Changes in Oral Health Behavior According to Dental Calculus Removal Health Insurance in Korea
Abstract
1. Introduction
2. Materials and Methods
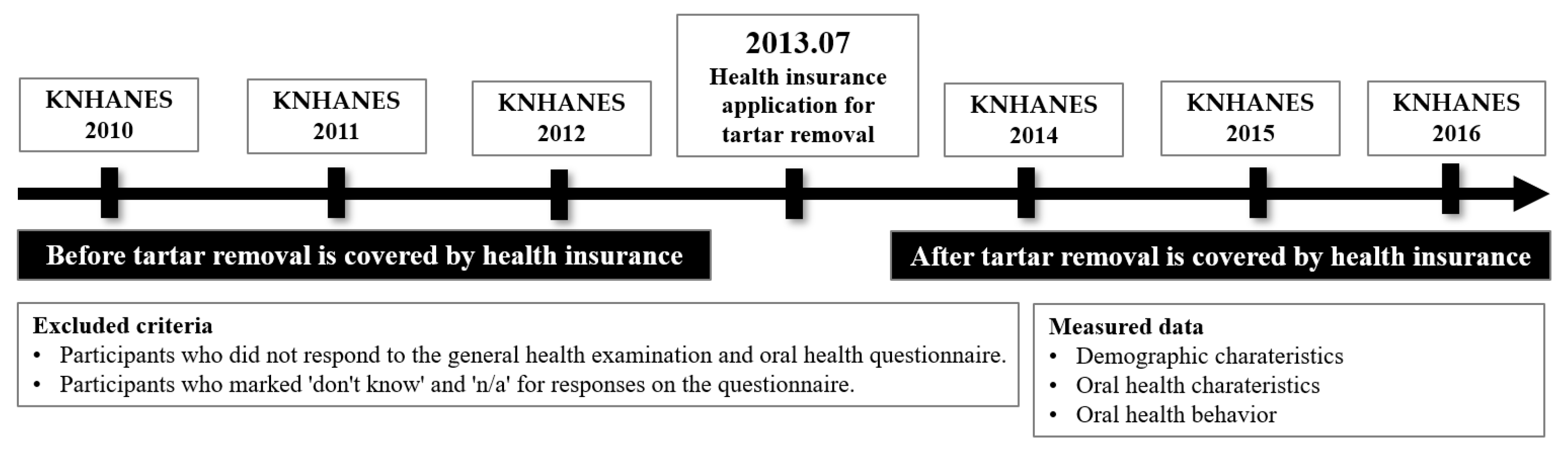
2.1. Study Design
2.2. Setting
2.3. Study Participants
2.4. Variables
2.4.1. Demographic Characteristics
2.4.2. Oral Health Characteristics
2.4.3. Oral Health Behavior
2.5. Data Sources/Measurement
2.6. Bias
2.7. Study Size
2.8. Quantitative Variables
2.9. Statistical Methods
3. Results
3.1. Comparison of the Demographic Characteristics before and after the Once-a-Year Scaling Insurance
3.2. Comparison of the Oral Health Characteristics before and after the Once-a-Year Scaling Insurance Application
3.3. Comparison of Dental-Clinic Use before and after the Once-a-Year Scaling Insurance Application
3.4. Comparison of Brushing before and after the Once-a-Year Scaling Insurance
3.5. Comparison of the Use of Oral Care Supplies before and after the Once-a-Year Scaling Insurance Application
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Livingston, M.; Parsell, D.; Pollack, S. Periodontal disease: Systemic risk factors. J. Correct. Health Care 2002, 9, 247–255. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Oral Health. Available online: https://www.cdc.gov/oralhealth/about/healthy-people-2020.html (accessed on 23 February 2023).
