Do I Really Want to Change? The Effectiveness of Goal Ambivalence Feedback on Dieters’ Motivation
Abstract
1. Introduction
2. Study 1
2.1. Method
2.1.1. Participants
2.1.2. Goal Ambivalence Scale
2.1.3. Health-Related Concerns and Actions (HRCA)
2.2. Procedure
2.3. Results
3. Discussion
4. Study 2
4.1. Participants
4.2. Instruments
4.3. Procedure
4.4. Results
4.4.1. Primary Analyses
4.4.2. Secondary Analyses
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Strongly disagree ☐ (1) | Disagree ☐ (2) | Agree ☐ (3) | Strongly agree ☐ (4) |
| Strongly disagree ☐ (1) | Disagree ☐ (2) | Agree ☐ (3) | Strongly agree ☐ (4) |
| Strongly disagree ☐ (1) | Disagree ☐ (2) | Agree ☐ (3) | Strongly agree ☐ (4) |
| Strongly disagree ☐ (1) | Disagree ☐ (2) | Agree ☐ (3) | Strongly agree ☐ (4) |
| Strongly disagree ☐ (1) | Disagree ☐ (2) | Agree ☐ (3) | Strongly agree ☐ (4) |
| Strongly disagree ☐ (1) | Disagree ☐ (2) | Agree ☐ (3) | Strongly agree ☐ (4) |
| WHAT DO YOUR SCORES MEAN? 0–3: It appears that your chances of doing something about your health-related concerns are not very high. But don’t lose hope! Read the sheet again and think about how you could change. Ask other people for help if you need it. 4–6: It appears that you have a moderate chance of doing something about your health-related concerns. Read the sheet again and think about how you could become more serious about doing something about your health-related concerns. Ask other people for help if you need it. 7–9: Your answers suggest that you are seriously planning to change or that you are already doing something to change. Congratulations! Just make sure that you make the change happen. |
Appendix B
| ☐ Blood test issues | ☐ HIV/AIDS | ☐ Smoking and vapors |
| ☐ Chronic pain | ☐ Memory loss | ☐ Stress/depression/anxiety |
| ☐ Diabetes and consequences | ☐ Mobility problems | ☐ medications and side effects |
| ☐ Eating and weight control | ☐ Relationship issues | ☐ Others (please list here) |
| ☐ Exercise | ☐ Sex-related issues | ………………………………… |
- ………………….
- ………………….
- ………………….
- ………………….
| ☐ I consent to being contacted via text messaging in two weeks for a 30-sec follow-up. ☐ I consent to being contacted via text messaging/email on how to receive information about the items that I marked in Section 3. ☐ My cellphone: ____________________or ☐ My email address: _______________________________ Note. For each box that you marked, we will send to you only one message: MOTIVE **** |
References
- Berrios, R.; Totterdell, P.; Kellett, S. Investigating goal conflict as a source of mixed emotions. Cogn. Emot. 2015, 29, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Freitas, A.L.; Clark, S.L.; Kim, J.Y.; Levy, S.R. Action-construal levels and perceived conflict among ongoing goals: Implications for positive affect. J. Res. Personal. 2009, 43, 938–941. [Google Scholar] [CrossRef]
- Gorges, J.; Esdar, W.; Wild, E. Linking goal self-concordance and affective reactions to goal conflict. Motiv. Emot. 2014, 38, 475–484. [Google Scholar] [CrossRef]
- Klinger, E. Meaning and Void: Inner Experience and the Incentives in People’s Lives; University of Minnesota Press: Minneapolis, MN, USA, 1977. [Google Scholar]
