Depression and Anxiety Mediate the Association between Sleep Quality and Self-Rated Health in Healthcare Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Procedure
2.2. Measures
2.2.1. Sleep Quality Questionnaire (Chinese Version)
2.2.2. Patient Health Questionnaire (Chinese Version)
2.2.3. Self-Rated Health Questionnaire
2.2.4. Sample Description
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Associations among Sleep Quality, Mental Health Symptoms, and Self-Rated Health
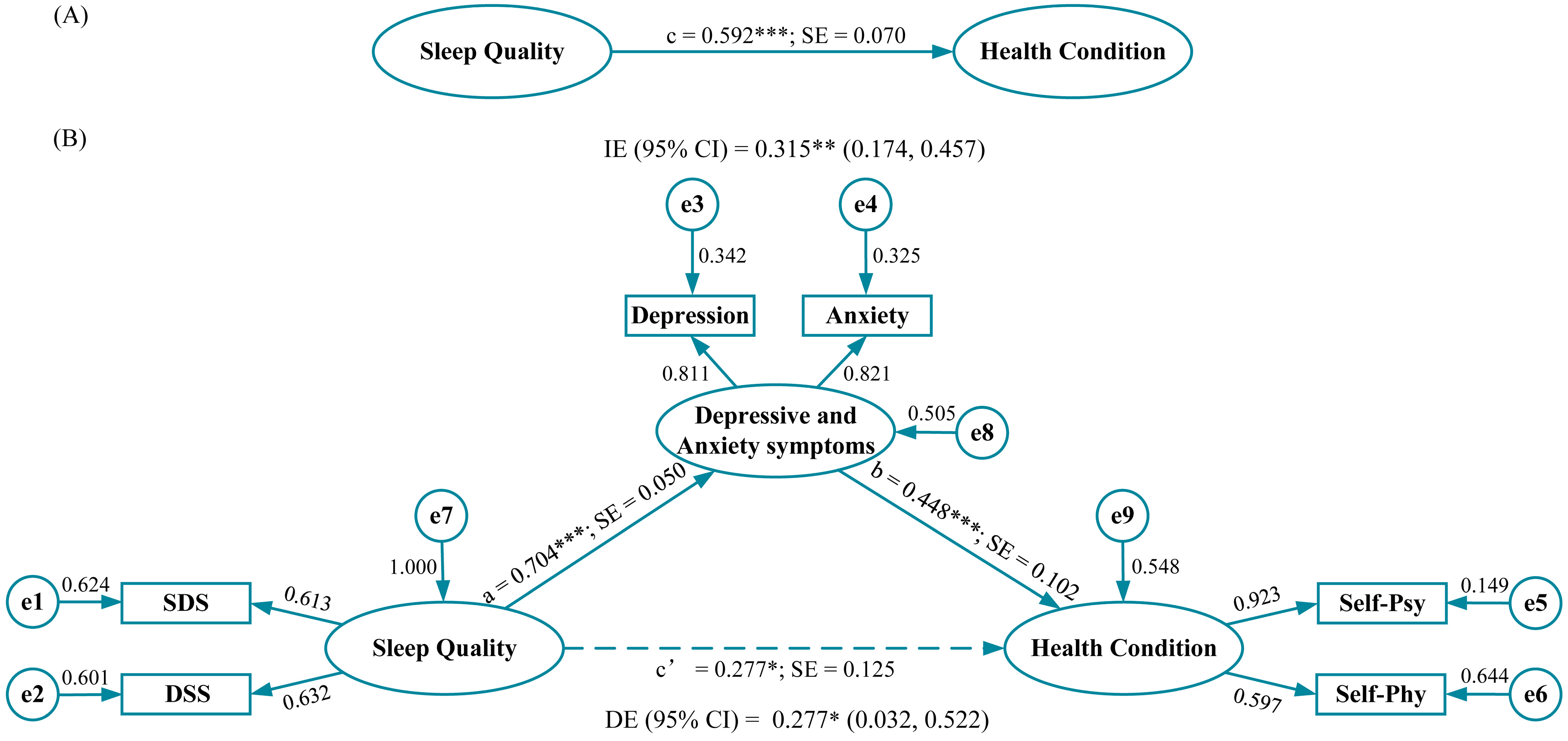
3.3. Structural Equation Model: Direct, Indirect, and Total Effects of Sleep Quality on Self-Rated Health through Mental Health Symptom
4. Discussion
4.1. Strengths and Limitations
4.2. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jahrami, H.A.; Alhaj, O.A.; Humood, A.M.; Alenezi, A.F.; Fekih-Romdhane, F.; AlRasheed, M.M.; Saif, Z.Q.; Bragazzi, N.L.; Pandi-Perumal, S.R.; BaHammam, A.S.; et al. Sleep disturbances during the COVID-19 pandemic: A systematic review, meta-analysis, and meta-regression. Sleep Med. Rev. 2022, 62, 101591. [Google Scholar] [CrossRef] [PubMed]
- Rao, W.-W.; Li, W.; Qi, H.; Hong, L.; Chen, C.; Li, C.-Y.; Ng, C.H.; Ungvari, G.S.; Xiang, Y.-T. Sleep quality in medical students: A comprehensive meta-analysis of observational studies. Sleep Breath. 2020, 24, 1151–1165. [Google Scholar] [CrossRef] [PubMed]
- Almojali, A.I.; Almalki, S.A.; Alothman, A.S.; Masuadi, E.M.; Alaqeel, M.K. The prevalence and association of stress with sleep quality among medical students. J. Epidemiol. Glob. Health 2017, 7, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Damiano, R.F.; de Oliveira, I.N.; da Ezequiel, O.S.; Lucchetti, A.L.; Lucchetti, G. The root of the problem: Identifying major sources of stress in Brazilian medical students and developing the Medical Student Stress Factor Scale. Braz. J. Psychiatry 2021, 43, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Mastrotheodoros, S.; Zhu, Y.; Yang, Y.; Hallit, S.; Zhao, B.; Fan, Y.; Huang, M.; Chen, C.; Ma, H.; et al. The Chinese Version of the Perceived Stress Questionnaire-13: Psychometric Properties and Measurement Invariance for Medical Students. Psychol. Res. Behav. Ma. 2023, 16, 71–83. [Google Scholar] [CrossRef]
- Yin, F.; Chen, C.; Song, S.; Chen, Z.; Jiao, Z.; Yan, Z.; Yin, G.; Feng, Z. Factors Affecting University Students’ Sleep Quality during the Normalisation of COVID-19 Epidemic Prevention and Control in China: A Cross-Sectional Study. Sustainability 2022, 14, 10646. [Google Scholar] [CrossRef]
- Viselli, L.; Salfi, F.; D’Atri, A.; Amicucci, G.; Ferrara, M. Sleep Quality, Insomnia Symptoms, and Depressive Symptomatology among Italian University Students before and during the COVID-19 Lockdown. Int. J. Env. Res. Public Health 2021, 18, 13346. [Google Scholar] [CrossRef]
