Public Service Motivation and Determining Factors to Attract and Retain Health Professionals in the Public Sector: A Systematic Review
Abstract
:1. Introduction
- (i)
- To characterize the research about health professionals’ motivational determinants, including the methodological quality, geographical distribution, choice of journals, cross-country and author collaboration, and co-citation trends;
- (ii)
- To identify the motivational factors influencing the sector’s choice by health professionals in different territories;
- (iii)
- To identify the dissemination and use of the main instruments to measure PSM; and
- (iv)
- To identify the main motivational theories supporting the studies.
2. Materials and Methods
2.1. Research Questions
- -
- What characterizes the research on health professionals’ motivation regarding geographical and authorship distribution, collaborations, and co-citations?
- -
- What are the factors motivating health professionals to choose the public sector for their activity?
- -
- What are the methods and instruments employed to assess health professionals’ motivation?
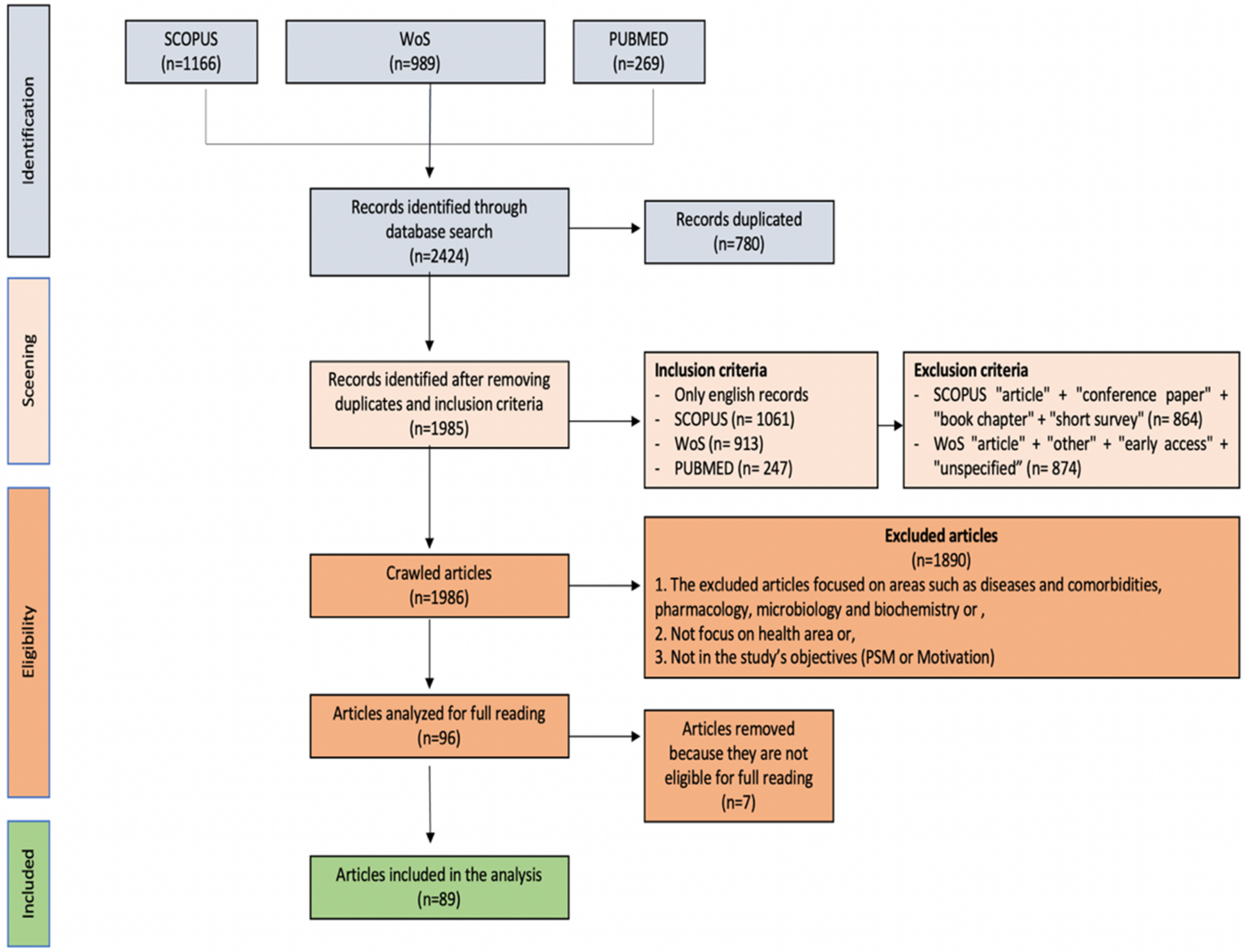
2.2. Search Strategy, Inclusion and Exclusion Criteria
2.3. Methodological Quality Assessment
3. Results
3.1. Authors
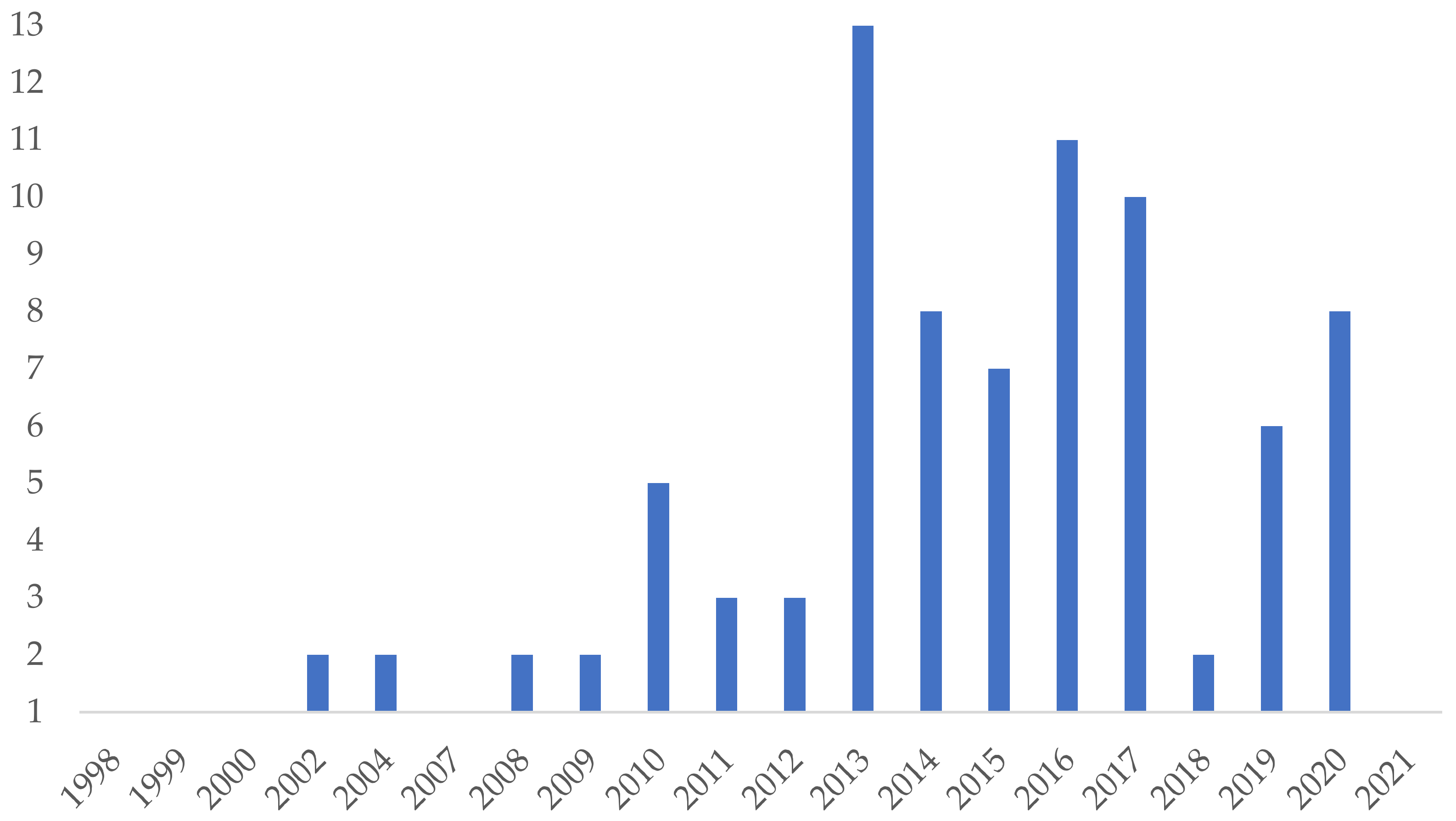
3.2. Publications
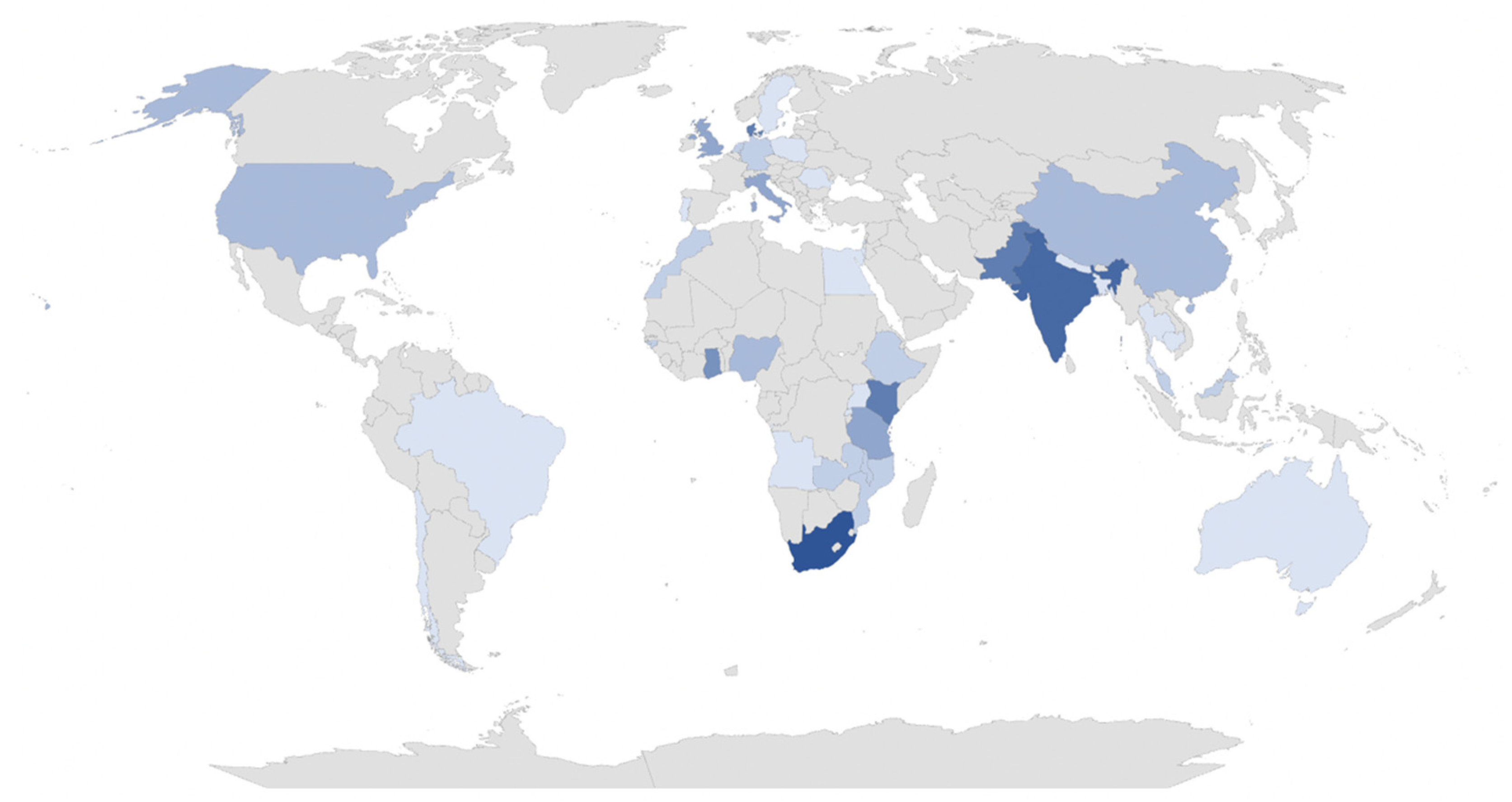
3.3. Countries
3.4. Analysis of Scientific Collaboration
3.4.1. Cross-Country Collaboration
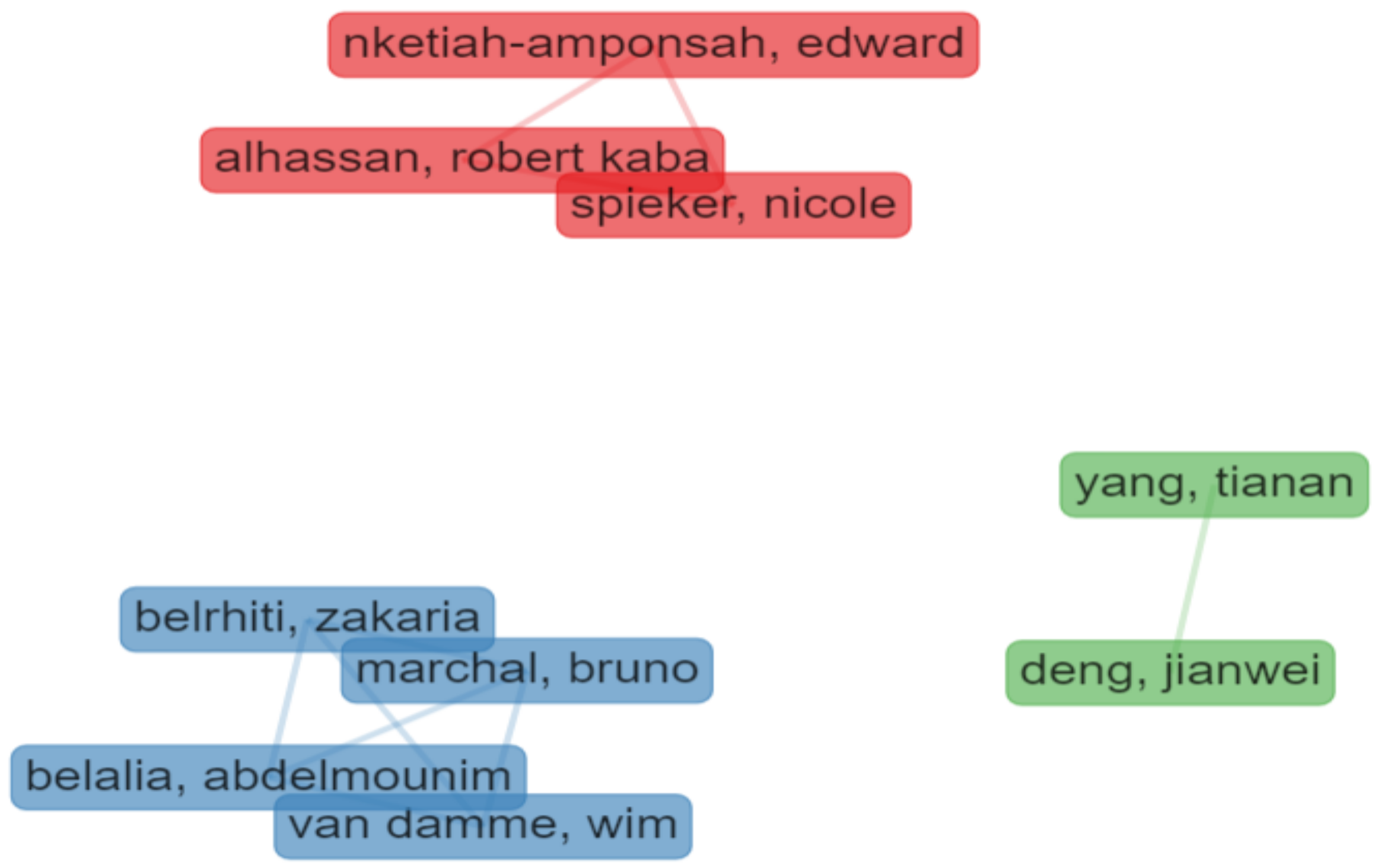
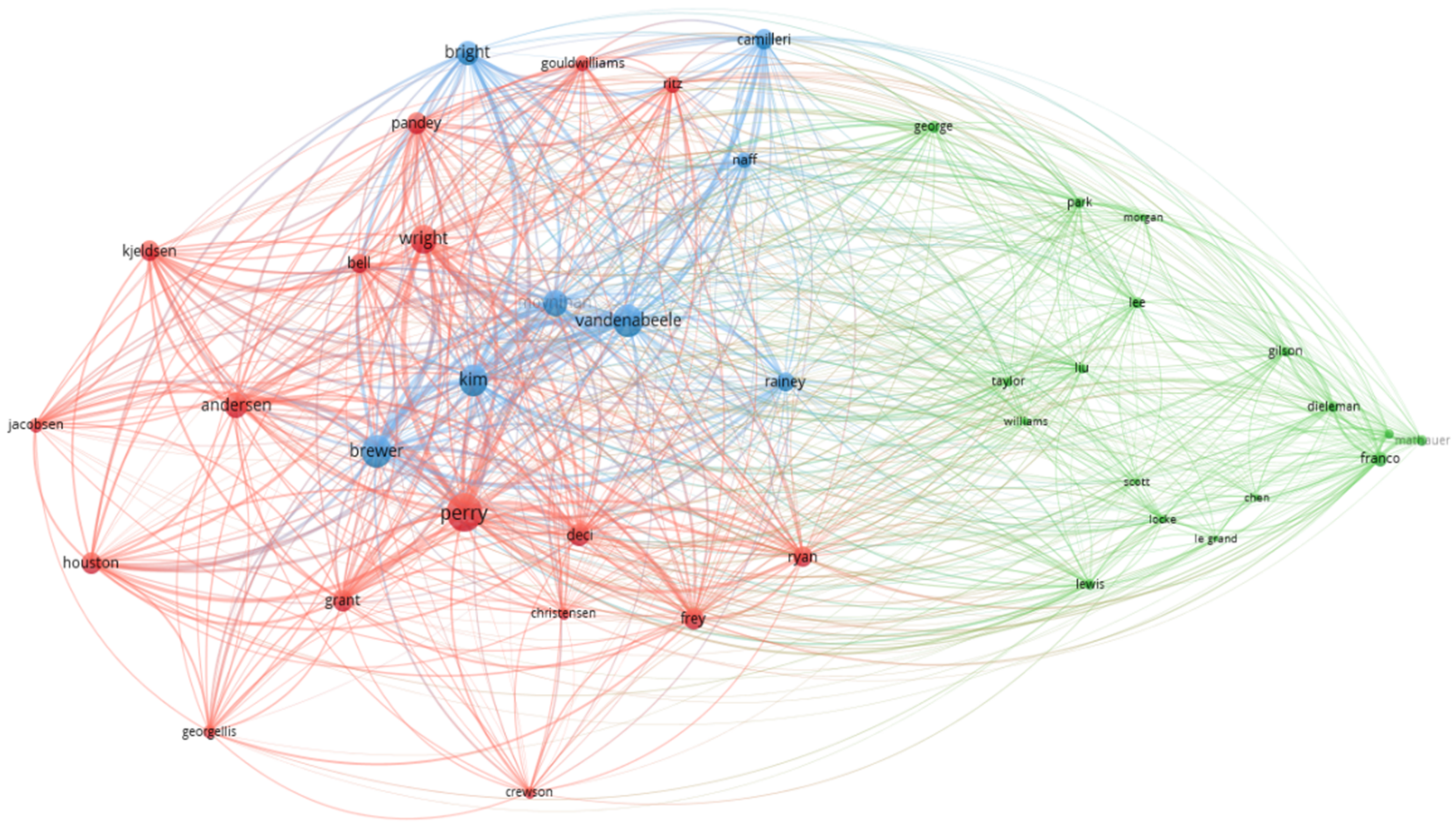
3.4.2. Collaboration among Authors
- Cluster 1 (in blue) includes four authors from Morocco and Belgium and focuses on motivation and public sector choice;
- Cluster 2 (in red) includes three authors from The Netherlands and Ghana and mostly pays attention to the quality of health services and human resources; and
- Cluster 3 (in green) is based on two Chinese authors from the Institute of Technology in Beijing, focused on health policies management.