- Gil-Montoya, J.A.; de Mello, A.L.; Barrios, R.; Gonzalez-Moles, M.A.; Bravo, M. Oral health in the elderly patient and its impact on general well-being: A nonsystematic review. Clin. Interv. Aging 2015, 11, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Won, J.H.; Ha, M.N. An association of periodontitis and diabetes. J. Dent. Hyg. Sci. 2014, 14, 107–113. [Google Scholar]
- Jo, M.J.; Min, K.J. Effect of repeated directing tooth-brushing education on plaque control. J. Korea Acad. Industr. Coop. Soc. 2010, 11, 2088–2092. [Google Scholar]
- Ximenez-Fyvie, L.A.; Haffajee, A.D.; Som, S.; Thompson, M.; Torresyap, G.; Socransky, S.S. The effect of repeated professional supragingival plaque removal on the composition of the supra-and subgingival microbiota. J. Clin. Periodontol. 2000, 27, 637–647. [Google Scholar] [CrossRef]
- Kang, H.J. Policy directions for the national health insurance for 2017: Harmonizing equity and efficiency through innovation. Health Welf. Forum 2017, 243, 18–28. [Google Scholar]
- Lee, Y.M. Health policy for the people. J. Korean Med. Assoc. 2017, 60, 286–288. [Google Scholar] [CrossRef]
- Lee, T.R.; Bae, S.M.; Kim, H.J. Awareness of the cost of dental care consumers after the reimbursement of preventive scaling. J. Next-Gener. Converg. Technol. Assoc. 2022, 6, 1478–1485. [Google Scholar]
- An, H.H.; Lee, M.H.; Seo, H.J. Oral hygiene performance ability according to toothbrushing instruction. J. Korea Soc. Health. Inform. Stat. 2012, 37, 43–52. [Google Scholar]
- Jeong, S.H.; Kim, J.Y.; Park, J.H.; Choi, Y.H.; Song, K.B.; Kim, Y.J. Dental caries status and related factors among disabled children and adolescent in Korea. J. Korean Acad. Pediatr. Dent. 2008, 35, 102–109. [Google Scholar]
- Page, R.C.; Beck, J.D. Risk assessment for periodontal diseases. Int. Dent. J. 1997, 47, 61–87. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance Service. Policy Center. Available online: https://www.nhis.or.kr/static/html/wbma/c/wbmac0218.html (accessed on 23 February 2023).
- Lee, H.S.; Lee, K.H. Recognition about national health insurance of dental scaling in industry accident injury patients. J. Korean Soc. Dent. Hyg. 2013, 13, 561–568. [Google Scholar] [CrossRef]
- Ju, O.J.; Kang, E.J.; Woo, S.H.; Lee, H.J. Recognition between layperson and dental hygienists on expansion of health insurance of scaling. J. Korean. Soc. Dent. Hyg. 2014, 14, 431–438. [Google Scholar] [CrossRef]
- Lee, M.S.; Lim, H.J. The factors of oral health beliefs on scaling performance by national health insurance coverage in consumers. J. Korean Soc. Dent. Hyg. 2015, 15, 31–38. [Google Scholar] [CrossRef]
- Kim, Y.T.; Lee, J.H.; Kweon, H.I.; Lee, J.S.; Choi, J.K.; Kim, D.W.; Choi, S.H. Evaluation of national health insurance coverage of periodontal scaling: A nationwide cohort study in Korea. J. Korea Dent. Assoc. 2016, 54, 604–612. [Google Scholar]
- Page, R.C.; Schroeder, H.E. Pathogenesis of inflammatory periodontal disease. A summary of current work. Lab. Invest. 1976, 34, 235–249. [Google Scholar]
- Park, H.J.; Lee, J.H. The effect of socioeconomic status, oral health consciousness and behaviors on the periodontal-health disparities among Korean adults. Korean J. Health Edu. Promot. 2010, 27, 61–66. [Google Scholar]
- Park, H.J.; Lee, J.H.; Cho, S.H.; Heo, S.; Yoon, C.Y.; Baek, S.Y. Establishment of analytical methods for HPHC list of mainstream cigarette smoke. Anal. Sci. Technol. 2015, 28, 385–397. [Google Scholar] [CrossRef]
- Lee, H.S.; Kim, M.E. Effects of smoking on oral health: Preliminary evaluation for a long-term study of a group with good oral hygiene. J. Oral Med. Pain. 2011, 36, 225–234. [Google Scholar]