- Kowalsky, R.J.; Farney, T.M.; Kline, C.E.; Hinojosa, J.N.; Creasy, S.A. The impact of the covid-19 pandemic on lifestyle behaviors in U.S. college students. J. Am. Coll. Health 2021, 1–6. [Google Scholar] [CrossRef]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int. J. Env. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Lin, C.-Y.; Broström, A.; Bülow, P.H.; Bajalan, Z.; Griffiths, M.D.; Ohayon, M.M.; Pakpour, A.H. Internet addiction and sleep problems: A systematic review and meta-analysis. Sleep Med. Rev. 2019, 47, 51–61. [Google Scholar] [CrossRef]
- Zhong, Y.; Ma, H.; Liang, Y.F.; Liao, C.J.; Zhang, C.C.; Jiang, W.J. Prevalence of smartphone addiction among Asian medical students: A meta-analysis of multinational observational studies. Int. J. Soc. Psychiatry 2022, 68, 1171–1183. [Google Scholar] [CrossRef]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef]
- Steptoe, A.; Peacey, V.; Wardle, J. Sleep Duration and Health in Young Adults. Arch. Int. Med. 2006, 166, 1689–1692. [Google Scholar] [CrossRef]
- Park, S.; Lee, Y.; Yoo, M.; Jung, S. Wellness and sleep quality in Korean nursing students: A cross-sectional study. Appl. Nurs. Res. 2019, 48, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.-B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2010, 33, 414–420. [Google Scholar] [CrossRef]
- Tasali, E.; Leproult, R.; Ehrmann, D.A.; Van Cauter, E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc. Natl. Acad. Sci. USA 2008, 105, 1044–1049. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Cooper, D.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef]
- Gottlieb, D.J.; Redline, S.; Nieto, F.J.; Baldwin, C.M.; Newman, A.B.; Resnick, H.E.; Punjabi, N.M. Association of Usual Sleep Duration With Hypertension: The Sleep Heart Health Study. Sleep 2006, 29, 1009–1014. [Google Scholar] [CrossRef]
- Wulff, K.; Gatti, S.; Wettstein, J.G.; Foster, R.G. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat. Rev. Neurosci. 2010, 11, 589–599. [Google Scholar] [CrossRef]
- Baglioni, C.; Nanovska, S.; Regen, W.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Reynolds Iii, C.F.; Riemann, D. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 2016, 142, 969–990. [Google Scholar] [CrossRef]
- Kahn-Greene, E.T.; Killgore, D.B.; Kamimori, G.H.; Balkin, T.J.; Killgore, W.D.S. The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Med. 2007, 8, 215–221. [Google Scholar] [CrossRef]
- Cohrs, S. Sleep Disturbances in Patients with Schizophrenia. CNS Drugs 2008, 22, 939–962. [Google Scholar] [CrossRef]
- Posmontier, B. Sleep quality in women with and without postpartum depression. J. Obst. Gyn. Neo. 2008, 37, 722–737. [Google Scholar] [CrossRef]