3.4.3. Co-Citation Analysis
3.5. Methodological Quality Assessment
3.6. Object of Analysis
3.7. Main Motivation Theories
3.8. Methods
3.9. Instruments Used to Measure Motivation and Related Constructs
3.10. Main Extrinsic and Intrinsic Factors
4. Discussion of Intrinsic and Extrinsic Factors
4.1. Work Environment
4.2. Career Progression
4.3. Work Conditions
4.4. Remuneration
4.5. Recognition, Self-Realization, and Responsibility
4.6. Life-Long Learning and Professional Development
5. Summary of Main Findings
6. Final Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Authors | Year | Remuneration | Work Environment/ Work Conditions | Life-Long Learning/ Professional Development | High Workload | Absenteeism | Altruism | Job Security | Recognition of Work | Responsibility/ Autonomy |
| Jiang et al. [97] | 2021 | x | ||||||||
| Stefurak et al. [98] | 2020 | x | ||||||||
| Cantarelli et al. [85] | 2020 | x | x | x | x | |||||
| Ebenso et al. [99] | 2020 | x | x | |||||||
| Jensen et al. [100] | 2020 | x | x | x | x | x | ||||
| Belrhiti et al. [86] | 2020 | x | x | |||||||
| Androniceanu et al. [73] | 2020 | x | x | x | ||||||
| Abdelmotaleb et al. [101] | 2020 | x | x | |||||||
| van Loon et al. [102] | 2020 | x | x | |||||||
| Belrhiti et al. [86] | 2019 | x | x | x | x | |||||
| Deng et al. [103] | 2019 | x | ||||||||
| Deng et al. [104] | 2019 | x | x | |||||||
| Adams et al. [105] | 2019 | x | x | |||||||
| Prust et al. [75] | 2019 | x | x | x | ||||||
| Chang et al. [63] | 2019 | x | x | x | ||||||
| Borghi, et al. [106] | 2018 | x | x | |||||||
| Zweigenthal et al. [107] | 2018 | x | x | |||||||
| Aguilera et al. [108] | 2017 | x | ||||||||
| Abera et al. [109] | 2017 | x | x | x | ||||||
| Masood et al. [110] | 2017 | x | ||||||||
| Levitats et al. [111] | 2017 | x | ||||||||
| Millar et al. [112] | 2017 | x | x | x | x | |||||
| Sato et al. [75] | 2017 | x | x | x | ||||||
| Korlén et al. [76] | 2017 | x | x | x | ||||||
| Bhatnagar et al. [42] | 2017 | x | x | x | ||||||
| Seth [113] | 2017 | x | x | |||||||
| Mazahir et al. [77] | 2017 | x | x | |||||||
| Hou et al. [114] | 2016 | x | x | x | ||||||
| Russo et al. [82] | 2016 | x | ||||||||
| Bhatnagar and George [115] | 2016 | x | x | x | ||||||
| Shah et al. [116] | 2016 | x | x | x | x | x | ||||
| Alhassan et al. [64] | 2016 | x | x | x | x | |||||
| Namakula et al. [117] | 2016 | x | x | |||||||
| Bansal and Malhotra [71] | 2016 | x | x | x | ||||||
| Van Loon [118] | 2016 | x | x | x | ||||||
| Kadam et al. [119] | 2016 | x | x | |||||||
| Aninanya et al. [87] | 2016 | x | x | x | ||||||
| Khim [55] | 2016 | x | x | x | x | |||||
| Mir et al. [61] | 2015 | x | x | |||||||
| Hotchkiss et al. [53] | 2015 | x | x | x | x | |||||
| Gasiorowski et al. [56] | 2015 | x | x | x | x | |||||
| Ashmore and Gilson [120] | 2015 | x | ||||||||
| Shibata et al. [92] | 2015 | x | x | |||||||
| Bellé [121] | 2015 | x | ||||||||
| Schmiedeknecht et al. [122] | 2015 | x | x | x | x | x | ||||
| Russo et al. [123] | 2014 | x | x | x | ||||||
| Bonenberger et al. [65] | 2014 | x | x | x | ||||||
| Ojakaa et al. [57] | 2014 | x | x | x | x | |||||
| Hennig-Schmidt and Wiesen [124] | 2014 | x | x | |||||||
| Purohit et al. [66] | 2014 | x | x | x | x | x | x | |||
| Lagarde and Blaauw [125] | 2014 | x | ||||||||
| Krogsgaard et al. [126] | 2014 | x | ||||||||
| Schott and Pronk [127] | 2014 | x | x | x | ||||||
| Diwan et al. [128] | 2013 | x | x | x | ||||||
| Alhassan et al. [129] | 2013 | x | x | x | ||||||
| Kolstad et al. [130] | 2013 | x | ||||||||
| Ghimire et al. [57] | 2013 | x | x | x | x | x | ||||
| George et al. [131] | 2013 | x | x | x | ||||||
| Mutale et al. [93] | 2013 | x | x | x | x | |||||
| Dos Santos et al. [132] | 2013 | x | ||||||||
| Bellé [133] | 2013 | x | ||||||||
| van Loon et al. [134] | 2013 | x | ||||||||
| Chew et al. [67] | 2013 | x | x | |||||||
| Mariappan [135] | 2013 | x | x | x | x | |||||
| Ashmore [68] | 2013 | x | x | |||||||
| Andersen et al. [136] | 2013 | x | x | x | x | x | ||||
| Songstad et al. [137] | 2012 | x | x | x | x | |||||
| Waitzkin H. et al. [69] | 2012 | x | x | x | ||||||
| Kjeldsen [138] | 2012 | x | ||||||||
| Georgellis et al. [139] | 2011 | x | ||||||||
| Aysen and Parumasur [140] | 2011 | x | x | x | ||||||
| Halepota and Shah [95] | 2011 | x | x | x | ||||||
| Leonard and Masatu [141] | 2010 | x | x | x | x | |||||
| Peters et al. [59] | 2010 | x | x | x | ||||||
| Malik et al. [142] | 2010 | x | x | x | x | x | x | |||
| Serneels et al. [143] | 2010 | x | ||||||||
| Le Julian [144] | 2010 | x | ||||||||
| Mbindyo et al. [67] | 2009 | x | x | x | x | x | x | x | ||
| Andersen [145] | 2009 | x | ||||||||
| Mangham and Hanson [146] | 2008 | x | x | |||||||
| Modipa and Dambisya [147] | 2008 | x | ||||||||
| Dambisya et al. [79] | 2007 | x | x | x | x | |||||
| Agyepong et al. [148] | 2004 | x | x | x | x | |||||
| Humphrey and Russell [62] | 2004 | x | x | x | ||||||
| Franco et al. [89] | 2002 | x | x | x | x | |||||
| Lee-Ross [149] | 2002 | x | x | |||||||
| Pipan [150] | 2000 | x | ||||||||
| Smith [94] | 1999 | x | x | x | ||||||
| Ferrinho et al. [83] | 1998 | x | x |
References
- Perry, J.L.; Wise, L. The motivational bases of public service. Public Adm. Rev. 1990, 50, 367–373. [Google Scholar]
- Ritz, A.; Brewer, G.A.; Neumann, O. Public Service Motivation: A Systematic Literature Review and Outlook. Public Adm. Rev. 2016, 76, 414–426. [Google Scholar]
- Waterhouse, J. Motivation in Public Management: The Call of Public Service. Aust. J. Public Adm. 2008, 67, 505–507. [Google Scholar]
- O’Riordan, J. Public Service Motivation: State of Public Service Series. Inst. Public Adm. 2013, 1–36. [Google Scholar]
- George, A.; Scott, K.; Govender, V. A Health Policy and Systems Research Reader on Human Resources for Health; World Health Organization: Geneva, Switzerland, 2017; pp. 1–528. [Google Scholar]
- Dieleman, M.; Gerretsen, B.; van der Wilt, G. Human resource management interventions to improve health workers’ performance in low and middle income countries: A realist review. Health Res. Policy Syst. 2009, 7, 7. [Google Scholar]
- Lee, M.T.; Raschke, R.L. Understanding employee motivation and organizational performance: Arguments for a set-theoretic approach. J. Innov. Knowl. 2016, 1, 162–169. [Google Scholar]
- Santinha, G.; Carvalho, T.; Forte, T.; Fernandes, A.; Tavares, J. Profiling Public Sector Choice: Perceptions and Motivational Determinants at the Pre-Entry Level. Sustainability 2021, 13, 1272. [Google Scholar]
- Collins, B. What’s the problem in Public Sector workforce recruitment? A comparative analysis of the public, non-profit, and private sectors. Int. J. Public Adm. 2008, 31, 1592–1608. [Google Scholar]
- French, P.; Emerson, M. Assessing the Variations in Reward Preference for Local Government Employees in Terms of Position, Public Service Motivation, and Public Sector Motivation. Public Perform. Manag. Rev. 2014, 37, 552–576. [Google Scholar]
- Rainey, H.G. Reward preferences among public and private managers: In search of the service ethic. Am. Rev. Public Adm. 1982, 16, 288–302. [Google Scholar]
- Perry, J.L. Measuring Public Service Motivation: An Assessment of Construct Reliability and Validity. J. Public Adm. Res. Theory 1996, 6, 5–22. [Google Scholar]
