46.1% | 51.6% | 43.1% |
| M (SD) (n = 89) | ||
|---|---|---|
| Accelerometer variables | ||
| Wear time (min/day) | 921.86 (84.99) | |
| Daily MVPA time (min/day) | 25.92 (22.63) | |
| Daily Sedentary time (min/day) | 604.34 (75.46) | |
| Muscle Strength | ||
| Handgrip Strength (Kg) | Baseline | 25.14 (7.12) |
| Follow-Up | 26.31 (7.04) | |
| Five-Times STS Test (s) | Baseline | 6.86 (1.59) |
| Follow-Up | 6.78 (1.83) | |
| Balance | ||
| One Leg Standing Test (s) | Baseline | 39.05 (22.55) |
| Follow-Up | 45.65 (21.85) |
| Total (%) | MVPA < 15 min/day (%) | MVPA ≥ 15 min/day (%) | ||||
|---|---|---|---|---|---|---|
| Improvement Maintenance | Decline | Improvement Maintenance | Decline | Improvement Maintenance | Decline | |
| Grip strength | 66.3 | 33.7 | 67.7 | 32.3 | 65.5 | 34.5 |
| Five-Times STS | 52.8 | 47.2 | 29.0 | 71.0 | 65.5 | 34.5 |
| One Leg Standing | 76.4 | 23.6 | 54.8 | 45.2 | 87.9 | 12.1 |
| Upper Strength | Lower Strength | Balance | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Model 1 | ||||||
| <15 min MVPA per day | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| ≥15 min MVPA per day | 0.905 (0.358–2.287) | 0.833 | 4.644 (1.804–11.959) | 0.001 * | 6.000 (2.078–17.325) | 0.001 * |
| Model 2 | ||||||
| <15 min MVPA per day | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| ≥15 min of MVPA per day | 0.731 (0.210–2.542) | 0.622 | 2.471 (0.767–7.957) | 0.130 | 6.462 (1.455–28.704) | 0.014 * |
| Model 3 | ||||||
| <15 min of MVPA per day | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | |||
| ≥15 min of MVPA per day | 0.709 (0.202–2.488) | 0.592 | 2.814 (0.825–9.596) | 0.098 | 8.123 (1.611–40.966) | 0.011 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.-Y.; Hsueh, M.-C.; Park, J.-H.; Lai, T.-F.; Hung, Y.-C.; Liao, Y. The Association between a Minimum Amount of Physical Activity and Subsequent Muscle Strength and Balance in Older Adults: A Prospective Study. Behav. Sci. 2023, 13, 316. https://doi.org/10.3390/bs13040316
Li Y-Y, Hsueh M-C, Park J-H, Lai T-F, Hung Y-C, Liao Y. The Association between a Minimum Amount of Physical Activity and Subsequent Muscle Strength and Balance in Older Adults: A Prospective Study. Behavioral Sciences. 2023; 13(4):316. https://doi.org/10.3390/bs13040316
Chicago/Turabian StyleLi, Yuan-Yu, Ming-Chun Hsueh, Jong-Hwan Park, Ting-Fu Lai, Yi-Chuan Hung, and Yung Liao. 2023. "The Association between a Minimum Amount of Physical Activity and Subsequent Muscle Strength and Balance in Older Adults: A Prospective Study" Behavioral Sciences 13, no. 4: 316. https://doi.org/10.3390/bs13040316
APA StyleLi, Y.-Y., Hsueh, M.-C., Park, J.-H., Lai, T.-F., Hung, Y.-C., & Liao, Y. (2023). The Association between a Minimum Amount of Physical Activity and Subsequent Muscle Strength and Balance in Older Adults: A Prospective Study. Behavioral Sciences, 13(4), 316. https://doi.org/10.3390/bs13040316