- Monti, J.M.; Monti, D. Sleep disturbance in generalized anxiety disorder and its treatment. Sleep Med. Rev. 2000, 4, 263–276. [Google Scholar] [CrossRef]
- Dahlin, M.; Joneborg, N.; Runeson, B. Stress and depression among medical students: A cross-sectional study. Med. Educ. 2005, 39, 594–604. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, H.; Jin, T.; Qiu, F.; Wang, X. Prevalence of Sleep Problems Among Chinese Medical Students: A Systematic Review and Meta-Analysis. Front. Psychiatry 2022, 13, 753419. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World. Health. Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Kato, T. Development of the Sleep Quality Questionnaire in healthy adults. J. Health Psychol. 2014, 19, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Fei, S.; Gong, B.; Sun, T.; Meng, R. Understanding the Mediating Role of Anxiety and Depression on the Relationship Between Perceived Stress and Sleep Quality Among Health Care Workers in the COVID-19 Response. Nat. Sci. Sleep 2021, 13, 1747–1758. [Google Scholar] [CrossRef]
- Meng, R.; Kato, T.; Mastrotheodoros, S.; Dong, L.; Fong, D.Y.T.; Wang, F.; Cao, M.; Liu, X.; Yao, C.; Cao, J.; et al. Adaptation and validation of the Chinese version of the Sleep Quality Questionnaire. Qual. Life Res. 2022. [Google Scholar] [CrossRef] [PubMed]
- Meng, R. Development and Evaluation of the Chinese Version of the Sleep Quality Questionnaire. Ph.D. Dissertation, Wuhan University, Wuhan, China, 2020. (In Chinese). [Google Scholar]
- Meng, R.; Lau, E.Y.Y.; Spruyt, K.; Miller, C.B.; Dong, L. Assessing Measurement Properties of a Simplified Chinese Version of Sleep Condition Indicator (SCI-SC) in Community Residents. Behav. Sci. 2022, 12, 433. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W. Validation and Utility of a Self-report Version of PRIME-MDThe PHQ Primary Care Study. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Löwe, B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. Psychosomatics 2009, 50, 613–621. [Google Scholar]
- Buhi, E.R.; Goodson, P.; Neilands, T.B. Out of sight, not out of mind: Strategies for handling missing data. Am. J. Health Behav. 2008, 32, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Joseph, F.; Hair, W.C.B.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis: Pearson New International Edition, 7th ed.; Pearson: London, UK, 2009. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Mulaik, S.A.; James, L.R.; Van Alstine, J.; Bennett, N.; Lind, S.; Stilwell, C.D. Evaluation of goodness-of-fit indices for structural equation models. Psychol. Bull. 1989, 105, 430–445. [Google Scholar] [CrossRef]
- Lukowski, A.F.; Karayianis, K.A.; Kamliot, D.Z.; Tsukerman, D. Undergraduate Student Stress, Sleep, and Health before and during the COVID-19 Pandemic. Behav. Med. 2022; ahead of print. [Google Scholar] [CrossRef]