- Kim, S.; Vandenabeele, W.; Wright, B.E.; Andersen, L.B.; Cerase, F.P.; Christensen, R.K.; Desmarais, C.; Koumenta, M.; Leisink, P.; Liu, B.; et al. Investigating the Structure and Meaning of Public Service Motivation across Populations: Developing an International Instrument and Addressing Issues of Measurement Invariance. J. Public Adm. Res. Theory 2013, 23, 79–102. [Google Scholar]
- Paarlberg, L.E.; Perry, J.L. Values Management: Aligning Employee Values and Organization Goals. Am. Rev. Public Adm. 2007, 37, 387–408. [Google Scholar]
- Miao, Q.; Eva, N.; Newman, A.; Schwarz, G. Public service motivation and performance: The role of organizational identification. Public Money Manag. 2019, 39, 77–85. [Google Scholar]
- Breaugh, J.; Ritz, A.; Alfes, K. Work motivation and public service motivation: Disentangling varieties of motivation and job satisfaction. Public Manag. Rev. 2018, 20, 1423–1443. [Google Scholar]
- O’Leary, C. Public Service Motivation: A Rationalist Critique. Public Pers. Manag. 2019, 48, 82–96. [Google Scholar]
- Legault, L. Intrinsic and Extrinsic Motivation. In Encyclopedia of Personality and Individual Differences; Zeigler-Hill, V., Shackelford, T., Eds.; Springer: Cham, Switzerland, 2016. [Google Scholar]
- Lewis, B.G.; Frank, S.A. Who Wants to Work for the Government? Public Adm. Rev. 2002, 62, 395–404. [Google Scholar]
- Okello, D.R.; Gilson, L. Exploring the influence of trust relationships on motivation in the health sector: A systematic review. Hum. Resour. Health 2015, 13, 16. [Google Scholar]
- Fritzen, S. Strategic management of the health workforce in developing countries: What have we learned? Hum. Res. Health 2007, 5, 4. [Google Scholar]
- Campbell, J.; Dussault, G.; Buchan, J.; Pozo-Martin, F.; Guerra, M.G.; Leone, C.; Siyam, A.; Cometto, G. A Universal Truth: No Health without a Workforce. Forum Report, Third Global Forum on Human Resources for Health; Global Health Workforce Alliance and World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Muthuri, R.; Senkubuge, F.; Hongoro, C. Determinants of Motivation among Healthcare Workers in the East African Community between 2009–2019: A Systematic Review. Healthcare 2020, 8, 164. [Google Scholar]
- World Health Organization. Health Workforce Policy and Management in the Context of the COVID-19 Pandemic Response: Interim Guidance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Kunisch, S.; Menz, M.; Bartunek, J.M.; Cardinal, L.B.; Denyer, D. Feature topic at organizational research methods: How to conduct rigorous and impactful literature reviews? Organ. Res. Methods 2018, 21, 519–523. [Google Scholar]
- Dixon-Woods, M.; Bonas, S.; Booth, A.; Jones, D.R.; Miller, T.; Sutton, A.J.; Shaw, R.; Smith, J.; Young, B. How can systematic reviews incorporate qualitative research? A critical perspective. Qual. Res. 2006, 6, 27–44. [Google Scholar]
- Cooper, H. Research Synthesis and Meta-Analysis, 4th ed.; Sage Publications: Thousand Oaks, CA, USA, 2010. [Google Scholar]
- Migchelbrink, K.; Van de Walle, S. A systematic review of the literature on determinants of public managers’ attitudes toward public participation. Local Gov. Stud. 2021, 48, 1–22. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.P.; Devereaux, J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-analyses of Studies that Evaluate Health Care Interventions: Explanation and Elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 4, 1. [Google Scholar]
- Pitchforth, E.; Nolte, E.; Corbett, J.; Miani, C.; Winpenny, E.; van Teijlingen, E.; Elmore, N.; King, S.; Ball, S.; Miler, J.; et al. Community hospitals and their services in the NHS: Identifying transferable learning from international developments—Scoping review, systematic review, country reports and case studies. NIHR J. Libr. 2017, 5, 1–220. [Google Scholar]
- Yang, L.; Zhang, H.; Shen, H.; Huang, X.; Zhou, X.; Rong, G.; Shao, D. Quality Assessment in Systematic Literature Reviews: A Software Engineering Perspective. Inf. Softw. Technol. 2020, 130, 106397. [Google Scholar]
- Critical Appraisal Skills Programme (2013) CASP Checklist. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 2 January 2022).
- Health Evidence. Quality Assessment Tool—Review Articles. Available online: https://healthevidence.org/practice-tools.aspx#PT1 (accessed on 2 January 2022).
- Wismar, M.; Maier, C.B.; Glinos, I.A.; Dussault, G.; Figueras, J. Health Professional Mobility and Health Systems: Evidence from 17 European Countries; European Observatory on Health Systems and Policies, WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Mathauer, I.; Imhoff, I. Health Worker Motivation in Africa: The Role of Non-Financial Incentives and Human Resource Management Tools. Hum. Resour. Health 2006, 4, 24. [Google Scholar]
- Eskildsen, J.K.; Kristensen, K.; Westlund, A.H. Work motivation and job satisfaction in the Nordic countries. Empl. Relat. 2004, 26, 122–136. [Google Scholar]
- Abbasi, A.; Hossain, L.; Uddin, S.; Rasmussen, K.J. Evolutionary dynamics of scientific collaboration networks: Multi-levels and cross-time analysis. Scientometrics 2011, 89, 687–710. [Google Scholar]
- Trujillo, C.M.; Long, T.M. Document co-citation analysis to enhance transdisciplinary research. Sci. Adv. 2018, 4, e1701130. [Google Scholar]
- Garfield, E.; Pudovkin, A.I.; Istomin, V.S. Why do we need algorithmic historiography? J. Am. Soc. Inf. Sci. Technol. 2003, 54, 400–412. [Google Scholar]
- Mutale, W.; Ayles, H.; Bond, V.; Mwanamwenge, M.T.; Balabanova, D. Measuring Health Workers’ Motivation in Rural Health Facilities: Baseline Results from Three Study Districts in Zambia. Hum. Resour. Health 2013, 11, 8. [Google Scholar]
- Maslow, A.H. A theory of human motivation. Psychol. Rev. 1943, 50, 370–396. [Google Scholar]
- Deci, E.L.; Ryan, R.M. Self-Determination Theory: When Mind Mediates Behavior. J. Mind Behav. 1980, 1, 33–43. [Google Scholar]
- McClelland, C.A. The function of theory in international relations. J. Confl. Resolut. 1960, 4, 303–336. [Google Scholar]
- Herzberg, F.; Mausner, B.; Snyderman, B. The Motivation to Work, 2nd ed.; Wiley: Hoboken, NJ, USA, 1959. [Google Scholar]
- Hackman, J.R.; Oldham, G.R. Development of the job diagnostic survey. J. Appl. Psychol. 1975, 60, 159–170. [Google Scholar]
- Wang, T.M.; Witteloostuijn, A.; Heine, F. A Moral Theory of Public Service Motivation. Front. Psychol. 2020, 11, 517763. [Google Scholar]
- Cavanaugh, M.A.; Boswell, W.R.; Roehling, M.V.; Boudreau, J.W. An empirical examination of self-reported work stress among U.S. managers. J. Appl. Psychol. 2000, 85, 65–74. [Google Scholar]
- Koopman, C.; Pelletier, K.R.; Murray, J.F.; Sharda, C.E.; Berger, M.L.; Turpin, R.S.; Hackleman, P.; Gibson, P.; Holmes, D.M.; Bendel, T. Stanford presenteeism scale: Health status and employee productivity. J. Occup. Environ. Med. 2002, 44, 14–20. [Google Scholar]
- Vandenabeele, W. The mediating effect of job satisfaction and organizational commitment on self-reported performance: More robust evidence of the PSM-performance relationship. Int. Rev. Adm. Sci. 2009, 75, 11–34. [Google Scholar]
- Naff, K.C.; Crum, J. Working for America: Does Public Service Motivation Make a Difference? Rev. Public Pers. Adm. 1999, 19, 5–16. [Google Scholar]
- Belita, A.; Mbindyo, P.; English, M. Absenteeism amongst Health Workers—Developing a Typology to Support Empiric Work in Low-Income Countries and Characterising Reported Associations. Hum. Resour. Health 2013, 11, 34. [Google Scholar]
