Comparison of Risk Stratification Tools for Atherosclerotic Cardiovascular Disease and Cardiovascular–Kidney–Metabolic Syndrome in Primary Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. Statistical Analysis
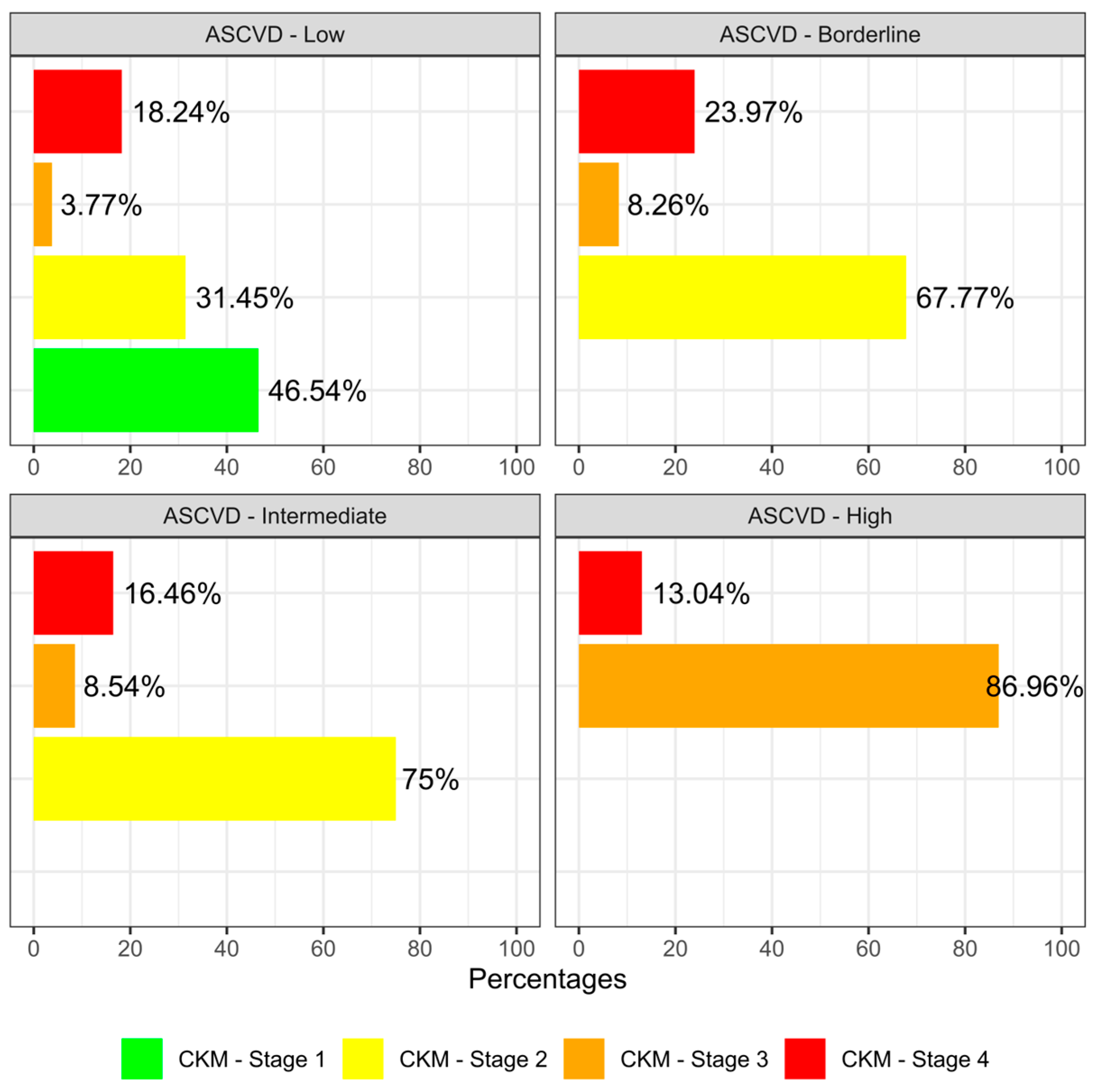
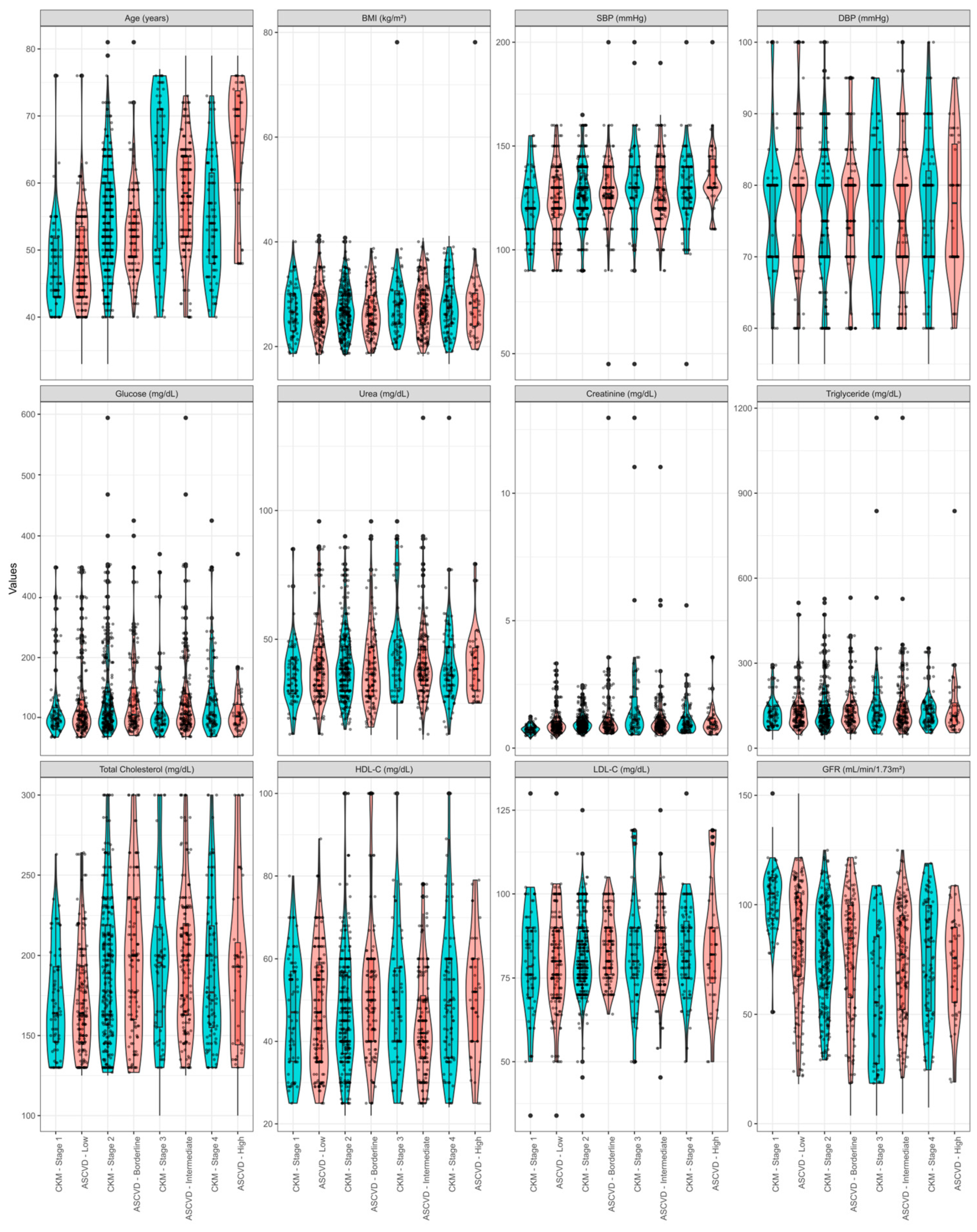
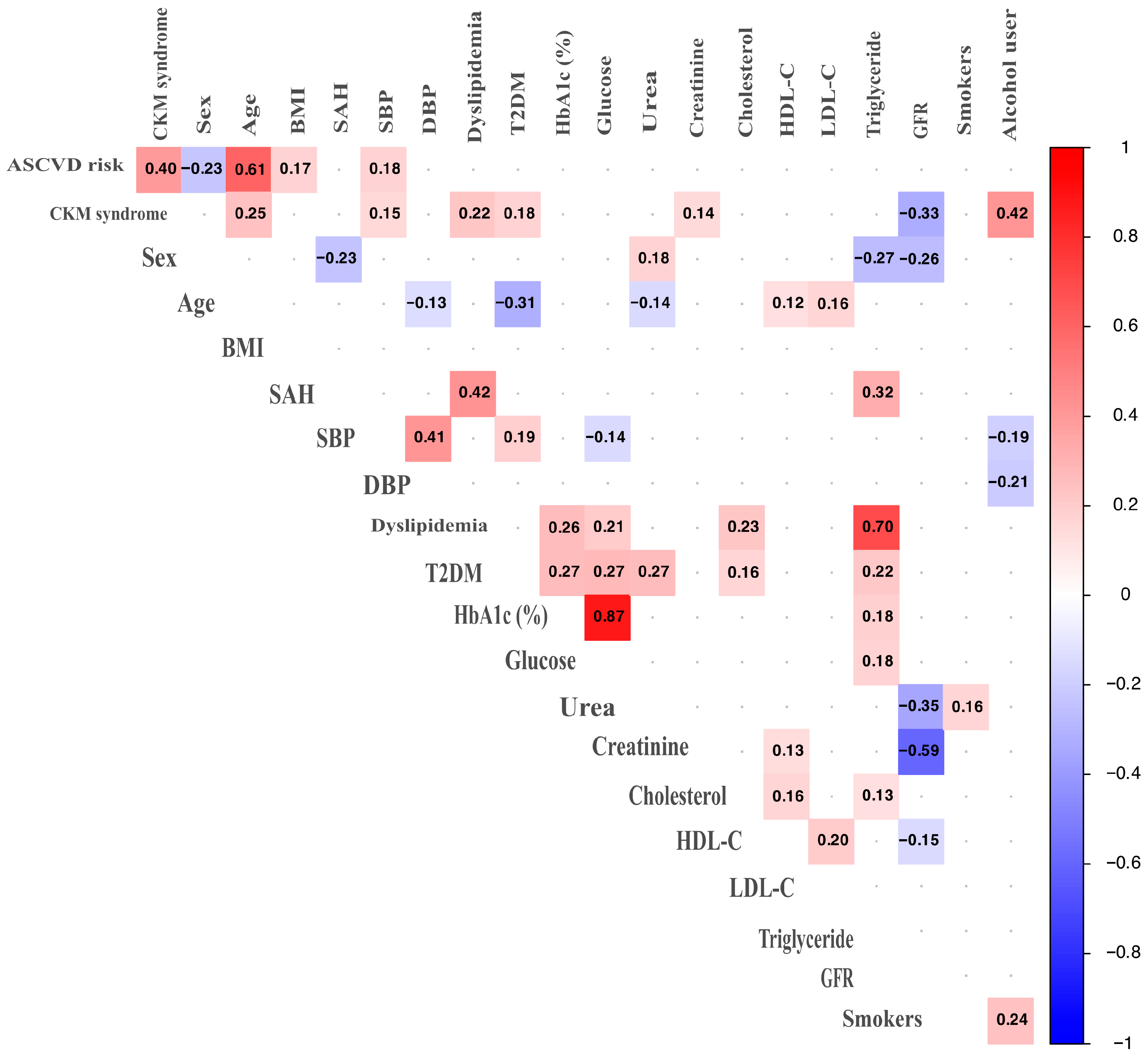
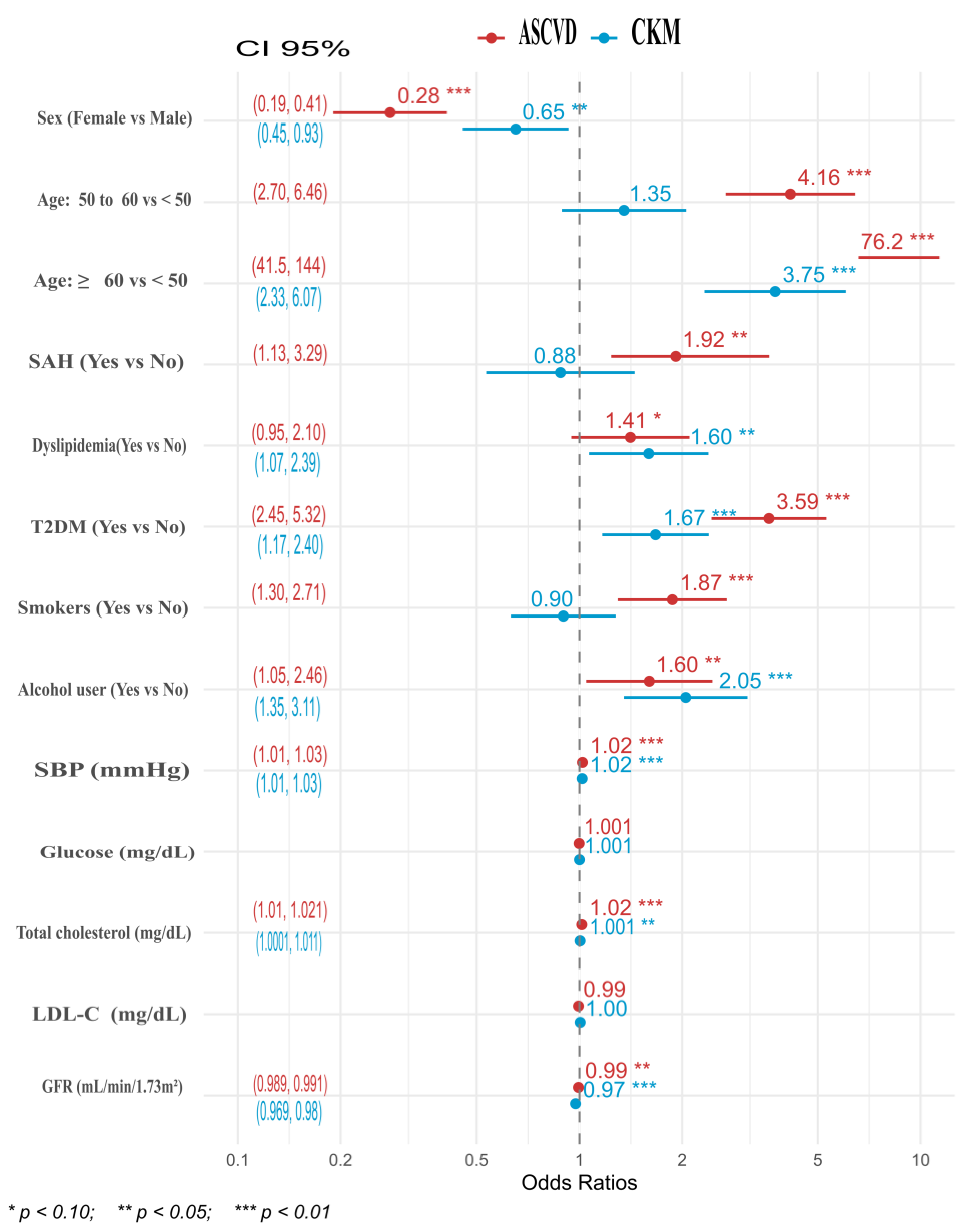
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ASCVD | Atherosclerotic cardiovascular disease |
| CKM | Cardiovascular–kidney–metabolic |
| CKD | Chronic kidney disease |
| NCDs | Chronic non-communicable diseases |
| DBP | Diastolic blood pressure |
| GFR | Glomerular filtration rate |
| HbA1c | Glycated hemoglobin |
| HDL-C | High-density lipoprotein cholesterol |
| LDL-C | Low-density lipoprotein cholesterol |
| SAH | Systemic arterial hypertension |
| SBP | Systolic blood pressure |
| T2DM | Type 2 diabetes mellitus |
References
- Khan, M.A.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Al Suwaidi, S.K.B.M.; Alkatheeri, R.; Alblooshi, F.M.K.; Almatrooshi, M.E.A.H.; Alzaabi, M.E.H.; Al Darmaki, R.S.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Q.; Zhou, S.; Zhong, H.; Wang, Z.; Liu, C.; Sun, J.; Deng, J. Global, regional, and national burden and risk factors of ischemic heart disease, 1990–2021: An analysis of the global burden of disease study. Front. Public Health 2025, 13, 1563631. [Google Scholar] [CrossRef]
- Lanas, F.; Soto, A. Trends in Mortality from Ischemic Heart Disease in the Region of the Americas, 2000–2019. Glob. Heart 2022, 17, 53. [Google Scholar] [CrossRef]
- Basto-Abreu, A.; López-Olmedo, N.; Rojas-Martínez, R.; Aguilar-Salinas, C.A.; Moreno-Banda, G.L.; Carnalla, M.; Rivera, J.A.; Romero-Martinez, M.; Barquera, S.; Barrientos-Gutiérrez, T. Prevalencia de prediabetes y diabetes en México: Ensanut 2022. Salud Publica Mex. 2023, 65, s163–s168. [Google Scholar] [CrossRef]
