Mental Health of Mothers of Children with Neurodevelopmental and Genetic Disorders in Pakistan
Abstract
:1. Introduction
1.1. Maternal Education
1.2. Stigma and Affiliate Stigma Related to Child Disability in Developing Countries
1.3. Aim of the Present Study
2. Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Demographic Questionnaire
2.3.2. Depression and Anxiety Scales
2.3.3. Affiliate Stigma Scale
3. Analytic Plan
4. Results
4.1. Anxiety and Maternal Education
4.2. Depression and Maternal Education
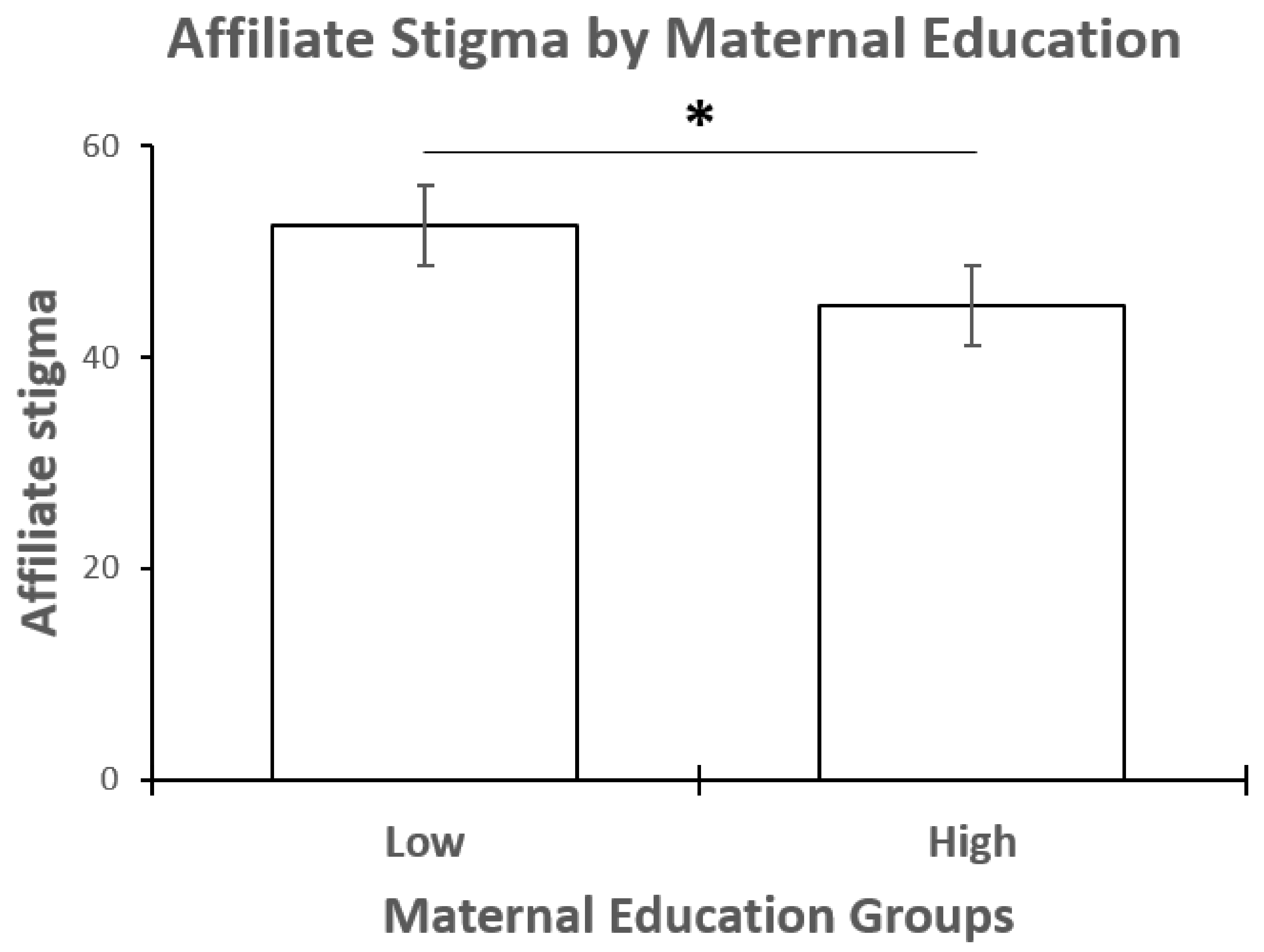
4.3. Affiliate Stigma and Maternal Education
4.4. Affiliate Stigma and Maternal Education Excluding the Effect of Anxiety
4.5. Affiliate Stigma and Maternal Education Excluding the Effect of Depression
5. Discussion
5.1. Limitations
5.2. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Summary: World Report on Disability 2011; Technical Report; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- The World Bank. Pakistan Overview. 2018. Available online: http://www.worldbank.org/en/country/pakistan/overview (accessed on 11 April 2022).