- Cox, W.M.; Klinger, E. A Motivational Model of Alcohol Use: Determinants of Use and Change. In Handbook of Motivational. Counseling: Goal-Based Approaches to Assessment and Intervention with Addiction and Other Problems; Cox, W.M., Klinger, E., Eds.; Wiley: Hoboken, NJ, USA, 2011; pp. 131–158. [Google Scholar]
- Cox, W.M.; Klinger, E. A Psychological-Systems Goal-Theory Model of Alcohol Consumption and Treatment. In The Handbook of Alcohol Use; Frings, D., Albery, I.P., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 237–260. [Google Scholar] [CrossRef]
- Parks, L.; Guay, R.P. Personality, values, and motivation. Personal. Individ. Differ. 2009, 47, 675–684. [Google Scholar] [CrossRef]
- Ruigendijk, H.A.H.; Koole, S.L. When focusing on a goal interferes with action control: Action versus state orientation and over-maintenance of intentions. Motiv. Emot. 2014, 38, 659–672. [Google Scholar] [CrossRef][Green Version]
- Shamloo, Z.S.; Cox, W.M. Information-enhancement and goal setting techniques for increasing adaptive motivation and decreasing urges to drink alcohol. Addict. Behav. 2014, 39, 1205–1213. [Google Scholar] [CrossRef]
- Cox, W.M.; Klinger, E.; Fadardi, J.S. Nonconscious Motivational Influences on Cognitive Processes in Addictive Behaviors. In Addiction and Choice: Rethinking the Relationship; Heather, N., Segal, G., Eds.; Oxford University Press: Oxford, UK, 2016; pp. 258–296. [Google Scholar] [CrossRef]
- Emmons, R.A. Personal strivings: An approach to personality and subjective well-being. J. Personal. Soc. Psychol. 1986, 51, 1058–1068. [Google Scholar] [CrossRef]
- Wiese, B.S.; Salmela-Aro, K. Goal conflict and facilitation as predictors of work-family satisfaction and engagement. J. Vocat. Behav. 2008, 73, 490–497. [Google Scholar] [CrossRef]
- Boiché, J.; Sarrazin, P.; Chanal, J. A longitudinal study of perceived conflict and instrumental relationships between life contexts among adolescents: The role of self-determined motivation. J. Appl. Sport. Psychol. 2015, 27, 430–448. [Google Scholar] [CrossRef]
- Etkin, J.; Evangelidis, I.; Aaker, J. Pressed for Time? Goal Conflict Shapes how Time is Perceived, Spent, and Valued. J. Mark. Res. 2015, 52, 394–406. [Google Scholar] [CrossRef]
- Kehr, H.M. Goal conflicts, attainment of new goals, and well-being among managers. J. Occup. Health. Psychol. 2003, 8, 195–208. [Google Scholar] [CrossRef]
- Elliston, K.G.; Schuz, B.; Ferguson, S.G. Inter-goal conflict and facilitation as predictors of adherence to dieting goals: An ecological momentary assessment study. Psychol. Health. 2020, 35, 701–717. [Google Scholar] [CrossRef]
- Sun, W.; Zheng, Z.; Jiang, Y.; Tian, L.; Fang, P. Does Goal Conflict Necessarily Undermine Wellbeing? A Moderated Mediating Effect of Mixed Emotion and Construal Level. Front. Psychol. 2021, 12, 653512. [Google Scholar] [CrossRef]
- Kindt, S.; Goubert, L.; Ruddere, L.; Cano, A.; Vansteenkiste, M. “What Should I Do First?” The Effect of Manipulated Goal Conflict on Affect, Motivation, and Helping Behavior in Chronic Pain Couples. J. Pain. 2020, 21, 1187–1197. [Google Scholar] [CrossRef]
- Riediger, M. On the Dynamic Relations among Multiple Goals: Intergoal Conflict and Intergoal Facilitation in Younger and Older Adulthood. Available online: http://darwin.inf.fu-berlin.de/2001/266 (accessed on 14 December 2001).