- Campos-Nonato, I.; Oviedo-Solís, C.; Vargas-Meza, J.; Ramírez-Villalobos, D.; Medina-García, C.; Gómez-Álvarez, E.; Hernández-Barrera, L.; Barquera, S. Prevalencia, tratamiento y control de la hipertensión arterial en adultos mexicanos: Resultados de la Ensanut 2022. Salud Publica Mex. 2023, 65, s169–s180. [Google Scholar] [CrossRef]
- Escamilla-Núñez, M.C.; Castro-Porras, L.; Romero-Martínez, M.; Zárate-Rojas, E.; Rojas-Martínez, R. Detección, diagnóstico previo y tratamiento de enfermedades crónicas no transmisibles en adultos mexicanos. Ensanut 2022. Salud Publica Mex. 2023, 65 (Suppl. S1), S153–S162. [Google Scholar] [CrossRef] [PubMed]
- Goff, D.C.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk. Circulation 2014, 129 (Suppl. S2), 2935–2959. [Google Scholar] [CrossRef]
- Ndumele, C.E.; Rangaswami, J.; Chow, S.L.; Neeland, I.J.; Tuttle, K.R.; Khan, S.S.; Coresh, J.; Mathew, R.O.; Baker-Smith, C.M.; Carnethon, M.R.; et al. Cardiovascular-Kidney-Metabolic Health: A Presidential Advisory From the American Heart Association. Circulation 2023, 148, 1606–1635. [Google Scholar] [CrossRef]
- Ndumele, C.E.; Neeland, I.J.; Tuttle, K.R.; Chow, S.L.; Mathew, R.O.; Khan, S.S.; Coresh, J.; Baker-Smith, C.M.; Carnethon, M.R.; Després, J.-P.; et al. A Synopsis of the Evidence for the Science and Clinical Management of Cardiovascular-Kidney-Metabolic (CKM) Syndrome: A Scientific Statement From the American Heart Association. Circulation 2023, 148, 1636–1664. [Google Scholar] [CrossRef]
- Cases, A.; Broseta, J.J.; Marqués, M.; Cigarrán, S.; Julián, J.C.; Alcázar, R.; Ortiz, A. Cardiovascular-kidney-metabolic syndrome definition and its role in the prevention, risk staging, and treatment. An opportunity for the Nephrology. Nefrologia (Engl. Ed.) 2024, 44, 771–783. [Google Scholar] [CrossRef] [PubMed]
- Fernando, K.; Connolly, D.; Darcy, E.; Evans, M.; Hinchliffe, W.; Holmes, P.; Strain, W.D. Advancing Cardiovascular, Kidney, and Metabolic Medicine: A Narrative Review of Insights and Innovations for the Future. Diabetes Ther. 2025, 16, 1155–1176. [Google Scholar] [CrossRef]