- Yoon, U.Y.; Yang, W.H. PHP index according to toothbrushing behavior and smoke status of some local residents. Korean Soc. Dent. Hyg. 2013, 13, 261–269. [Google Scholar] [CrossRef]
- Jo, B.D.; Kim, D.K.; Lee, B.J. Change in plaque control ability by the professional oral health care program. J. Korean Acad. Oral Health 2015, 39, 25–36. [Google Scholar] [CrossRef]
- Kim, J.B.; Paik, D.I.; Moon, H.S.; Jin, B.H.; Song, Y.H. Dentists and dental patients attitudes toward oral hygiene devices selection. J. Korean Acad. Oral Health 1992, 16, 493–504. [Google Scholar]
- Kim, H.S. Evolution of microbiology in the 21st century and the change of oral health care management paradigm. J. Korean Acad. Dent. Administ. 2018, 6, 1–10. [Google Scholar]
- Lee, B.J. Oral health care professionals with toothpick toothbrushing program. J. Korean Dent. Assoc. 2009, 47, 272–281. [Google Scholar]
| Before | After | p * | ||
|---|---|---|---|---|
| Gender | Male | 9330 (49.4) | 8400 (50.6) | 0.871 |
| Female | 1226 (49.3) | 10,950 (50.7) | ||
| Total | 21,595 (49.4) | 19,350 (50.6) | ||
| Age | <20 | 5365 (52.3) | 4322 (47.7) | 0.000 |
| 20–39 | 4506 (50.7) | 3939 (49.3) | ||
| 40–59 | 5942 (48.2) | 5518 (51.8) | ||
| 60≤ | 5782 (45.8) | 5571 (54.2) | ||
| Total | 21,595 (49.4) | 19,350 (50.6) | ||
| Marital status | Married | 14,322 (48.7) | 13,003 (51.3) | 0.012 |
| Single | 7223 (50.3) | 6346 (49.7) | ||
| Total | 21,545 (49.3) | 19,349 (50.7) | ||
| Economic activity | Active | 9151 (50.5) | 8120 (49.5) | 0.148 |
| None | 7519 (49.5) | 6591 (50.5) | ||
| Total | 16,670 (50.1) | 14,711 (49.9) | ||
| Household income | Lower | 4199 (51.8) | 3822 (48.2) | 0.000 |
| Lower-middle | 4339 (51.0) | 3845 (49.0) | ||
| Middle | 4298 (49.3) | 3840 (50.7) | ||
| High-middle | 4259 (47.5) | 3891 (52.5) | ||
| High | 4239 (45.8) | 3864 (54.2) | ||
| Total | 21,334 (49.2) | 19,262 (50.8) |
| Before | After | p * | ||
|---|---|---|---|---|
| Oral examination | No | 14,599 (52.3) | 11,761 (47.7) | 0.000 |
| Yes | 6338 (43.5) | 6895 (56.5) | ||
| Total | 20,937 (49.5) | 18,656 (50.5) | ||
| Consultation on drinking problems | No | 13,350 (47.4) | 13,227 (52.6) | 0.000 |
| Yes | 181 (67.0) | 89 (33.0) | ||
| Total | 13,531 (47.6) | 13,316 (52.4) | ||
| Currently smoking | Every day | 2623 (53.4) | 2126 (46.6) | 0.000 |
| Sometimes | 300 (45.0) | 347 (55.0) | ||
| Non-smoking | 3242 (48.3) | 3000 (51.7) | ||
| Total | 6165 (50.0) | 5475 (49.5) | ||
| Willingness to quit smoking ** | 2.28 ± 0.02 | 2.37 ± 0.03 | 0.008 | |
| Chewing problem ** | 2.31 ± 0.02 | 2.22 ± 0.01 | 0.000 | |
| Speaking problem ** | 1.64 ± 0.02 | 1.62 ± 0.001 | 0.110 | |
| Before | After | p * | ||
|---|---|---|---|---|
| Dental-clinic use | Used | 4305 (27.2) | 10,304 (72.8) | 0.000 |
| Unused | 16,633 (62.8) | 8352 (37.2) | ||
| Total | 20,938 (49.4) | 18,656 (50.6) | ||
| Oral examination | Inexperienced | 2365 (50.7) | 1958 (49.3) | 0.000 |
| Experienced | 1990 (17.8) | 8346 (82.2) | ||
| Total | 4355 (27.4) | 10,304 (72.6) | ||
| Periodontal treatment | Inexperienced | 3787 (28.6) | 8345 (71.4) | 0.000 |
| Experienced | 568 (21.9) | 1959 (78.1) | ||
| Total | 4355 (27.4) | 10,304 (72.6) | ||
| Caries treatment | Inexperienced | 3127 (28.1) | 7068 (71.9) | 0.022 |
| Experienced | 1228 (25.9) | 3236 (74.1) | ||
| Total | 4355 (27.4) | 10,304 (72.6) | ||
| Dental pulp treatment | Inexperienced | 3764 (28.4) | 8369 (71.6) | 0.000 |
| Experienced | 591 (22.9) | 1935 (77.1) | ||