- Hotchkiss, D.R.; Banteyerga, H.; Tharaney, M. Job Satisfaction and Motivation among Public Sector Health Workers: Evidence from Ethiopia. Hum. Resour. Health 2015, 13, 83. [Google Scholar]
- Bhatnagar, A.; Gupta, S.; Alonge, O.; George, A.S. Primary Health Care Workers’ Views of Motivating Factors at Individual, Community and Organizational Levels: A Qualitative Study from Nasarawa and Ondo States, Nigeria. Int. J. Health Plan. Manag. 2017, 32, 217–233. [Google Scholar]
- Khim, K. Are Health Workers Motivated by Income? Job Motivation of Cambodian Primary Health Workers Implementing Performance-Based Financing. Glob. Health Action 2016, 9, 31068. [Google Scholar]
- Gąsiorowski, J.; Rudowicz, E.; Safranow, K. Motivation towards medical career choice and future career plans of Polish medical students. Adv. Health Sci. Educ. Theory Pract. 2015, 20, 709–725. [Google Scholar]
- Ojakaa, D.; Olango, S.; Jarvis, J. Factors Affecting Motivation and Retention of Primary Health Care Workers in Three Disparate Regions in Kenya. Hum. Resour. Health 2014, 12, 33. [Google Scholar]
- Ghimire, J.; Gupta, R.P.; Kumal, A.B.; Mahato, R.K.; Bhandari, R.M.; Thapa, N. Factors associated with the motivation and de-motivation of health workforce in Nepal. J. Nepal Health Res. Counc. 2013, 11, 112–118. [Google Scholar]
- Peters, D.H.; Chakraborty, S.; Mahapatra, P.; Steinhardt, L. Job Satisfaction and Motivation of Health Workers in Public and Private Sectors: Cross-Sectional Analysis from Two Indian States. Hum. Resour. Health 2010, 8, 27. [Google Scholar]
- Bansal, R.N.; Malhotra, M. A Case Study of Motivational Levels among Personnel Working in a Government Teaching Hospital of Punjab. Biomed. Pharmacol. J. 2016, 9, 585–591. [Google Scholar]
- Mir, A.M.; Shaikh, M.S.; Rashida, G.; Mankani, N. To Serve or to Leave: A Question Faced by Public Sector Healthcare Providers in Pakistan. Health Res. Policy Syst. 2015, 13, S58. [Google Scholar]
- Humphrey, C.; Russell, J. Motivation and Values of Hospital Consultants in South-East England Who Work in the National Health Service and Do Private Practice. Soc. Sci. Med. 2004, 59, 1241–1250. [Google Scholar]
- Chang, C.T.; Hassali, M.A.; Hss, A.S.; Lee, J.C.Y.; Chan, H.K. Perceived motivators, training supports and challenges to career advancement among pharmacists in the Malaysian public healthcare system. Int. J. Pharm. Pract. 2019, 27, 555–564. [Google Scholar]
- Alhassan, R.K.A.; Nketiah-Amponsah, E.; Spieker, N.; Arhinful, D.K.; de Rinke Wit, T.F. Assessing the Impact of Community Engagement Interventions on Health Worker Motivation and Experiences with Clients in Primary Health Facilities in Ghana: A Randomized Cluster Trial. PLoS ONE 2016, 11, e0158541. [Google Scholar]
- Bonenberger, M.; Aikins, M.; Akweongo, P.; Wyss, K. The Effects of Health Worker Motivation and Job Satisfaction on Turnover Intention in Ghana: A Cross-Sectional Study. Hum. Resour. Health 2014, 12, 43. [Google Scholar]
- Purohit, B.; Bandyopadhyay, T. Beyond Job Security and Money: Driving Factors of Motivation for Government Doctors in India. Hum. Resour. Health 2014, 12, 12. [Google Scholar]
- Chew, B.; Ramli, A.; Omar, M.; Ismail, I. A preliminary study of job satisfaction and motivation among the Malaysian primary healthcare professionals. Malays. Fam. Physician 2013, 8, 15–25. [Google Scholar]
- Ashmore, J. “Going Private”: A Qualitative Comparison of Medical Specialists Job Satisfaction in the Public and Private Sectors of South Africa. Hum. Resour. Health 2013, 11, 6. [Google Scholar]
- Waitzkin, H.; Yager, J.; Santos, R. Advancing the Business Creed? The Framing of Decisions about Public Sector Managed Care. Sociol. Health Illn. 2012, 34, 31–48. [Google Scholar]
- Frehywot, S.; Mullan, F.; Payne, P.W.; Ross, H. Compulsory service programmes for recruiting health workers in remote and rural areas: Do they work? Bull. World Health Organ. 2010, 88, 364–370. [Google Scholar]
- Rahman, S.M.; Ali, N.A.; Jennings, L.; Seraji, M.H.R.; Mannan, I.; Shah, R.; Al-Ahmud, A.B.; Bari, S.; Hossain, D.; Das, M.K.; et al. Factors affecting recruitment and retention of community health workers in a newborn care intervention in Bangladesh. Hum. Resour. Health 2010, 8, 10–12. [Google Scholar]
- Armstrong, M. Human Resource Management Practice, 12th ed.; KoganPage: London, UK, 2012. [Google Scholar]
- Androniceanu, A.; Sabie, O.M.; Pegulescu, A. An integrated approach of the human resources motivation and the quality of health services. Theor. Empir. Res. Urban Manag. 2020, 15, 42–53. [Google Scholar]
- Prust, M.L.; Kamanga, A.; Ngosa, L.; McKay, C.; Muzongwe, C.M.; Mukubani, M.T.; Chihinga, R.; Misapa, R.; van den Broek, J.W.; Wilmink, N. Assessment of Interventions to Attract and Retain Health Workers in Rural Zambia: A Discrete Choice Experiment. Hum. Resour. Health 2019, 17, 26. [Google Scholar]
- Sato, M.; Maufi, D.; Mwingira, U.J.; Leshabari, M.T.; Ohnishi, M.; Honda, S. Measuring Three Aspects of Motivation among Health Workers at Primary Level Health Facilities in Rural Tanzania. PLoS ONE 2017, 12, e0184599. [Google Scholar]
- Korlén, S.; Essén, A.; Lindgren, P.; Amer-Wahlin, I.; von Thiele Schwarz, U. Managerial Strategies to Make Incentives Meaningful and Motivating. J. Health Organ. Manag. 2017, 31, 126–141. [Google Scholar]
- Mazahir, S.; Khalid, S. Work Environment and Situational Motivation of Doctors in Public Sector Hospitals. Ann. King Edw. Med. Univ. 2017, 23, 1509. [Google Scholar]
- Mbindyo, P.; Gilson, L.; Blaauw, D.; English, M. Contextual Influences on Health Worker Motivation in District Hospitals in Kenya. Implement. Sci. 2009, 4, 43. [Google Scholar]
- Dambisya, Y.M.; Modipa, I.S.; Legodi, M.G. Factors Influencing the Distribution of Pharmacy Graduates of the University of the North, South Africa. East Afr. Med. J. 2007, 84, 481–488. [Google Scholar]
- Jaeger, F.N.; Bechir, M.; Harouna, M.; Moto, D.D.; Utzinger, J. Challenges and opportunities for healthcare workers in a rural district of Chad. BMC Health Serv. Res. 2018, 18, 7. [Google Scholar]
- Topp, S.M.; Chipukuma, J.M.; Hanefeld, J. Understanding the dynamic interactions driving Zambian health centre performance: A case-based health systems analysis. Health Policy Plan. 2015, 30, 485–499. [Google Scholar]
- Russo, G.; Rego, I.; Perelman, J.; Barros, P.P. A Tale of Loss of Privilege, Resilience and Change: The Impact of the Economic Crisis on Physicians and Medical Services in Portugal. Health Policy 2016, 120, 1079–1086. [Google Scholar]
- Ferrinho, P.; Van Lerberghe, W.; Julien, M.R.; Fresta, E.; Gomes, A.; Dias, F.; Gonçalves, A.; Bäckström, B. How and why public sector doctors engage in private practice in Portuguese-speaking African countries. Health Policy Plan. 1998, 13, 332–338. [Google Scholar]
- Bratton, J.; Sawchuk, P.; Forshaw, C.; Callinan, M.; Corbet, M. Work and Organizational Behaviour, 2nd ed.; Palgrave Macmillan: Basingstoke, UK, 2010. [Google Scholar]
- Cantarelli, P.; Belle, N.; Longo, F. Exploring the Motivational Bases of Public Mission-Driven Professions Using a Sequential-Explanatory Design. Public Manag. Rev. 2020, 22, 1535–1559. [Google Scholar]
- Belrhiti, Z.; van Damme, W.; Belalia, A.; Marchal, B. The Effect of Leadership on Public Service Motivation: A Multiple Embedded Case Study in Morocco. BMJ Open 2020, 10, e033010. [Google Scholar]