- Marassi, M.; Fadini, G.P. The cardio-renal-metabolic connection: A review of the evidence. Cardiovasc. Diabetol. 2023, 22, 195. [Google Scholar] [CrossRef] [PubMed]
- Özyüncü, N.; Erol, Ç. From Metabolic Syndrome to Cardiovascular-Kidney-Metabolic Syndrome and Systemic Metabolic Disorder: A Call to Recognize the Progressive Multisystemic Dysfunction. Anatol. J. Cardiol. 2025, 29, 384–393. [Google Scholar] [CrossRef]
- Skou, S.T.; Mair, F.S.; Fortin, M.; Guthrie, B.; Nunes, B.P.; Miranda, J.J.; Boyd, C.M.; Pati, S.; Mtenga, S.; Smith, S.M. Multimorbidity. Nat. Rev. Dis. Primers 2022, 8, 48. [Google Scholar] [CrossRef]
- Goldsborough, E.; Osuji, N.; Blaha, M.J. Assessment of Cardiovascular Disease Risk. Endocrinol. Metab. Clin. N. Am. 2022, 51, 483–509. [Google Scholar] [CrossRef]
- Kruskal, W.H.; Wallis, W.A. Use of Ranks in One-Criterion Variance Analysis. J. Am. Stat. Assoc. 1952, 47, 583. [Google Scholar] [CrossRef]
- Drasgow, F. Encyclopedia of Statistical Science, Polychoric and Polyserial Correlations; Kotz, S., Johnson, N., Eds.; Wiley: Hoboken, NJ, USA, 1986; Volume 7, pp. 68–74. [Google Scholar]
- McCullagh, P. Regression Models for Ordinal Data. J. R. Stat. Soc. Series B Stat. Methodol. 1980, 42, 109–127. [Google Scholar] [CrossRef]
- Fagerland, M.W.; Hosmer, D.W. How to Test for Goodness of Fit in Ordinal Logistic Regression Models. Stata J. Promot. Commun. Stat. Stata 2017, 17, 668–686. [Google Scholar] [CrossRef]
- Pregibon, D. Goodness of Link Tests for Generalized Linear Models. J. R. Stat. Soc. Ser. C (Appl. Stat.) 1980, 29, 15–23. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Braun, L.T.; Ndumele, C.E.; Smith, S.C., Jr.; Sperling, L.S.; Virani, S.S.; Blumenthal, R.S. Use of Risk Assessment Tools to Guide Decision-Making in the Primary Prevention of Atherosclerotic Cardiovascular Disease: A Special Report From the American Heart Association and American College of Cardiology. Circulation 2019, 139, e1162–e1177. [Google Scholar] [CrossRef] [PubMed]