- Riediger, M.; Freund, A.M. Interference and facilitation among personal goals: Differential associations with subjective well-being and persistent goal pursuit. Personal. Soc. Psychol. Bull. 2004, 30, 1511–1523. [Google Scholar] [CrossRef]
- Tomasik, M.J.; Knecht, M.; Freund, A.M. Some evidence for the usefulness of an optimal foraging theory perspective on goal conflict and goal facilitation. J. Pers. Soc. Psychol. 2017, 113, 962–980. [Google Scholar] [CrossRef]
- Beck, J.W.; Scholer, A.A.; Hughes, J. Divergent effects of distance versus velocity disturbances on emotional experiences during goal pursuit. J. Appl. Psychol. 2017, 102, 1109–1123. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with EQS and EQS/Windows: Basic Concepts Applications and Programming; Sage: Thousand Oaks, CA, USA, 1994. [Google Scholar]
- Hofer, M. Goal conflicts and self-regulation: A new look at pupils’ off-task behaviour in the classroom. Educ. Res. Rev. 2007, 2, 28–38. [Google Scholar] [CrossRef]
- Kleiman, T.; Hassin, R.R. Non-conscious goal conflicts. J. Exp. Soc. Psychol. 2011, 47, 521–532. [Google Scholar] [CrossRef]
- Herrmann, M.; Baur, V.; Brandstatter, V.; Hanggi, J.; Jancke, L. Being in two minds: The neural basis of experiencing action crises in personal long-term goals. Soc. Neurosci. 2014, 9, 548–561. [Google Scholar] [CrossRef]
- Wiemers, E.A.; Redick, T.S. Working memory capacity and intra-individual variability of proactive control. Acta. Psychol. 2018, 182, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Klinger, E.; Cox, W. The Motivational Structure Questionnaire, Personal Concerns Inventory, and Their Variants: Psychometric properties. In Handbook of Motivational Counseling: Goal-Based Approaches to Assessment and Intervention with Addiction and Other Problems; Cox, W., Ed.; Wiley-Blackwell: New York, NY, USA, 2011; pp. 204–232. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F.; Rossi, J.S.; Goldstein, M.G.; Marcus, B.H.; Rakowski, W.; Fiore, C.; Harlow, L.L.; Redding, C.A.; Rosenbloom, D.; et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994, 13, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 11th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2021. [Google Scholar]