- Aninanya, G.A.; Howard, N.; Williams, J.E.; Apam, B.; Prytherch, H.; Loukanova, S.; Kamara, E.K.; Otupiri, E. Can Performance-Based Incentives Improve Motivation of Nurses and Midwives in Primary Facilities in Northern Ghana? A Quasi-Experimental Study. Glob. Health Action 2016, 9, 32404. [Google Scholar]
- Kitsios, F.; Kamariotou, M. Job satisfaction behind motivation: An empirical study in public health workers. Heliyon 2021, 7, e06857. [Google Scholar]
- Franco, L.M.; Bennett, S.; Kanfer, R. Health sector reform and public sector health worker motivation: A conceptual framework. Soc. Sci. Med. 2002, 54, 1255–1266. [Google Scholar]
- Ralston, D.A.; Egri, C.P.; Stewart, S.; Terpstra, R.H.; Yu, K. Doing business in 21st century with the new generation of Chinese manager: A study of generational shifts in work values in China. J. Int. Bus. Stud. 1999, 30, 415–428. [Google Scholar]
- Jing, L.; Ma, Z.; Ma, Z.; Chen, B.; Cheng, S. Nurse Practitioners’ Work Values and Their Conflict Management Approaches in a Stressful Workplace: A Taiwan Study. Sustainability 2020, 12, 1040. [Google Scholar]
- Shibata, S.; Thepthien, B.T.; Sermsri, S. Intention toward Working in the Private Sector among Fourth-Year Nursing Students in Thailand. J. Health Res. 2015, 29, 23–29. [Google Scholar]
- Halepota, J.A.; Shah, N. An Empirical Investigation of Organisational Antecedents on Employee Job Satisfaction in a Developing Country. Transform. Gov. People Process Policy 2011, 5, 280–294. [Google Scholar]
- Smith, L. An Evaluation of Programmes for Staff Motivation in NHS and Hotel Ancillary Staff. Facilities 1999, 17, 264–271. [Google Scholar]
- Bimpong, K.A.A.; Khan, A.; Slight, R.; Tolley, C.L.; Slight, S.P. Relationship between labour force satisfaction, wages and retention within the UK National Health Service: A systematic review of the literature. BMJ Open 2020, 10, e034919. [Google Scholar]
- McCarthy, D.; Wei, P.; Homberg, F.; Tabvuma, V. Public service motivation in the Chinese public and private sectors. Evid. -Based HRM 2021, 9, 1–17. [Google Scholar]
- Jiang, H.; Jia, H.; Zhang, J.; Li, Y.; Song, F.; Yu, X. Nurses’ Occupational Stress and Presenteeism: The Mediating Role of Public Service Motivation and the Moderating Role of Health. Int. J. Environ. Res. Public Health 2021, 18, 3523. [Google Scholar]
- Stefurak, T.; Morgan, R.; Johnson, R.B. The Relationship of Public Service Motivation to Job Satisfaction and Job Performance of Emergency Medical Services Professionals. Public Pers. Manag. 2020, 49, 590–616. [Google Scholar]
- Ebenso, B.; Mbachu, C.; Etiaba, E.; Huss, R.; Manzano, A.; Onwujekwe, O.; Uzochukwu, B.; Ezumah, N.; Ensor, T.; Hicks, J.P.; et al. Which Mechanisms Explain Motivation the of Primary Health Workers? Insights from the Realist Evaluation of a Maternal and Child Health Programme in Nigeria. BMJ Glob. Health 2020, 5, e002408. [Google Scholar]
- Jensen, U.T.; Kjeldsen, A.M.; Vestergaard, C.F. How is public service motivation affected by regulatory policy changes? Int. Public Manag. J. 2020, 23, 465–495. [Google Scholar]
- Abdelmotaleb, M. The Moderating and Mediating Role of Public Service Motivation between Organization’s Social Responsibility and Employee Engagement: Evidence from Egyptian Public Hospitals. Int. Rev. Public Adm. 2020, 25, 207–223. [Google Scholar]
- Van Loon, N.M.; Baekgaard, M.; Moynihan, D.P. Stability Not Change: Improving Frontline Employee Motivation through Organizational Reform Is Harder than It Looks. Public Adm. 2020, 98, 591–608. [Google Scholar]
- Deng, J.; Li, Y.; Sun, Y.; Lei, R.; Yang, T. Public Service Motivation as a Mediator of the Relationship between Job Stress and Presenteeism: A Cross-Sectional Study from Chinese Public Hospitals. BMC Health Serv. Res. 2019, 19, 625. [Google Scholar]
- Deng, J.; Guo, Y.; Ma, T.; Yang, T.; Tian, X. How Job Stress Influences Job Performance among Chinese Healthcare Workers: A Cross-Sectional Study. Environ. Health Prev. Med. 2019, 24, 2. [Google Scholar]
- Adams, A.M.; Ahmed, R.; Shuvo, T.A.; Yusuf, S.S.; Akhter, S.; Anwar, I. Exploratory Qualitative Study to Understand the Underlying Motivations and Strategies of the Private For-Profit Healthcare Sector in Urban Bangladesh. BMJ Open 2019, 9, e026586. [Google Scholar]
- Borghi, J.; Lohmann, J.; Dale, E.; Meheus, F.; Goudge, J.; Oboirien, K.; Kuwawenaruwa, A. How to Do (or Not to Do)—Measuring Health Worker Motivation in Surveys in Low- and Middle-Income Countries. Health Policy Plan. 2018, 33, 192–203. [Google Scholar]
- Zweigenthal, V.E.M.; Pick, W.M.; London, L. Motivations of South African Physicians Specialising in Public Health. Glob. Health Action 2018, 11, 1475039. [Google Scholar]
- Aguilera Dreyse, B.; López Gaete, G. ¿Tiene El Médico El Deber Moral de Trabajar En El Sector Público de Salud? Consideraciones Éticas Sobre Las Obligaciones Sociales Del Médico. Medwave 2017, 17, 7105. [Google Scholar]
- Abera, G.G.; Alemayehu, Y.K.; Henry, J. Public-on-Private Dual Practice among Physicians in Public Hospitals of Tigray National Regional State, North Ethiopia: Perspectives of Physicians, Patients and Managers. BMC Health Serv. Res. 2017, 17, 713. [Google Scholar]
- Masood, M.; Afsar, B. Transformational Leadership and Innovative Work Behavior among Nursing Staff. Nurs. Inq. 2017, 24, e12188. [Google Scholar]
- Levitats, Z.; Vigoda-Gadot, E. Yours Emotionally: How Emotional Intelligence Infuses Public Service Motivation and Affects the Job Outcomes of Public Personnel. Public Adm. 2017, 95, 759–775. [Google Scholar]
- Millar, R.; Chen, Y.; Wang, M.; Fang, L.; Liu, J.; Xuan, Z.; Li, G. It’s All about the Money? A Qualitative Study of Healthcare Worker Motivation in Urban China. Int. J. Equity Health 2017, 16, 120. [Google Scholar]
- Seth, K. Heterogeneity in the Background and Earnings of Nurses in India: Evidence from a Cross-Sectional Study in Gujarat. Health Policy Plan. 2017, 32, 1285–1293. [Google Scholar]
- Hou, X.; Witter, S.; Zaman, R.U.; Engelhardt, K.; Hafidz, F.; Julia, F.; Lemiere, C.; Sullivan, E.B.; Saldanha, E.; Palu, T.; et al. What Do Health Workers in Timor-Leste Want, Know and Do Findings from a National Health Labour Market Survey. Hum. Resour. Health 2016, 14, 69. [Google Scholar]
- Bhatnagar, A.; George, A.S. Motivating Health Workers up to a Limit: Partial Effects of Performance-Based Financing on Working Environments in Nigeria. Health Policy Plan. 2016, 31, 868–877. [Google Scholar]
- Shah, S.M.; Zaidi, S.; Ahmed, J.; Ur Rehman, S. Motivation and Retention of Physicians in Primary Healthcare Facilities: A Qualitative Study from Abbottabad, Pakistan. Int. J. Health Policy Manag. 2016, 5, 467–475. [Google Scholar]
- Namakula, J.; Witter, S.; Ssengooba, F. Health Worker Experiences of and Movement between Public and Private Not-for-Profit Sectors-Findings from Post-Conflict Northern Uganda. Hum. Resour. Health 2016, 14, 18. [Google Scholar]
- Van Loon, N.M. Is Public Service Motivation Related to Overall and Dimensional Work-Unit Performance as Indicated by Supervisors? Int. Public Manag. J. 2016, 19, 78–110. [Google Scholar]
- Kadam, S.; Nallala, S.; Zodpey, S.; Pati, S.; Hussain, M.A.; Chauhan, A.S.; Das, S.; Martineau, T. A Study of Organizational versus Individual Needs Related to Recruitment, Deployment and Promotion of Doctors Working in the Government Health System in Odisha State, India. Hum. Resour. Health 2016, 14, 7. [Google Scholar]