- Mutruc, V.; Bologa, C.; Șorodoc, V.; Ceasovschih, A.; Morărașu, B.C.; Șorodoc, L.; Catar, O.E.; Lionte, C. Cardiovascular–Kidney–Metabolic Syndrome: A New Paradigm in Clinical Medicine or Going Back to Basics? J. Clin. Med. 2025, 14, 2833. [Google Scholar] [CrossRef]
- Aggarwal, R.; Ostrominski, J.W.; Vaduganathan, M. Prevalence of Cardiovascular-Kidney-Metabolic Syndrome Stages in US Adults, 2011–2020. JAMA 2024, 331, 1858. [Google Scholar] [CrossRef]
- Kaufmann, J.; Marino, M.; Lucas, J.A.; Rodriguez, C.J.; Boston, D.; Giebultowicz, S.; Heintzman, J. Atherosclerotic Cardiovascular Disease Primary and Secondary Prevention in Latino Subgroups. J. Gen. Intern. Med. 2024, 39, 2041–2050. [Google Scholar] [CrossRef] [PubMed]
- Guadamuz, J.S.; Kapoor, K.; Lazo, M.; Eleazar, A.; Yahya, T.; Kanaya, A.M.; Cainzos-Achirica, M.; Bilal, U. Understanding Immigration as a Social Determinant of Health: Cardiovascular Disease in Hispanics/Latinos and South Asians in the United States. Curr. Atheroscler. Rep. 2021, 23, 25. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, M.R.; Ardehali, M.; Diamantidis, C.J.; Corsino, L. The diabetes cardiovascular outcomes trials and racial and ethnic minority enrollment: Impact, barriers, and potential solutions. Front. Public Health 2024, 12, 1412874. [Google Scholar] [CrossRef] [PubMed]
- Reininger, B.M.; Wang, J.; Fisher-Hoch, S.P.; Boutte, A.; Vatcheva, K.; McCormick, J.B. Non-communicable diseases and preventive health behaviors: A comparison of Hispanics nationally and those living along the US-Mexico border. BMC Public Health 2015, 15, 564. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary. J. Am. Coll. Cardiol. 2019, 73, 3168–3209. [Google Scholar] [CrossRef]
- Gavina, C.; Carvalho, D.S.; Pardal, M.; Afonso-Silva, M.; Grangeia, D.; Dinis-Oliveira, R.J.; Araújo, F.; Taveira-Gomes, T. Cardiovascular Risk Profile and Lipid Management in the Population-Based Cohort Study LATINO: 20 Years of Real-World Data. J. Clin. Med. 2022, 11, 6825. [Google Scholar]