- Ehlers, L.I. A Validated Model of the South African Labour Relations System; University of Pretoria: Pretoria, South Africa, 2002. [Google Scholar]
- Browne, M.W.; Cudeck, R. Alternative Ways of Assessing Model Fit. In Testing Structural Equation Models; Bollen, K.A., Long, J.S., Eds.; Sage: Thousand Oaks, CA, USA, 1993; pp. 136–162. [Google Scholar]
- Awang, H.Z. Structural Equation Modelling Using AMOS Graphic; UiTM Press: Kuala Lumpur, Malaysia, 2012. [Google Scholar]
- Annis, H.M. The Situational Confidence Questionnaire (SCQ-39); Addiction Research Foundation: Toronto, ON, Canada, 1982. [Google Scholar]
- Rollnick, S.; Heather, N.; Gold, R.; Hall, W. Development of a short “readiness to change” questionnaire for use in brief‚ opportunistic interventions among excessive drinkers. Br. J. Addic. 1992, 87, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Norcross, J.C.; Krebs, P.M.; Prochaska, J.O. Stages of change. J. Clin. Psychol. 2011, 67, 143–154. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Sorgente, A.; Rossi, A.; Simpson, S.; Riva, G.; Manzoni, G.M.; Prochaska, J.O.; Prochaska, J.M.; Cattivelli, R.; Castelnuovo, G. Stages of change in obesity and weight management: Factorial structure of the Italian version of the University of Rhode Island Change Assessment Scale. Eat. Weight. Disord. 2017, 22, 361–367. [Google Scholar] [CrossRef]
- Hilbert, A.; Vogele, C.; Himmelmann, U. Cue reactivity in male restrained eaters: The role of negative cognitions as predictors of food intake. Eat. Weight. Disord. 2007, 12, 27–34. [Google Scholar] [CrossRef]
- Paterson, C.; Lacroix, E.; von Ranson, K.M. Conceptualizing addictive-like eating: A qualitative analysis. Appetite 2019, 141, 104326. [Google Scholar] [CrossRef]
- Klinger, E.; Cox, W.M. Motivation and the Goal Theory of Current Concerns. In Handbook of Motivational Counseling: Goal-based Approaches to Assessment and Intervention with Addiction and Other Problems; Klinger, E., Cox, W.M., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011; pp. 1–47. [Google Scholar] [CrossRef]
- Shamloo, Z.; Shamloo, Z.S.; Cox, W.M. Individual and combined effects of information-enhancement and goal-setting on improving motivational structure. Int. J. Psychol. 2008, 43, 184. [Google Scholar]