- Liu, B.; Gao, F.; Zhang, J.; Zhou, H.; Sun, N.; Li, L.; Liang, L.; Ning, N.; Wu, Q.; Zhao, M. Sleep Quality of Students from Elementary School to University: A Cross-Sectional Study. Nat. Sci. Sleep 2020, 12, 855–864. [Google Scholar] [CrossRef]
- Mai, Q.D.; Jacobs, A.W.; Schieman, S. Precarious sleep? Nonstandard work, gender, and sleep disturbance in 31 European countries. Soc. Sci. Med. 2019, 237, 112424. [Google Scholar] [CrossRef]
- Grandner, M.A.; Patel, N.P.; Gehrman, P.R.; Xie, D.; Sha, D.; Weaver, T.; Gooneratne, N. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010, 11, 470–478. [Google Scholar] [CrossRef]
- Virtanen, P.; Vahtera, J.; Broms, U.; Sillanmäki, L.; Kivimäki, M.; Koskenvuo, M. Employment trajectory as determinant of change in health-related lifestyle: The prospective HeSSup study. Eur. J. Public Health 2008, 18, 504–508. [Google Scholar] [CrossRef]
- Kretschmer, V.; Riedel, N. Effects of atypical employment on difficulties in falling asleep and maintaining sleep—Gender differences in the lidA study. Gesundheitswesen 2015, 77, e77–e84. [Google Scholar] [PubMed]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and exercise: A reciprocal issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Johnson, E.O.; Roth, T.; Breslau, N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J. Psychiatr. Res. 2006, 40, 700–708. [Google Scholar] [CrossRef] [PubMed]
- Eaton, W.W.; Badawi, M.; Melton, B. Prodromes and precursors: Epidemiologic data for primary prevention of disorders with slow onset. Am. J. Psychiatry 1995, 152, 967–972. [Google Scholar]
- Alvaro, P.K.; Roberts, R.M.; Harris, J.K. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep 2013, 36, 1059–1068. [Google Scholar] [CrossRef]
- Hull, T.H. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications [Book Review]. J. Popul. Res. 2007, 24, 133. [Google Scholar] [CrossRef]
- Latas, M.; Stojković, T.; Ralić, T.; Jovanović, S.; Spirić, Z.; Milovanović, S. Medical students’ health-related quality of life—A comparative study. Vojnosanit. Pregl. 2014, 71, 751–756. [Google Scholar] [CrossRef]
- Maharlouei, N.; Akbari, M.; Khabbaz Shirazy, M.; Yazdanpanah, D.; Lankarani, K.B. Factors associated with self-rated health status in Southwestern Iran: A population-based study. Public Health 2016, 140, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Maguire, P.A.; Reay, R.E.; Raphael, B. Correlates of a single-item Self-Rated Mental Health Question in people with schizophrenia. Australas Psychiatry 2016, 24, 473–477. [Google Scholar] [CrossRef]
- Sun, W.; Watanabe, M.; Tanimoto, Y.; Shibutani, T.; Kono, R.; Saito, M.; Usuda, K.; Kono, K. Factors associated with good self-rated health of non-disabled elderly living alone in Japan: A cross-sectional study. BMC Public Health 2007, 7, 297. [Google Scholar] [CrossRef]