- Madaudo, C.; Bono, G.; Ortello, A.; Astuti, G.; Mingoia, G.; Galassi, A.R.; Sucato, V. Dysfunctional High-Density Lipoprotein Cholesterol and Coronary Artery Disease: A Narrative Review. J. Pers. Med. 2024, 14, 996. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; A Ference, B.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Ference, B.A.; Yoo, W.; Alesh, I.; Mahajan, N.; Mirowska, K.K.; Mewada, A.; Kahn, J.; Afonso, L.; Williams, K.A.; Flack, J.M. Effect of Long-Term Exposure to Lower Low-Density Lipoprotein Cholesterol Beginning Early in Life on the Risk of Coronary Heart Disease. J. Am. Coll. Cardiol. 2012, 60, 2631–2639. [Google Scholar] [CrossRef]
- Gavina, C.; Seabra-Carvalho, D.; Aguiar, C.; Anastassopoulou, A.; Teixeira, C.; Ruivo, J.A.; Almeida, É.; Luz-Duarte, L.; Corte-Real, A.; Canelas-Pais, M.; et al. Characterization and LDL-C management in a cohort of high and very high cardiovascular risk patients: The PORTRAIT-DYS study. Clin. Cardiol. 2024, 47, e24183. [Google Scholar] [CrossRef]
- Whelton, S.P.; McEvoy, J.W.; Shaw, L.; Psaty, B.M.; Lima, J.A.C.; Budoff, M.; Nasir, K.; Szklo, M.; Blumenthal, R.S.; Blaha, M.J. Association of Normal Systolic Blood Pressure Level With Cardiovascular Disease in the Absence of Risk Factors. JAMA Cardiol. 2020, 5, 1011. [Google Scholar] [CrossRef] [PubMed]
- Ndejjo, R.; Masengere, P.; Bulafu, D.; Namakula, L.N.; Wanyenze, R.K.; Musoke, D.; Musinguzi, G. Drivers of cardiovascular disease risk factors in slums in Kampala, Uganda: A qualitative study. Glob. Health Action 2023, 16, 2159126. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Regional Health-Americas. Cardiovascular disease: Addressing poverty is key. Lancet Reg. Health Am. 2025, 42, 101029. [Google Scholar]
- Wang, Y.; Duan, Y.; Zhang, Y.; Li, N.; Hu, Y.; Gu, L.; Hou, Y.; Ma, Y. Alcohol consumption, high-sensitivity C-reactive protein, and estimated glomerular filtration rate: Tripartite predictors of 10-year cardiovascular risk progression in patients with type 2 diabetes mellitus after COVID-19. Front. Endocrinol. 2025, 16, 1609144. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Hu, L.; Chen, A.; Wu, Y.; Wang, G.; Xie, X.; He, Q.; Xue, Y.; Lin, J.; Zheng, Z.; et al. Relationship between moderate alcohol consumption and all-cause mortality across different stages of Cardiovascular-Kidney-Metabolic (CKM) Syndrome: A cohort study. Nutr. Metab. Cardiovasc. Dis. 2025, in press. [Google Scholar] [CrossRef]