- Ashmore, J.; Gilson, L. Conceptualizing the Impacts of Dual Practice on the Retention of Public Sector Specialists—Evidence from South Africa. Hum. Resour. Health 2015, 13, 3. [Google Scholar]
- Bellé, N. Performance-Related Pay and the Crowding out of Motivation in the Public Sector: A Randomized Field Experiment. Public Adm. Rev. 2015, 75, 230–241. [Google Scholar]
- Schmiedeknecht, K.; Perera, M.; Schell, E.; Jere, J.; Geoffroy, E.; Rankin, S. Predictors of Workforce Retention Among Malawian Nurse Graduates of a Scholarship Program: A Mixed-Methods Study. Glob. Health Sci. Pract. 2015, 3, 85–96. [Google Scholar]
- Russo, G.; de Sousa, B.; Sidat, M.; Ferrinho, P.; Dussault, G. Why Do Some Physicians in Portuguese-Speaking African Countries Work Exclusively for the Private Sector? Findings from a Mixed-Methods Study. Hum. Resour. Health 2014, 12, 51. [Google Scholar]
- Hennig-Schmidt, H.; Wiesen, D. Other-Regarding Behavior and Motivation in Health Care Provision: An Experiment with Medical and Non-Medical Students. Soc. Sci. Med. 2014, 108, 156–165. [Google Scholar]
- Lagarde, M.; Blaauw, D. Pro-Social Preferences and Self-Selection into Jobs: Evidence from South African Nurses. J. Econ. Behav. Organ. 2014, 107, 136–152. [Google Scholar]
- Krogsgaard, J.A.; Thomsen, P.; Andersen, L.B. Only If We Agree? How Value Conflicts Moderate the Relationship Between Transformational Leadership and Public Service Motivation. Int. J. Public Adm. 2014, 37, 895–907. [Google Scholar]
- Schott, C.; Pronk, J.L.J. Investigating and Explaining Organizational Antecedents of PSM. Evid. Based HRM 2014, 2, 28–56. [Google Scholar]
- Diwan, V.; Minj, C.; Chhari, N.; de Costa, A. Indian Medical Students in Public and Private Sector Medical Schools: Are Motivations and Career Aspirations Different?—Studies from Madhya Pradesh, India. BMC Med. Educ. 2013, 13, 127. [Google Scholar]
- Alhassan, R.K.; Spieker, N.; van Ostenberg, P.; Ognik, A.; Nketiah-Amponsah, E.; De Wit, T.F.R. Association between health worker motivation and healthcare quality efforts in Ghana. Hum. Resour. Health 2013, 11, 37. [Google Scholar]
- Kolstad, J.R.; Lindkvist, I. Pro-Social Preferences and Self-Selection into the Public Health Sector: Evidence from an Economic Experiment. Health Policy Plan. 2013, 28, 320–327. [Google Scholar]
- George, G.; Gow, J.; Bachoo, S. Understanding the Factors Influencing Health-Worker Employment Decisions in South Africa. Hum. Resour. Health 2013, 11, 15. [Google Scholar]
- Dos Santos, B.F.; Nicolau, B.; Muller, K.; Bedos, C.; Zuanon, A.C. Brazilian dental students’ intentions and motivations towards their professional career. J. Dent. Educ. 2013, 77, 337–344. [Google Scholar]
- Bellé, N. Experimental Evidence on the Relationship between Public Service Motivation and Job Performance. Public Adm. Rev. 2012, 73, 143–153. [Google Scholar]
- Van Loon, N.M.; Leisink, P.; Vandenabeele, W. Talking the Talk of Public Service Motivation: How Public Organization Logics Matter for Employees’ Expressions of PSM. Int. J. Public Adm. 2013, 36, 1007–1019. [Google Scholar]
- Mariappan, M. Analysis of Nursing Job Characteristics in Public Sector Hospitals. J. Health Manag. 2013, 15, 253–262. [Google Scholar]
- Andersen, L.B.; Kristensen, N.; Pedersen, L.H. Models of Public Service Provision-When Will Knights and Knaves Be Responsive to Pawns and Queens? Int. J. Public Adm. 2013, 36, 126–136. [Google Scholar]
- Songstad, N.G.; Moland, K.M.; Massay, D.A.; Blystad, A. Why Do Health Workers in Rural Tanzania Prefer Public Sector Employment? BMC Health Serv. Res. 2012, 12, 92. [Google Scholar]
- Kjeldsen, A.M. Sector and Occupational Differences in Public Service Motivation: A Qualitative Study. Int. J. Public Adm. 2012, 35, 58–69. [Google Scholar]
- Georgellis, Y.; Iossa, E.; Tabvuma, V.; Smith, S.; Estache, A.; Pommet, S.; Hunter, J.; Roy, J.; Pouliakas, K.; Clark, A. Crowding Out Intrinsic Motivation in the Public Sector. J. Public Adm. Res. Theory 2011, 21, 473–493. [Google Scholar]
- Aysen, G.; Parumasur, S.B. Managerial role in enhancing employee motivation in public health care. Corp. Ownersh. Control. 2011, 8, 401–410. [Google Scholar]
- Leonard, K.L.; Masatu, M.C. Professionalism and the Know-Do Gap: Exploring Intrinsic Motivation among Health Workers in Tanzania. Health Econ. 2010, 19, 1461–1477. [Google Scholar]
- Malik, A.A.; Yamamoto, S.S.; Souares, A.; Malik, Z.; Sauerborn, R. Motivational Determinants among Physicians in Lahore, Pakistan. BMC Health Serv. Res. 2010, 10, 201. [Google Scholar]
- Serneels, P.; Montalvo, J.G.; Pettersson, G.; Lievens, T.; Buterae, J.D.; Kidanu, A. Qui Est Disposé à Travailler Dans Un Poste de Santé En Milieu Rural? Le Rôle de La Motivation Propre, Des Origines Rurales et Des Institutions Confessionnelles En Éthiopie et Au Rwanda. Bull. World Health Organ. 2010, 88, 342–349. [Google Scholar]
- Le Julian, G. Knights and Knaves Return: Public Service Motivation and the Delivery of Public Services. Int. Public Manag. J. 2010, 13, 56–71. [Google Scholar]
- Andersen, B.L. What Determines the Behaviour and Performance of Health Professionals? Public Service Motivation, Professional Norms and/or Economic Incentives. Int. Rev. Adm. Sci. 2009, 75, 79–97. [Google Scholar]
- Mangham, L.J.; Hanson, K. Employment Preferences of Public Sector Nurses in Malawi: Results from a Discrete Choice Experiment. Trop. Med. Int. Health 2008, 13, 1433–1441. [Google Scholar]
- Modipa, S.I.; Dambisya, Y.M. Profile and career preferences of pharmacy students at the University of Limpopo, Turfloop Campus, South Africa. Educ. Health 2008, 21, 164. [Google Scholar]
- Agyepong, I.A.; Anafi, P.; Asiamah, E.; Ansah, E.K.; Ashon, D.A.; Narh-Dometey, C. Health Worker (Internal Customer) Satisfaction and Motivation in the Public Sector in Ghana. Int. J. Health Plan. Manag. 2004, 19, 319–336. [Google Scholar]
- Lee-Ross, D. An Exploratory Study of Work Motivation among Private and Public Sector Hospital Chefs in Australia. J. Manag. Dev. 2002, 21, 576–588. [Google Scholar]
- Pipan, T. Metaphors and Organizational Identity in the Italian Public Services. Scand. J. Manag. 2000, 16, 391–409. [Google Scholar]


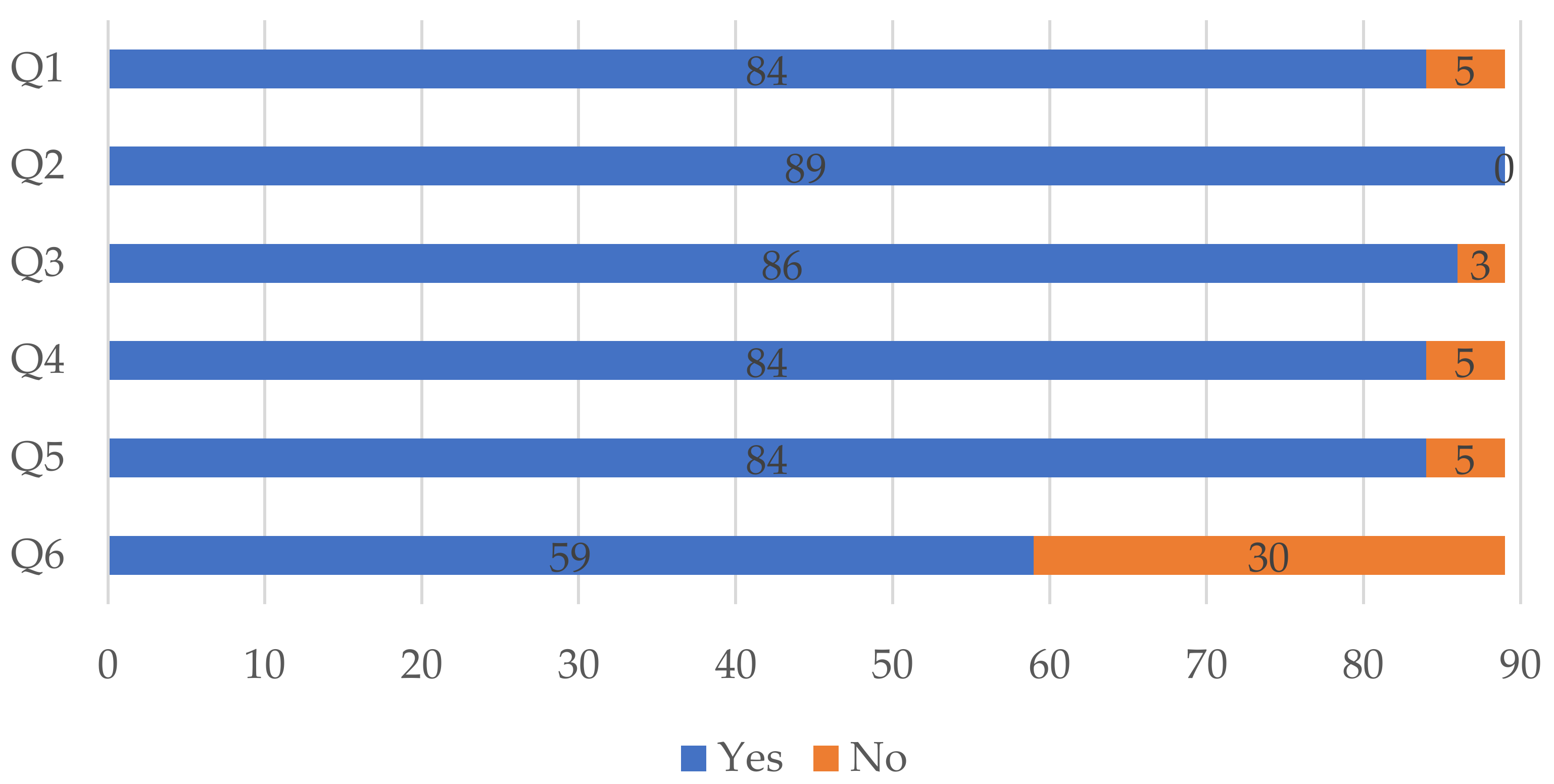
| # | Study Quality Assessment Questions |
|---|---|
| Q1 | Are the objectives of the study clearly identified? |
| Q2 | Is the context of the study clearly stated? |
| Q3 | Do the research methods support the aims of the study? |
| Q4 | Does the study have a comprehensive description of the instruments/scales employed? |
| Q5 | Is there a clear statement of the findings? |
| Q6 | Are the limitations of the study discussed extensively and explicitly? |
| Author | N | Institution | Research Area | Citations (Sum of Articles) | H-Index (Scopus) |
|---|---|---|---|---|---|
| Andersen, Lotte Bogh | 3 | Arizona State University | Political Science | 98 | 22 |
| Bellé, Nicola | 2 | Scuola Superiore Sant’Anna | Management | 278 | 14 |
| Blaauw, Duane | 2 | Univ. of the Witwatersrand Johannesburg | Health Policy | 97 | 22 |
| Alhassan, Robert Kaba | 2 | University of Health and Allied Sciences | Public Health | 85 | 10 |
| George, Asha S. | 2 | University of the Western Cape | Public Health | 59 | 30 |