- Shamloo, Z.S.; Cox, W.M. The relationship between motivational structure, sense of control, intrinsic motivation and university students’ alcohol consumption. Addict. Behav. 2010, 35, 140–146. [Google Scholar] [CrossRef]

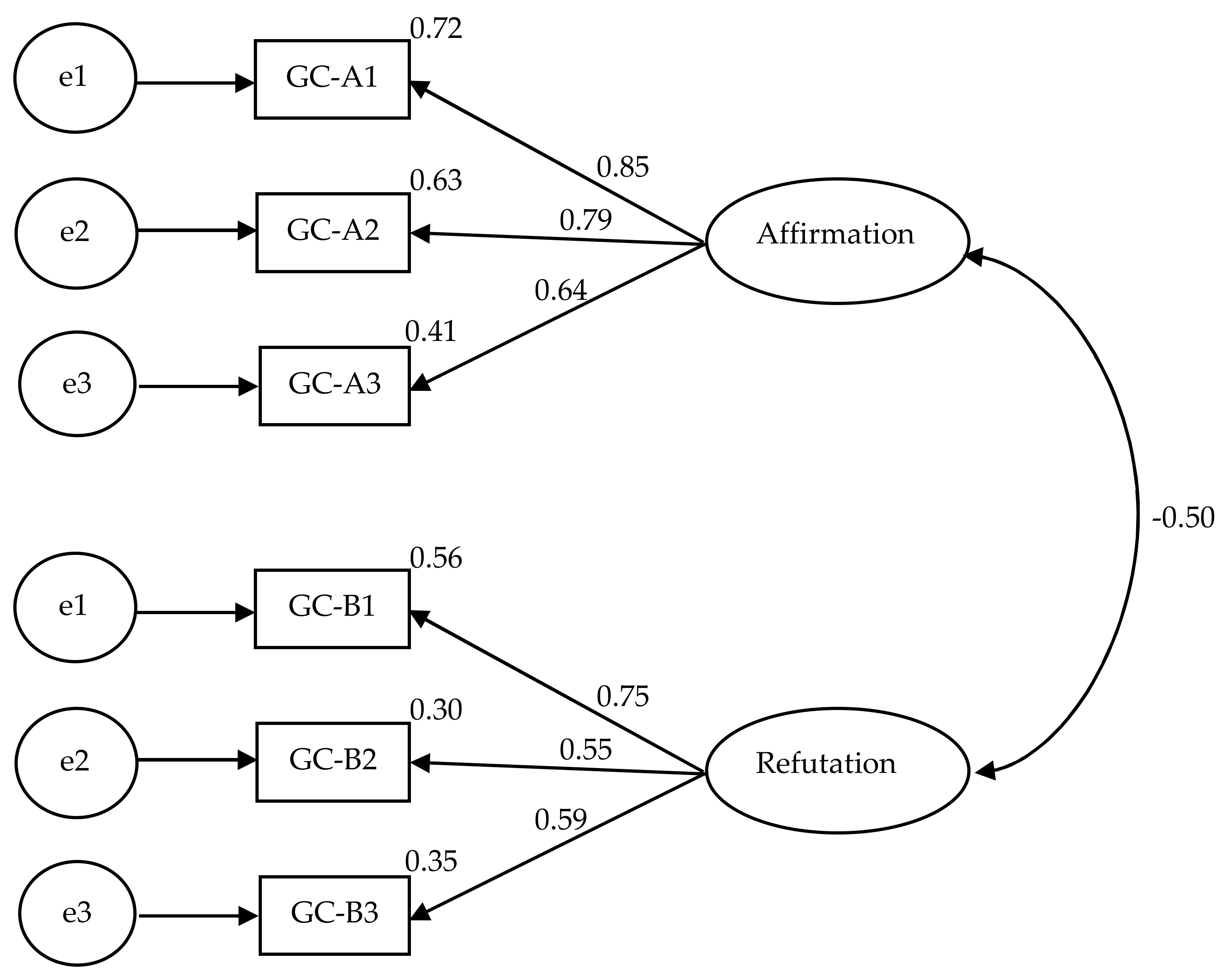
| Study 1 | Study 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| GAS Items | Principal Axis Factoring | Principal Component Analysis | Principal Axis Factoring | Principal Component Analysis | ||||
| 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | |
| Part A (affirmation) | ||||||||
| Item 1 | 0.78 | 0.84 | 0.92 | 0.92 | ||||
| Item 2 | 0.73 | 0.82 | 0.80 | 0.87 | ||||
| Item 3 | 0.64 | 0.79 | 0.52 | 0.68 | ||||
| Part B (refutation) | ||||||||
| Item 1 | 0.56 | 0.68 | 0.47 | 0.63 | ||||
| Item 2 | 0.78 | 0.84 | 0.47 | 0.78 | ||||
| Item 3 | 0.63 | 0.82 | 0.87 | 0.81 | ||||
| Component 1 | Component 2 | GAS Part A (Affirmation) | GAS Part B (Refutation) | |
|---|---|---|---|---|
| GAS Part A | 0.98 ** | 0.20 ** | ||
| GAS Part B | 0.23 ** | 0.97 ** | 0.40 ** | |
| GCLS | 0.69 ** | 0.72 ** | 0.83 ** | 0.86 ** |
| PCA Affirmation | PCA Refutation | GCLS | |
|---|---|---|---|
| Refutation | 0.001 | ||
| GCLS | 0.59 ** | −0.74 ** | |
| Age | 0.088 | −0.25 * | 0.22 * |
| Education | −0.013 | 0.15 | −0.14 |
| Diet History | 0.18 * | −0.035 | 0.13 |
| NO. health con. | 0.19 * | 0.082 | 0.069 |
| Actions to be taken | −0.020 | −0.11 | 0.088 |
| Health info. Required | 0.22 * | 0.016 | 0.16 |
| RTC Precontemplation | −0.19 * | 0.14 | −0.21 * |
| RTC Contemplation | 0.086 | −0.38 ** | 0.36 ** |
| RTC Action | 0.11 | −0.35 ** | 0.39 ** |
| RTC total score | 0.23 * | −0.43 ** | 0.51 ** |
| SCQ: Pleasant Emotions | 0.043 | −0.042 | 0.077 |
| SCQ: Unpleasant Emotions | −0.13 | 0.050 | −0.097 |
| SCQ: Urges and Temptations | 0.048 | −0.005 | 0.029 |
| SCQ: Positive Social Situation | 0.016 | −0.012 | 0.013 |
| SCQ: Social Tension | −0.022 | 0.073 | −0.070 |
| SCQ: Social problems at work | −0.081 | 0.056 | −0.060 |
| SCQ: Testing Personal Control | −0.018 | −0.126 | 0.093 |
| SCQ: Physical Discomfort | −0.090 | −0.079 | −0.005 |
| SCQ total score | −0.055 | 0.004 | −0.029 |
| Experimental Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t (194) | p | |
| Age | 32.78 | 14.16 | 32.68 | 10.94 | 0.056 | 0.96 |