- Trimarco, V.; Izzo, R.; Pacella, D.; Manzi, M.V.; Trama, U.; Lembo, M.; Piccinocchi, R.; Gallo, P.; Esposito, G.; Morisco, C.; et al. Increased prevalence of cardiovascular-kidney-metabolic syndrome during COVID-19: A propensity score-matched study. Diabetes Res. Clin. Pract. 2024, 218, 111926. [Google Scholar] [CrossRef]
- Mocumbi, A.O. Cardiovascular Health Care in Low- and Middle-Income Countries. Circulation 2024, 149, 557–559. [Google Scholar] [CrossRef]
| Total | ASCVD Risk | CKM Syndrome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 500 | Low | Borderline | Intermediate | High | p-Value 1 | Stage 1 | Stage 2 | Stage 3 | Stage 4 | p-Value 1 | |
| n = 160 | n = 124 | n = 170 | n = 46 | n = 74 | n = 263 | n = 72 | n = 91 | ||||
| Sex | |||||||||||
| Male | 222 (44) | 53 (33) | 64 (52) | 80 (47) | 25 (54) | 0.004 | 34 (46) | 114 (43) | 32 (44) | 42 (46) | 0.959 |
| Female | 278 (56) | 107 (67) | 60 (4) | 90 (53) | 21 (46) | 40 (54) | 149 (57) | 40 (56) | 49 (54) | ||
| Age | |||||||||||
| <50 years | 170 (34) | 94 (59) | 48 (39) | 23 (14) | 5 (11) | <0.001 | 47 (64) | 73 (28) | 17 (24) | 33 (36) | <0.001 |
| ≥50 and <60 years | 194 (39) | 57 (36) | 62 (50) | 68 (40) | 7 (15) | 24 (32) | 124 (47) | 17 (24) | 29 (32) | ||
| ≥60 years | 136 (27) | 9 (5.6) | 14 (11) | 79 (46) | 34 (74) | 3 (4.1) | 66 (25) | 38 (53) | 29 (32) | ||
| BMI | |||||||||||
| Underweight to healthy weight | 186 (37) | 60 (38) | 55 (44) | 54 (32) | 17 (37) | 0.437 | 30 (41) | 100 (38) | 25 (35) | 31 (34) | 0.963 |
| Overweight | 174 (35) | 58 (36) | 40 (32) | 61 (36) | 15 (33) | 23 (31) | 93 (35) | 25 (35) | 33 (36) | ||
| Obese | 140 (28) | 42 (26) | 29 (23) | 55 (32) | 14 (30) | 21 (28) | 70 (27) | 22 (31) | 27 (30) | ||
| SAH | |||||||||||