- Maselko, J.; Sikander, S.; Bangash, O.; Bhalotra, S.; Franz, L.; Ganga, N.; Rajan, D.G.; O’Donnell, K.; Rahman, A. Child mental health and maternal depression history in Pakistan. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Bano, H.; Anjum, N. Therapeutic, Educational and Employment Services for Children with Intellectual Disability in Pakistan. New Horiz. 2013, 7, 51. [Google Scholar]
- Husain, N.; Parveen, A.; Husain, M.; Saeed, Q.; Jafri, F.; Rahman, R.; Tomenson, B.; Chaudhry, I.B. Prevalence and psychosocial correlates of perinatal depression: A cohort study from urban Pakistan. Arch. Women’s Ment. Health 2011, 14, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.; Mello, M.C.d.; Patel, V.; Rahman, A.; Tran, T.; Holton, S.; Holmes, W. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: A systematic review. Bull. World Health Organ. 2012, 90, 139–149. [Google Scholar] [CrossRef]
- Ali, N.S.; Azam, I.S.; Ali, B.S.; Tabbusum, G.; Moin, S.S. Frequency and associated factors for anxiety and depression in pregnant women: A hospital-based cross-sectional study. Sci. World J. 2012, 2012, 653098. [Google Scholar] [CrossRef] [Green Version]
- Valicenti-McDermott, M.; Lawson, K.; Hottinger, K.; Seijo, R.; Schechtman, M.; Shulman, L.; Shinnar, S. Parental stress in families of children with autism and other developmental disabilities. J. Child Neurol. 2015, 30, 1728–1735. [Google Scholar] [CrossRef]
- Carollo, A.; Bonassi, A.; Lim, M.; Gabrieli, G.; Setoh, P.; Dimitriou, D.; Aryadoust, V.; Esposito, G. Developmental disabilities across the world: A scientometric review from 1936 to 2020. Res. Dev. Disabil. 2021, 117, 104031. [Google Scholar] [CrossRef]
- Esposito, G.; Setoh, P. Parental involvement in developmental disabilities across cultures. Res. Dev. Disabil. 2021, 116, 104023. [Google Scholar] [CrossRef]
- Abbas, Q.; Feroz, R.; Alyana, S. Determinants of Psychological Wellbeing in Mothers of Children with Intellectual Disability. Pak. J. Clin. Psychol. 2016, 15, 1. [Google Scholar]
- Azeem, M.W.; Dogar, I.A.; Shah, S.; Cheema, M.A.; Asmat, A.; Akbar, M.; Kousar, S.; Haider, I.I. Anxiety and depression among parents of children with intellectual disability in Pakistan. J. Can. Acad. Child Adolesc. Psychiatry 2013, 22, 290. [Google Scholar]
- Bizzego, A.; Gabrieli, G.; Bornstein, M.H.; Deater-Deckard, K.; Lansford, J.E.; Bradley, R.H.; Costa, M.; Esposito, G. Predictors of contemporary under-5 child mortality in low-and middle-income countries: A machine learning approach. Int. J. Environ. Res. Public Health 2021, 18, 1315. [Google Scholar] [CrossRef] [PubMed]
- Bizzego, A.; Lim, M.; Schiavon, G.; Setoh, P.; Gabrieli, G.; Dimitriou, D.; Esposito, G. Child disability and caregiving in low and middle income countries: Big data approach on open data. Res. Dev. Disabil. 2020, 107, 103795. [Google Scholar] [CrossRef] [PubMed]
- Bizzego, A.; Lim, M.; Schiavon, G.; Esposito, G. Children with developmental disabilities in low-and middle-income countries: More neglected and physically punished. Int. J. Environ. Res. Public Health 2020, 17, 7009. [Google Scholar] [CrossRef] [PubMed]