| Education | 14.09 | 3.14 | 14.59 | 3.41 | −1.062 | 0.28 |
| Diet history | 1.84 | 1.29 | 2.13 | 1.47 | −1.50 | 0.14 |
| No. of health concerns | 3.30 | 2.15 | 3.00 | 1.78 | 1.047 | 0.30 |
| Sum of actions | 1.29 | 0.71925 | 1.2816 | .63 | 0.12 | 0.90 |
| Need for information | 1.55 | 1.918 | 1.16 | 1.41 | 1.64 | 0.10 |
| RTC: Precontemplation | −1.95 | 3.72 | −1.067 | 3.28 | −1.75 | 0.083 |
| RTC: Contemplation | 4.12 | 3.33 | 3.63 | 3.47 | 0.99 | 0.32 |
| RTC: Action | 3.13 | 3.46 | 2.75 | 3.29 | 0.77 | 0.44 |
| RTC total score | 9.17 | 6.65 | 7.59 | 6.84 | 1.63 | 0.10 |
| SCQ: Pleasant emotions | 75.11 | 20.94 | 69.23 | 21.43 | 1.94 | 0.054 |
| SCQ: Unpleasant emotions | 66.95 | 57.11 | 60.00 | 26.84 | 1.11 | 0.26 |
| SCQ: Urges and temptations | 62.88 | 26.36 | 53.89 | 24.95 | 2.45 | 0.015 |
| SCQ: Positive social situation | 64.67 | 25.74 | 56.15 | 24.93 | 2.35 | 0.020 |
| SCQ: Social tension | 63.91 | 30.91 | 59.13 | 28.18 | 1.13 | 0.26 |
| SCQ: Social problems at work | 73.040 | 56.22 | 57.40 | 27.76 | 2.51 | 0.013 |
| SCQ: Testing personal control | 64.13 | 26.024 | 60.57 | 24.36 | 0.99 | 0.32 |
| SCQ: Physical discomfort | 65.87 | 27.46 | 61.051 | 26.17 | 1.26 | 0.21 |
| SCQ total score | 67.029 | 23.99 | 59.65 | 18.77 | 2.41 | 0.017 |
| Age | Edu. | Diet History | No. Health Con. | Sum of Actions | Health Info. Required | RTC Total Score | SCQ Total Score | |
|---|---|---|---|---|---|---|---|---|
| Age | 0.46 ** | 0.058 | −0.035 | 0.19 | 0.31 * | −0.12 | 0.38 ** | |
| Edu. | −0.17 * | 0.15 | 0.15 | −0.039 | 0.27 | 0.025 | 0.33 * | |
| Diet history | 0.16 * | 0.12 | 0.18 | −0.15 | 0.14 | 0.31 * | −0.064 | |
| No. health con. | 0.031 | −0.016 | 0.20 * | 0.16 | 0.24 | 0.25 | 0.043 | |
| Sum of actions | 0.001 | −0.064 | −0.069 | 0.20 * | −0.096 | −0.031 | 0.13 | |
| Health info. required | 0.005 | 0.13 | −0.022 | 0.26 ** | 0.21 * | 0.18 | 0.24 | |
| RTC total score | 0.22 ** | 0.049 | 0.28 ** | 0.22 ** | 0.011 | 0.11 | 0.07 | |
| SCQ total score | 0.083 | −0.034 | −0.11 | −0.16 * | −0.14 | 0.017 | −0.062 |
| Main Effect | Interaction | Covariate | Pairwise Comparison | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | Group F [p] η2 | Sex F [p] η2 | Group*Sex F [p] η2 | Age F [p] η2 | Diet Hist. F [p] η2 | Edu. F [p] η2 | No. Health Concern F [p] η2 | Exp M (SD) | Ctrl M (SD) | Result |