| Yes | 427 (85) | 131 (82) | 106 (85) | 148 (87) | 42 (91) | 0.354 | 63 (85) | 225 (86) | 64 (89) | 75 (82) | 0.715 |
| Dyslipidemia | |||||||||||
| Yes | 136 (27) | 37 (23) | 31 (25) | 57 (34) | 11 (24) | 0.149 | 12 (16) | 75 (29) | 18 (25) | 31 (34) | 0.069 |
| T2DM | |||||||||||
| Yes | 287 (57) | 71 (44) | 80 (65) | 110 (65) | 26 (57) | <0.001 | 30 (41) | 158 (60) | 43 (60) | 56 (62) | 0.017 |
| Smokers | |||||||||||
| Yes | 228 (46) | 72 (45) | 54 (44) | 80 (47) | 22 (48) | 0.925 | 36 (49) | 124 (47) | 30 (42) | 38 (42) | 0.677 |
| Alcohol user | |||||||||||
| Yes | 114 (23) | 36 (23) | 33 (27) | 33 (19) | 12 (26) | 0.489 | 13 (18) | 55 (21) | 22 (31) | 24 (26) | 0.187 |
| Total n = 500 | ASCVD Risk | CKM Syndrome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Borderline | Intermediate | High | p-Value 1 | Stage 1 | Stage 2 | Stage 3 | Stage 4 | p-Value 1 | ||
| n = 160 | n = 124 | n = 170 | n = 46 | n = 74 | n = 263 | n = 72 | n = 91 | ||||
| Age (years) | 54 ± 9 | 49 ± 7 | 53 ± 6 | 58 ± 8 | 66 ± 10 | <0.001 | 48 ± 6 | 54 ± 8 | 61 ± 11 | 55 ± 9 | <0.001 |
| BMI (kg/m2) | 27.2 ± 5.4 | 27.2 ± 5.0 | 26.4 ± 4.7 | 27.6 ± 5.0 | 28.2 ± 8.7 | 0.236 | 26.9 ± 5.2 | 26.8 ± 4.7 | 28.2 ± 7.4 | 27.8 ± 5.5 | 0.502 |
| SBP (mmHg) | 127 ± 17 | 124 ± 17 | 128 ± 18 | 128 ± 16 | 135 ± 16 | <0.001 | 121 ± 16 | 127 ± 15 | 131 ± 21 | 129 ± 18 | <0.001 |
| DBP (mmHg) | 77 ± 9 | 77 ± 10 | 78 ± 8 | 75 ± 9 | 77 ± 9 | 0.160 | 77 ± 9 | 76 ± 9 | 78 ± 9 | 77 ± 10 | 0.800 |
| HbA1c (%) | 6.9 ± 1.7 | 6.9 ± 1.7 | 7.1 ± 1.6 | 7.1 ± 1.8 | 6.4 ± 1.3 | 0.302 | 6.4 ± 1.5 | 7.2 ± 1.7 | 6.7 ± 1.6 | 6.9 ± 1.8 | 0.039 |
| Glucose (mg/dL) | 128 ± 65 | 127 ± 64 | 133 ± 64 | 130 ± 70 | 113 ± 47 | 0.318 | 118 ± 58 | 132 ± 69 | 116 ± 55 | 133 ± 64 | 0.029 |
| Urea (mg/dL) | 40 ± 15 | 40 ± 15 | 39 ± 16 | 40 ± 15 | 40 ± 12 | 0.600 | 36 ± 12 | 40 ± 13 | 45 ± 20 | 39 ± 16 | 0.057 |
| Creatinine (mg/dL) | 1.1 ± 0.9 | 0.9 ± 0.5 | 1.2 ± 1.2 | 1.1 ± 1.0 | 1.0 ± 0.5 | 0.104 | 0.7 ± 0.2 | 1.0 ± 0.4 | 1.8 ± 2.0 | 1.1 ± 0.7 | <0.001 |