| Total | 4355 (27.4) | 10,304 (72.6) | ||
| Oral prevention | Inexperienced | 3488 (35.2) | 5889 (64.8) | 0.000 |
| Experienced | 867 (14.9) | 4415 (85.1) | ||
| Total | 4355 (27.4) | 10,304 (72.6) | ||
| Oral surgical treatment | Inexperienced | 3909 (27.9) | 9028 (72.1) | 0.012 |
| Experienced | 446 (24.2) | 1276 (75.8) | ||
| Total | 4355 (27.4) | 10,304 (72.6) | ||
| Trauma treatment | Inexperienced | 4260 (27.4) | 10,089 (72.6) | 0.223 |
| Experienced | 95 (31.0) | 215 (69.0) | ||
| Total | 4355 (27.4) | 10,304 (72.6) | ||
| Prosthetic treatment | Inexperienced | 3494 (28.0) | 8169 (72.0) | 0.006 |
| Experienced | 861 (24.8) | 2135 (75.2) | ||
| Total | 4355 (27.4) | 10,304 (72.6) |
| Before | After | p * | ||
|---|---|---|---|---|
| Yesterday brushing | No | 364 (43.3) | 410 (56.7) | 0.007 |
| Yes | 20,573 (49.5) | 18,251 (50.5) | ||
| Total | 20,937 (49.4) | 18,661 (50.6) | ||
| Before breakfast | No | 16,354 (54.1) | 12,241 (45.9) | 0.000 |
| Yes | 4270 (38.9) | 6010 (61.1) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) | ||
| After breakfast | No | 5457 (43.7) | 6175 (56.3) | 0.000 |
| Yes | 15,167 (52.5) | 12,076 (47.5) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) | ||
| Before lunch | No | 20,407 (49.7) | 17,987 (50.3) | 0.014 |
| Yes | 217 (41.1) | 264 (58.9) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) | ||
| After lunch | No | 12,231 (53.3) | 9515 (46.7) | 0.000 |
| Yes | 8393 (45.1) | 8736 (54.9) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) | ||
| Before dinner | No | 20,193 (49.7) | 17,819 (50.3) | 0.418 |
| Yes | 431 (47.8) | 432 (52.2) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) | ||
| After dinner | No | 7183 (43.1) | 8204 (56.9) | 0.000 |
| Yes | 13,441 (53.9) | 10,047 (46.1) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) | ||
| After snacking | No | 20,182 (49.9) | 17,651 (50.1) | 0.000 |
| Yes | 442 (40.1) | 600 (59.9) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) | ||
| Before sleeping | No | 14,062 (57.1) | 9478 (42.9) | 0.000 |
| Yes | 6562 (39.3) | 8773 (60.7) | ||
| Total | 20,624 (49.6) | 18,251 (50.4) |
| Before | After | p * | ||
|---|---|---|---|---|
| Dental floss | Unused | 7367 (33.5) | 12,619 (66.5) | 0.000 |
| Use | 2383 (37.8) | 3326 (62.2) | ||
| Interdental toothbrush | Unused | 7583 (34.2) | 13,054 (65.8) | 0.129 |
| Use | 2167 (35.6) | 2893 (64.4) | ||
| Toothpaste solution | Unused | 8223 (35.3) | 12,592 (64.7) | 0.000 |
| Use | 1527 (31.2) | 3355 (68.8) | ||
| Electric toothbrush | Unused | 9040 (33.8) | 15,215 (66.2) | 0.000 |
| Use | 710 (45.5) | 732 (54.5) | ||
| Other | Unused | 9073 (34.4) | 15,004 (65.6) | 0.538 |
| Use | 677 (35.4) | 943 (64.6) | ||
| Total | 9750 (34.5) | 15,947 (65.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.-R.; Kang, H.-K. Changes in Oral Health Behavior According to Dental Calculus Removal Health Insurance in Korea. Behav. Sci. 2023, 13, 315. https://doi.org/10.3390/bs13040315
Kim Y-R, Kang H-K. Changes in Oral Health Behavior According to Dental Calculus Removal Health Insurance in Korea. Behavioral Sciences. 2023; 13(4):315. https://doi.org/10.3390/bs13040315
Chicago/Turabian StyleKim, Yu-Rin, and Hyun-Kyung Kang. 2023. "Changes in Oral Health Behavior According to Dental Calculus Removal Health Insurance in Korea" Behavioral Sciences 13, no. 4: 315. https://doi.org/10.3390/bs13040315
APA StyleKim, Y.-R., & Kang, H.-K. (2023). Changes in Oral Health Behavior According to Dental Calculus Removal Health Insurance in Korea. Behavioral Sciences, 13(4), 315. https://doi.org/10.3390/bs13040315