| Models 1–4, F (1, 188) | ||||||||||
| 1. Plan for action | 0.39 [0.53] 0.002 | 1.50 [0.065] 0.018 | 0.40 [0.53] 0.002 | 0.33 [0.57] 0.002 | 2.80 [0.09] 0.015 | 0.50 [0.48] 0.003 | 9.15 [0.003] 0.047 | 1.29 (0.71) | 1.25 (0.60) | |
| 2. Need for info. | 4.16 [0.043] 0.022 | 1.41 [0.221] 0.008 | 2.029 [0.156] 0.011 | 1.34 [0.24] 0.007 | 0.88 [0.35] 0.005 | 6.19 [0.014] 0.032 | 13.49 [0.001] 0.068 | 1.55 (1.92) | 1.16 (1.42) | |
| 3. RTC total score | 5.06 [0.026] 0.026 | 0.28 [0.59] 0.001 | 1.22 [0.27] 0.006 | 2.69 [0.102] 0.014 | 11.03 [0.001] 0.055 | 0.31 [0.57] 0.002 | 3.59 [0.026] 0.026 | 9.17 (6.65) | 7.27 (7.07) | Exp > Ctrl |
| 4. SCQ total score | 5.18 [0.017] 0.030 | 0.40 [0.52] 0.002 | 0.21 [0.64] 0.001 | 5.24 [0.023] 0.027 | 1.65 [0.20] 0.009 | 2.022 [0.15] 0.011 | 2.76 [0.098] 0.014 | 67.02 (23.99) | 60.21 (19.00) | Exp > Ctrl |
| Model 5, F (3, 190) | 2.65 [0.049] 0.040 | 0.96 [0.41] 0.014 | 0.46 [0.70] 0.007 | 6.30 [0.001] 0.092 | 4.24 [0.001] 0.062 | 2.60 [0.05] 0.039 | 5.84 [0.001] 0.085 | Exp > Ctrl | ||
| RTC: Precontemplation | 4.79 [0.030] 0.024 | 0.74 [0.389] 0.004 | 0.36 [0.550] 0.002 | 3.34 [0.069] 0.017 | 2.67 [0.10] 0.014 | 6.030 [0.015] 0.030 | 0.66 [0.42] 0.003 | −1.95 (3.719) | −1.046 (3.270) | Exp < Ctrl |
| RTC: Contemplation | 2.28 [0.133] 0.012 | 35 [0.556] 0.002 | 0.69 [0.408] 0.004 | 2.34 [0.13] 0.012 | 8.96 [0.003] 0.045 | 1.103 [0.29] 0.006 | 13.86 [0.000] 0.067 | 4.12 (3.33) | 3.44 (3.60) | |
| RTC: Action | 2.64 [0.106] 0.014 | 2.23 [0.137] 0.011 | 0.84 [0.361] 0.004 | 16.59 [0.001] 0.080 | 5.97 [0.015] 0.030 | 0.252 [0.62] 0.001 | 0.093 [0.76] 0.000 | 3.13 (3.45) | 2.56 (3.39) | |
| Model 6, F (8, 185) | 1.89 [0.064] 0.076 | .63 [0.75] 0.027 | 1.087 [0.37] 0.045 | 1.64 [0.12] 0.066 | 0.73 [0.67] 0.031 | 2.17 [0.031] 0.086 | 1.32 [0.24] 0.054 | |||
| SCQ: Pleasant emotions | 5.39 [0.021] 0.027 | 0.30 [0.58] 0.002 | 0.94 [0.33] 0.005 | 4.30 [0.039] 0.022 | 0.29 [0.59] 0.001 | 4.24 [0.041] 0.022 | 1.91 [0.16] 0.010 | 75.10 (20.93) | 69.44 (21.52) | Exp > Ctrl |
| SCQ: Unpleasant emotions | 0.76 [0.38] 0.004 | 0.66 [0.42] 0.003 | 0.025 [0.87] 0.001 | 0.59 [0.44] 0.003 | 0.657 [0.42] 0.003 | 0.073 [0.79] 0.001 | 0.76 [0.38] 0.004 | 66.95 (57.17) | 60.56 (26.65) | |