| Total cholesterol (mg/dL) | 191 ± 47 | 173 ± 35 | 202 ± 51 | 200 ± 48 | 190 ± 53 | <0.001 | 172 ± 32 | 195 ± 49 | 198 ± 52 | 190 ± 45 | 0.003 |
| HDL-C (mg/dL) | 48 ± 15 | 48 ± 14 | 51 ± 17 | 44 ± 13 | 51 ± 13 | <0.001 | 47 ± 13 | 47 ± 14 | 49 ± 15 | 50 ± 17 | 0.381 |
| LDL-C (mg/dL) | 82 ± 14 | 80 ± 17 | 84 ± 10 | 81 ± 11 | 84 ± 18 | 0.043 | 80 ± 19 | 81 ± 11 | 83 ± 16 | 83 ± 13 | 0.319 |
| Triglyceride (mg/dL) | 141 ± 102 | 130 ± 67 | 136 ± 76 | 153 ± 135 | 145 ± 120 | 0.859 | 122 ± 53 | 137 ± 79 | 185 ± 201 | 130 ± 59 | 0.151 |
| GFR (mL/min/1.73 m2) | 78 ± 27 | 84 ± 27 | 78 ± 28 | 74 ± 26 | 73 ± 22 | 0.002 | 104 ± 15 | 77 ± 23 | 58 ± 30 | 75 ± 28 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vázquez Martínez, V.H.; Martínez Bautista, H.; Muñoz Villegas, P.; Loera Morales, J.I.; Salazar, M.d.R.P. Comparison of Risk Stratification Tools for Atherosclerotic Cardiovascular Disease and Cardiovascular–Kidney–Metabolic Syndrome in Primary Care. Med. Sci. 2025, 13, 240. https://doi.org/10.3390/medsci13040240
Vázquez Martínez VH, Martínez Bautista H, Muñoz Villegas P, Loera Morales JI, Salazar MdRP. Comparison of Risk Stratification Tools for Atherosclerotic Cardiovascular Disease and Cardiovascular–Kidney–Metabolic Syndrome in Primary Care. Medical Sciences. 2025; 13(4):240. https://doi.org/10.3390/medsci13040240
Chicago/Turabian StyleVázquez Martínez, Victor Hugo, Humberto Martínez Bautista, Patricia Muñoz Villegas, Jesús III Loera Morales, and María del Rosario Padilla Salazar. 2025. "Comparison of Risk Stratification Tools for Atherosclerotic Cardiovascular Disease and Cardiovascular–Kidney–Metabolic Syndrome in Primary Care" Medical Sciences 13, no. 4: 240. https://doi.org/10.3390/medsci13040240
APA StyleVázquez Martínez, V. H., Martínez Bautista, H., Muñoz Villegas, P., Loera Morales, J. I., & Salazar, M. d. R. P. (2025). Comparison of Risk Stratification Tools for Atherosclerotic Cardiovascular Disease and Cardiovascular–Kidney–Metabolic Syndrome in Primary Care. Medical Sciences, 13(4), 240. https://doi.org/10.3390/medsci13040240