- Demirchyan, A.; Thompson, M.E. Determinants of self-rated health in women: A population-based study in Armavir Marz, Armenia, 2001 & 2004. Int. J. Equity Health 2008, 7, 25. [Google Scholar] [PubMed]
- Xu, Z.; Su, H.; Zou, Y.; Chen, J.; Wu, J.; Chang, W. Self-rated health of Chinese adolescents: Distribution and its associated factors. Scand J. Caring. Sci. 2011, 25, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Haddock, C.K.; Poston, W.S.C.; Pyle, S.A.; Klesges, R.C.; Vander Weg, M.W.; Peterson, A.; Debon, M. The validity of self-rated health as a measure of health status among young military personnel: Evidence from a cross-sectional survey. Health Qual. Life Out. 2006, 4, 57. [Google Scholar] [CrossRef]
- Haseli-Mashhadi, N.; Pan, A.; Ye, X.; Wang, J.; Qi, Q.; Liu, Y.; Li, H.; Yu, Z.; Lin, X.; Franco, O.H. Self-Rated Health in middle-aged and elderly Chinese: Distribution, determinants and associations with cardio-metabolic risk factors. BMC Public Health 2009, 9, 368. [Google Scholar] [CrossRef]
- Yeo, S.C.; Jos, A.M.; Erwin, C.; Lee, S.M.; Lee, X.K.; Lo, J.C.; Chee, M.W.L.; Gooley, J.J. Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: Problems and possible solutions. Sleep Med. 2019, 60, 96–108. [Google Scholar] [CrossRef]
- Zhao, X.; Lynch, J.G., Jr.; Chen, Q. Reconsidering Baron and Kenny: Myths and Truths about Mediation Analysis. J. Consum. Res. 2010, 37, 197–206. [Google Scholar] [CrossRef]

| Variable | n (%) | SQQ Total | Statistics | |||
|---|---|---|---|---|---|---|
| Mean | SD | df | t/F | p | ||
| Gender | 1 | 2.382 | 0.123 | |||
| Male | 156 (24.490) | 17.462 | 6.539 | |||
| Female | 481 (75.510) | 18.345 | 6.104 | |||
| Age | 1 | 7.326 | 0.007 | |||
| <20 | 458 (71.900) | 18.544 | 6.187 | |||
| ≥20 | 179 (28.100) | 17.067 | 6.194 | |||
| Home location | 2 | 2.528 | 0.081 | |||
| Urban | 246 (38.619) | 17.622 | 6.064 | |||
| Rural | 236 (37.049) | 18.055 | 6.300 | |||
| Suburban | 155 (24.333) | 19.045 | 6.280 | |||
| Only child | 1 | 2.396 | 0.122 | |||
| Yes | 257 (40.345) | 17.665 | 6.273 | |||
| No | 380 (59.655) | 18.442 | 6.172 | |||
| Academic year | 2 | 3.386 | 0.034 | |||
| First year | 274 (43.014) | 17.810 | 6.464 | |||
| Second year | 161 (25.275) | 19.224 | 5.967 | |||
| Third year | 202 (31.711) | 17.688 | 6.002 | |||
| Family income | 1 | 0.040 | 0.842 | |||
| <CNY 10,000 | 261 (40.973) | 18.188 | 6.205 | |||
| ≥CNY 10,000 | 376 (59.027) | 18.088 | 6.238 | |||
| Part-time employment | 1 | 5.276 | 0.022 | |||
| Yes | 110 (17.268) | 19.364 | 5.967 | |||
| No | 527 (82.732) | 17.871 | 6.246 | |||
| Leisure time sports involvement | 1 | 7.068 | 0.008 | |||
| Yes | 316 (49.608) | 17.472 | 6.314 | |||
| No | 321 (50.392) | 18.776 | 6.067 | |||