| SCQ: Urge and temptation | 7.42 [0.007] 0.037 | 0.29 [0.59] 0.001 | 1.20 [0.27] 0.006 | 7.35 [0.007] 0.037 | 0.019 [0.89] 0.000 | 4.971 [0.027] 0.025 | 0.170 [0.68] 0.001 | 62.88 (26.37) | 54.49 (25.08) | Exp > Ctrl |
| SCQ: Positive social situations | 1.92 [0.17] 0.010 | 0.37 [0.54] 0.002 | 0.55 [0.46] 0.003 | 9.83 [0.002] 0.049 | 2.15 [0.14] 0.011 | 0.16 [0.69] 0.001 | 0.10 [0.75] 0.001 | 64.67 (25.74) | 57.13 (24.99) | |
| SCQ: Social tension | 1.99 [0.160] 0.010 | 1.13 [0.29] 0.006 | 0.84 [0.36] 0.004 | 0.70 [0.40] 0.004 | 2.12 [0.15] 0.011 | 1.64 [0.20] 0.008 | 3.078 [0.081] 0.016 | 63.91 (30.92) | 59.90 (28.00) | |
| SCQ: Social problems at work | 4.04 [0.046] 0.021 | 0.008 [0.92] 0.001 | 0.047 [0.83] 0.001 | 0.62 [0.43] 0.003 | 1.56 [0.21] 0.008 | 0.003 [0.96] 0.000 | 2.38 [0.12] 0.012 | 73.038 (56.23) | 58.33 (27.90) | Exp > Ctrl |
| SCQ: Testing self-control | 0.91 [0.34] 0.005 | 0.076 [0.78] 0.001 | 0.004 [0.95] 0.001 | 9.67 [0.002] 0.048 | 1.23 [0.27] 0.006 | 2.061 [0.15] 0.11 | 3.050 [0.082] 0.016 | 64.13 (26.02) | 60.65 (24.43) | |
| SCQ: Physical discomfort | 3.39 [0.067] 0.017 | 0.10 [0.75] 0.001 | 1.16 [0.28] 0.006 | 1.68 [0.19] 0.009 | 0.82 [0.36] 0.004 | 8.06 [0.005] 0.040 | 4.00 [0.047] 0.020 | 65.87 (27.46) | 61.39 (25.92) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fadardi, J.S.; Borhani, S.; Cox, W.M.; Stacy, A.W. Do I Really Want to Change? The Effectiveness of Goal Ambivalence Feedback on Dieters’ Motivation. Behav. Sci. 2022, 12, 441. https://doi.org/10.3390/bs12110441
Fadardi JS, Borhani S, Cox WM, Stacy AW. Do I Really Want to Change? The Effectiveness of Goal Ambivalence Feedback on Dieters’ Motivation. Behavioral Sciences. 2022; 12(11):441. https://doi.org/10.3390/bs12110441
Chicago/Turabian StyleFadardi, Javad S., Samiyeh Borhani, W. Miles Cox, and Alan W. Stacy. 2022. "Do I Really Want to Change? The Effectiveness of Goal Ambivalence Feedback on Dieters’ Motivation" Behavioral Sciences 12, no. 11: 441. https://doi.org/10.3390/bs12110441
APA StyleFadardi, J. S., Borhani, S., Cox, W. M., & Stacy, A. W. (2022). Do I Really Want to Change? The Effectiveness of Goal Ambivalence Feedback on Dieters’ Motivation. Behavioral Sciences, 12(11), 441. https://doi.org/10.3390/bs12110441