- Lakshman, R.; Zhang, J.; Zhang, J.; Koch, F.S.; Marcus, C.; Ludvigsson, J.; Ong, K.K.; Sobko, T. Higher maternal education is associated with favourable growth of young children in different countries. J. Epidemiol. Community Health 2013, 67, 595–602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aslam, M.; Kingdon, G.G. Parental education and child health—Understanding the pathways of impact in Pakistan. World Dev. 2012, 40, 2014–2032. [Google Scholar] [CrossRef] [Green Version]
- Patka, M.; Keys, C.B.; Henry, D.B.; McDonald, K.E. Attitudes of Pakistani community members and staff toward people with intellectual disability. Am. J. Intellect. Dev. Disabil. 2013, 118, 32–43. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, S.; Bryant, L.D.; Ahmed, M.; Jafri, H.; Raashid, Y. Experiences of parents with a child with Down syndrome in Pakistan and their views on termination of pregnancy. J. Community Genet. 2013, 4, 107–114. [Google Scholar] [CrossRef] [Green Version]
- Banga, G.; Ghosh, S. The impact of affiliate stigma on the psychological well-being of mothers of children with specific learning disabilities in India: The mediating role of subjective burden. J. Appl. Res. Intellect. Disabil. 2017, 30, 958–969. [Google Scholar] [CrossRef]
- Cuthill, F.M.; Espie, C.A.; Cooper, S.A. Development and psychometric properties of the Glasgow Depression Scale for people with a learning disability: Individual and carer supplement versions. Br. J. Psychiatry 2003, 182, 347–353. [Google Scholar] [CrossRef] [Green Version]
- Mindham, J.; Espie, C. Glasgow Anxiety Scale for people with an Intellectual Disability (GAS-ID): Development and psychometric properties of a new measure for use with people with mild intellectual disability. J. Intellect. Disabil. Res. 2003, 47, 22–30. [Google Scholar] [CrossRef]
- Mak, W.W.; Cheung, R.Y. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J. Appl. Res. Intellect. Disabil. 2008, 21, 532–545. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; HarperCollins College Publishers: Boston, MA, USA, 2007; Volume 5. [Google Scholar]
- Araya, R.; Lewis, G.; Rojas, G.; Fritsch, R. Education and income: Which is more important for mental health? J. Epidemiol. Community Health 2003, 57, 501–505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bornstein, M.H.; Cote, L.R.; Haynes, O.M.; Hahn, C.S.; Park, Y. Parenting knowledge: Experiential and sociodemographic factors in European American mothers of young children. Dev. Psychol. 2010, 46, 1677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bornstein, M.H.; Rothenberg, W.A.; Lansford, J.E.; Bradley, R.H.; Deater-Deckard, K.; Bizzego, A.; Esposito, G. Child Development in Low-and Middle-Income Countries. Pediatrics 2021, 148, e2021053180. [Google Scholar] [CrossRef]
- Jeong, J.; McCoy, D.C.; Fink, G. Pathways between paternal and maternal education, caregivers’ support for learning, and early child development in 44 low-and middle-income countries. Early Child. Res. Q. 2017, 41, 136–148. [Google Scholar] [CrossRef]
- Palermo, F.; Carlo, G.; Ispa, J.M.; Squires, C. Latina mothers’ mental health and children’s academic readiness: Moderation by maternal education. J. Appl. Dev. Psychol. 2019, 62, 260–269. [Google Scholar] [CrossRef]
- Güneş, P.M. The role of maternal education in child health: Evidence from a compulsory schooling law. Econ. Educ. Rev. 2015, 47, 1–16. [Google Scholar] [CrossRef] [Green Version]
- McConkey, R.; Truesdale-Kennedy, M.; Chang, M.Y.; Jarrah, S.; Shukri, R. The impact on mothers of bringing up a child with intellectual disabilities: A cross-cultural study. Int. J. Nurs. Stud. 2008, 45, 65–74. [Google Scholar] [CrossRef]