| Bhatnagar, Aarushi | 2 | J.H. Bloomberg School of Public Health | International Health | 59 | 10 |
| Ferrinho, Paulo | 2 | IMHT—University of Lisbon | Human Resources for Health | 52 | 18 |
| Deng, Jianwei | 2 | Beijing Institute of Technology | Public Management | 17 | 8 |
| Belalia, Abdelmounin | 2 | National School of Public Health | Health Management | 14 | 4 |
| Belrhiti, Zakaria | 2 | National School of Public Health | Health Management | 14 | 5 |
| Journal | Number of Articles | Subject Area and Category | Quartile (2020) |
|---|---|---|---|
| Human Resources for Health | 15 | Public Health, Environmental and Occupational Health | Q1 |
| Health Policy and Planning | 5 | Health Policy | Q1 |
| BMC Health Services Research | 4 | Health Policy | Q1 |
| International Journal of Public Administration | 4 | Public Administration | Q2 |
| Global Health Action | 3 | Health Policy | Q1 |
| International Public Management Journal | 3 | Public Administration | Q1 |
| Social Science and Medicine | 3 | Health (Social Science) | Q1 |
| Country (ISO Code) | F | % | Continent | F | % |
|---|---|---|---|---|---|
| IN | 7 | 7.87 | Europe | 22 | 24.44 |
| DK, PK | 6 | 6.74 | North America | 3 | 3.33 |
| GH | 5 | 5.62 | Asia | 24 | 26.67 |
| CN, IT, TZ | 4 | 4.49 | Africa | 36 | 40.00 |
| NG, UK | 3 | 3.37 | South America | 2 | 2.22 |
| ZA, DE, ET, US, NL, MY, MW, MA, KN, ZM | 2 | 2.25 | Oceania | 1 | 1.11 |
| AO-GN-MZ-ST; AU; BD; BR; CV-GN-MZ; KH, CL, EG, UK-US; IL, NP, PL, PT, RO, RW, SE, TH, TP, UG | 1 | 1.12 | Not reported | 2 | 2.22 |
| Not reported | 2 | 2.25 | |||
| Total | 89 | 100 | Total | 90 1 | 100 |
| Country | Nº Articles | SCP | MCP | MCP_Ratio |
|---|---|---|---|---|
| United Kingdom | 8 | 6 | 2 | 0.25 |
| USA | 8 | 6 | 2 | 0.25 |
| Denmark | 5 | 5 | 0 | 0.00 |
| South Africa | 5 | 5 | 0 | 0.00 |
| China | 3 | 3 | 0 | 0.00 |
| Ghana | 3 | 2 | 1 | 0.33 |
| India | 3 | 3 | 0 | 0.00 |
| Italy | 3 | 3 | 0 | 0.00 |
| The Netherlands | 3 | 3 | 0 | 0.00 |
| Germany | 2 | 2 | 0 | 0.00 |
| Cluster | Designation | Number of Authors | Main Authors | Focus of Work | Links (n) | Total Link Strength (n) |
|---|---|---|---|---|---|---|
| Red | PSM and Organization Management | 17 | Perry (University of Indiana) | PSM scale | 41 | 2213 |
| Wright (Geórgia University) | Organizational behavior | 40 | 1310 | |||
| Andersen (Aarhus University) | PSM and factors affecting professional performance | 41 | 961 | |||
| Blue | Motivation and Organizational Behavior | 8 | Brewe (Georgia University) | Public management and organizational behavior | 40 | 1594 |
| Vandenabeele (Utrecht University) | Human resources motivation | 40 | 1546 | |||
| Kim (Seoul University) | PSM, organizational behavior, and personnel management | 36 | 1426 | |||
| Green | Policies for Health Motivation | 17 | Franco (University Research Co) | Motivation of health professionals and sector reforms | 37 | 312 |
| George (Western Cap University) | Motivation of health professionals | 34 | 231 | |||
| Dieleman (Amsterdam’s Vrije Universiteit) | Health human resources policies and motivation determinants | 34 | 196 |
| Organizations | F | % |
|---|---|---|
| Health Units (various levels) | 31 | 34.83 |
| Hospitals | 29 | 32.58 |
| Primary Health Care | 12 | 13.48 |
| Universities | 11 | 12.36 |
| Third-Sector Entities | 2 | 2.25 |
| Pharmacies | 2 | 2.25 |
| Primary Health Care/Hospitals | 1 | 1.12 |
| Hospitals/Universities | 1 | 1.12 |
| Professionals | F |
|---|---|
| Physician | 38 |
| Nurses | 29 |
| Hospital Administrators/Managers | 16 |
| Health Professionals (no area specification) | 14 |
| Technicians | 12 |
| Health Students | 11 |
| Pharmacists | 3 |
| Dentists | 1 |
| Type of Theory of Motivation | Main Theories | Freq. |
|---|---|---|
| Needs-based | Maslow Theory | 4 |
| Needs-based | Self-Determination Theory—Deci and Ryan | 3 |
| Needs-based | McClelland Theory | 3 |
| Needs-based | Herzberg’s Two-Factor Theory | 3 |
| Task-based | Job Characteristics Model—Hackman and Oldham | 3 |
| Motivation Theory | Brief Description |
|---|---|
| Maslow’s Hierarchy of Needs (Maslow, 1943) | A person is driven by achieving their necessities, from basic physiological factors, followed by security needs, safety, social interactions, self-esteem, and self-realization. |
| Job Characteristics Model (Hackman and Oldham, 1976) | There are five important work characteristics—skills, identity of the task, meaning of the task, feedback, and autonomy—which are essentially intrinsic motivational factors. |
| Self-Determination Theory (Deci and Ryan, 1980) | Explains the effects of the external consequences on intrinsic motivation. As such, external factors such as remuneration may contribute to question intrinsic behavior. |
| McClelland Theory (McClelland, 1960) | There are three main motivational drives in work contexts: realization, affiliation, and power. The first entails a need to achieve and show one’s own competences (self-realization). The second is an urge to be accepted and acknowledged by peers and others, and the third is the need to control their own work and the work of others. |
| Herzberg Theory (Herzberg, 1959) | Classifies the necessities in two categories: hygiene factors (or extrinsic) and motivational factors (or intrinsic). The motivational principles of this theory are achievement and recognition and the extrinsic remuneration and work safety. |
| Methodological Method | Freq. | % |
|---|---|---|
| Questionnaire | 42 | 47.19 |
| Interviews | 22 | 24.72 |
| Interviews/Focus Group | 6 | 6.74 |
| Questionnaire/Interviews | 6 | 6.74 |
| Secondary Analysis of Primary Sources | 4 | 4.49 |
| Direct Observation | 4 | 4.49 |
| Questionnaire/Interviews/Focus Group | 3 | 3.37 |
| Questionnaire/Focus Group | 1 | 1.12 |
| Questionnaire/Direct Observation | 1 | 1.12 |
| Main Factors | F |
|---|---|
| Low Salaries | 47 |
| Lack of Resources/Poor Working Conditions | 23 |
| Career Development | 11 |
| High Workload | 9 |
| Workplace | 8 |
| Balance Between Work and Family Life | 2 |
| Distance to the Workplace | 2 |
| Performance Evaluation | 1 |
| Main Factors | F |
|---|---|
| Absenteeism | 22 |
| Frequency of Contact With Patients/Altruism | 21 |
| Job Security | 16 |
| Recognition of Work | 11 |
| More Autonomy | 7 |
| Provision of Care | 3 |
| Religion | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, A.; Santinha, G.; Forte, T. Public Service Motivation and Determining Factors to Attract and Retain Health Professionals in the Public Sector: A Systematic Review. Behav. Sci. 2022, 12, 95. https://doi.org/10.3390/bs12040095
Fernandes A, Santinha G, Forte T. Public Service Motivation and Determining Factors to Attract and Retain Health Professionals in the Public Sector: A Systematic Review. Behavioral Sciences. 2022; 12(4):95. https://doi.org/10.3390/bs12040095
Chicago/Turabian StyleFernandes, Alexandre, Gonçalo Santinha, and Teresa Forte. 2022. "Public Service Motivation and Determining Factors to Attract and Retain Health Professionals in the Public Sector: A Systematic Review" Behavioral Sciences 12, no. 4: 95. https://doi.org/10.3390/bs12040095
APA StyleFernandes, A., Santinha, G., & Forte, T. (2022). Public Service Motivation and Determining Factors to Attract and Retain Health Professionals in the Public Sector: A Systematic Review. Behavioral Sciences, 12(4), 95. https://doi.org/10.3390/bs12040095