| Perceived employment prospects | 4 | 3.431 | 0.009 | |||
| Excellent | 56 (8.791) | 17.982 | 7.129 | |||
| Good | 347 (54.474) | 17.715 | 5.996 | |||
| Average | 189 (29.670) | 18.228 | 6.340 | |||
| Poor | 39 (6.122) | 21.564 | 5.389 | |||
| Extremely poor | 6 (0.942) | 18.000 | 6.099 | |||
| Engagement in hobbies | 1 | 6.133 | 0.014 | |||
| Yes | 451 (70.801) | 17.738 | 6.338 | |||
| No | 186 (29.199) | 19.075 | 5.831 | |||
| Preferred coping strategies | 2 | 22.558 | <0.001 | |||
| Active copy | 375 (58.870) | 18.664 | 5.793 | |||
| Push through | 211 (33.124) | 16.237 | 6.240 | |||
| Ignore problems | 51 (8.006) | 22.020 | 6.701 | |||
| Academic major | 6 | 1.483 | 0.181 | |||
| Clinical medicine | 127 (18.937) | 18.378 | 6.279 | |||
| Preventive medicine | 98 (15.385) | 18.612 | 5.452 | |||
| Nursing | 93 (14.600) | 18.774 | 6.216 | |||
| Pharmacy | 95 (14.914) | 18.789 | 5.909 | |||
| Health policy and management | 87 (13.658) | 17.471 | 6.077 | |||
| Health services and management | 76 (11.931) | 17.566 | 6.616 | |||
| Master of Medicine | 61 (9.576) | 16.459 | 7.208 | |||
| GOF Index | Mediation Model | Threshold |
|---|---|---|
| Absolute measures | ||
| RMSEA (90% CI) | 0.069 (0.042, 0.099) | <0.080 |
| SRMR | 0.027 | <0.080 |
| GFI | 0.987 | >0.900 |
| χ2/df | 4.075 | 2.000–3.000 |
| Incremental fit measures | ||
| TLI | 0.959 | >0.900 |
| CFI | 0.984 | >0.900 |
| Parsimony measures | ||
| AGFI | 0.955 | >0.900 |
| PNFI | 0.391 | >0.500 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Y.; Jiang, C.; Yang, Y.; Dzierzewski, J.M.; Spruyt, K.; Zhang, B.; Huang, M.; Ge, H.; Rong, Y.; Ola, B.A.; et al. Depression and Anxiety Mediate the Association between Sleep Quality and Self-Rated Health in Healthcare Students. Behav. Sci. 2023, 13, 82. https://doi.org/10.3390/bs13020082
Zhu Y, Jiang C, Yang Y, Dzierzewski JM, Spruyt K, Zhang B, Huang M, Ge H, Rong Y, Ola BA, et al. Depression and Anxiety Mediate the Association between Sleep Quality and Self-Rated Health in Healthcare Students. Behavioral Sciences. 2023; 13(2):82. https://doi.org/10.3390/bs13020082
Chicago/Turabian StyleZhu, Yihong, Chen Jiang, You Yang, Joseph M. Dzierzewski, Karen Spruyt, Bingren Zhang, Mengyi Huang, Hanjie Ge, Yangyang Rong, Bolanle Adeyemi Ola, and et al. 2023. "Depression and Anxiety Mediate the Association between Sleep Quality and Self-Rated Health in Healthcare Students" Behavioral Sciences 13, no. 2: 82. https://doi.org/10.3390/bs13020082
APA StyleZhu, Y., Jiang, C., Yang, Y., Dzierzewski, J. M., Spruyt, K., Zhang, B., Huang, M., Ge, H., Rong, Y., Ola, B. A., Liu, T., Ma, H., & Meng, R. (2023). Depression and Anxiety Mediate the Association between Sleep Quality and Self-Rated Health in Healthcare Students. Behavioral Sciences, 13(2), 82. https://doi.org/10.3390/bs13020082