- Yamaoka, Y.; Tamiya, N.; Izumida, N.; Kawamura, A.; Takahashi, H.; Noguchi, H. The relationship between raising a child with a disability and the mental health of mothers compared to raising a child without disability in Japan. SSM-Popul. Health 2016, 2, 542–548. [Google Scholar] [CrossRef] [Green Version]
- Leiter, V.; Krauss, M.W.; Anderson, B.; Wells, N. The consequences of caring: Effects of mothering a child with special needs. J. Fam. Issues 2004, 25, 379–403. [Google Scholar] [CrossRef]
- Thuy, N.T.M.; Berry, H.L. Social capital and mental health among mothers in Vietnam who have children with disabilities. Glob. Health Action 2013, 6, 18886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McHatton, P.A.; Correa, V. Stigma and discrimination: Perspectives from Mexican and Puerto Rican mothers of children with special needs. Top. Early Child. Spec. Educ. 2005, 25, 131–142. [Google Scholar] [CrossRef]
- Zafar, S. Integration of a Maternal Psychosocial Well-Being Component into a Early Child-Development Intervention. Ph.D. Thesis, University of Liverpool, Liverpool, UK, 2014. [Google Scholar]
- Jayawickreme, N.; Jayawickreme, E.; Atanasov, P.; Goonasekera, M.A.; Foa, E.B. Are culturally specific measures of trauma-related anxiety and depression needed? The case of Sri Lanka. Psychol. Assess. 2012, 24, 791. [Google Scholar] [CrossRef] [PubMed]
| Mean | SD | |
|---|---|---|
| Age | 37.1 | 6.2 |
| Depression score | 13.88 | 6.59 |
| Anxiety score | 20.04 | 7.66 |
| Affiliate stigma score | 47.98 | 9.82 |
| Not Clinically Anxious | Clinically Anxious | Total | |
|---|---|---|---|
| Not clinically depressed | 13 | 17 | 30 (40.5%) |
| Clinically depressed | 6 | 38 | 44 (59.5%) |
| Total | 19 (25.7%) | 55 (74.3%) | 74 |
| Not Clinically Anxious | Clinically Anxious | Total | |
|---|---|---|---|
| Middle/high school education | 4 | 28 | 32 (44.4%) |
| Tertiary education | 15 | 25 | 40 (55.6%) |
| Total | 19 (26.4%) | 53 (73.6%) | 72 |
| Not Clinically Depressed | Clinically Deppressed | Total | |
|---|---|---|---|
| Middle/high school education | 12 | 20 | 32 (44.4%) |
| Tertiary education | 18 | 25 | 40 (55.6%) |
| Total | 30 (41.7%) | 42 (58.3%) | 72 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neoh, M.J.Y.; Airoldi, L.; Arshad, Z.; Bin Eid, W.; Esposito, G.; Dimitriou, D. Mental Health of Mothers of Children with Neurodevelopmental and Genetic Disorders in Pakistan. Behav. Sci. 2022, 12, 161. https://doi.org/10.3390/bs12060161
Neoh MJY, Airoldi L, Arshad Z, Bin Eid W, Esposito G, Dimitriou D. Mental Health of Mothers of Children with Neurodevelopmental and Genetic Disorders in Pakistan. Behavioral Sciences. 2022; 12(6):161. https://doi.org/10.3390/bs12060161
Chicago/Turabian StyleNeoh, Michelle Jin Yee, Livia Airoldi, Zarah Arshad, Wasmiah Bin Eid, Gianluca Esposito, and Dagmara Dimitriou. 2022. "Mental Health of Mothers of Children with Neurodevelopmental and Genetic Disorders in Pakistan" Behavioral Sciences 12, no. 6: 161. https://doi.org/10.3390/bs12060161
APA StyleNeoh, M. J. Y., Airoldi, L., Arshad, Z., Bin Eid, W., Esposito, G., & Dimitriou, D. (2022). Mental Health of Mothers of Children with Neurodevelopmental and Genetic Disorders in Pakistan. Behavioral Sciences, 12(6), 161. https://doi.org/10.3390/bs12060161





